Types of hysterectomy operations
When prescribing surgery to remove the uterus (hysterectomy), doctors take into account not only the nature of the disease, but also the woman’s age. If she is young, then they try to preserve at least the ovaries so that the hormonal levels in the body are not disrupted and the patient’s life is not further complicated by the consequences of a lack of estrogen.
There are several options for performing a hysterectomy. One of them is amputation of the uterine body (subtotal hysterectomy) with preservation of the cervix, tubes and ovaries.
Extirpation of the uterus (total hysterectomy) is an operation in which the organ is cut out along with the cervix. There are 2 types of operation:
- Removal of the uterus and cervix without appendages. If a woman manages to save her ovaries, her quality of life does not deteriorate, since the production of sex hormones continues. If she wants to have a child, she can use the services of a surrogate mother, who will be implanted with the patient’s own eggs.
- Removal of the organ along with the cervix and appendages - fallopian tubes and ovaries (hysterosalpingo-oophorectomy).
Note: Surgeons, taking into account the nuances of the operation, also distinguish intrafascial, extrafascial and extended extirpation.
The most difficult option is the so-called radical hysterectomy, that is, removal of the uterus, cervix, appendages, upper part of the vagina and nearby lymph nodes.
Video: Indications and contraindications for hysterectomy. Possible consequences
https://youtu.be/6Kuv9fCTRwg
https://youtu.be/ZubdEWxCPGY
Rehabilitation
To minimize the negative consequences after surgery to remove the uterus and ovaries, you should adhere to some recommendations regarding lifestyle and diet. Rehabilitation after a hysterectomy lasts from one to one and a half months, depending on the type of operation and the severity of the clinical case.
During the recovery period, pain in the lower abdomen, uncharacteristic vaginal discharge and prolapse of its walls are possible. Neurotic disorders are not excluded.
General restrictions for all categories of patients include:
- Do not lift heavy objects (weighing more than three kilograms);
- minimize physical activity;
- do not have sex for 4-6 weeks;
- do not take a bath or swim in the pool for two months.
Patients are advised to adhere to a diet to prevent anemia. Your diet should include beef, pomegranates, apples and other foods rich in iron. The doctor may prescribe medications to compensate for the deficiency of this microelement. High fiber foods are recommended to prevent constipation. You should exclude flour, smoked, sweet, carbonated drinks and alcohol.
The specialist should also tell the patient how to properly care for postoperative sutures. They need to be treated with antiseptic solutions after careful rinsing in the shower using regular soap.
If absorbable materials were used to close the surgical wound, no additional visit to the doctor is required to remove the sutures. In other situations, the surgeon removes the sutures in an inpatient setting. After removing the sutures, scars should be treated using ointments, gels, and creams that accelerate resorption.
The doctor should also recommend wearing compression stockings to prevent complications such as thrombophlebitis. Rehabilitation measures should also include:
- physiotherapeutic techniques;
- therapeutic exercises;
- Kegel exercises to strengthen the pelvic floor muscles to prevent
- urinary incontinence.
Physiotherapy
The prescription of physiotherapeutic techniques is rational for the correction of conditions such as:
- urinary incontinence due to bladder hypotension;
- tissue fibrosis;
- swelling of the legs;
- post-castration syndrome.
In order to alleviate the course of post-castration syndrome, so that life after removal of the appendages and uterus does not cause difficulties, electrosleep is prescribed. This technique significantly reduces the intensity of vegetative-vascular and neuropsychic disorders.
To prevent and correct disorders of the urination process, neuromuscular stimulation with sinusoidal modulated currents is prescribed. And in order to improve blood flow and stimulate regenerative processes, low-frequency magnetic therapy is used, which also promotes faster resorption of edema.
Swelling of the legs can also be relieved using pneumatic lymphatic drainage. Wearing compression stockings also helps eliminate the problem.
However, physiotherapy cannot be prescribed in the following situations:
- pathologies of the blood coagulation system;
- neoplasms of any localization;
- acute phase of inflammatory diseases;
- decompensated stages of chronic diseases;
- cachexia;
- mental disorders;
- general serious condition.
Exercise therapy
Therapeutic gymnastics exercises are designed to strengthen muscles and ensure a speedy return to a normal lifestyle. A physical therapy doctor will help you choose a complex. Once again, the value of performing Kegel exercises should be mentioned: with their help, you can normalize the processes of defecation and urination, which may be disrupted after surgery.
Indications and contraindications for
Extirpation of the uterus is performed in extreme cases when its preservation is impossible due to the increased risk of developing severe and life-threatening complications.
