The disease alveococcosis is infectious because it is caused by infection with helminths (tapeworms of the order tapeworms). Another name is alveolar or multilocular echinococcosis. The pathology is characterized by a long-term chronic course.
Alveococcosis of the liver occurs with a frequency of 44.2–84.2% (according to some sources, 90%). The favorite localization of the consequences of the introduction of the parasite is in the right lobe of the liver (2 times more often than other parts). This is explained by more convenient circulatory conditions for pathogen entry: on the right, the branch of the portal vein has a relatively large diameter, and the angle of its departure from the main vessel is obtuse.
Liver damage is tumor-like in nature and often metastasizes to other organs, especially the brain and lungs. In the International Classification of Diseases, alveococcosis is taken into account together with liver echinococcosis under code B67.5.
Features of distribution
In nature, there are geographical foci of alveococcosis. In them, the pathogen constantly circulates in the blood of wild animals, which become sources of human infection. These include:
- countries of Central Europe;
- South and Central America;
- Alaska;
- northern part of Canada;
- Middle Asia;
- countries of Transcaucasia.
The trade of the peoples of the north is associated with dog breeding and hunting
In Russia, dangerous territories are considered:
- Far East;
- Ural region;
- Siberia,
- Kirov region.
The maximum incidence of alveococcosis is determined by:
- in Yakutia;
- Krasnoyarsk, Altai and Khabarovsk territories;
- Omsk and Tomsk regions.
Isolated cases (sporadic) are reported in Bashkortostan and Tatarstan.
Prevention
To avoid infection with such a dangerous disease as pulmonary alveoccosis, you must follow the following simple rules:
- Wash your hands thoroughly with detergent after contact with animals;
- Subject animal meat to thorough heat treatment before use for food;
- During forest walks, take special care when collecting wild berries and plants. Water from natural sources must be boiled.
- Periodically carry out antiparasitic prophylaxis in domestic animals;
- Prevent dogs and cats from eating mice.
Specialized government organizations are required to control the number and migration of wild animals - carriers of infection.
Alveococcosis of the lungs is sometimes called “parasitic cancer.”
Although humans rarely become infected with this helminth, in recent decades the world has seen an increase in cases of alveococcus infection among the population. Therefore, awareness about the seriousness of the disease and ways to prevent it is so important.
Characteristics of the pathogen
The class of tapeworms (tapeworms), to which alveococcus belongs, parasitize primarily in the body of warm-blooded animals (birds, mammals). There are several species that also infect humans. The development of alveococcus corresponds to the general rule of the mandatory change of two hosts. The first of them is intermediate, the second is final.
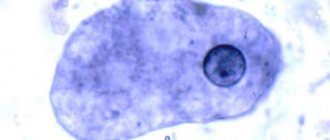
The causative agent of liver alveococcosis is an alveococcus larva called oncosphere. It is located inside each of many small bubbles (alveoli), which have grown together into a knot. The cavities are filled with a yellowish liquid with a thick consistency; there may be a dark-looking mass. Each vesicle contains a parasite embryo.
The structure of the female worm is distinguished:
- head or scolex with hooks (up to 30);
- neck;
- segments 2–5 pieces containing the uterus with eggs.
Alveococcus in a photo taken with a high magnification microscope
The conglomerate of vesicles continuously grows by budding. Such a node is called a finna or larvocyst. Its structure is characterized by multi-chamber. Inside each vesicle there are 1–3 embryonic heads. Increasing in size, the larvocyst forms a cyst with many chambers.
The development cycle of alveococcus is similar to the causative agent of echinococcosis, but the disease has a more severe course due to the germinating nature of the spread of finna from the affected liver. In addition, differences are determined when comparing sexually mature forms of worms: alveococci have smaller sizes (less than 2 mm) and different structures of hooks and uterus.
When Finna increases in volume, it compresses the surrounding liver tissue like a tumor. The separation of vesicles containing the alveococcal germ and its spread through the bloodstream are similar to the process of metastasis.
Node Description
Formed alveococcal nodes (larvocysts) in the liver are histologically represented by an inflammatory reaction and necrosis of parenchymal cells. They reach a size of 30 cm or more. The section shows a whitish color, with a density reminiscent of cartilage tissue. There are cystic cavities inside. If growth is directed towards the surface, the alveococcal liver node is capable of sprouting into neighboring organs:
- right kidney;
- diaphragm;
- bones;
- other fabrics.
Distant metastasis is possible.
Reservoir of infection and type of human infection
The reservoir for alveococcus are wild animals:
- foxes;
- wolf;
- arctic foxes;
- coyotes.
Very rarely – pets (dogs). Typically, cats and dogs serve as carriers only for echinococcosis.
These cute beavers in some areas are taken under protection by ecologists, but do not forget that they can also be distributors of alveococcosis
Rodents can be intermediate distributors:
- field mice,
- gerbils,
- gophers,
- muskrats,
- nutria.
In exceptional cases - a sick person.
