A liver rupture is a serious injury that requires emergency medical attention. After damage to this important organ, shock and profuse hemorrhage occur. Therefore, the victim needs urgent hospitalization.
According to medical statistics, closed-type injuries are diagnosed more often than open ones. The likelihood of liver rupture exists in all patients, regardless of age and gender. The prognosis for injury depends on the degree of damage to the gland and nearby organs. In addition, there is a high risk of complications after injury or in the postoperative period.
Description of injury
Damage in which the integrity of the Glissonian capsule (the outer shell of the gland) and the structure of the organ is disrupted is called liver rupture. Common signs of such injuries include disconnection and separation of liver sections with the formation of a slit-like space.
Men are more likely to suffer from liver rupture than women
This is an emergency condition that is caused by trauma to the abdominal space, closed or open. After an injury, massive bleeding almost always occurs, and there is a sharp, intense pain on the right under the ribs and below. Complications of injury include peritonitis, biliary fistula, gland sequestration (tissue death after unsuccessful surgery), etc.
According to medical statistics, gland damage is diagnosed in 25% of cases of all abdominal injuries. At the same time, closed type ruptures are detected 5 times more often than open ones. Gland rupture as an independent disease is rarely recorded (about 8% of cases); in 92% of cases, the organ is damaged as a result of other pathologies. Trauma can occur due to a rupture of the spleen, intestines, kidney bruise, bone fracture, concussion, etc.
In 56% of cases, damage to the right lobe of the liver occurs, in 16% there is a rupture of the left lobe of the organ, in 10% the gate of the gland is damaged, and in 7% the ligamentous apparatus is damaged.
Reference. As a rule, men more often suffer from gland rupture, and in most cases these are open wounds. Closed-type injuries are more often recorded in women after an accident.
With open ruptures, the integrity of the abdomen is compromised, but with closed ones, it is not.
Attention. The fatality rate is 10.6%. As a rule, victims die due to excessive bleeding, bleeding disorders, or shock after surgery.
Forecast
The prognosis for liver rupture depends on a number of factors, among which the most significant are the severity of the injury, the general physical condition of the patient and age. Due to the physiological characteristics of the body, newborns and infants, as well as elderly people, are difficult to tolerate even minor liver injuries. An unfavorable prognosis exists with extensive damage and crushing of the organ, and untimely first aid - up to 60% of patients die from blood loss and pain shock.
An unfavorable outcome is possible with surgical intervention and in the long term. Death during and after surgery occurs from bleeding due to loose sutures or from sepsis or peritonitis. Negative consequences may not occur if the operation is performed on time by a qualified surgeon, and postoperative care is provided with high quality.
If a victim with a liver rupture received modern medical care, and the organ is damaged no more than 60%, the prognosis is favorable. The liver recovers over time, which takes from 2 months to 2 years.
Causes
There are 3 types of liver rupture: closed, open, combined.
Causes of gland injury:
- Hit.
- Falling from height.
- Road traffic accident.
- Compression of the torso on both sides by massive objects.
An open type rupture occurs after a violation of the integrity of the anterior abdominal wall with a cold weapon.
Most often, the organ is damaged due to an accident, and direct damage is observed. Due to a blow to the right hypochondrium or a bruise of the gland, the integrity of the lower surface is disrupted, and, a little less often, the lower and upper surfaces.
When the body is compressed (especially the chest and abdomen) during various disasters (destruction of buildings, tree collapse, etc.), the upper surface is more often injured, less often the lower one. Sometimes extensive destruction of gland tissue occurs with separation of its parenchyma.
Rupture of the liver tissue according to the principle of impact occurs after a fall from a height. In this case, the anterosuperior surface of the organ is more often affected, less often the organ is completely or partially torn off from the ligaments. Sometimes, after a fall, ribs are broken, then the end of the damaged bone further injures the liver.
Attention. Open type ruptures provoke gunshot wounds or damage to the integrity of the abdomen on the right under the ribs with a cold weapon.
Combined ruptures combine open and closed liver injuries.
There is a high probability of damage to the gland during minor physical activity (sports training, childbirth, etc.) in patients who suffer from amyloidosis (deposition of a specific protein-carbohydrate complex in hepatocytes), polycystic disease (multiple cysts), hepatitis, alcoholism and parasitic liver diseases (echinococcosis or alveococcosis). Against the background of morphological changes, the resistance of the gland decreases. Then even minimal trauma can provoke its rupture.
Precapsular rupture of the liver and spleen occurs due to closed-type abdominal trauma. Then hematomas form inside the organ.
