The term "involution" means the "reverse development" of something. Breast involution is not considered a disease.
These are just physiological changes in the glandular tissues of the breast associated with different periods of a woman’s life: pregnancy and lactation, menopause and other hormonal changes in the female body.
This change in structure causes the fat tissue to loosen to fill the empty space. However, the functional tree of the mammary ducts can be reformed when the woman is pregnant again. This review focuses on the development and hormonal responses of mouse and human mammary glands. The main focus of the review is the role of mesenchymal-epithelial interactions in the development of embryonic mammary glands and the role of stromal-epithelial interactions in mammary gland biology. This new model involves the generation of tissue recombinants consisting of human or mouse mammary fibroblasts plus human mammary epithelium in polymerized collagen gels. In the model, mouse mammary fibroblasts and human mammary fibroblasts appear to equally support normal differentiation and growth of the human mammary epithelium. This observation raises the possibility of using murine mammary fibroblasts from various mutant mice to evaluate the role of specific paracrine gene products in the biology and carcinogenesis of the human mammary gland. The mammary gland is a useful model for studying epithelial-stromal interactions because these interactions are important in embryonic development, postnatal ductal growth, ductal branching morphogenesis, and carcinogenesis.
Causes of breast involution
The female body has to go through several natural stages, during which the development of involution of the mammary glands is possible:
- from the beginning of puberty to 45 years of age (reproductive period);
- from 45 to 60 years (menopause);
- from 60 years (period of approaching old age).
The mammary glands react very sensitively to any changes in hormone levels in the female body. Sometimes it may be enough for an experienced doctor to examine a woman’s breasts to make a diagnosis. With stable active hormone levels, involution may not occur even at 50 or 60 years of age. However, if the hormonal level is insufficient, changes in the mammary gland can also develop in young twenty-year-old girls. This phenomenon requires an indispensable examination for gynecological and endocrinological diseases.
The mammary gland is a dynamic organ whose structure changes throughout the female reproductive cycle. The development of the gland occurs at certain stages associated with sexual development and reproduction, namely the embryonic, prepubertal and pubertal stages, pregnancy, lactation and involution. Two cellular compartments make up the glands: the epithelium and the surrounding stroma, which are produced embryologically from the ectoderm and mesoderm, respectively. In all mammals, the mammary glands arise from localized thickenings of the ventral ectoderm or epidermis.
Glandular tissue of the mammary glands: structure and abnormal changes
The mammary glands (hereinafter referred to as the mammary glands) are located on the chest (from 3 to 6 ribs) and occupy the surface of the pectoralis major muscle. These are modified sweat glands. In men, these formations remain in their original (rudimentary) form throughout their lives; in females, the glandular tissue begins to gradually grow with the onset of puberty.
Anatomical features
The structure of the mammary gland of a mature woman is as follows:
- glandular tissue;
- fatty and epithelial (connective) layer.
Glandular tissue of the mammary glands
The breasts are divided into 15-20 lobes, each of which, moreover, is “broken” into several small parts.
The volume of adipose tissue determines the size of the mammary gland. The epithelium is “entrusted” with the function of attachment - it holds the breast on the pectoral muscles and does not allow it to fall down.
Glandular tissue is a collection of small milky structures that are localized in the lobules of the mammary glands. These formations consist of many branching tubes widened at the ends (these are alveoli in which the synthesis of breast milk occurs). The ends of the tubes - the milk ducts - pass into the sinuses, which open in the nipple.
The shape, size and volume of the breast in women change with age.
Diagnosis of breast cancer
Ultrasound (echography) of the mammary glands allows us to identify structural or functional changes in these organs. The structure of the breast varies from woman to woman (this is the norm). Thus, in young female representatives, the central part of the breast (glandular tissue) is characterized by homogeneous average echogenicity, and the fat layer is characterized by low echogenicity.
Interpretation of echograms, which are carried out in the diagnosis of breast diseases, includes the following components:
- assessment of the form of the neoplasm (correct, incorrect);
- its contours (can be clear, even, uneven, blurry);
- echogenicity of the structure;
- sound conductivity of the neoplasm.
Ultrasound helps detect breast tumors ranging in size from 4-5 mm. After examining the breast, it is necessary to study the condition of the areas of regional lymphatic drainage (indicates the absence/presence of metastases in the lymph nodes in breast cancer).
After an ultrasound examination of the breast, the doctor determines pathological changes in the structure of the organs (or other deviations from the norm) and, if necessary, prescribes treatment.
Breast pathologies
The mammary glands are under constant influence of various hormones (adrenal cortex, pituitary gland, thyroid and pancreas, ovaries). By the appearance and condition of the breast, one can judge the presence (absence) of hormonal disorders in a woman’s body.
For example, polycystic ovary syndrome is accompanied by fatty transformation into the breast. Uterine fibroids, endometriosis, polyps, endometrial hyperplasia - all these diseases cause pathological changes in the structure of the mammary gland.