Indications for such an operation are:
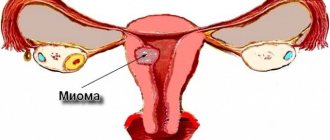
- The presence of numerous rapidly growing fibroids in the cavity or on its outer surface. Twisting of tumors that have a long thin stalk leads to tissue necrosis, peritonitis and sepsis.
- Uterine prolapse (a problem that occurs in older women);
- Heavy uterine bleeding that cannot be eliminated by conservative methods.
- Endometriosis in severe form.
- The formation of numerous polyps in the organ cavity.
- Detection of malignant tumors of the body of the uterus or its cervix. In this case, a radical hysterectomy is often performed.
The ovaries are removed if cysts or tumors are found in them.
A contraindication to extirpation is the presence of infectious diseases and inflammatory processes in the woman in the vagina, cervix, and other organs (for example, in the respiratory tract, bladder). Extirpation is not performed on patients with severe cardiac, respiratory or renal failure.
Indications
Indications for emergency hysterectomy are diffuse peritonitis after childbirth and abortion, necrosis of the myomatous node, nascent fibroids, twisting of the pedicle of the subserous myoma node.
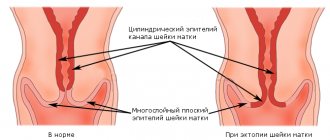
Indications for planned hysterectomy without removal of appendages include uterine fibroids when nodes are located in the isthmus and cervix area, rapidly growing uterine fibroids, a combination of uterine fibroids with erosion and deformation of the cervix, stage zero cervical cancer in women over 40 years of age, body cancer stage 1 uterus in young women.
Indications for panhysterectomy are malignant ovarian tumors, common inflammatory processes of the internal genital organs with damage to the ovaries, as well as pathological processes in which extirpation of the uterus without removal of the appendages is indicated (see above), in combination with ovarian pathology. Often the question of the need to remove appendages arises only during surgery, often after a solid histological examination of the removed organs.
Extended hysterectomy is performed for stage I and II cervical cancer as one of the stages of combined treatment. There is an opinion about the advisability of extended hysterectomy for uterine cancer, with the exception of elderly patients, who prefer to undergo panhysterectomy.
Extirpation methods
Removal of the uterus, cervix and possibly the appendages is done in three main ways: through an incision in the peritoneum (laparotomy), punctures in the abdomen (laparoscopy) or through the vagina (vaginal hysterectomy).
Laparotomy
More often, a horizontal incision is made below the navel, and the suture is less noticeable. Less commonly, a vertical incision is made.
Open access to the abdominal cavity allows for a thorough examination. If during the operation it is discovered that the lesion is more extensive than expected, then not only the appendages, but also the lymph nodes can be immediately removed.
Typically, extirpation is performed using this method if the uterus is large, as well as if there is advanced endometritis. Careful removal of the uterus will avoid the spread of the inflammatory process to other organs.
Laparotomy is performed for endometriosis, cancer, in the presence of constant uterine bleeding and pain of unknown origin.
The advantage of this operation is good access to the abdominal organs and the use of cheaper equipment. There are many disadvantages: a high probability of complications during and after surgery, a long recovery period. There is a stitch left on the stomach.
Laparoscopy
Hysterectomy is performed through several small incisions in the abdomen into which a video camera and surgical instruments are inserted.
The advantages of this technique are that punctures heal approximately 2 times faster than large incisions, and there are practically no traces of surgical intervention left. The use of optics gives the doctor the opportunity to clearly control the manipulation during the operation, since the image is displayed on the monitor screen. Possible use of robotics.
The disadvantage is the limited use of the technique: it is not suitable if the organ is large, there are adhesions in the abdominal cavity, if the patient has poor blood clotting.
Vaginal extirpation
The operation is mainly performed for complete or incomplete prolapse of the uterus in combination with weakening of the pelvic floor muscles, urinary retention, the formation of fibroids, ovarian cysts, and endometriosis.
There are contraindications to the use of this method. Extirpation through the vagina is impossible if the patient has malignant tumors of the genitourinary organs, as well as sexually transmitted diseases. The technique is not used in the presence of large benign tumors of the uterus and ovaries, or the formation of adhesions between the uterus, ovaries and neighboring organs.
The advantage is the absence of a postoperative suture on the abdomen.
Procedure
Laparoscopic removal is performed using a special laparoscope apparatus. The woman is given anesthesia, which leads to general anesthesia. The operation then proceeds according to the points below.
- The surface of the abdomen is treated with special antiseptics for disinfection.
- Several incisions are made in the peritoneum to insert instruments. First, carbon dioxide is released to separate the peritoneal walls from the organs. This expands your horizons.
