Every pregnant woman must undergo diagnostics such as ultrasound screening three times during the entire period. The first time it is prescribed is at 12 weeks of pregnancy. Conducting this type of research earlier or later may provide unreliable information. Ultrasound screening examination is repeated in the 2nd and 3rd trimesters. If there are certain indications or if the expectant mother wishes, ultrasound diagnostics can be performed unscheduled.
At 12 weeks, the results of the study provide complete information about the development of the fetus and all its vital organs. After ultrasound diagnostics, the doctor deciphers the indicators, compares them with the norm, and identifies the peculiarities of the course of pregnancy. Based on this, a decision is made to continue the pregnancy, further appointments and the need for additional tests.
What is perinatal screening?
Perinatal screening involves examining a pregnant woman to identify various defects of the child at the stage of intrauterine development. This method includes two types of examination: a biochemical blood test and an ultrasound examination.
The optimal period for conducting such an examination has been determined - a period from ten weeks and six days to thirteen weeks and six days. There is a certain standard for ultrasound screening in the 1st trimester, with which the results of the examination of a pregnant woman are compared. The main task of ultrasound at this time is to identify serious malformations of the embryo and identify markers of chromosomal abnormalities.
The main anomalies are:
- TVP size—thickness of the space of the collar zone;
- underdevelopment or absence of nasal bones.
Ultrasound during pregnancy can reveal signs of a disease such as Down syndrome, and some other pathologies of fetal development. The screening norm (ultrasound) of the 1st trimester should be analyzed before 14 weeks. After this period, many indicators are no longer informative.
What is a screening test during pregnancy?
Screening is a series of medical procedures through which pathologies and diseases of the fetus can be recognized. The results point to certain causes of the problem that contribute to its development.
Perinatal screening is performed on a pregnant woman to calculate the likelihood of the child having neural tube defects, Down syndrome, and Patau syndrome. It is carried out in several stages:
- Ultrasound examination - examination of the fetal body, features, presence of chromosomal abnormalities. They also study blood flow in the umbilical cord and heartbeat, as well as the functionality of the placenta.
- Biochemical analysis - the presence of proteins in the blood of the expectant mother is calculated in order to identify possible pathologies of the child.
- If the first two stages showed a high risk of genetic pathologies, then invasive methods are used to clarify the result.
Screening identifies multiple pregnancies, the location of the placenta and the overall risk of developing pathologies.
1st trimester screening: ultrasound norms (table)
To make it easier for a doctor to determine the condition of a pregnant woman, there are certain tables of indicators of the development of the baby’s organs. The ultrasound examination protocol itself is drawn up in a structured manner so that the dynamics of the formation and growth of the embryo are clear. The article presents screening standards for the 1st trimester.
An ultrasound transcript (the table below) will help you get information about whether everything is okay with the fetus.
| Name of body (criteria) | Normal indicators | Gestation period (weeks) |
| KTR (size from coccyx to crown) |
|
|
| HR (heart rate) |
|
|
| TVP |
|
|
| Yolk sac | rounded shape, organ diameter 4-6 mm. | up to twelve weeks |
First screening during pregnancy
In the first three months of pregnancy, absolutely all women undergo this painless procedure.
First screening during pregnancy
provides an opportunity to recognize pathologies in fetal development. It consists of an ultrasound examination and blood tests. To carry out diagnostics, all personal data of a woman are taken into account (from age, weight, presence of chronic diseases to bad habits). Blood is taken from her vein and an ultrasound is performed.
Determination of embryo viability
To assess the viability of the embryo, it is very important to look at the heartbeat in the early stages. A small person’s heart begins to beat already in the fifth week of being in the mother’s womb, and it can be detected using 1st trimester screening (ultrasound standards) as early as seven weeks of the fetus’s life. If at this time a heartbeat is not detected, we can talk about the likelihood of intrauterine fetal death (frozen pregnancy).
To assess the viability of the embryo, the heart rate is also taken into account, which normally ranges from 90 to one hundred and ten beats per minute at a period of six weeks. These important indicators of 1st trimester screening, ultrasound standards, together with the study of blood flow and body length, must correspond to the reference data for the duration of pregnancy.
