Injuries to the soft tissues of the birth canal, unfortunately, occur as a result of the pathological course of labor or due to untimely or unqualified obstetric care. The main reasons that cause injury to the soft tissues of the birth canal include: rapid and rapid labor, delivery of a large fetus, delayed labor, prolonged labor, narrow pelvis, incorrect insertion of the fetal head, breech presentation of the fetus, application of obstetric forceps. An unfavorable background for the occurrence of injuries is rigidity, inflammatory or scar tissue changes.
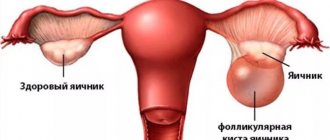
Ruptures of the vulva and vaginal walls
Vulvar ruptures most often occur in the area of the labia minora and clitoris, which is accompanied by bleeding, which in some cases becomes quite significant. Ruptures of the vaginal walls, depending on their location, have their own characteristics. Thus, when localized in the lower third, vaginal ruptures are often combined with a perineal rupture. In the case of a rupture in the upper third, vaginal ruptures extend to the fornix and are combined with cervical ruptures. The clinical manifestations of vaginal ruptures during childbirth are, first of all, bleeding. Both tears in the vulva and vaginal walls are repaired by suturing the wound under anesthesia.
In some cases, when a submucosal tissue rupture occurs, a hematoma forms in the corresponding place. A prerequisite for the development of hematoma formation may be a violation of the structure of the vascular wall due to varicose veins of the genitals, a decrease in the level of vitamin C in the body, hypertension, chronic glomerulonephritis, and gestosis. More often, a hematoma forms on the left, which is associated with the asymmetry of the development of the venous system and the typical location of the fetus. The size of hematomas may vary. The most characteristic symptoms are: pain and a feeling of pressure at the site of localization. Externally, the hematoma looks like a bluish tumor-like formation that protrudes into the vaginal lumen or outward. If the hematoma is small and does not increase, then treatment can be conservative. If the hematoma rapidly increases in size with signs of blood loss, emergency surgical treatment is performed under general anesthesia, and consists of the following stages: incision of tissue above the hematoma, removal of blood clots, ligation of bleeding vessels, closure and drainage of the hematoma cavity.
https://youtu.be/siV7rIu5ALU
Treatment
Treatment of perineal ruptures includes surgery - suturing the damage.
During the operation, local or general anesthesia is used and stitches are applied. If a silk thread is used, it must be removed after 5 days. The doctor can apply catgut threads, which dissolve on their own (do not require removal). In the following days, the suturing site is treated with antiseptics, and the woman in labor is under the supervision of a doctor. It is strictly forbidden to sit on a chair for the first few days, depending on the severity.
In case of ruptures of the vaginal walls, sutures are also applied, but exclusively with catgut. If the uterus ruptures, obstetricians prescribe a rapid caesarean section, after which treatment is directed towards stopping the bleeding and applying stitches. If the cervix is damaged, the abdominal cavity is opened and the ruptures are sutured.
Rules of conduct after suturing
To reduce the risk of complications and unpleasant consequences, a woman must follow all the doctor’s instructions and recommendations. General rules:
- It is forbidden to sit down fully for the time specified by the doctor. This can be either 5 days or three weeks. Otherwise, the seams may come apart.
- You should not wear tight underwear made of synthetic fabrics. Preference should be given to cotton underwear.
- Special gaskets must be used. They are called postpartum. They can be replaced with pads made of natural fabric. This will avoid infection.
- It is important to carry out hygiene procedures after defecation and urination.
- It is advisable to wash the perineum with hygienic gels.
- You can't have sexual intercourse for a while.
- It is not recommended to push.
Complications
After suturing ruptures, the following unpleasant consequences and complications may occur: swelling of the genital organs, hematomas and pain, discharge of purulent fluid from the sutures, inflammatory processes, impaired urination. As well as loss of sensitivity in the area of suturing, suture dehiscence, fecal and gas incontinence, tissue scarring, prolapse of the vagina or uterus, prolapse of the uterus and vagina.
Prevention
Preventive measures are necessary for every woman in labor. They allow you to avoid labor ruptures, so during pregnancy it is necessary to carry out the following activities:
- Visit the gynecologist regularly (exactly as many times as the doctor prescribes).
- Register for pregnancy in a timely manner. The maximum period is 12 weeks.
- You need to train the muscles of the perineum. The exercises consist of alternately contracting and relaxing the pelvic muscles. You can take the Kegel training complex as an example.
- After 7 months of pregnancy, you need to do a special massage in the perineal area.
- If there are any diseases of the reproductive system, it is necessary to carry out timely treatment.
- Be sure to follow all the obstetrician's recommendations during labor.
- Breathe correctly during labor.
Sex after breakups
Many women who have experienced a rupture of the perineum or vaginal walls are interested in whether it is possible to have sex and from when. It is possible, but it is permissible to do it only when the doctor allows it. The period of abstinence depends on the severity of the injury and the course of the rehabilitation period. One woman may be allowed to be sexually active after a couple of weeks, and another after 2 months.