- Then a laparoscope with a video camera is inserted, which displays the image on the screen.
- A manipulator is inserted into the next incision, which is used to perform all the actions of excision and removal of the organ. To do this, first the ligaments are cut off, the vessels are cauterized, then the uterus is cut off and removed through the vagina. If the organ is too large, it is crushed inside and then removed.
- Afterwards, the vessels are ligated and the peritoneum is examined for the presence of postoperative blood and lymphatic fluid.
- Eliminate carbon dioxide and remove all instruments.
- Sutures are placed at the insertion sites of the manipulators.
Such an operation can last 15 minutes, or maybe 1.5 hours. It all depends on the extent of the disease and the diagnosis leading to laparoscopic hysterectomy.
The procedure for performing the operation is shown in the picture.
Preparation for the operation
Special preparation is required for hysterectomy. Preliminary examination includes:
If necessary, diagnostic curettage is performed using a hysteroscope, as well as examination of the vagina using colposcopy. A biopsy may be performed to perform a cytological examination of the sample and detect abnormal cells.
The operation is not performed during menstruation.
During extirpation, the intestines should be completely empty, so within 2-3 days the woman should switch to a diet with a predominant intake of liquid light foods. Avoid the consumption of gas-forming products and those containing fiber. In the last 8-10 hours before the operation, you should not eat at all; it is advisable to drink as little as possible. This will avoid vomiting after general anesthesia.
Before the operation, a cleansing enema is performed, the pubic and vaginal area is shaved. A catheter is installed in the bladder, which is not removed in the first days after the operation.
Even before the operation, the anesthesiologist finds out whether the patient is allergic to medications and selects a combination of anesthetics taking into account the individual characteristics of the patient’s body. Various types of anesthesia are used: endotracheal (deep narcotic sleep), spinal and epidural anesthesia (through the spine).
Is pregnancy possible after surgery?
A hysterectomy involves removing the uterus. The uterus is the organ in which the child is born. If there is no uterus, then there can be no talk of pregnancy. After the operation, the woman does not even menstruate.
If a woman dreams of having a child after such an operation, then the only way out for her may be surrogacy or adoption of a child from an orphanage.
Recovery period after extirpation
Restorative treatment includes pain relief and the administration of antibiotics to prevent inflammatory processes. Sedatives and vitamins are also prescribed. Intravenous infusions of saline solution with glucose are carried out to eliminate the consequences of blood loss and disturbances in the water-salt balance in the body. The patient should drink a lot and often to replenish fluid loss by the body.
Sutures or punctures are treated daily with antiseptic solutions, lubricated with syntomycin ointment or levomekol, and sterile napkins are applied.
For 6 to 8 weeks after surgery, women should wear compression stockings or wrap their legs with elastic bandages to prevent blood clots.
Within a few hours after laparoscopy and the next day after laparotomy, it is necessary to get up, change body position, and walk so that adhesions do not form in the abdominal cavity and the organs take a normal position. After laparotomy, the woman must wear a bandage that tightens the abdomen for 1 month. This prevents seams from coming apart and reduces pain.
It is necessary to regulate intestinal function through diet and prevent constipation.
You can resume sexual activity no earlier than the doctor confirms that the stitches have completely healed and your general health has been restored.
Surgical interventions on the internal genital organs can be performed using both laparotomy and laparoscopic approaches.
Before the operation, the surgical field (the entire anterior abdominal wall) is treated with antiseptic solutions. The surgical field is limited by sheets, leaving the incision site free.
With laparotomy access for surgical intervention on the pelvic organs, it is necessary to open the anterior abdominal wall. The most acceptable in gynecology are median transections and a transverse incision according to Pfannenstiel. With a midline incision, the anterior abdominal wall is opened layer by layer from the pubis (upper edge) to the navel.
When making a Pfannenstiel incision, the skin and subcutaneous tissue are dissected with a transverse incision parallel to the pubis and 3-4 cm above it. The length of the incision is usually 10-12 cm. The aponeurosis is opened in the form of a horseshoe, the upper edges of the incisions on both sides should be at the level of the navel . The intermuscular fascia (between the rectus abdominis muscles) is opened sharply during any incision. When opening the peritoneum, it is important to lift it with soft tweezers and carefully dissect it (in the middle between the pubis and the navel) so as not to damage the intestinal loops and bladder under the pubis. The peritoneum is fixed with clamps to napkins, which are placed along the incision on both sides. The anterior abdominal wall can be dissected either with a scalpel or with an electric knife with coagulation or ligation of vessels with suture material (silk, catgut, vicryl).