The more modern equipment is used for examination, the better you can see all organs and get the most accurate results. If there is a high probability of congenital defects or genetic developmental abnormalities, then the pregnant woman is sent for a more in-depth examination.
In some regions, when registering with antenatal clinics, 1st trimester screening is mandatory for all pregnant women. Ultrasound standards may not coincide with the results obtained, so doctors immediately take the necessary measures to preserve the life and health of the child or mother. But most often, pregnant women who are at risk are referred for such an examination: these are women from thirty-five years of age, those who have genetic diseases in their family and previously born children, had miscarriages in previous pregnancies, stillborn children or non-developing pregnancies. Close attention is also paid to expectant mothers who suffered viral diseases at the beginning of pregnancy, are taking dangerous medications or are under the influence of radiation.
If a woman has spotting in the first trimester, then an ultrasound makes it possible to determine the degree of viability of the child or its death.
Explanation of screening indicators
The screening determines:
- size of the coccygeal-parietal part (CTP);
- biparietal head size (BSD);
- collar space thickness (TNT);
- heart rate (HR);
- state of plasma protein (PAPP-A).
What pathologies are detected at the first screening?
Thanks to a set of procedures, deviations are identified:
- genetic diseases (Down syndrome, Patau syndrome, Edwards syndrome);
- physical development of the fetus;
- location, which allows to exclude ectopic pregnancy;
- predisposition to spontaneous miscarriage;
- exact gestational age;
- defects in the development of the nervous system;
- umbilical hernia;
- predisposition to heart disease;
- condition, location of the placenta.
The main purpose of the study in the first trimester of pregnancy is to identify chromosomal abnormalities.
Sometimes the results may be incorrect or inaccurate, this happens rarely, sometimes the human factor affects. The following reasons may influence the outcome:
- diabetes mellitus in a woman in labor;
- multiple pregnancy;
- screening too early or too late;
- overweight woman;
- if IVF is used to conceive, then the protein A value will be below normal;
- stress, severe anxiety;
- progesterone-based medications.
Should you worry if the placenta is prolapsed?
An ultrasound shows the location of the placenta.
This is an important organ that grows simultaneously with the development of the fetus, providing it with nutrients, microelements, and oxygen. Incorrect placement can block the exit from the internal os of the uterus and disrupt the child’s nutrition. In the first trimester, such presentation is not dangerous. Most often, as the placenta grows, it migrates. But the patient must be under regular monitoring so that the abnormal location does not harm the child and the expectant mother.
The position of the placenta is monitored at 16, 25, 34 weeks of pregnancy. If an organ abnormality is observed, the organ is checked more often.
Parameters of the fetus and uterus
RAPP-A standards:
| A week | PARR-A, IU/l |
| 9 | 357-597 |
| 10 | 648-1030 |
| 11 | 1108-1674 |
| 12 | 1785-2562 |
| 13 | 2709-3692 |
If PAPP-A levels are high, the ultrasound result is negative, and the protein content is low, then there may be problems:
- abnormalities of the fetal nervous system;
- threat of spontaneous miscarriage;
- frozen pregnancy;
- conflict of Rh factors of the child and mother;
- risk of premature birth.
Ultrasound indicators:
| A week | KTE, mm | TVP, mm | BPR, mm |
| 11 | 34-50 | 0,8-2,2 | 13-21 |
| 12 | 42-59 | 0,8-2,5 | 18-24 |
| 13 | 51-75 | 0,8-2,7 | 20-28 |
Uterus:
- in the eighth, ninth week of pregnancy - 8-9 centimeters;
- sixteenth, seventeenth - 14-19 centimeters.
If the height of the uterus is greater than normal, there is a high probability of multiple pregnancy.
In the opposite case, the indicators indicate abnormal fetal position, oligohydramnios and low development. Perinatal screening examination is important for the expectant mother and child.
A complex of modern procedures allows early detection of pathologies and diseases. This allows for timely elimination or adjustment of treatment. Doctors recommend not to ignore screening; this guarantees the correct development of pregnancy and a positive delivery.
