Risk factors and main causes
There are several theories that try to explain the origin of the injury. The founder of one of them is Bandl, who associated pathology with mechanical causes. He described the process as overstretching of the lower segment of the uterus, which occurs due to the large size of the fetus and at the same time the narrow pelvis of the woman in labor. But the theory could not explain why injury occurs when a small baby is born.
This theory was supplemented by the research of Ya. F. Verbov, who believed that pathologically altered tissues are necessary for the occurrence of a wall defect. The condition occurs against the background of chronic endometritis, after repeated abortions and curettage, endometriosis or scar changes.
Currently, the causes of uterine rupture have been significantly expanded. It is believed that histological changes in the wall predispose to the formation of a defect, and mechanical or violent actions initiate the process.
Histological causes include the following:
- scars after operations (caesarean section, plastic surgery of congenital anomalies, removal of myomatous node, perforation);
- chronic inflammatory process;
- tight attachment of the placenta;
- dystrophic changes after frequent curettage;
- infantilism and congenital developmental anomalies;
- biochemical changes during prolonged labor.
The defect can form not only at the site of a scar or altered wall, the injury occurs in the area of the rudimentary horn. In this case, the rupture occurs at 16-20 weeks of pregnancy, provided that the fetus is attached in the area of the rudimentary horn. Clinical manifestations of the pathology resemble tubal abortion.
Mechanical causes combine cases that lead to a discrepancy between the size of the fetus and the woman’s pelvis:
- clinically or anatomically narrow pelvis;
- hydrocephalus;
- large fruit;
- frontal presentation or posterior view of the face;
- violation of head insertion;
- transverse or oblique position of the fetus;
- myometrial tumors;
- birth canal with cicatricial changes;
- tumors or bone deformities in the pelvis.
The appearance of complications is sometimes provoked by violent actions, which are the result of incorrect use of surgical or obstetric manipulations:
- application of obstetric forceps;
- vacuum extraction of the fetus;
- Kristeller's maneuver;
- extraction of the fetus by the pelvic end;
- internal rotation;
- removal of the head of Morisseau-Levret;
- release of thrown back arms during breech presentation;
- fruit-destroying operations.
Violent causes include accidental injuries that may occur outside of childbirth.
Features of the mechanism
A discoordinated type of labor becomes one of the common causes of complications. The condition develops as a result of labor stimulation, for which there are no indications, or due to individual characteristics of the body (read about the indications and contraindications of labor stimulation at the link). These include imbalance in the autonomic nervous system with a predominance of the influence of the parasympathetic department. Such a rupture occurs during childbirth against the background of increased myometrial tone. When stimulated, contractions become more frequent and do not weaken.
The pressure in the uterus changes abruptly; instead of a gradual divergence of muscle fibers, they sharply stretch. In the presence of pathological changes, a crack forms.
A rupture that occurs primarily due to a mechanical obstruction proceeds through a different mechanism. The fetus cannot move along the birth canal, so the myometrium moves to the bottom, and the lower segment becomes tense. The baby’s head presses the neck against the pelvic bones, causing blood stagnation and swelling. The minimum thickness of the uterine wall with the probability of rupture in this condition is several millimeters. When the tissues can no longer stretch, the following process begins:
- rupture of the walls of blood vessels;
- hematoma formation;
- crack formation;
- in conclusion, incomplete or complete uterine rupture occurs.
The mechanism of forced rupture during childbirth is associated with additional impact on the uterus, which is already in a critical condition. Overstretching of the lower segment in a clinically narrow pelvis and pressure on the uterine fundus will lead to increased tissue tension and the appearance of a defect.
It is generally accepted that healthy myometrium is not susceptible to rupture. If a healthy woman experiences a discrepancy between the size of the fetal head and the birth canal, then labor will normally stop. Pathologically changed tissues after abortion, curettage, inflammation are characterized by the presence of connective tissue and impaired blood supply. Histological changes occur at the cellular level, so they are sometimes impossible to notice during examination.
Such a modified wall is capable of stretching during pregnancy, can withstand contractions during normal childbirth, but is not able to bear additional load.
After any operation on the internal genital organs, which was accompanied by an incision in the wall, some of the muscle cells along the edge of the wound die. At the time of healing, the wound surface is filled with new myocytes and connective tissue, but the structure does not recover. If not enough time has passed after the formation of the scar, and pregnancy has occurred, then the inferiority of its tissue can cause rupture of the uterus along the scar.
Treatment
Therapeutic tactics for scar failure directly depend on whether the patient is pregnant or not.
When a thin and defective suture is detected on a patient’s uterus, it is important to immediately decide whether the patient is planning a pregnancy or not, as well as what the woman will do with an unplanned pregnancy - maintain it or definitely terminate it.