The risk group for developing breast diseases includes:
- women who have not given birth;
- those who did not breastfeed;
- female representatives who do not have regular sex life.
Other factors causing pathological changes in the breast: benign and malignant tumors of the ovaries and uterus;
- excess body weight;
- hypertonic disease;
- dysfunction of the thyroid gland.
Other factors against which hyperplasia may develop: heredity;
- regular stress;
- long period of breastfeeding;
- chest injuries;
- working with toxic chemicals.
Breast hyperplasia “announces itself” with the following symptoms:
- chest pain, increased swelling in this area;
- nodules are detected on palpation;
- discharge from the nipple is observed (their color and consistency may vary).
Unfortunately, hyperplasia can be completely asymptomatic, so most often the phenomenon is discovered accidentally during a routine ultrasound.
Breast hyperplasia
There are several types of breast hyperplasia:
- dishormonal (cause – endocrine disruption, patients are prescribed hormonal therapy);
- glandular (tissue grows, forms disc-shaped structures). In the early stages, the disease is not diagnosed.
- Epithelial hyperplasia of the mammary gland (proliferation of connective tissue of the mammary gland). It is treated with medication, sometimes the phenomenon disappears on its own, and the condition returns to normal (for example, some time after childbirth).
- Diffuse. This hyperplasia is accompanied by the appearance of tumor-like and nodular formations in the breast.
- Nodular gland (degeneration of diffuse proliferation of glandular tissue of the mammary gland).
- Ductal g-th (epithelium grows in the ducts of the breast).
- Focal m. Seals are localized in different parts of the mammary glands.
- Stromal hyperplasia is a benign muscular fibrous tumor.
- Fatty gland (proliferation of adipose tissue of the mammary gland).
- Atypical Ms. The anomaly is accompanied not only by the proliferation of glandular, epithelial and adipose tissue, but also by pathological changes in the structure of the cells themselves. This disease is regarded by experts as a precancerous condition. Treatment is exclusively surgical.
Basically, in the early stages of the development of the disease, hyperplasia itself and the causes of its occurrence must be eliminated with the help of medications. In the later stages of the disease, with its complicated or atypical forms, patients are prescribed surgery.
When the first symptoms of pathology appear, you should seek help from a gynecologist (mammologist).
(voted:8, rating: 4.50 out of 5)
moloczheleza.ru
Symptoms of breast involution
Often there are no obvious symptoms of breast involution. In isolated cases, patients may notice pain in the chest area, radiating to the upper back.
- Age-related involution of the mammary glands most often occurs as follows:
- from 25 to 40 years - the mammary glands are subject to natural cyclic changes depending on the phase of the monthly cycle. Ultrasound examination indicates the presence of glandular tissue, the channels are not dilated, no pathologies are observed;
- from 40 to 50 years – signs of developing breast involution are observed, which are expressed in the form of fibrous mastopathy, fatty changes, fibroadenomatosis, papillomas or tumors;
- from 50 to 55 years – involution worsens, ultrasound shows a predominance of adipose tissue with preserved glandular tissue;
- from 55 years of age and over - an ultrasound shows almost complete replacement of tissue (glandular tissue is replaced by fatty tissue), there are normally no compactions.
- When feeling the gland, the doctor may note changes in the structure and loss of firmness of the breast. The skin may sag and the breasts may droop and become flaccid.
- Fatty involution of the mammary glands is a natural change in the female body during menopause, or after completion of lactation. The reasons are the same hormones, the levels of which are unstable.
Fat involution has no characteristic external signs. It can only be noticed using ultrasound or mammography. If involution is present, then in the photographs the mammary gland will appear lighter than usual, with a clear structure of blood vessels, milk canals and connective tissue fibers.
The shape of the mammary gland is formed by the height of the epidermal "milk ridge" which forms the milk line in some species. The milk line is a linear thickening of the epidermis on either side of the middle aspect of the embryo. In the mouse at embryonic day 16, cell proliferation at the tip of the mammary bud causes elongation of the primary duct, which grows toward the precursor mammary adipose tissue.
Human and muscle mammary glands have many differences and will therefore be discussed individually. The functional part of the human mammary gland is called the terminal tubular lobular unit, while the main functional units of the muscular mammary glands are called lobuloalveolar units. The human terminal ductal lobe consists of a small group of lobules emerging from the terminal duct, and thus resembles a cluster of grapes at the end of a stem. The muscular mammary gland at birth consists of a main duct with modest carbonization within the stroma of the mammary fat pad; However, in the pubescent mouse, the individual milk ducts terminate in a single bulbous terminal bud.
Signs of breast involution found in young girls and nulliparous women may indicate major hormonal problems. Such women require additional examination, especially for pathologies of the endocrine system.