Infection of wild animals occurs during the consumption of intermediate hosts of alveococcus (rodents) with larvocysts filled with larvae. In the intestines of predators (definitive hosts), embryos mature into adults in very large numbers. This process takes 35 days. In each segment, up to 800 oncospheres (eggs) are formed. The release of oncospheres to animals lasts 7 months.
Alveococcal oncospheres are extremely stable in the external environment. They retain their infectious properties for 143 days at a temperature of minus 40 degrees Celsius.
A person becomes infected when alveococcus eggs enter the digestive system. It occurs through the mouth by ingestion if proper hand washing after contact with fur is not followed. Less commonly, cases of infection occur after eating unwashed berries collected in the forest or using herbs for traditional treatment. They may be contaminated with animal feces.
Contact with alveococcal eggs occurs:
- when walking and working in the forest, in the field;
- picking berries and mushrooms;
- drinking water from rivers and streams;
- hunting;
- processing of hides;
- caring for sick animals.
A rare mechanism of infection is inhalation of dust particles contaminated with feces containing oncospheres. In such cases, alveococcosis affects the lungs. Anyone is susceptible to infection. Most often, the disease spreads among the population aged 30 to 50 years.
How can you get infected?
People become infected by ingesting parasite eggs or failing to comply with hygiene rules. There is a high risk of infection among hunters and anyone who has anything to do with animals. In rare cases, you can become infected from domestic animals, but when cutting up a fox carcass you need to be especially careful.
The disease does not spread from person to person because the parasite inside cannot reach maturity and cannot produce eggs. People do not infect each other with alveococcosis; this is impossible.
It is possible to become infected by eating unwashed berries and herbs that have been contaminated with the feces of various wild animals. In rare cases, eggs enter the human body through inhalation of dust.
Mechanism of liver damage
Alveococcal oncospheres enter the digestive tract through the mouth. In the human small intestine, eggs lose their outer shell and become embedded in the wall. Then they are absorbed into the blood, lymphatic vessels through the intestinal wall and reach the right lobe of the liver with the bloodstream. Another localization is a consequence of metastasis.
It takes several years for a multilocular cyst to form in humans.
The effect of alveococcus on the human body
The entry of alveococcus into the human body causes responses that are serious for health. An infected person has to deal with the consequences:
- sensitization of the body by waste products of the parasite, which are toxins for humans;
- mechanical compression of tissue by a growing node (cyst), which causes serious impairment of liver function, increases the spread of toxins through the bloodstream, and creates a danger to other organs and systems;
- obstructive jaundice, foci of necrosis in the liver;
- formation of secondary foci (metastases) in the lungs, brain, heart, adrenal glands, spleen with disruption of the functioning of these organs;
- the appearance of immunodeficiency, the development of an autoimmune reaction to destroy one’s own cells.
Stages of the disease
During alveococcosis there are several stages:
- Asymptomatic (preclinical). Can last up to 10 years. The disease is discovered as an incidental diagnostic finding during the examination of a patient for another reason.
- Uncomplicated. The pathological process is localized in the liver, that is, the location of the primary tumor. Patients complain of digestive disorders.
- Complicated. It is characterized by the presence of metastatic tumors and significant dysfunction of a number of internal organs.
Symptoms
Symptoms of liver alveococcosis appear several years after infection. Before this, the person does not feel the disease, there are no complaints. The doctor suspects the disease if, upon examination, a dense, lumpy, enlarged liver is detected. Doctors in endemic areas are especially wary.
The initial signs of the disease are usually caused by impaired liver function. In the clinical course of alveococcosis, several stages are distinguished.
Early stage – accompanied by:
- intermittent dull pain in the right hypochondrium;
- feeling of heaviness;
- weakness;
- loss of appetite.
Examination of the patient already at this stage makes it possible to palpate a dense node if it is located closer to the periphery of the liver. A laboratory blood test for protein shows an increase in total protein due to the gamma globulin fraction. ESR increases.
The stage of the height of the disease is characterized by the progression of all signs and symptoms of digestive disorders:
- pain in the right hypochondrium becomes constant and intense; the patient has a feeling of heaviness and belching after eating;
- there is a bowel disorder;
- weakness increases;
- no appetite.
At the height of the disease, pain in the right hypochondrium spreads to the epigastric region
Palpation reveals a dense tuberosity due to inflamed areas of the liver and multiple nodes. Such a liver is usually called “stony”. Laboratory indicators become sharper:
- a moderate increase in blood eosinophils appears (up to 15% of all leukocytes);
- significant acceleration of ESR;
- dysproteinemia is expressed (with an increase in total protein to 110 g/l, albumin decreases, but gamma globulins are significantly increased);
- increased C-reactive protein;
- growth of thymol test (a sign of inflammation of the liver tissue).
The stage of severe manifestations is most often accompanied by the development of severe obstructive jaundice:
- light stool appears and urine darkens;
- yellowness is visible in the color of the sclera, oral mucosa, skin, is persistent, sometimes a greenish tint appears;
- severe itching of the skin of the extremities and back.
In laboratory indicators, the total amount of bilirubin in the blood increases due to the direct form, and an increase in bile pigments in the urine is detected.