In patients who consciously plan pregnancy or do not object to its occurrence, surgical treatment is clearly necessary. It involves re-entering the abdominal cavity, excising the old scar, and re-suturing the uterus with several rows of strong sutures. In the postoperative period, competent rehabilitation, prevention of inflammation and suppuration of sutures, and planning pregnancy no earlier than a year after the operation are very important.
In patients who clearly object to a new pregnancy, careful selection of reliable contraceptives is necessary, since in this case not only the onset of pregnancy is dangerous, but also its termination. Alternatively, such patients may consider surgical sterilization options. Intrauterine contraceptives - IUDs or "spirals" - are strictly not recommended for this category of women.
During pregnancy
This is the most dangerous option, relating to emergency situations in obstetrics. Unfortunately, if it is determined that the scar on the uterus is incomplete at any stage of pregnancy, its urgent termination is indicated.
Of course, there are no special issues with early pregnancy (6-12 weeks), as well as with an almost full-term or completely full-term pregnancy. In the first case, the pregnancy is terminated as an abortion and the patient is offered uterine plastic surgery, in the second option - an emergency caesarean section.
The situation is worse with very premature pregnancies, when a child born prematurely will obviously have a lot of health problems and dubious chances of survival. Such patients with an incompetent scar without signs of uterine rupture can be managed observationally for quite a long time, of course, in a hospital setting, bed rest and constant combat readiness of the operating team.
Beginning or threatening uterine rupture along the scar is an absolute indication for immediate cesarean section, regardless of the stage of pregnancy. Here you need to save both the mother - from bleeding and blood loss, and the child - from hypoxia and intrauterine death. In the event of a uterine rupture, seconds count; unfortunately, the fetus cannot always be saved.
Options for birth trauma
There are several different options for uterine rupture, which form the basis of different approaches to the classification of the pathological condition. Based on the features of the formation mechanism, the following are distinguished:
- spontaneous - occurs without external influence due to pathological changes in the wall and disturbances in labor;
- violent – during obstetric manipulations and operations.
The clinical course determines the stage:
- threatening;
- beginning;
- accomplished.
The nature of the damage may vary:
- A fissure is a small tear in a section of the uterine wall.
- An incomplete rupture is the appearance of a defect only in the mucous and muscular membranes. The outer serosa remains intact. This type of damage is most often observed on the lateral surfaces of the lower segment or along the rib of the uterus. The injury is accompanied by internal bleeding with the formation of a huge hematoma between the ligaments of the uterus.
- A complete defect is most common. It is characterized by damage to all layers of the wall.
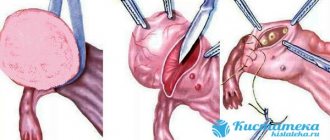
Uterine ruptures: Fig. 1 - along the scar after cesarean section; rice. 2 - incomplete, in the lower segment with the development of a hematoma
Most often, the tear occurs in the lower segment. This area thins the most during childbirth. But another localization is also possible:
- in the uterine day;
- along the side walls;
- in body;
- separation of the uterus from the vaginal vaults.
Uterine rupture is a condition that is associated with the period of gestation. Therefore, the causes of rupture outside of pregnancy cannot be considered from this point of view. Violations of the integrity of the wall in non-pregnant women are often referred to as perforation.
Clinical manifestations of different stages of the process
Signs of uterine rupture are varied and depend on the stage of the process. For clinical manifestations, the mechanism and time at which the injury occurs are important. Sometimes, with pronounced changes in the wall, the symptoms at the initial stage are minimal; gradual spreading of tissue occurs, which is difficult to diagnose.
Threatening
In the presence of an incompetent scar or inflammatory tissue changes, it can occur after 30 weeks of gestation. Myometrial stretch reaches its maximum during this period. The woman experiences the following symptoms:
- radiating pain in the lower abdomen and lower back, which cannot be clearly localized;
- decreased blood pressure;
- scanty bleeding from the genital tract;
- increased uterine tone;
- decrease in fetal vital signs.
During the period of delivery, a threatening rupture manifests itself with other symptoms:
- rapid labor activity;
- hyperextension of the lower segment and change in the shape of the abdomen;
- sharp pain when touching the uterus;
- severe vaginal swelling and swelling of the genitals;
- continuous leakage of amniotic fluid.
Symptoms of birth trauma may be more subdued due to frequent use of painkillers.
Started
The next stage is characterized by all the symptoms listed above, but they can be observed in different combinations and will be more pronounced.