- Fibrous involution of the mammary glands is a physiological replacement of glandular tissue with connective (fibrous) tissue. The involutionary process extremely rarely occurs in exactly this form. Most often it is combined, with replacement by connective and adipose tissue. This process is called “fibrofatty involution of the mammary glands”;
- fibrocystic involution of the mammary glands is the replacement of glandular tissue with connective tissue, with the simultaneous formation of cysts - cavitary benign neoplasms. In this case, by palpation you can identify areas of compaction in the mammary gland that resemble nodes or balls of liquid.
The involutionary processes of breast withering intensify towards the end of reproductive age: after 45-50 years. Ultrasound and mammographic examination at this time indicate diffuse proliferation of connective and fatty tissue elements. The thickness of the parenchymal layer gradually decreases from 14 mm to 4-6 mm. Such symptoms after 45 years are considered a physiological norm.
Prevention of Breast Involution
In the adult muscle mouse, the ducts have grown to completely "fill" the fat pad, and the terminal buds are no longer present; however, there is significant space between the minimally branched channels. Histologically, the stroma of the mouse uterus is strikingly different from that of humans. The muscular mammary gland contains a large amount of fat with a small amount of mixed fibrous connective tissue. Although the human breast also contains large areas of adipose tissue, the epithelium is not usually closely associated with the adipose tissue; Rather, it is due to fibrous connective tissue.
Always manifests as nipple discharge
Diffuse mastopathy with a predominance of the glandular component is always manifested by fluid discharge from the nipples, most often having a transparent color. As part of the restructuring of the hormonal background and the predominance of the concentration of some hormones over others, a false appearance of colostrum is noted (a secretion normally produced under the influence of prolactin in the very first days after childbirth).
Speaking about the characteristic lump in the breast, women note that there is no connection with the menstrual cycle. Solid formations in the glands remain unchanged at any time. Therefore, it is necessary to clarify the nature of the disease - whether it is benign or malignant.
In addition to compaction, swelling of both glands is simultaneously noted, and the skin color does not change its shade (unlike the inflammatory nature of the disease). Edema is also associated with hormonal changes in a woman’s body. Before the onset of menstruation, there is an increase in the release of prolactin, which is responsible for preparing the mammary glands for breastfeeding. As a result, the lobules enlarge and the breasts become larger, but compression of the blood vessels occurs, the passage of which is already difficult due to the development of mastopathy with a predominance of the glandular component. With the end of menstruation, the volume of the glands returns to its normal state, but the existing seals remain unchanged.
As the disease progresses to a more severe stage, enlarged lymph nodes may be palpated in the axillary region, and sometimes simultaneously above the collarbone. In this case, it is necessary to exclude the oncological process, which is most characterized by lymphadenopathy (enlarged lymph nodes).
Also read: Tests for laparoscopy of ovarian cysts
Diagnosis of breast involution
Diagnosis of breast involution is often based on two research options: ultrasound and mammography.
If necessary, the doctor may prescribe comprehensive examinations of the mammary glands, which include:
- examination and palpation of the breast, questioning about the course of menstruation, previous pregnancies or their interruptions, the presence of diseases, especially chronic ones;
- mammography (one of the most effective diagnostic methods in this case);
- ultrasonography;
- auxiliary thermography;
- computed tomography;
- ductography (galactography) - x-ray examination of the milk canals of the breast using contrast agents;
- If endocrine pathology is recognized as the fundamental factor in the development of involution, then the patient is prescribed hormonal replacement treatment to stabilize normal hormone levels.
- If, along with involution, the patient is diagnosed with other breast diseases (neoplasms, cysts, mastopathy), then, accordingly, first of all, treatment is aimed at combating more important manifestations.
- If there is severe breast tenderness against the background of involution, it is possible to prescribe anti-inflammatory, analgesic and sedatives. In some cases, hormone treatment is used.
This is important for the timely detection of various neoplasms that often appear at this age.
Both human and mouse mammary ducts contain similar epithelial cells. Initial pioneering work by Klaus Kratochwil, Teruyo Sakakura and Ken De Oem established the importance of mesenchymal-epithelial and stromal-epithelial interactions in the mammary gland from embryo to adult.
Epithelial-mesenchymal interactions in the embryonic mouse mammary gland
Mammalian muscular epithelial buds emerge from the embryonic epidermis as a result of mesenchymal induction. This initial stage of mammary gland development is independent of systemic signals and instead depends on mutual signaling between the epithelium and mesenchyme. They form as separate spots on two lines running ventrally only inside the limbs from the neck to the groin area.
Treatment of fatty involution of the mammary glands in young patients is mandatory, but only after determining the cause of the pathology.