In the presence of liver hemangioma (a vascular cavity filled with blood), the likelihood of rupture of the gland also increases. The nature of the formation is still unknown (except for parasitic cysts); they are usually discovered during random diagnosis. The hemangioma grows, over time it can reach the size of 1 lobe of the organ. The neoplasm compresses the surrounding tissue, causing rupture of the gland. When struck or compressed, there is a possibility of rupture of the hemangioma itself, which causes massive hemorrhage and inflammation of the peritoneum.
Important. In some cases, spontaneous rupture of the organ occurs.
There are known cases of spontaneous injury in pregnant women, especially with gestosis (a serious complication of late pregnancy). This likelihood increases in the third trimester of pregnancy, during or after childbirth.
In children or elderly patients, the resistance of the gland tissue is low, so the risk of severe damage is high. There are known cases where the liver ruptured in newborns during the pathological course of labor or during CPR (cardiopulmonary resuscitation).
Closed damage (cracks and crush marks)
Closed injuries occur less frequently than open ones, and the location of the injury and the risk of mortality depend on the blow to the liver itself:
- a direct blow to the liver - the lower surface of the organ, and the upper is often barely touched;
- shock resistance and compression - mainly the upper surface;
- a fall—severation of the liver and damage to the ligamentous apparatus.
Liver Delivered to hospital Died within a few hours Died immediately
| breast organs and skeleton | 15% | 9% | 76% |
| pelvis and limbs | 15% | 14% | 71% |
| spine and head | 14% | 4% | 82% |
| abdominal organs | 20% | 21% | 59% |
https://youtu.be/ksnheMrHQ8g
Classification of hepatic ruptures
Depending on the depth of the lesion, liver injuries are divided into the following types: superficial (the rupture occurs as a result of a minor bruise), deep, through (most often appear after an accident).
There are different types of injuries during which cracks form on the liver
Damage can be caused by various injuries, which have many development options:
- Trauma due to stretching of gland tissue. The reasons are the bending of the organ or the separation of its sections that are adjacent to the ligamentous apparatus. After damage, the liver bends and its edges become jagged.
- Damage due to compression of the torso. The slot gap is placed at an angle, the edges are uneven, and there are crush marks. Injury occurs due to intense compression of the gland towards the spine or kidneys.
- Blunt organ trauma (impact with a blunt object). There are crushed areas and there is a risk of detachment of the outer shell. The depth of the wound reaches 6 cm.
- Liver puncture injury. The injury occurs after a rib fracture that ruptures the gland. In appearance, it is a deep wound that has smooth edges.
- Damage to the gland due to displacement of its anterior edge and sprain of the round ligament. A rupture occurs after a strong blow to the stomach, an accident, or resuscitation measures.
With central ruptures of the organ, hematomas are formed. They occur as a result of a fall from a height or strong compression of the torso. After injury, the tissue of the gland is stretched, and its surfaces move in opposite directions.
Depending on the area of damage, ruptures are divided into the following:
- Subcapsular, in which hematomas are formed.
- Capsular (formation of cracks in the upper tissues).
- Injuries during which the gallbladder and its ducts are damaged.
There are several classifications of gland trauma according to severity, one of them will be presented below:
| Degree | Gap | Points |
| I | Under the capsule:
| 2 |
| II | On the organ:
| 2 |
| III |
| 3 |
| IV | Destruction of the hepatic lobe is observed (from 20 to 25%), and there is heavy bleeding. | 4 |
| V | The degree of destruction of the hepatic lobe reaches 50%. | 5 |
| VI | Both lobes of the organ are destroyed. | 6 |
The level of danger for each type of rupture depends on the severity of the injury and is assessed in points.
At grade 1, the integrity of the capsule is not compromised:
- minor bleeding into the liver tissue – 0 points;
- limited accumulation of blood under the membrane, the diameter of which is about 3 cm - 2 points;
- capsule detachment, hemorrhage – 4 points;
- central gap less than 2 cm – 6 points;
- central damage of 2 cm or more – 8 points.
At grade 2, the outer shell is damaged:
How does a person’s liver hurt (symptoms)
- the integrity of the liver tissue is not compromised – 1 point;
- wound depth up to 2 cm – 4 points;
- crack depth from 2 cm – 8 points;
- through wound – 10 points;
- damaged area of the gallbladder (GB), extrahepatic bile ducts – 4 points;
- injury to gland tissue, gallbladder, its ducts – 4 points;
- extensive destruction of organ tissue with loss of viability – 14 points.