After dissection of the anterior abdominal wall, it is necessary to visually and palpate the abdominal organs with a hand inserted into the abdominal cavity. Then the dilator is inserted, and the intestinal loops are carefully moved with a napkin into the upper abdominal cavity, thereby ensuring visibility and accessibility of the pelvic organs.
When removing an organ or part of an organ, first of all, the vessels are clamped, and then they are crossed, followed by ligation. You can cut fabrics with scissors. To apply sutures to the ligamentous apparatus, vessels, cervical stumps and vaginal walls, silk, catgut, vicryl, etc. are used.
Fallopian tube removal technique.
To remove the fallopian tube, regardless of the nosological form of the disease, to the mesosalpinx and the isthmus of the fallopian tube, in which the branches of the ovarian and uterine pass
arteries and veins, apply a clamp (Kocher). The tube is cut off above the clamps and removed from the abdominal cavity (the material is sent for histological examination). The mesosalpinx is sutured under the clamp and a ligature is tied, carefully removing the Kocher clamp. After cutting off the isthmus of the tube, 1-2 separate sutures are applied to the angle of the uterus.
Peritonization can be performed with a continuous suture, connecting the layers of the peritoneum of the broad uterine ligament. The area of the isthmus of the tube is usually peritonized by the round uterine ligament.
Technique for removing the uterine appendages.
Operating clamps (Kocher) are applied to the infundibulopelvic ligament, which contains the ovarian artery; mesosalpinx; the own ligament of the ovary with the branches of the ovarian and uterine vessels passing through it; isthmus of the pipe. The uterine appendages are cut off above the clamps. The stumps are ligated with separate sutures. Peritonization is carried out by the leaves of the peritoneum of the broad uterine ligaments and the round uterine ligament. After cutting, the uterine appendages are removed from the abdominal cavity and sent for histological examination (Fig. 22.1, a, b).
Supravaginal amputation of the uterus (subtotal, supravaginal) without appendages.
Surgical clamps (Kocher) are applied alternately on both sides to the rib of the uterus. The lower edge of the clamp should be at the level of the internal pharynx. In this case, the clamp contains the fallopian tube (isthmus), round uterine ligament, and the ovarian ligament. 0.5-1 cm lateral to the previous clamp, apply a separate clamp to the round uterine ligament and a clamp to the fallopian tube and the proper ovarian ligament. The “noses” of the lateral clamps should be at the same level. The ligaments are crossed between the clamps. Using scissors, a piece of the peritoneum of the vesicouterine fold is opened from the front, and the bladder is lowered downwards. From behind, the posterior leaf of the broad uterine ligament is opened in the direction of the uterosacral ligaments (to avoid ligation and injury to the ureters). The round ligaments and stumps of the uterine appendages are separately sutured and bandaged. Vascular clamps are applied perpendicularly to the uterine vessels at the level of the internal os on both sides. The vessels are crossed and sutured with separate ligatures. The body of the uterus is cut off at the level of the internal os above the ligatures of the uterine vessels and removed from the abdominal cavity. Separate ligatures are applied to the cervical stump. Peritonization of the stumps of the uterine appendages and its cervix is carried out with a continuous suture using the leaves of the broad uterine ligaments and the leaves of the vesicouterine fold (Fig. 22.2, a-g).
Rehabilitation period
After laparoscopic hysterectomy, the recovery period does not take much time, unlike abdominal surgery. After 10 hours, patients can get out of bed. In the absence of complications and a favorable clinical picture, women are discharged on the fourth day. The doctor's decision also depends on the complexity of the operation using the laparoscopic technique. During the first few days, it is important to take medications to reduce pain, as well as antibiotic medications. They will help prevent possible infection of the body.
After laparoscopic extirpation, it is recommended to adhere to a special diet:
- the first day you are allowed to drink still mineral water and rosehip infusions;
- on the second day you can introduce fermented milk products into the diet;
- on the third day, chicken meat chopped in a blender, broth or fruit puree are allowed.
On average, the recovery period after laparoscopic extirpation is about one month. It is recommended to refrain from visiting the sauna and steam baths, and also to maintain sexual rest.
If, a few days after laparoscopic extirpation of the uterine cavity, girls experience heavy discharge with blood streaks or pus, inflammation of the punctures, as well as an increase in body temperature. In this case, you should urgently seek help from a doctor. To avoid possible postoperative complications, during the rehabilitation period, patients need to do special Kegel exercises and include physical therapy classes. They help strengthen the muscular walls of the vagina, eliminate defecation and urination problems.
In some cases, it is advisable to take hormone replacement drugs after laparoscopic extirpation, which stop the development of atherosclerosis and osteoporosis. Often, during hysterectomy, the ovaries are removed, so women are advised to follow a special diet. It must be rational and balanced.