Diagnostics
Mastopathy with a predominance of the glandular component is diagnosed by a mammologist without difficulty if the patient completes the entire range of examinations that are prescribed to her. These include:
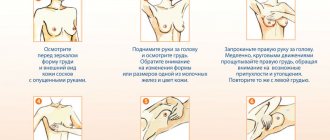
1) Self-examination of the mammary glands by a woman, which should be performed between the 5th and 12th days from the start of menstruation. Such periods are most favorable for this technique, since hormonal levels return to normal levels after menstruation. At the same time, the breast decreases in volume, becomes soft and painless, which facilitates palpation. Using the technique, a woman can detect certain changes in the form of compactions over the entire area of the mammary gland when mastopathy with a predominance of the glandular component is observed. During squeezing of the nipple, discharge necessarily appears, which also characterizes the diagnosis of glandular type mastopathy.
2) The next stage is a consultation with a mammologist with a survey and palpation of the mammary glands. The woman should provide all the information necessary to determine the cause of lumps and discharge from the breast. When collecting anamnesis, it is important to clarify:
· age of the woman (the occurrence of pathology is more typical in women under 40 years of age);
· the appearance of pain that is associated with the menstrual cycle or does not have a clear correlation with any circumstances. It is important for a woman to remember when in what period of time they intensify, and in what case they subside, what makes her character easier (aching, stabbing, pulsating);
· the occurrence of pain simultaneously not only in the chest, but also in nearby areas (neck, shoulder, shoulder blade);
· whether there is discharge from the nipples and when it is observed (spontaneous discharge or with pressure, increases or decreases in volume during the period of menstruation);
· whether operations were performed on the mammary glands or thyroid gland;
· presence or absence of sexual activity, its regularity, use of contraceptives;
· age when the first menstruation appeared and the cycle was established, duration, pain, heavy or scanty discharge, normalized schedule or there are delays;
· the number of pregnancies, children born alive, the presence of abortions, a frozen fetus or other types of miscarriage (mastopathy with a predominance of the glandular component in most cases occurs in nulliparous women);
· inflammatory diseases of the genital organs (cysts, fibroids, endometriosis, vaginitis, colpitis) in women who have previously suffered from it or have become chronic;
· presence of hereditary burden in relatives with detection of oncology, pathology of endocrine organs, liver and biliary tract.
3) Palpation of the mammary glands is carried out after carefully collecting from the patient the information necessary for diagnosis. Subsequently, the chest is examined and palpated in standing and then lying positions. The symmetry of the glands is assessed, the contours are compared, it is assessed whether there is a change in skin color, a protruding venous pattern, or deformation of the nipples. In the period from the 5th to 12th days of the menstrual cycle, the mammologist can perform palpation, which reveals lumps, and with this pathology they are observed throughout the mammary gland. Soreness is also noted, which often remains after the end of menstruation, the nature and color of the discharge from the nipples is assessed when they are compressed by the areola.
4) After a thorough objective examination, instrumental methods are used. The main one is mammography, performed on the 5-12th day of the menstrual cycle. This is due to the normalization of hormonal levels, when mastopathy with a predominance of the glandular component becomes clearly visible. At the same time, complete disappearance of signs of altered morphology is not observed, unlike other forms of pathology. Typically, the examination clearly reveals multiple formations without clear contours with a diameter not exceeding 1.5 cm.
5) Ultrasound of the mammary glands. It allows you to determine the presence of hyperplastic (increased number of cells and tissue components) lobules. The technique is also used when performing a biopsy with the collection of material for subsequent histological examination, where the abundance of glandular cells with altered morphology will be determined under a microscope.
6) Determination of the level of estrogen, prolactin and progesterone in the blood (in the 1st and 2nd phases of the cycle - on the 7-9th and 20-22nd days from the beginning of menstruation), and, if necessary, assessment of the functional state of the thyroid gland and adrenal glands .
7) Ultrasound of the pelvic organs is necessary to identify concomitant gynecological pathologies.
 If there is a need to conduct a study of the gland ducts, a referral for ductography is issued. Mastopathy with a predominance of the glandular component is accompanied by changes not only in the lobules, but also in the ducts. When the ducts are affected by a pathological process, zones of defective filling are revealed on the x-ray.
If there is a need to conduct a study of the gland ducts, a referral for ductography is issued. Mastopathy with a predominance of the glandular component is accompanied by changes not only in the lobules, but also in the ducts. When the ducts are affected by a pathological process, zones of defective filling are revealed on the x-ray.
9) Establishing pathology in a woman from other organs that can affect hormonal status is based on additional instrumental methods. For diseases of the endocrine system, it is advisable to conduct an ultrasound of the thyroid gland and adrenal glands. X-rays of the sella turcica area may also be indicated to examine the pituitary gland. If possible, a CT scan is performed, because Not all tumors can be detected by X-rays.
10) The presence of dense formations, which must be distinguished from pathology that turns into a malignant form. In this case, radiometry and histological examination are indicated. Atypical cells of the glandular epithelium during radiometry are characterized by increased temperature compared to tissue with normal morphology.