Perineal rupture
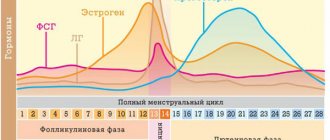
Perineal rupture is one of the most common injuries of the birth canal, and is more common in primigravidas. The main causes of perineal rupture are: violations of its anatomical and functional state, high perineum, inflexibility of tissues and poor extensibility, scar changes after trauma in previous births and after plastic surgery, swelling of the perineum, narrow pelvis, complications during childbirth (rapid and rapid labor , operative delivery, incorrect implementation of obstetric care during the removal of the fetal head and shoulders). The presenting part of the fetus, which moves along the birth canal, reaching the pelvic floor, leads to stretching of the perineal tissue. Rupture of the perineum occurs when the head erupts, less often when the shoulders of the fetus are removed. As a result of compression of the venous vessels by the presenting part of the fetus, the outflow of blood from the tissues of the perineum is disrupted, cyanosis of the skin of the perineum and its swelling appear. Due to a pronounced disturbance of metabolic processes, the strength of tissues decreases and their rupture occurs.
There are spontaneous and forced ruptures that occur due to a violation of the technique of performing vaginal delivery operations or due to improper provision of manual assistance. According to the severity of the ruptures and the depth of the resulting wound, perineal ruptures are divided into three degrees.
- I degree - rupture of the skin of the perineum over a small area of the posterior commissure and the lower third of the vagina.
- II degree - along with rupture of the listed formations, rupture of the pelvic floor muscles also occurs.
- III degree - a deeper rupture, which also involves the muscle sphincter (sphincter) of the anus, and in some cases, part of the anterior wall of the rectum.
A rare type of injury is a central perineal rupture, when the posterior wall of the vagina, pelvic floor muscles and perineal skin are ruptured, but the posterior commissure and anal sphincter remain intact, and childbirth occurs through this formed canal. Perineal rupture is accompanied, first of all, by bleeding and is detected during examination of the birth canal. If there is a suspicion of a third degree perineal rupture, then to clarify the diagnosis you should insert a finger into the rectum. If the integrity of the sphincter is not broken, then it creates resistance when a finger is inserted into the rectum. A rupture of the intestinal wall is easily determined by the specific appearance of the inverted intestinal mucosa. The integrity of the perineum is restored by layer-by-layer sutures on the wound, taking into account all anatomical relationships, under general anesthesia, in compliance with all the rules of asepsis and antiseptics. Due to a rupture of the perineum, especially with ineffective restoration of its integrity, complications such as inflammation of the vagina and cervix, prolapse and prolapse of the uterus, incontinence of gases and feces (with a 3rd degree rupture), and sexual dysfunction are possible.
Vaginal lacerations
The cause of such ruptures is premature pushing or the child’s head remaining in one place for a long time. In this case, this pathology of childbirth can manifest itself as bleeding during the birth process or be detected during examination of the birth canal in the form of hemorrhage under the vaginal mucosa.
Vaginal tears are sutured using absorbable sutures. Usually there are no serious consequences for ruptures of this type. Only in rare cases is it possible to develop an inflammatory process in the scar area. If the uterine cavity connects with the cavity of the bladder or rectum, the formation of a vaginal-vesical or vaginal-intestinal fistula occurs. This is a rather complex pathology, which, fortunately, occurs very rarely.
Cervical ruptures
Cervical ruptures most often occur in the direction from the external to the internal os. There are three degrees of cervical rupture.
- I degree - rupture of cervical tissue on one or both sides with a length of no more than 2 cm.
- II degree - rupture(s) more than 2 cm deep, but not reaching the vaginal vault by 1 cm.
- III degree - transition of the cervical rupture to the area of its lower segment.
The main symptom of cervical rupture is bleeding of varying intensity depending on the extent of the damage. Lacerations are detected during examination of the cervix after childbirth, in the first 2 hours. The integrity of the cervix is restored by suturing the wound. If a third degree cervical rupture is detected, it is necessary to perform a manual examination of the uterus to exclude rupture of its lower segment.
Causes of rupture of the perineum and vagina
- Inelastic tissue of the vulva (external genitalia) and vagina, especially in first-time mothers, high perineum.
- Thrush and other diseases, for example: HPV (human papillomavirus) can cause perineal rupture.
- When the baby's head erupts large, or the head size is very large, then vaginal rupture is likely.
- The cause of the rupture may be the application of forceps.
- With a narrow pelvis, ruptures of the perineum and vagina often occur.
- Incorrect management of childbirth.
Prevention of ruptures during childbirth
Prevention of ruptures of the soft tissues of the birth canal consists of: rational management of labor, the use of antispasmodics, the use of adequate step-by-step anesthesia; prevention of premature attempts, timely diagnosis of complicated labor, qualified performance of vaginal delivery operations. The correct management of childbirth during the period of exile deserves special attention.
In order to prevent damaging rupture of the soft tissues of the birth canal, and for a more gentle delivery, a dissection of the perineum is performed. This method is justified by the fact that an incised wound heals better than a lacerated one; the dissection of the perineum is carried out in a safer place away from the rectum and in a minimal volume. In this case, the integrity of the perineum is restored more easily and without complications.