In grade 3, the integrity of the gland ligaments is compromised:
- Limited accumulations of blood in the ligaments – 0.5 points each;
- sprain – 1 point;
- ligament separation – 2 points;
- separation of the gland from the ligaments – 14 points.
In grade 4, organ vessels rupture:
- separation of the inferior vena cava – 11 points;
- portal vein avulsion – 11 points;
- separation of the venous vessels of the gland – 11 points;
- the celiac trunk and its branches are torn – 11 points.
Reference. Thus, degree 1 is considered mild, degree 2 - moderate, degree 3 - severe, degree 4 - extremely severe, degree 5 - incompatible with life.
Types of damage to the driver and passenger
An accident can cause injury to any part of the body or several at once. You can distinguish the type of damage visually, but only a specialist can characterize it more accurately after an examination. However, an eyewitness to the incident is able to recognize the type of injury in order to help the victim.
Cranial
The head often suffers in road accidents. After all, when a car suddenly stops, a person leans forward sharply and can be injured on the glass or steering wheel. The head is not secured by anything, so it hits a hard surface, resulting in a traumatic brain injury. It can also be caused by a late deployed airbag.
Passengers sitting in the rear seats receive a concussion or brain injury from impact with the front seats. If the collision is sideways, the head hits the car pillar or door. A traumatic brain injury can be recognized by a wound on the forehead or crown, the back of the head, or a broken face. If it is severe, fluid may leak from the ears, nose, and a visible fracture of the skull bones. A cracked car window indicates a head impact.
The most severe traumatic brain injuries occur in those who are not wearing a seat belt. Another factor in receiving such damage is the high speed of the car, its fall from a great height.
Spine and ribs
Stopping the car abruptly can lead to a dislocation or fracture of the spine. The cervical region is especially often affected. The head sharply tilts down, then it is immediately thrown back, which causes injury. Those who sit with a bent back and a poorly adjusted headrest are at greater risk.
The spine also suffers when a person is not wearing a seat belt. Sharp jerks of the body lead to deformation of ligaments and impacts. The rear passenger may be injured. He is thrown forward with tremendous force. And the blow falls precisely on the back of the person in front.
Injuries to the neck and spine are indicated by increased pain when trying to change the position of the body, turn the head, or move the arms. Sometimes deformation is noticeable. The localization of sensations depends on which part of the spine is injured.
https://www.youtube.com/watch?v=_hi926Vf3Kk
Fractures and bruises of the ribs are caused by contact with the steering wheel. The part can press them inward, resulting in deformation of the bones. Dangerous for ribs and belt. He holds the body in place, and it rushes forward. The consequence is sudden compression and tissue damage.
Symptoms
Some gland injuries are not accompanied by severe symptoms. The first signs appear when the patient's condition worsens due to light physical activity. This is because the injury worsens and the subcapsular hematomas rupture, causing bleeding.
Intense pain in the right hypochondrium, which intensifies during movement, indicates liver injury
You can detect that the liver is ruptured by the following signs:
- increased heart rate and pulse;
- sometimes the heartbeat slows down due to the accumulation of bile;
- breathing depth is below normal;
- nausea, vomiting.
Attention! Intense pain in the right hypochondrium, which intensifies during movement, is a clear sign of liver problems.
- paleness of the skin and visible internal membranes;
- cold sweat;
- severe decrease in pressure;
- vertigo (dizzy).
Due to excess intestinal gas formation and blood accumulation, the abdominal circumference increases and the tone of the abdominal wall muscles increases. Although the latter symptoms may be absent. The victim lacks clarity and clarity of thought, which increases the likelihood of coma. The child experiences the same symptoms as adult patients.
Structure of the liver
Before proceeding to the characteristics of liver damage, it is worth saying a few words about the structure of this organ.
What is the liver, where is it located and how does this organ hurt? The liver is located in the upper part of the peritoneum, occupying the right hypochondrium. The weight of an adult’s liver reaches an average of one and a half kilograms. The organ has two surfaces: the upper, located directly under the diaphragm, and the lower. The liver consists of two lobes: right and left. The lobes are separated from each other by the falciform ligament. Adjacent to the liver is the gallbladder, which is a reservoir for the bile secreted by the organ.
Diagnostic measures
After a visual examination, the victim is prescribed laboratory tests. A clinical blood test will show a decrease in the concentration of red blood cells, hemoglobin, and an increase in the level of reticulocytes. The number of leukocytes and platelets in the blood decreases significantly.