Prevention
The most important point in the treatment of any breast disease is prevention. As for the prevention of breast involution, the recommendations here are quite simple at first glance:
Patterns of gene expression were detected in the embryonic mammary bud and epithelial and mesenchymal specificity were demonstrated. Genes expressed during embryonic mouse mammary gland development. Note that genes are expressed in a tissue-specific pattern, with many genes expressed exclusively in the epithelium or mesenchyme.
Placodal formation: migration versus proliferation
Two mechanisms of formation of the placodal mammary gland are considered. One possibility is a local increase in cell proliferation. Accordingly, the possible role of cell proliferation in mammary placode formation was rejected in favor of an alternative theory. Squamous amoeboid cells were observed on top of cuboidal mammary ridge epithelial cells in the rabbit embryo, indicating that cell motility played a role in the formation of the placodal mammary gland. The initial expression profile and rapid shape change strongly suggest that ectodermal cells migrate along the presumptive mammary line to various locations where they form mammary placodes.
Forms of the disease
It is customary to distinguish 5 types of adenosis:
- Tumor-like. A lump is diagnosed in the mammary gland. Usually it is single and mobile. Its size is not too big. In most cases, the formation has a lobular structure. Such seals usually do not cause any discomfort in the patient, discharge from the nipple is not observed in most cases, and there are no changes in the skin of the gland. Lymph nodes are most often not enlarged.
- Adenosis of the terminal ducts of the mammary gland. Incorrectly formed lobules of milk ducts are found in the breast tissue. Internal papillomas and sometimes epithelial metaplasia are common. There are usually many seals, and they differ in density. With this form of the disease, a woman may experience quite painful sensations.
- Apocrine. Palpable nodes are localized in the chest, repeating the configuration of the lobules.
- Tubular. The mammary glands contain multiple tubes (slightly elongated) of the same size. Microcalcifications or a double layer of epithelial cells are often found in the ducts.
- Microgranular. This form of the disease does not have its own symptoms and is diagnosed accidentally.
Forecast
Even if involution processes do not bother a woman in any way, periodic visits to a gynecologist should not be ignored. It is necessary to constantly keep breast health under control, and after 40-50 years, ultrasound of the mammary glands must be done annually. It is during this period that there is an increase in hormonal instability, and the risk of developing breast tumors increases significantly.
Formation of the milk placode: the role of mesenchymal induction
However, he was unable to examine induced epithelial buds for the expression of mammary gland-specific markers.
This work was repeated many years later, growing embryonic epidermis from the middle or dorsal portions of 13-day-old rat embryos in combination with 13-day-old mouse embryonic mammary mesenchyme. The resulting tissue recombinants were inoculated into virgin and lactating female anhydrous mouse hosts. In both host types, these tissue recombinants formed keratinized skin with hair follicles and sebaceous glands. Of course, the earlier these diseases are detected, the more optimistic the prognosis will be.
The diagnosis of “breast involution” should under no circumstances cause panic. After all, with age we change, and the organs and tissues in our body also change, including the mammary glands. But if such changes occur during reproductive age, then you should be wary: this indicates a hormonal imbalance. But this problem can also be solved: the doctor will evaluate the causes of the pathology and prescribe appropriate treatment.
When grown in lactating female hosts, induced mammary epithelial cells formed lobuloalveolar structures and expressed casein and α-lactalbumin. These data confirmed Proper's original data and showed that fetal mammary mesenchyme induces and determines the differentiation of the mammary epithelium from the epidermis, both morphologically and functionally. Thus, the epithelial identity of the mammary gland appears to be stable at 13 days of gestation.
Differences between men and women in breast development
Control homotypic tissue recombinants, consisting of embryonic epidermis and dermis, differentiate into skin. However, functional cytodifferentiation of the epithelium pointed to the mammary gland. Once formed, embryonic mouse mammary buds either survive, produce mammary tissue in females, or regress in males. In most mouse strains, androgens cause condensation of mesenchyme around male mammary buds and cause destruction of the epithelial bud by day 16.
Changes in breast tissue occur throughout a woman’s life, from the moment the organ is formed until the onset of menopause. In nature, everything is organized rationally, so an organ that no longer performs its functions gradually atrophies. About the same thing happens to the mammary gland at the age when a woman loses the opportunity to become a mother. This is a natural condition that can only be classified as fibrofatty mastopathy if it is diagnosed in a young woman.
This complex process described involves a series of reciprocal interactions between the epithelium and mesenchyme. Sexually dimorphic development of female and male muscular mammary glands. The appearance of mammary gland placodes and bud formation are the same in men and women.