Dates of pregnancy
An additional examination to determine the exact date of pregnancy is indicated for women who have an irregular menstrual cycle or do not even know approximately the date of conception of the child. For this, in most cases, 1st trimester screening is used. Ultrasound standards, deciphering the main indicators and dates of conception do not require special medical knowledge. The woman herself can see the expected date of birth, gestational age and number of embryos. Basically, the number of weeks determined by ultrasound corresponds to the period that is calculated from the first day of the female cycle.
While conducting the study, the doctor takes control measurements of the size of the embryo. The specialist compares the 1st trimester screening standards with the data obtained. Ultrasound interpretation occurs according to the following parameters:
- measuring the distance between the sacrum and the crown of the embryo (7-13 weeks), making it possible to determine the real gestational age using special tables;
- measuring the length of the parietal bone of the unborn child’s head (after 13 weeks), this is an important indicator in the second half of pregnancy;
- determining the size of the longest - the femur of the embryo's body, its indicators reflect the child's growth in length (at 14 weeks), in the early stages it should be approximately 1.5 cm, and by the end of bearing the child it will increase to 7.8 cm;
- measurement of the child’s abdominal circumference – indicates the size of the embryo and its estimated weight;
- determination of the head circumference of a maturing fetus, which is also used to predict the natural birth of a child. This measurement is carried out in the last stages of pregnancy, according to which the doctor looks at the size of the small pelvis of the expectant mother and the child’s head. If the head circumference exceeds the parameters of the pelvis, then this is a direct indication for a cesarean section.
Interpretation of ultrasound screening results: indicators, norms
The final stage of a screening ultrasound examination is deciphering the protocol, after which the data is analyzed and compared with the norm. Initially, during an ultrasound, the doctor finds out whether the pregnancy is singleton or multiple. In the second case, the diagnosis shows exactly how many fruits are developing, in one fertilized egg or in different ones.
The ultrasound screening protocol contains information about the location of the embryo, namely which part of the body is directed towards the birth canal. At the 12th week of pregnancy, any presentation of the fetus, even diagonal placement, is considered normal.
This indicator becomes important at 32 weeks. By this period, the child should take the desired position - head down. Deviation from the norm is the impetus for the beginning of medical action - a change in the presentation of the fetus.
The ultrasound screening protocol performed at 12 weeks contains data on the size of the child. After interpreting such important indicators, the doctor draws conclusions about the correct course of pregnancy and fetal development. The ultrasound screening procedure will provide reliable information if it is interpreted by a qualified specialist.
In the process of analyzing the obtained indicators, the doctor is guided by the following standards:
- The height of the fetus should reach 8.2 cm;
- The weight value varies from 17 to 19 grams;
- The collar area is characterized by a value from 0.71 to 2.5 mm;
- The head size should be within 21 mm;
- From the parietal zone to the coccyx, the length of the fetus should be in the range from 43 to 73 mm. CTE is one of the most important indicators when establishing the exact gestational age;
- The femoral part of the leg is characterized by a length of 7 to 9 mm.
In addition to the above indicators, the doctor takes into account other measurements, such as head circumference, shoulder length, diameter and circumference of the abdomen, and heart size. These values are especially significant if there are deviations from the norm in the size of the fetus. Then the doctor assesses the uniformity of fetal growth.
The presence of small deviations from the norm to a lesser extent is not considered a developmental pathology. If an ultrasound shows the small size of the fetus relative to standard indicators, then the reason for this is not necessarily developmental delay. This can be explained by an incorrectly determined gestational age, as well as heredity.
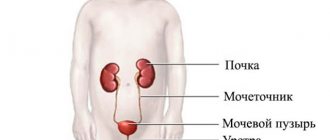
When interpreting a screening ultrasound examination performed during the 12-week period of pregnancy, the doctor also pays attention to such parameters as the quantity and quality of amniotic fluid. Any deviations from the norm, both upward and downward, may indicate infection of the expectant mother, as well as disturbances in the functioning of the fetus’s kidneys or its central nervous system. The presence of a cloudy shade is considered a deviation from the norm and indicates that the expectant mother has become infected with an infectious disease.
Based on the results of ultrasound screening at 12 weeks, the condition of the placenta and its attachment site (anterior, posterior walls of the uterus or its fundus) are assessed. If the internal os is completely or partially closed by the placenta, a cesarean section is performed at the required time.
