Preparing for anesthesia
To ensure that the removal of an ovarian cyst goes well for a woman, and that anesthesia does not cause side effects, several rules should be followed:
- Before the operation, all organs and systems are examined. For this purpose, a general blood test, urine test, and heart function are checked using an electrocardiogram;
- if a woman takes medications, she must inform the anesthesiologist and surgeon about this;
- the day before surgery to remove the cyst, the gastrointestinal tract is cleansed using enemas or laxatives;
- Avoid eating at least 18 hours before surgery, and follow a strict diet for a week before surgery.
If you follow these recommendations, the postoperative period will be favorable and recovery will be quick.
Features of the use of anesthesia
The choice of anesthesia for knee arthroscopy depends on the goals. Will this be a routine diagnosis that requires a small amount of time for the procedure? Or a full-fledged surgical intervention on the knee joint will be carried out and will take a lot of time.
Anesthesia for laparoscopic knee surgery:
- Multicomponent anesthesia. It contains several types of drugs. These are intravenous and volatile anesthetics, muscle relaxants, artificial ventilation. This anesthesia is easy to use because it is easily controlled, the patient’s consciousness is turned off, and the body is completely immobilized. But in addition to its positive qualities, this type of anesthesia is complex and requires careful preoperative preparation.
- Intravenous administration of anesthetic drugs. Spontaneous breathing is maintained. They are used only in diagnostics, since the patient’s muscles are in good shape, which is unacceptable for therapeutic manipulations.
- Epidural anesthesia. This is the most commonly administered type of anesthesia for arthroscopy. Pain relief begins from the waist down to the feet. You can turn off the sensation in your legs, but still maintain motor function. After surgery, epidural anesthesia continues to provide pain relief to the limb.
- Use of local anesthetics. This is only appropriate for minor interventions and does not require the presence of an anesthesiologist.
- Spinal anesthesia. Just like the epidural, it is indicated for long-term operations. There is a risk of a drop in blood pressure with this type of anesthesia, but it can be raised with medications.
Learn about anesthesia during laparoscopy in this video.
Laparoscopy currently remains one of the most accurate methods for diagnosing diseases and pathological conditions. Therefore, it is important to choose the right anesthesia when performing it.
Under what anesthesia is laparoscopy of an ovarian cyst performed?
The choice of type of anesthesia for laparoscopy of an ovarian cyst depends on many factors:
- volume of surgical intervention;
- how urgent is laparoscopy;
- patient test results data;
- the presence of concomitant pathologies;
- blood pressure level.
There are two types of anesthesia that are used to remove an ovarian cyst:
- General anesthesia, in which the woman is completely unconscious.
- Local and epidural anesthesia, which is characterized by preserved consciousness in the patient.
The types of anesthesia are briefly described in the following video:
General anesthesia
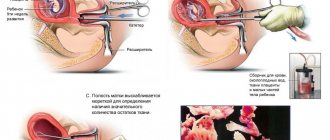
Depending on the method of introducing the anesthetic into the body, there are several types of general anesthesia for ovarian laparoscopy:
- Endotracheal - the anesthetic enters the body due to tracheal intubation.
- Inhalation - the anesthetic substance is inhaled through a special mask.
- Intravenous - an anesthetic drug is administered through a catheter into a peripheral vein.
- Spinal - the drug is injected under the arachnoid membrane of the spinal cord.
A feature of endotracheal general anesthesia when performing ovarian laparoscopy is the need for intubation. To do this, the anesthesiologist inserts a tube under visual control into the patient's trachea. The presence of a tube prevents gastric contents from entering the lungs, and the anesthetic goes directly into the respiratory tract.
Attention! It is this type of general anesthesia that is most common during laparoscopy. Its main advantage is the need for less anesthetic.
And this, in turn, means less toxic effects on the body during laparoscopy.
Inhalation general anesthesia is used much less frequently during ovarian laparoscopy.
Medication-induced sleep using intravenous drugs is used for short-term operations. Spinal anesthesia is used in emergency situations.
Epidural anesthesia
Epidural anesthesia is used for planned interventions that should not take a long time. When an ovarian cyst is removed under epidural anesthesia, the drug is injected into the space near the dura mater that surrounds the spinal cord. The injection of anesthetic causes complete loss of sensation below the puncture site.
The greatest advantage of epidural anesthesia over general anesthesia during ovarian laparoscopy is the lack of effect on the central nervous system. The anesthetic acts strictly on a limited area of the body.
But this method also has a number of disadvantages. During laparoscopy of an ovarian cyst under local anesthesia, gastric masses may enter the respiratory tract. This is due to the fact that during the operation the pressure in the abdominal cavity increases and the contents of the stomach are literally pushed upward.
Another disadvantage of epidural anesthesia is the need for parallel injection of sedatives. Because of this, respiratory function may be impaired, which leads to a lack of oxygen in the blood.