Mesenchyme of the mammary gland compared to the chest
Fetal mammary explants were exposed to testosterone for varying periods of time to determine the acquisition and subsequent loss of androgen sensitivity. These data suggest that the mammary buds were destroyed by mesonymous cells activated by testosterone rather than by the direct action of hormones. Epithelial-stromal interactions in the postnatal mouse mammary gland: hormonally mediated growth and development. Mice mammary gland development mainly occurs after death.
A gradual decrease in the level of sex hormones leads not only to the absence of menstruation and the inability to get pregnant. This causes significant changes in a woman’s body, affecting not only the genitals, but also the mammary glands. Some women experience mastopathy associated with “jumps” of hormones, but this type of change in gland tissue does not apply to the disease at this age. Approaching menopause, women begin to notice changes in the condition of their breasts - they become larger, softer, lose their density and clear outline.
Other diseases from the group Diseases of the endocrine system, nutritional disorders and metabolic disorders
Initially, the ductal system begins to develop from the nipple during the embryonic stage.
During puberty, specialized structures called terminal buds develop at the ends of the ducts. In addition to the terminal terminal buds responsible for ductal elongation, there are two other types of buds. Lateral buds develop along mature ducts, grow for a short distance, and then stop due to the presence of other competing ductal elements. This condition is associated with decreased hormonal levels and the gradual replacement of glandular tissue of the breast lobules with fibrous tissue and fat. We can say that involution is a gradual transition from the functional role of the mammary gland to a purely decorative one.
Alveolar buds develop in most mouse strains only in response to pregnancy hormones. The development and function of the postnatal mammary gland is largely dependent on the actions of the pituitary gland, adrenal glands and ovaries. During the release of ovarian hormones during puberty, the terminal terminal buds grow in the fat layer, undergo branched morphogenesis and lay out the minimally branched mammary ductal “tree” characteristic of the virgin state.
During the entire estrus cycle, modest development of the ductal system occurs. During pregnancy, there is dramatic growth of the lateral and alveolar buds, leading to the development of the lobuloalveolar structures that produce milk. This rapid epithelial growth is caused by an increase in ovarian hormones and prolactin. Once weaning has occurred, the fully developed mammary gland enters a virgin state. Interactions between the epithelium and stroma play an important role in mammary gland development and branching morphogenesis.
Natural state:
- After the age of 40, the onset of this process is not a pathology and does not relate to mastopathy, being a normal physiological phenomenon. The longer a woman maintains a high hormonal level, the later the fibrotic change occurs.
- In some women, even after 50, with a prolonged or late menopause, the mammary glands not only retain their shape, but also their internal lobular structure. But with a gradual decrease in the amount of hormones, the lobules become smaller and are replaced by fibrous tissue, and subsequently by fat.
- At an advanced age, there is no functional mammary gland tissue left in the breast. This suggests that the process of involution is the norm and inevitably awaits all women, most importantly - at what age.
Pathological process:
In rare cases, fibrofatty involution can occur in young women long before the premenopausal period. This means a hormonal imbalance in the body caused by a decrease in the production of sex hormones.
This condition is equivalent to mastopathy and requires treatment.
The largest percentage of the disease is observed in women with hormonal problems affecting not only the breasts, but also the genital and endocrine organs.
There are documented cases of changes in tissue composition in women who have given birth and breastfed a lot. But such changes also occur in very young girls who are in the process of puberty. In this situation, it is very important to quickly determine the cause of the disease and begin treatment in order to avoid not only the degeneration of breast tissue, but also disturbances in reproductive function.
Classification of female breast tissue
The entire variety of structures of the female bust is classified according to morphotypes, and for the same woman it changes throughout life depending on the state of the hormonal background.
The following morphotypes of mammary glands are distinguished:
- Juvenile.
The chest is small in size, fine-grained in structure. There is a highly echogenic glandular layer under the skin near the nipple.
Fine-mesh hypoechoic areas are observed, there is no retromammary fiber, premammary fiber is present in fragments.
There is an increase in the number and size of hypoechoic areas, a mesh pattern is visible, there is no retromammary fiber, premammary fiber is observed as a continuous layer.
Normally, the glandular tissue of the mammary gland predominates, but fatty lobules of 1-2 cm in size are formed in it, and retromammary tissue is visible as a continuous layer.
The parenchyma is almost completely replaced by adipose tissue, there is no layered structure, no mesh pattern is observed, adipose tissue is presented in the form of a uniform strip, premammary tissue has many partitions.
The breast consists entirely of connective tissue and fat lobes. There is little glandular tissue in the mammary gland (only round islands measuring approximately 3-5 mm are observed).
- Lactational.
The breast consists of glandular tissue. Near the nipple, the ducts widen.
Wulf classification
There are several classifications of breast density, but the first qualitative one is considered to be the Wulff mammogram division, according to which 4 types of density are distinguished depending on which tissue predominates in the gland - adipose or glandular.
According to this classification, the following types are distinguished:
- N1. The gland is dominated by adipose tissue. The risk of developing breast cancer is almost zero.