It is possible to establish the fact that the placenta is low attached (7 cm or less from the pharynx) only through ultrasound screening. If this happens at 12 weeks, the expectant mother is prescribed a quiet regimen. If the placenta is leveled by 36 weeks, there is no need for a caesarean section.
The normal maturity of the placenta by 12 weeks should be zero. During this period of pregnancy, the placenta may contain calcifications, which is acceptable and considered normal.
If, during an ultrasound screening at 12 weeks, the doctor discovers that the placenta is in the process of partial or complete death, the pregnant woman needs urgent treatment.
At the time of screening ultrasound, the cervix is measured. According to the norm, its length should be at least 3 cm. If the figure is reduced (2 cm or less), the expectant mother is prescribed hospitalization and bed rest. If the deviation from the norm is large, then surgical intervention occurs as prescribed by the doctor.
A pregnant woman at 12 weeks should not feel the tone of the uterus, which manifests itself in the form of pain in the lower abdomen and its stiffness. The presence of hypertension, confirmed by ultrasound screening, is a threat to bearing a child. In this case, the expectant mother is hospitalized or treatment is prescribed at home.
Upon completion of the ultrasound examination, data on the embryo’s brain and the symmetry of its hemispheres is also deciphered. Normally, the appearance of the brain on an ultrasound machine resembles butterflies. When carrying out the first screening using ultrasound, the doctor receives the gestational age and PDA calculated by the device.
At the moment when an ultrasound screening examination of the fetus occurs at 12 weeks, the specialist may be suspicious of the following points:
- The nasal bone does not correspond to the norm in size, but is smaller than it or is not determined at all;
- There is no clear outline of the face;
- The second umbilical artery is absent;
- A hernia in the navel area is displayed;
- Heart rate is lower or higher than normal.
Definition of malformations
Using ultrasound in the first weeks of pregnancy, various problems in the development of the child are identified and the possibility of treating it before birth. For this purpose, an additional consultation with a geneticist is scheduled, who compares the indicators obtained during the examination and the screening norms of the 1st trimester.
An ultrasound scan may indicate the presence of any malformations in the child, but the final conclusion is given only after a biochemical study.
What screening tests should be taken during pregnancy?
An ultrasound should examine the thickness of the nuchal translucency (nuchal translucency).
Its coefficient, if it exceeds 2-2.5 cm, indicates the possible presence of Down syndrome in the child. TVP is measured at strictly limited periods of pregnancy - from 11 to 14 weeks, more precisely - up to 12 weeks. Later, the fetus will grow up and the TVP indicators will lose their information content.
In the first trimester, blood is donated for the hormones b-hCG and PAPP-A.
The second screening (16-18 weeks) does not include an ultrasound scan - the indications for it are taken from the first. And blood must be donated for the hormone b-hCG, the alpha protein AFP and estriol - that is, the so-called “triple test”.
1st trimester screening, ultrasound norms: nasal bone
In an embryo with chromosomal abnormalities, ossification occurs later than in a healthy one. This can be seen as early as 11 weeks, when the 1st trimester screening is carried out. Ultrasound standards, the interpretation of which will show whether there are deviations in the development of the nasal bone, help the specialist determine its size starting from 12 weeks.
If the length of this bone does not correspond to the gestational age, but all other indicators are in order, then there is no reason to worry. Most likely, these are the individual characteristics of the embryo.
Timing of the second screening during pregnancy
A secondary comprehensive study is carried out to determine the likelihood of the formation of chromosomal abnormalities in the fetus: at this time their probability is quite high.
There are three types of second screening:
- ultrasound (detection of abnormalities using ultrasound),
- biochemical (blood parameters),
- combined, where the first two are used.
An ultrasound is usually performed as a screening test at the end of the second trimester and consists of a blood test for various signs.