Contractions become severely painful and are sometimes accompanied by convulsions. Sharp abdominal pain in the uterine area persists beyond contractions. The woman's state is excited, her pupils are dilated, and a feeling of fear appears. Bloody discharge from the genital tract is scanty, there may be urinary retention or blood in the urine. The fetal head stops moving along the birth canal, and a noticeable bulge appears above the womb.
The condition of the fetus worsens. He may become overly active. According to CTG data, the heart rate slows down or accelerates, and the sounds become muffled. If assistance is not provided at this stage, fetal death occurs in 80% of cases.
Accomplished
The symptoms of the incident correspond to the clinical signs of massive bleeding. But first there is a sharp pain in the abdomen. A woman may feel as if something has burst inside. The contractions stop abruptly, and the fetus subsides and dies. The shape of the abdomen changes, and parts of the fetal body are felt under the skin. The woman’s condition is serious, signs of bleeding predominate:
- decreased blood pressure;
- pale skin;
- dry mouth;
- weakness, loss of consciousness;
- tachycardia;
- the pulse is difficult to palpate.
Bleeding from the genital tract increases. The uterus takes on an irregular shape and moves upward. The rupture along the scar gives a bulging configuration, and a protrusion appears along the anterior wall. When the rupture is incomplete and a hematoma is formed, it is palpated as a space-occupying formation that is adjacent to the lateral surface.
If the tear occurred during the period of expulsion of the fetus, the child may remain alive and have no signs of oxygen starvation. But immediately after birth, the mother’s condition deteriorates sharply, massive bleeding begins, and signs of hemorrhagic shock appear.
Diagnostic techniques
Even during the gestation period, pregnant women are examined and assigned to a group at risk of labor anomalies. A history of abortion, chronic endometritis, previous cesarean section birth, or surgery increases the chances of injury.
The condition of the scar must be assessed. Vaginal birth after the first cesarean section is not contraindicated, but most often in post-Soviet countries they prefer to perform a second cesarean section.
On the subject: If you had a cesarean section, is it possible to give birth naturally?
Diagnosing a rupture during labor can be difficult. The doctor must urgently assess the deteriorating condition of the mother and fetus and decide on a diagnosis and tactics.
During examination of the birth canal, the following signs are noted:
- enlarged birth tumor on the fetal head;
- lack of head advancement;
- the anterior lip of the neck is pinched and swollen;
- swelling spreads to the vagina and external genitalia.
When viewed externally, the contraction ring is located high and may have an oblique position.
Diagnostics includes measuring blood pressure and pulse. To determine the condition of the fetus, a CTG is recorded.
If a 1st degree uterine rupture occurs during childbirth, there are no diagnostic problems. All signs of massive bleeding appear, the woman’s condition requires emergency help.
Sometimes the diagnosis can be made after childbirth. The woman has bloating. Manual examination of the uterine cavity allows you to identify the defect and take the necessary measures to eliminate bleeding and its consequences. If the condition is not diagnosed in the delivery room, within a day signs of peritonitis appear.
Diagnostics
Uterine rupture is diagnosed based on the collected history and visual examination of the woman. If necessary, an ultrasound examination is prescribed. Most often, an accurate diagnosis needs to be established in a short time, because this pathology develops very quickly and its treatment must be carried out without delay.
In a situation where a doctor makes an incorrect diagnosis based on symptoms, the risk of death for mother and child increases many times.
During the history taking, the doctor asks the following questions:
- the nature of the pain that appears;
- are there any discharges of various types from the vagina;
- sexual diseases that were previously;
- previous surgical interventions;
- the course of previous births.
Read more Dryness after ovulation
Basically, the development of this pathology is easily determined before the onset of the birth process, and for this it is necessary to do an ultrasound examination. The results must be reported to the obstetrician-gynecologist who will deliver the baby.
During a physical examination of a pregnant woman suspected of developing this condition, pay attention to:
- blood pressure indicators;
- heart rate;
- heart rate.
The doctor also conducts:
- palpation of the abdominal cavity;
- gynecological examination to determine the size and muscle tone of the uterus, as well as the presentation of the fetus;
- ultrasound examination, if the above methods fail to make a correct diagnosis (ultrasound will show the thickness of the organ wall, visible violations of integrity, and indicate the stage of the rupture);
- cardiotocography.
It should be noted that pregnancy, if ruptures are detected, must be urgently interrupted by delivery, because any delay threatens the life of the mother and child.
Caring for a woman during pregnancy and childbirth
Women with a threatening rupture are not transportable. This means that if alarming symptoms appear, she cannot be transferred to another clinic, even if assistance cannot be fully provided under the existing conditions. The death of the fetus and the woman in labor may occur during transportation, when it will be impossible to provide assistance.
Clinical recommendations for this complication prohibit active management of labor and require its completion by cesarean section. The woman is given deep anesthesia. If the fetus is still alive, then the operation is performed regardless of the obstetric situation.