At this stage, it is possible for alveococci to grow from the liver into large vessels and form secondary foci. Therefore, the clinic appears:
- as signs of increased pressure in the portal vein - swelling in the legs, ascites, varicose veins of the esophagus are accompanied by the danger of bleeding;
- 50% of patients experience symptoms of glomerulonephritis, possible urination problems, and urine analysis shows red blood cells, protein, pus, and white blood cells.
The terminal stage is characterized by a severe course. There are dysfunctions not only of the liver, but also of all affected organs. Their changes become irreversible. Patients are exhausted, suffer from pain, complications against the background of severe immunodeficiency.
Alveococcosis of the lungs
Lung damage occurs due to metastasis of cysts from the liver. It is possible that oncospheres can be transported with blood flows.
There are several forms of pulmonary alveococcosis:
- focal;
- nodal;
- infiltrative;
- strip;
- pneumonic;
- mixed.
From the listed forms it is clear how difficult it is to correctly diagnose the disease.
Symptoms
- chest pain;
- cough with purulent sputum (or mixed with blood).
In any form of the disease, it is necessary to examine the liver, since it is the root cause of the disease.
Alveococcosis of the lungs
What are the possible complications?
If the patient’s temperature rises sharply and pain intensifies, then one should assume:
- infection of cystic contents with the formation of a liver abscess and its disintegration;
- obstructive jaundice can contribute to purulent cholangitis;
- if a cavity breaks through, the patient’s pain increases and the temperature rises;
- inflammation of the fatty tissue around the liver (perihepatitis).
A serious complication is the growth of the node into surrounding organs and tissues (gall bladder, omentum, kidney, ligaments, through the diaphragm into the lungs, pericardial sac, heart) and the addition of systemic amyloidosis with kidney damage and the development of renal failure.
Diagnostics
To make a correct diagnosis, it is necessary to take into account the epidemiological history. It includes data from the previous few years:
- by way of life;
- contact with wild animals;
- areas of residence;
- hunting;
- professional risk.
A referral for examination will be issued by a qualified specialist.
For final diagnosis use:
- laboratory methods - changes in the general blood test, disturbances in the proportion of proteins, biochemical tests of the liver, the appearance of bilirubin in the urine and blood are important;
- serological tests - based on the detection of specific antibodies to alveococcus, indirect hemagglutination reaction, latex agglutination, enzyme immunoassay are used;
- a skin allergy test, called the Cazzoni reaction, is more indicated for liver echinococcosis; in the diagnosis of alveococcosis it is used to identify differences;
- instrumental studies can detect a violation of the size of the liver, tissue structure, cystic formation with chambers inside the liver, ultrasound, computed tomography and magnetic resonance imaging, radiography with contrast of the bile ducts, radiographs of the liver against the background of pumping air into the abdominal cavity (pneumoperitoneum) are used;
- a node biopsy is performed during laparoscopy if echinococcosis is completely excluded, since the procedure in this case threatens contamination of the abdominal cavity.
For the purpose of differential diagnosis, it is imperative to exclude:
- echinococcosis;
- liver cirrhosis of various etiologies;
- neoplasms of both malignant and benign nature;
- polycystic liver disease;
- hemangioma.
Treatment
Treatment of alveococcosis is carried out in a hospital setting. The possibilities and methods depend on the stage at which the process of liver damage is located. Surgical methods are indicated for timely detection, absence of spread of the lesion from the liver to neighboring organs and distant metastasis. Unfortunately, such radical treatment accounts for only 15% of cases. The cyst is surgically removed along with the liver lobe or within healthy tissue.
With incomplete removal, the goal is to reduce compression of adjacent structures. In the remaining areas of the liver tissue, they try to reduce the active growth of parasites using a circular injection with a solution:
- Trypaflavina,
- palmitic acid thymol ester,
- 96% alcohol.
Postoperative complications occur in every third patient, and mortality is quite high (13–15%). A liver transplant can solve some of the problems.
There is information about good results of treatment using the cryodestruction method (exposure to cold temperatures of minus 196 degrees).
The prescription of antiparasitic drugs is indicated in the postoperative period and in cases where it is impossible to use the surgical method. Therapy helps:
- delay the spread of alveococcus;
- limit the affected area;
- avoid metastasis.
But complete destruction of the pathogen in the liver cannot be achieved. The drug Albendazole and Mebendazole are used. Its dosage is calculated based on the patient’s weight. Treatment is carried out in long courses with breaks.
The drug is toxic, so monitoring by the attending physician is required.
Symptomatic remedies include:
- immunomodulators to activate defenses;
- diuretics;
- cardiac drugs;
- antiallergic drugs.
Forecast
The prognosis for alveococcosis is always serious. Without appropriate treatment, about 90% of patients die within 10 years. Lead to death:
- distant metastasis to the brain;
- tumor infiltration into neighboring organs with disruption of their functions;
- profuse bleeding;
- liver failure;
- purulent complications.
Surgical intervention leads to complete recovery, with early diagnosis and timely treatment, but the risk of incomplete removal of nodes and their further development cannot be excluded.