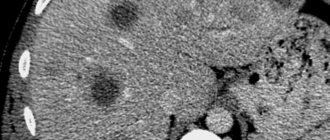
CT scan of the liver allows you to assess the severity of the rupture, the nature of the damage and the volume of blood in the abdominal space
When the gland ruptures, the acidity of the urine changes, then its reaction becomes alkaline or neutral. The number of squamous epithelial cells in urine increases.
Blood biochemistry demonstrates the following pathological changes:
- the amount of total protein decreases;
- albumin concentration decreases;
- glucose levels decrease;
- the amount of bilirubin (bile pigment) increases;
- the concentration of liver enzymes (ALT, AST, alkaline phosphatase) increases.
The coagulogram shows a decrease in the prothrombin index, platelet adhesion (gluing), and an increase in the duration of the APTT (active partial thromboplastin time).
X-rays can reveal fluid in the abdominal space and injury to the gland. CT and MRI are considered more informative, since they can be used to assess the severity of the rupture, the characteristics of the damage, and the volume of blood in the abdominal cavity.
Reference. Laparotomy is the most effective research method, which allows you to visually assess the condition of the gland through small incisions in the abdominal wall. In addition, after diagnosis, treatment can be carried out immediately.
What are the dangers of liver rupture?
Liver ruptures almost always pose a threat to the victim's life. It can be either single or multiple: the intensity of bleeding depends on this factor. It is worth noting that the parenchyma and blood vessels of the liver are not capable of contraction. This causes the development of bleeding, which cannot stop spontaneously.
Blood loss also increases due to the fact that the liver is constantly moving during breathing. In addition, bile is mixed with the blood, which makes it very difficult to clot. In rare cases, bleeding may stop without medical intervention. As a rule, this occurs in cases where large vessels have not been destroyed.
Treatment methods
A person with symptoms of a ruptured gland should be given first aid. First of all, you need to call an ambulance.
Carefully! The victim is prohibited from moving, as the risk of increased hemorrhage increases.
If the dynamics are unstable after liver damage, doctors prescribe laparotomy
A cold compress is applied to the area of the right hypochondrium. In addition, you should pay attention to your heart rate and breathing. It is important to constantly talk to the patient so that he does not lose consciousness.
Upon arrival, emergency doctors apply ice to the damaged area and inject the victim with adrenaline (no more than 1 ml). Painkillers are not recommended, as they can “lubricate” the symptoms.
Typically, the patient is given immediate medical attention. Watchful waiting is appropriate only if hemodynamics (blood movement) are stable and the free blood volume is up to 150 ml. In this case, the gap should be of a blunt, closed nature.
Reference. The victim is prescribed hemostatic drugs: Etamzilat, Vikasol, aminocaproic acid. Infusion treatment allows you to restore and maintain the volume and quality of blood.
If hemodynamic parameters are unstable, doctors prescribe laparotomy. The operation is performed under general anesthesia after intubation (insertion of a tube into the larynx and trachea) and administration of muscle relaxants (drugs that reduce muscle tension). Doctors insert venous catheters through which saline, Ringer-Locke solution, Reopoliglucin, and glucose are injected. Transfusions of platelet concentrates, plasma, and cryoprecipitate (precipitate from fresh frozen blood plasma) are also performed.
Upper midline laparotomy is used if the operation is not urgent or doctors have not yet established an accurate diagnosis. After examining the abdominal organs and establishing the degree of damage, access is expanded. Then the damaged gland tissue and vessels are sutured. If part of the liver needs to be removed, then thoracofrenolaparotomy is prescribed.
To stop bleeding, surgeons find the damaged vessel, grab its ends, fix it with a clip or stitch it. Dead areas are removed using an ultrasonic scalpel. A special fibrin insulator will help to completely stop the bleeding.
When suturing the vessel, a special self-absorbable material is used. A blunt, curved needle is used to apply sutures.
Liver functions
The liver performs a number of important functions. It cleanses the blood, reproduces various proteins necessary for the normal functioning of the body, produces enzymes and takes part in all types of metabolism. During human intrauterine development, the liver performs hematopoietic functions. At the same time, many people know very little about it, for example, where the liver is located and how this organ hurts. This knowledge is very important: if you suspect the presence of any disease in time, treatment will bring much better results.
Possible complications
The consequences of liver rupture occur more often during combined injuries. A few days after the injury, biliary peritonitis may develop. The patient experiences dull pain, bloating, fever, and intestinal paresis. Bile leakage requires surgical intervention.
After severe tissue damage, biliary fistulas develop. The reason for this is necrosis and suppuration. They can be internal or external, often accompanied by abscesses in the liver cavity or under the diaphragm.