- P1. The gland consists of adipose tissue and dilated ducts, which occupy 25%. Oncology with this type occurs extremely rarely.
- P2. The number of dilated ducts occupy more than 25% of the breast. Women with this type have an increased risk of breast cancer.
- Dy. Severe compaction of breast tissue . Belongs to the category of the highest likelihood of developing cancer.
- Qdy. Breast tissue with a dense spongy structure due to fatty inclusions.
Also read: Dermatitis on the neck of a baby
Boyd classification
In 1980, Boyd proposed another method of classification based on the ratio of the density of the mammary gland structures as a percentage.
In accordance with it, there are 6 categories of breast density:
BI-RADS density classification
BI-RADS refers to quantitative methods for classifying breast structure density. At its core, it is a modification of the Wulff mammogram separation.
The BI-RADS classification is discussed in the table.
| Type. | Characteristic. |
| a. | Fibroglandular tissue of the mammary gland makes up less than a quarter of the total area. The fat component is the main one. |
| b. | Fibroglandular tissue foci occupy 25-50% of the breast. |
| c. | The main tissue is fibroglandular tissue of the mammary gland (51-75% of the area). |
| d. | Dense breast tissue with predominant fibroglandular tissue. Its percentage is more than 75 of the mammogram area. |
Tabar classification
This classification of breast tissue density is based on the relationship between mammological and histological data. According to its division, there are 5 main types:
There is a balanced ratio of tissues, there is slight fibrosis of breast tissue .
There is a large amount of adipose tissue.
Adipose tissue predominates, but retroareolar fibrous tissue is also present.
Predominantly nodular density.
The main tissue is fibrous.
According to the Tabar classification, the first 3 types have a low probability of developing breast cancer, and types 4 and 5 have a high probability.
Causes of breast involution
In both cases, the cause of the degeneration of breast tissue into fibrous tissue and its gradual replacement with fat is caused by hormonal deficiency. Only in the case of a woman past childbearing age is this normal, but for a young woman it is a serious pathology. This form of mastopathy requires timely identification and treatment.
A gradual decrease in hormone production is a normal state of the body that comes with age. In a young woman, there may be many more reasons for involution.
This is hypofunction of any hormone-producing organ:
- Ovaries,
- Thyroid gland,
- Pancreas,
- Adrenal glands.
A decrease in the production of hormonal substances will lead to disruptions in the functioning of the entire body and to the development of many diseases, not only the sexual sphere. This is due to the regulating role of hormones in our body.
The most common breast pathologies and their ultrasound signs
Ultrasound signs of breast pathology depend on the type of pathology. Let's describe the most common of them.
Pathology
| Description | Ultrasound signs of pathology | |
| Fibroadenoma | It occurs more often in young women. This is a benign connective tissue tumor. Dense, elastic, not welded to surrounding structures. | It has regular contours, a homogeneous structure, is hypoechoic, enclosed in a hyperechoic capsule, and is solid in size. |
| Lipoma | Benign fatty tumor. Dense, not fused with surrounding structures. | An oval, clearly circumscribed formation with a hypoechoic structure in a hyperechoic capsule. |
| Mastopathy | A common disease, characterized by the proliferation of the glandular, stromal component of the organ, the formation of cysts, mastodynia and even pathological secretion. | The thickness of the parenchyma does not correspond to age (increased), echogenicity as after menopause, deformation and ectasia of the milk ducts are visualized. In the cystic form, many cysts are visualized. But the ultrasound morphotype of the gland corresponds to age. |
| Mastitis | Inflammatory disease of the breast, often develops as a result of injury or stagnation of milk. | The picture depends on the duration of the process. The doctor detects diffuse changes in the glandular tissue and area(s) of hypoechoic structure and hyperechoic elements of the capsule around them. |
| Injury | A blow, a bruise, the consequence of which is a hematoma. | Immediately after the injury, the doctor sees hypo- or anechoic lesions with a heterogeneous structure. Then an irregularly shaped formation with thickened walls and inclusions is formed, the echogenicity of which is increased. |
| Malignant tumors | Proliferation of atypical cells with invasion of blood vessels into the tumor. | Tumor growth gives a completely different picture depending on the form of the disease. For example, diffuse cancer imitates the ultrasound signs of diffuse mastitis. Most often, cancer on ultrasound is a heterogeneous structure with low (lower than fat) echogenicity and an acoustic shadow behind the tumor. |
Also read: Maxillary sinuses location diagram drawing maxillary sinuses
Any signs of breast disease indicated by ultrasound require treatment (and it will depend on the disease). Be sure to follow your doctor's advice and stay healthy!
This concludes our review of the topic. We invite you and your friends to our website again, just subscribe to our newsletter. You can share information from our website through social networks.