Laparoscopic extirpation is performed with excision of the mucous membrane of the cervical canal.
For these purposes, surgeons use a special uterine resector. During the operation, doctors insert 4 trocars into the abdominal cavity. Laparoscopic extirpation will help cope with polyposis, recurrent and atypical hyperplasia, external endometriosis, malignant lesions of the endometrium and pathological formations on the cervix.
https://youtu.be/GriA2JZKqKU
One of the most popular minimally invasive operations is the removal (extirpation) of the uterus using the laparoscopic method. But not all patients realize that with the help of laparoscopy it is possible not only to examine, but also to remove the uterus.
What is hysterectomy
In gynecology, such surgical intervention is prescribed to save a woman’s life when serious diagnoses are made. Before making a decision, doctors weigh the pros and cons. Hysterectomy with appendages is an operation to remove the uterus along with the cervix, fallopian tubes and ovaries. After it, a hormonal imbalance occurs, the woman is deprived of childbearing function. She receives psychological trauma, which she cannot always cope with.
Indications for removal of the uterus and appendages
Gynecologists, when prescribing an operation, pay close attention to the woman. Removal of the uterus after 50 years, from a psychological point of view, is less traumatic. The woman is past childbearing age. Until menopause has occurred, they try not to remove the ovaries. Operation is necessary when its cost is life. The indications are:
- prolonged uterine bleeding;
- cancer of the female genital organs;
- endometriosis;
- large uterine fibroids;
- uterine injuries;
- prolapse, loss of genitalia;
- active growth of fibroids during menopause.
Preparing for uterine amputation surgery
It all starts with collecting tests and examinations. When planning to remove the ovaries and uterus, they do:
- general tests;
- checking blood for the presence of venous diseases;
- colonoscopy – examination of the cervix and vaginal walls for the presence of tumors and cysts;
- biopsy and smear taken;
- cytological and biopsy examination of tissues;
- examinations to rule out inflammation in the body.
After it becomes clear that the woman is ready for extirpation of the uterus and appendages, the following procedures are performed:
- prepare donor blood;
- give an enema to cleanse the intestines;
- install a catheter to remove urine;
- consult a vascular surgeon;
- if there is a likelihood of blood clots forming in the veins of the lower extremities, apply a tight bandage with an elastic bandage;
- give medications.
How is hysterectomy performed and how long does it last?
Surgery is performed using full anesthesia. The process is complex and takes several hours to complete. Depending on the volume of intervention, they differ:
- extirpation - removal of the uterus and cervix;
- supravaginal amputation of the uterus - removal without the cervix;
- panhysterectomy – removal of the uterus and appendages;
- extended operation of extirpation of the uterus with appendages - lymph nodes and pelvic tissue are additionally removed.
Depending on the complexity of the situation and diagnosis, the operation is performed in various ways. There are different types of surgical intervention:
- Laparoscopic extirpation. It is performed for small fibroids. Removal of the uterus using the laparoscopic method is carried out using special equipment. Several holes are made in the abdominal wall through which instruments are inserted. Laparoscopy allows for quick recovery after surgery.
- Vaginal hysterectomy is performed externally, through the vagina.
- Laparotomy - abdominal surgery - is performed in difficult cases. The cause may be a large fibroid or a cancerous tumor. It is indicated in situations where it is necessary to remove not only the uterus, adnexal organs, but also lymph nodes. The operation is performed through an incision in the anterior abdominal wall. This gives you a complete overview of the organs. This is important for cancer symptoms to find out the area affected. Look at the photo to see how the female reproductive organs are located.
Consequences
The operation of removing the uterus leads to hormonal imbalance in the body. Young women are especially sensitive to it, because menopause occurs abruptly.
What is a laparoscopic hysterectomy?
Laparoscopic hysterectomy is the removal of the main female organ (uterus) using a laparoscope.
According to practicing surgeons, this method of removal is the most gentle and has a minority of complications. Why choose this particular method for such a complex operation?
- Laparoscopy has minimal invasive consequences;
- The operation is almost painless;
- Does not entail adhesive processes;
- It leaves almost no scars on the patient’s abdomen (a huge plus, considering the aesthetic aspect);
- During laparoscopy, it is possible not to remove important organs along with the uterus, such as the cervix, for example;
- A short rehabilitation period is a definite plus, because after a laparoscopic hysterectomy, a woman, after a few hours, can already walk, be discharged from the hospital after 4 days, and return to her normal life within two weeks;
- Minimal risk of complications after surgery;
- Quick return to sexual life, namely, after 4 weeks.