After a bruise or surgery, tissue around the edges of the wound may die. Liver infarction occurs with extensive necrosis. The patient's intoxication increases, bile leakage appears, and re-bleeding occurs. Small areas are replaced by connective tissue or suppurate. The consequences of a shock and rupture of the liver can be:
- Subphrenic abscess. It develops when fluid accumulations become infected and the edges of the wound become suppurated. Manifested by prolonged fever and weakness.
- Hematoma infection. The patient experiences aching pain on the right side, sweating, drowsiness, chills, and fever. When the abscess ruptures and the contents spill into the abdominal cavity, peritonitis develops.
- Secondary bleeding after surgery.
- Pseudocysts with a volume of up to 3 liters. They tend to necrosis of the contents, destruction of blood vessels and bile ducts.
- Air and tissue embolism due to damage to blood vessels.
- Inflammation of the liver as a result of ischemia, dystrophy and necrosis of the parenchyma.
- Hepatorenal syndrome with severe lesions with massive blood loss, death of hepatocytes, and intoxication. The patient develops jaundice, difficulty urinating until complete cessation (anuria), and coma.
- Biphasic rupture of the liver due to capsule detachment.
How is liver rupture diagnosed?
Diagnosing a liver rupture can be difficult, especially if the patient has suffered other injuries. If liver rupture is not diagnosed in time, the consequences can be very serious. Fortunately, thanks to modern diagnostic methods, errors are reduced to a minimum.
Recently, abdominal puncture with the introduction of a special catheter has been used to diagnose liver ruptures. Thanks to this method, it is possible to quickly identify the specifics of the injury and carry out the necessary therapeutic measures. Some patients are advised to undergo a liver ultrasound to make a correct diagnosis.
A blood test helps determine the intensity of changes caused by blood loss. The number of red blood cells begins to decrease a couple of hours after the rupture occurs, and acute anemia subsequently develops. The rate of decrease in the number of red blood cells allows you to determine the intensity of internal bleeding. Blood tests should be carried out every few hours, which allows you to monitor the dynamics of the patient's condition.
Diagnosis of subcapsular hemorrhages is quite difficult: with such lesions, the first few days the patient’s condition is satisfactory, after which it sharply worsens.
The patient's alcohol intoxication or unconsciousness caused by a traumatic brain injury can make diagnosis difficult.
Recommendations
- For 2-7 days after surgical treatment, it is recommended to remain in bed with therapeutic exercises .
- a special diet for a long time, limiting fried, spicy, and fatty foods. It is better to eat boiled or steamed food. Food must contain sufficient amounts of proteins, carbohydrates, animal fats and vitamins.
- It is necessary to completely give up alcoholic beverages and smoking.
- All patients who have suffered traumatic liver injury should be registered with a gastroenterologist and/or surgeon and regularly monitored by these specialists.
- an ultrasound examination of the abdominal organs 2 times a year
Treatment tactics
If there is a suspicion that the victim has a damaged liver, an ambulance should be called at the scene of the incident. It is impossible for a person to get up and move. The patient is taken to the hospital on a stretcher. Cold is applied to the site of the injury. In case of clinical death, indirect cardiac massage is performed until the ambulance arrives.
The patient continues to be treated in the intensive care unit. In case of massive blood loss, anti-shock therapy is carried out before surgery. The goal of treatment at the first aid stage is to correct hemodynamic disorders and functions of vital organs.
- Intravenous administration of blood substitutes (Gelofusin, Refortan), saline solutions, plasma.
- Oxygen inhalation.
- Adrenergic agonists: Dopamine, Norepinephrine.
Rehabilitation period
After surgery, patients are prescribed painkillers and antibiotics. The introduction of colloidal and saline solutions is indicated.
Prevention of complications, constant monitoring of heart function, control of the functions of the urinary organs are carried out. The fluid released through the drains is also monitored. The patient is kept in the intensive care unit until the condition of the cardiovascular and respiratory systems is stabilized.
To accelerate tissue regeneration and improve liver function, hepatoprotectors, vitamin and mineral complexes, and dietary nutrition are indicated. After the patient is discharged, diet No. 5 is recommended, heavy physical activity, alcohol intake and smoking are excluded.
How to be treated
Treatment is usually surgical. Whether this access will be through punctures (laparoscopy) or using incisions (laparotomy) - the doctor decides, based on the severity of the damage. Coagulation of ruptures and wounds is carried out, sutures are applied.
If there are tears or penetrating wounds and the bleeding cannot stop on its own, then in these cases drainage is installed and hemostatic therapy (hemostatic agents) is carried out. In case of major bleeding, the vessels are ligated and the wound is sutured.