A woman’s breasts are not only the subject of her pride and constant care. It is also a very complex organ in structure, which largely depends on the hormonal balance of the body. During life, breast tissue undergoes changes depending on the predominance of any hormone (estrogen, progesterone). In most cases, this is the norm, but sometimes changes in breast tissue may indicate the development of pathological processes.
Diagnosis of the condition and its symptoms
A woman can notice this process herself when it has already gone far enough.
- The mammary gland becomes softer, its elasticity decreases, and with severe degeneration it hangs, changing its usual shape. Another symptom that may not be present is the presence of chest pain. This condition is similar to the usual manifestations of mastopathy. In the early stages, changes in breast tissue are asymptomatic and do not cause the woman any discomfort.
- Fibrous involution is often mistaken for osteochondrosis, since the pain can be nagging and radiate to the spine or shoulder blades.
- By palpation, the doctor can determine changes in tissues and refer the patient for further examination. In each specific case, a blood test for hormones provides a lot of information.
- Ultrasound diagnostics is not informative and may miss small fibrous formations. X-ray of the mammary glands will provide more accurate data.
Diagnostic options
Glandular mastopathy can be detected during self-examination. Typically, women pay attention to enlarged lymph nodes and compacted lobes in the breast, which can be mobile and change in size or shape. But only a mammologist can make a final diagnosis.
He will conduct a professional examination of the affected gland, determine the location and size of the tumors. If the woman’s condition does not cause concern, the doctor will continue observation, determining how the lumps behave in different phases of the menstrual cycle.
If fibroids are detected, the patient will be offered an ultrasound examination. An ultrasound will help you understand whether the overgrown tissues are fibroids or cysts. Women over 40 years old are prescribed mammography.
It is not indicated for young patients, since dense tissue does not allow obtaining a reliable result. The looser the glandular tissue and the thinner the fat layer, the more accurate the diagnosis can be made.
If the tumor is in doubt, a puncture followed by sending the tissue for cytological analysis is possible. It must confirm the benign nature of the tumor. Sometimes the patient is additionally prescribed a blood test, and is also examined by a gynecologist to rule out tumors in the uterus or ovaries.
When and who needs treatment for fibrofatty involution?
Women over the age of 40 do not need treatment; their fibrotic changes in the mammary glands are not mastopathy or another disease.
In young women and girls, such mastopathy of the mammary glands is a dangerous pathological process that requires the use of oral contraceptives in mild cases, and in later stages - hormone replacement therapy.
If this is not done in a timely manner, the mammary gland may lose its functions. The selection and prescription of drugs, dosage and duration of treatment is the responsibility of the doctor. All medications are prescribed personally for a specific patient.
Regular visits to the doctor and careful attention to your health will help you quickly cope with the early manifestations of involution of breast tissue and preserve this organ for feeding your offspring.
Features of treatment
For the treatment of initial forms of glandular mastopathy, herbal remedies and homeopathic remedies are prescribed. Their task is to harmonize hormonal levels, relieve pain and a feeling of heaviness, and improve the general condition of the patient.
It is possible to take painkillers, and only a doctor can prescribe them.
To relieve anxiety and improve sleep, herbal teas based on mint, lemon balm, licorice, hawthorn fruit, and rose hips are useful.
At a later stage, hormonal drugs with natural prolactin or the latest generation of contraceptives work well. You can take pills, injections or vaginal suppositories.
External herbal remedies will help reduce discomfort:
- balms;
- ointments;
- creams;
- lotions.
When large fibroids and cysts form, injections of testosterone or steroids are indicated, but they are used quite rarely.
Medicines can be supplemented with traditional medicine recipes. Swelling and a feeling of heaviness are well relieved by compresses made from the leaves of white cabbage, burdock, and coltsfoot.
Applications with bee honey, propolis, and grated beets are good absorbent agents. Tinctures made from celandine or hop cones, which are drunk before meals, are useful.
You can find out the features of home treatment We have collected the best folk recipes especially for you:
- collection of the best recipes No. 1;
- collection of the best recipes No. 2;
- collection of the best recipes No. 3.
There are other ways to use folk remedies, more details here.
It is important to include the correct daily routine with continuous night sleep, walks, sports and fitness into the treatment regimen. Diet occupies a special place.
Glandular forms of mastopathy require a reduction in calorie intake to 2000-2200 kilocalories. Excess adipose tissue contributes to the production of estrogens and the deterioration of the patient’s condition.
The menu should include fresh, stewed or boiled vegetables (at least 400 g per day).
The diet will be supplemented with whole grain cereals, fermented milk products, lean white meat and fish. Fresh fruits and berries are required, providing the body with vitamin C and amino acids.
For successful treatment of the disease, it is important to completely abstain from alcohol; ethyl alcohol in any concentration is very harmful to the glandular tissue of the breast. From the menu you need to exclude fatty and fried foods, red meat, sweets and a variety of fast food rich in sugar, salt and hydrogenated fats.