Possible complications of anesthesia
- The presence of gas bubbles in the bloodstream and blockage of blood vessels by them (air embolism).
- Impaired patency (thrombosis) of the deep veins or pulmonary artery.
- The presence of air in one part of the pleural cavity (pneumothorax).
- Malfunctions of the cardiovascular system.
- Rejection of gastric contents into the esophagus.
- Violation of the integrity of the dura mater.
- Pain in the back and head varies in duration after surgery.
The choice of anesthesia method is the responsibility of the anesthesiologist. The choice is made based on the purpose of surgery, age criteria and the general condition of the patient.
Possible consequences after anesthesia
Nowadays, removal of ovarian cysts has become an almost routine operation, and the likelihood of complications after anesthesia is minimal. But in rare cases, the following unpleasant consequences occur:
- slow heartbeat;
- aspiration of gastrointestinal contents;
- pneumothorax - air entering the cavity surrounding the lungs;
- disruption of blood flow in the vessels due to blockage by a blood clot;
- allergy to anesthetic;
- purulent inflammation of soft tissues due to improper administration of anesthetic;
- respiratory depression.
When performing epidural anesthesia in patients with bleeding disorders, a hematoma may form in the spinal canal.
Warning! Approximately 5% of women who underwent laparoscopy for ovarian cysts under epidural anesthesia had partial or no pain relief.
How is anesthesia administered during laparoscopy?
General anesthesia, which is widely used in general surgery, involves complete loss of consciousness and sensitivity of nerve endings. Throughout the laparoscopic procedure, the anesthesiologist monitors the patient’s reaction to anesthesia and also maintains his vital signs (heart rate, blood pressure).
Drugs are administered intravenously through a catheter or by inhalation of inhaled drugs through a breathing apparatus or a combination of both. The anesthetic is administered in different dosages at different stages of anesthesia and the course of the operation, and its concentration depends on the general condition of the patient. More painful stages during surgery require a greater depth of anesthesia.
In addition to general, regional or local anesthesia, the use of sedation is practiced in medical practice. This is the simplest type of anesthesia, which is performed during minimally invasive procedures (colonoscopy, computed tomography or magnetic resonance imaging studies) to protect the patient from discomfort and allay his fears.
Removing stones without cholecystectomy
Before planned laparoscopic surgery, drug treatment of concomitant pathologies is carried out. In case of exacerbation of complications or inflammatory processes, a course of antibiotics is prescribed. In preparation for gallbladder removal in complicated cholelithiasis, preparations with bile acids are used to normalize the composition of bile. Treatment may precede and then continue after the ectomy to prevent recurrence of duct stones.
Direct preparation for laparoscopy of the gallbladder includes a complete diagnostic examination:
- lab tests;
- Ultrasound;
- ECG.
The patient eats in the evening; before surgery, fasting is indicated for 8-10 hours. In the morning he is given an enema. If the patient is able to take care of himself, he can prepare for surgery and remove hair on the abdomen.
The research results enable the surgeon to prepare for work. Before cholecystectomy, the doctor needs to have an idea of the location, number, size of stones, and associated pathological changes in organs.
Surgical techniques used in gallbladder removal
Currently, two well-established techniques are mainly used: traditional abdominal surgery and laparoscopy. Their main difference is the method of access to the organ being removed.
The traditional technique involves providing access to the operating area through a sufficiently large incision in the abdominal wall. In this case, the surgeon has direct visual contact with the organ being removed. The main disadvantages of such an intervention include:
- large size of the postoperative scar, causing aesthetic discomfort;
- quite a long rehabilitation period;
- high risk of postoperative complications.
In this regard, such operations are performed mainly in emergency cases and when, for some reason, laparoscopic surgery is contraindicated for the patient.
For planned operations in the absence of contraindications, the laparoscopy method is used.
The essence of this surgical intervention is that access to the operated organ is provided through three to four small (up to one and a half centimeters) punctures in the peritoneal wall. Through one of these punctures, a laparoscope is inserted (hence the name of the technique - laparoscopy) with a flashlight and a video camera attached to it, the image from which is displayed on the monitor and allows the surgeon to control the progress of the operation (without direct visual contact). Through the remaining punctures using special hollow tubes (trocars) special surgical instruments are introduced, with the help of which resection of the gallbladder is performed.
To ensure free access to the operating area, the abdominal cavity is pumped with gas (usually carbon dioxide) before surgery. In addition, this allows for much better visualization of internal organs, blood vessels and nerve plexuses in the area of the intervention.
Advantages of laparoscopy over conventional abdominal surgery:
- scars after such an intervention are almost invisible;
- since the impact on other internal organs is minimal, the likelihood of postoperative complications is significantly reduced;
- The recovery time for the body after such a minimally invasive intervention is much shorter than after a traditional one (often the patient is discharged from the hospital on the second or third day after gallstone laparoscopy).