Makarov Igor, Article provided by medical
Causes
The most common reasons include the following:
- Large fruit: weight more than 4 kg. The large size of the fetal head puts significant pressure on the tissues of the birth canal.
- Post-term fetus. In this case, the child’s skeletal system is already strengthened, which is why at birth the head cannot adapt to the shape of the mother’s canal, because the cranial bones no longer become so mobile relative to each other.
- Rapid labor activity. The intensity of labor does not allow the tissues of the birth canal to adapt to the pressure exerted.
- Excessively long labor. In such cases, the fetal head usually stops in one place, forming congestion (blood circulation is impaired). This factor also leads to tissue damage.
- Incorrect position of the fetal head during childbirth. For the baby to emerge normally, his head should be positioned so that the smallest side of the skull enters the birth canal. If the position is incorrect, initially there is a large circle, but it does not correspond to the dimensions of the channel.
- Scarring of tissue. This happens after significant ruptures during the first birth and surgical intervention. Most often, this provokes scarring of the tissue and its replacement with connective tissue, which does not have elastic properties.
- Inflammatory diseases of the genital organs lead to thinning of tissues, looseness and loss of elasticity.
- Early attempts. According to the law of nature, pushing should begin only after the cervix is dilated. If attempts are made prematurely, then the head descends into the canal and remains there until the uterus opens, exerting negative pressure on the tissue.
- Infection of the genital organs.
- Incorrect actions on the part of the woman in labor (therefore, you must strictly follow all the recommendations of the obstetrician).
- Age after 40 years. During this period, a woman begins to experience age-related changes, and therefore, muscle tone and tissue elasticity are lost.
- Anatomical features of the structure of the reproductive system: flat-rachitic or infantile narrow pelvis.
- Incorrect actions of medical personnel using forceps and other instruments.
Recommendations
First.
Any suture is a gateway for infection, so after childbirth complicated by ruptures, intimate hygiene must be carefully observed. To prevent the stitches from coming apart, it is recommended not to sit for 3-4 weeks and feed the baby only while lying down.
Second.
Do not lift heavy bags or other things. It is advisable to observe sexual rest for at least 2-3 months after stitching the tears.
Third.
Douching, using alkaline soap for intimate hygiene, and swimming in a bathtub or pond are prohibited. It is advisable not to wear synthetic underwear or use vaginal tampons. Since the level of immunity is temporarily reduced, it is important to avoid hypothermia and contact with sick viral infections.
Fourth.
To avoid straining during bowel movements, you should prevent constipation: eat cereal porridge, boiled, stewed and fresh vegetables and fruits, and fermented milk products. You cannot drink whole milk or eat sweets or baked goods.
10-14 days after discharge from the hospital, it is advisable to visit a gynecologist for a thorough examination. If there is pain or intense discharge, it is important to immediately seek medical help.
https://youtu.be/KZhhZb54BSI
Is it possible to avoid perineal rupture?
In order to avoid rupture of the perineum and vagina you need:
- Increase the elasticity of the female genital organs. This is done through exercise, Kegel exercises, a balanced diet and swimming. It is better to start before planning a pregnancy, and not before giving birth.
- Cure all diseases of the genital tract that can contribute to rupture of the perineum and vagina. If there are already scars and previous stitches, then the chances of avoiding ruptures are small.
- And the most important thing is to choose a good doctor; not all doctors have a large number of torn women in labor. A professional who knows his job, if necessary, will lubricate the vagina with a special gel, straighten the fold, etc. But the doctor is not a magician, if there are signs of a threat of rupture, the doctor will make an episiotomy (perineal incision).
How does a doctor see a possible rupture of the vagina and perineum? The rupture does not occur suddenly; there are signs of an impending rupture: the perineum protrudes like a dome and becomes swollen. Then the skin turns pale, becomes shiny, and small cracks appear. In this case, you need to make an incision because the smooth edges of an incised wound heal faster and easier than a lacerated wound.
Why can cervical rupture occur during childbirth?
It is believed that with age, the natural elasticity of tissues decreases. Thus, after 30 years, a woman experiences the first stages of tissue aging: potentially, she is no longer as ready for a healthy birth as at a younger age. These are only average data, but they cannot be ignored.
Possible causes of a ruptured cervix:
- Insufficient elasticity of cervical tissue due to abortion;
- Scars on the cervix left after a previous birth;
- Large child;
- Breech presentation of the baby;
- Narrow pelvis of a woman in labor;
- Long labor;
- Rigidity (poor uterine distension);
- Early rupture of amniotic fluid.
Of course, professional errors by doctors cannot be ruled out. But all the same, these will be spontaneous forms of cervical rupture. And there are also violent forms. These include the use by doctors of tools for emergency fetal extraction - these are either obstetric forceps or vacuum extraction of the fetus. Naturally, when several causes occur during one birth, the risk of rupture increases.
Apgar scale: 5 criteria for assessing a child