Even if the fetal head is in the pelvic cavity, attempts should not be made to remove it without surgery. In this case, the threatening state will turn into an accomplished one.
If the fetus has died, then a cesarean section is not performed; it is replaced by a fetal-destroying operation.
The protocol for uterine rupture that has already occurred involves emergency laparotomy. Delivery is not carried out in this case, since fetal death occurs almost instantly. It is necessary to stop the bleeding and prevent the development of severe hemorrhagic shock and disseminated intravascular coagulation. Therefore, even at the stage of preparation for surgery, transfusions of blood, plasma or other anti-shock solutions begin.
They try to complete the operation as quickly as possible. This requires ligation of the supply vessels and elimination of bleeding. Determine the indications for hysterectomy in case of rupture:
- hemorrhagic shock;
- damage to a large vascular bundle;
- extensive gap.
In case of a linear rupture, the wall defect is sutured. The abdominal cavity is inspected and blood clots are removed. In case of incomplete rupture, it is necessary to eliminate the resulting hematoma, determine the source of bleeding and stop it.
After the operation, infusions of solutions are prescribed to compensate for blood loss, and antibiotics to prevent infectious complications. Thorough pain relief is required.
Women who have lost a child during childbirth may need the help of an experienced psychologist.
Obstetric tactics
Treatment of uterine ruptures is carried out only surgically, regardless of the stage of the pathology, period of birth, or gestational age (failure of the postoperative scar). The woman in labor is administered muscle relaxants, followed by tracheal intubation to stop labor. A caesarean section is then performed.
note
Obstetric tactics about 30 years ago, in the event of a threat of organ rupture and antenatal fetal death, consisted of performing a fetal destruction operation. Today, given the high traumatic nature of embryotomy and overextension of the lower segment, abdominal delivery is indicated (high risk of violent injury to the fetal sac).
Surgery must be performed as quickly as possible. Surgical access – midline laparotomy. The extent of the operation is determined by the woman’s condition, stage and location of the damage. If possible, the uterus is preserved. During the process of transection, the fetus, placenta, and blood clots are removed from the uterus or abdomen. After removing the baby and placenta, the uterine walls are carefully examined, stitching together any damage found. When a rupture occurs, its edges are excised and the wound is sutured. If the wound on the organ is large and crushes the tissue, a hysterectomy is performed. After suturing or removing the uterus, an inspection of the abdominal organs is performed. If possible, autohemotransfusion is performed (transfusion of the patient's own blood after it is removed from the abdominal cavity and filtered).
Before, during and after the operation, measures for anti-shock therapy and replenishment of blood volume are carried out. Prevention and treatment of DIC syndrome and antibiotic therapy are also carried out.
Sozinova Anna Vladimirovna, obstetrician-gynecologist
6, total, today
( 41 votes, average: 4.71 out of 5)
Creams and ointments for diapers, preparations for the treatment of diaper dermatitis
How to choose a stroller for a newborn
Related Posts
Consequences and possibilities of prevention
The consequences of myometrial rupture can be disastrous. This condition, even with the modern level of obstetric care, is accompanied by high rates of fetal death. For a woman who has suffered massive bleeding, a long recovery period is required.
Blood transfusion is always accompanied by the risk of infection with HIV and hepatitis C viruses. But the danger is massive bleeding, which leads to hypoxia of the pituitary gland and the development of Sheehan syndrome. This hormonal disease makes it difficult to get pregnant again.
Prevention is carried out at the stage of pregnancy planning. Women who have undergone surgical procedures need a comprehensive assessment of the condition of the uterine scar, which should include not only ultrasound data, but also hysteroscopy.
Throughout pregnancy, you must follow your doctor's recommendations. If there are a large number of risk factors, delivery is permissible only in level 1-2 institutions, which include regional maternity hospitals and large perinatal centers. Hospitalization should be carried out ahead of schedule.
Preventing rupture
To reduce the risk of scar rupture and other complications, prevention begins at the stage of preconception preparation. In some cases, a woman may be offered uterine scar plastic surgery. This is a surgical operation that is aimed at restoring the integrity of a tissue area and forming a full-fledged scar. It is preferable to use absorbable synthetic threads as a suture material, and suture the incision with separate sutures.
After any operation, it is necessary to avoid infectious complications that can cause unsuccessful formation of connective tissue.
Treatment of uterine scars with traditional methods and medications is ineffective.
To reduce the likelihood of a rupture along the scar of a woman during pregnancy and childbirth, careful monitoring, regular CTG and ultrasound are necessary. During childbirth, monitoring the fetal heartbeat and uterine contractions is also required.