Read also: Why does bad breath occur due to problems with the gallbladder?
Laparoscopic cholecystectomy
It is worth saying that in the event of any unforeseen complications during laparoscopic intervention, the operation can be interrupted and continued in the traditional abdominal manner.
Modern medical science does not stand still, and currently there are already surgical techniques in which incisions in the peritoneal wall are not needed at all. This is the so-called transgastric (through the mouth) and transvaginal cholecystectomy. However, currently these methods of removing the gallbladder are at the stage of clinical testing, so we will not dwell on them in detail.
A very important point when performing not only cholecystectomy, but also any surgical intervention, is anesthesia.
Let's say right away - cholecystectomy does not imply local anesthesia, and is always performed under general anesthesia (and during laparoscopy, too).
This is due to the fact that the use of local anesthesia does not give the surgeon the necessary freedom of action, since the organs of the patient who are not immersed in sleep remain in a tense state.
Types of anesthesia used to perform laparoscopic operations
- Peredural anesthesia
Its essence is to perform a puncture of the epidural space, with the introduction of a medicinal substance into it that blocks sensitivity in the lower parts of the body. Recommended for use in patients with severe concomitant diseases of the cardiovascular and respiratory systems. Allows you to monitor the patient’s condition and quickly learn about the development of possible complications during surgery. If the technique is followed correctly, this method of pain relief provides a minimum of complications.
May occur in case of short-term diagnostic interventions. For this purpose, a solution of lidocaine or novocaine is most often used, which is used to inject the insertion site of the instrument. When choosing this method of pain relief, the doctor must take into account the characteristics of the action of a particular drug, its consumption, and duration of action.
- Conduction anesthesia
Achieved by injecting an anesthetic into the area located around a large nerve trunk. Due to this, the transmission of the nerve impulse signaling pain is blocked. A distinctive feature of this method is that the absence of pain sensitivity is achieved only in a specific area of the body, while maintaining consciousness.
Achieved by administering a drug or a mixture of drugs through intravenous injection. This type of general anesthesia can only be performed by an anesthesiologist. It is used in cases where a short-term surgical intervention or diagnostic procedure is expected.
It involves the introduction of a narcotic substance into the patient’s body through the respiratory system, through a special mask and tube. Intubation is performed after the patient, having received a small dose of anesthetic through a mask, falls asleep. To ensure uninterrupted breathing, the patient is connected to a machine that provides artificial ventilation. The breathing apparatus has such a structure that it allows you to change the concentration of anesthetic in the respiratory mixture, controlling the depth of anesthesia. When the surgical part of the intervention is completed, the anesthesiologist reduces the amount of anesthetic, and then begins to gradually remove it from the body, increasing the concentration of oxygen in the gas mixture.
Types of anesthesia
Among the anesthetic drugs recommended for use during laparoscopy are inhalation and non-inhalation anesthetics. The first group includes nitrous oxide, fluorothane or halothane, desflurane, isoflurane. Non-inhalational anesthetics are propofol, calypsol or ketamine, relanium, midazolam, droperidol. The choice of drug is made by an anesthesiologist based on the complexity of the planned intervention and the individual characteristics of the patient’s body. The effectiveness of inhalational and non-inhalational anesthetics is equivalent when removing an ovarian cyst.
Indications for laparoscopic surgery
Laparoscopy is performed both for diagnostic purposes (during examination of organs) and for the treatment of detected inflammations. It is prescribed when it is impossible to determine the disease using ultrasound, computed tomography, magnetic resonance therapy, etc.
Indications for laparoscopy:
- Gynecology. Used to determine infertility, if a tumor is suspected in the uterus and its appendages. In emergency cases of damage to the internal genital organs of a woman; threat of tubal pregnancy; inflammation.
- Surgical diseases. Acute diseases in the abdominal cavity that have unclear symptoms (pancreatitis, appendicitis).
- Jaundice. To determine the type of disease (hepatic or subhepatic form). Investigation of the cause of disruption of the normal flow of bile.
- Complex or closed injuries to the abdomen, head and limbs. In particular, laparoscopy is performed on persons with alcohol and drug intoxication, coma and traumatic shock. The procedure is prescribed to eliminate the risk of internal bleeding, limb injury and peritonitis.
- Various wounds in the abdominal cavity, ascites with unclear symptoms. The degree of organ damage, the presence of bleeding and inflammatory processes are diagnosed.
- Peritonitis after surgery with vague clinical symptoms.
- Tumors. Clarifying the diagnosis, establishing the boundaries of the tumor, determining metastases to other organs.
Diagnostics using laparoscopy allows you to clarify the patient’s diagnosis.