The results of the ultrasound examination, which was carried out earlier, are also taken into account. The system of sequential operations during this set of studies is as follows: after blood is donated and an ultrasound examination is performed, the woman fills out a questionnaire indicating personal data, which will be used to determine the duration of pregnancy and the likelihood of developing defects. When taking into account the duration of pregnancy, tests are performed. After this, the information received is processed by a computer program to calculate risks. However, even the results obtained cannot be considered a final diagnosis, an absolute guarantee of the presence of risk, if it is established. To obtain more accurate and detailed information, the pregnant woman is sent to undergo additional tests and consults with a geneticist. Second screening during pregnancy
is a biochemical study of the blood of the expectant mother using certain tests.
More precisely, according to the so-called “triple test”, which studies the level of proteins and hormones, such as: human chorionic gonadotropin (hCG) in the blood, alpha-fetoprotein (AFP), free estyrol. The test becomes “quadruple” when this secondary set of studies also involves taking blood to determine the level of inhibin A.
Studying the concentrations of these hormones and proteins in the blood makes it possible to judge with a high degree of probability the possibility of a child developing Down syndrome, Edwards syndrome, and neural tube defects.
The conclusions of a repeated set of studies may be an indirect indicator of the defective state of the child’s formation and exacerbations of the course of pregnancy. For example, an abnormal level of hCG indicates abnormalities in chromosomes, the danger of the formation of preeclampsia, or the presence of diabetes mellitus in the expectant mother.
Reduced hCG levels may indicate disturbances in the development of the placenta.
Increased or decreased AFP and inhibin A in the blood serum of a pregnant woman is a sign of a disorder in the natural formation of the baby and possible congenital anomalies - open neural tube defects, possibly Down syndrome or Edwards syndrome. If alpha-fetoprotein increases sharply, the fetus may die. If the level of the female steroid hormone, free estriol, changes, the activity of the fetoplacental system can be disrupted: its deficiency suggests probable abnormal functioning of the child.
If the results of a repeated set of studies turned out to be unfavorable, you should not worry ahead of time. They only talk about the estimated risks of deviations, they do not constitute a final diagnosis. In the case where at least a single component of the secondary screening does not fit into the norm, it is necessary to carry out additional research. The indicators of a screening study may be influenced by several reasons: in vitro fertilization, a woman’s weight, the presence of diabetes mellitus, bad habits, such as smoking.
Determining the location of the placenta
The baby's place (placenta) is necessary for the intrauterine blood supply of a small person. It is needed to provide him with food. Ultrasound makes it possible to determine abnormalities in the development and position of the placenta. If it is located too low relative to the fundus of the uterus, this is called placenta previa, which can lead to blocking the exit for the baby during labor.
A 1st trimester screening ultrasound can show the location of the baby's place well. The norms of such research reject low placenta previa. But even if it is located close to the fundus of the uterus, doctors are in no hurry to sound the alarm, since it may rise as pregnancy progresses. But if the position of the placenta has not changed in the later stages, then the following problems are possible:
- the placenta can obscure the cervix and prevent natural childbirth;
- Since the lower part of the uterus stretches in the second trimester, the placenta can detach from it and cause severe bleeding (placental abruption).
Who needs to be screened in the 1st trimester?
Early detection of possible deviations contributes to the timely adoption of measures to prevent possible complications of gestation and other negative consequences. Screening studies are recommended for all pregnant women, regardless of age, the presence of sick or healthy children. Those deviations that can be detected during one screening sometimes form spontaneously, without any connection with relatives, parents or lifestyle.
But if a mother refuses screening diagnostics, then she should take into account that these studies are important for everyone, and especially for certain groups of patients. Who is not recommended to refuse screening of the first stage of prenatal development?
- If maternal age exceeds 35 years, which is associated with a high risk of chromosomal abnormalities due to the onset of aging processes.
- If during the first gestational trimester the patient suffered from infectious pathologies such as ARVI, influenza, etc.
- If the mother was forced to take drugs that are prohibited in the first trimester or was treated with dangerous medications shortly before conception.
- If the patient has unhealthy habits such as smoking, drug addiction or a tendency to abuse alcohol.
- If the mother has deviations from the norm, threats of spontaneous termination of gestation or frozen pregnancy, recurrent miscarriage, non-developing pregnancy, etc.
- If the patient or the baby's father has genetic abnormalities, or during previous pregnancy the patient was at high risk of genetic abnormalities. If there are already children with abnormalities of chromosomal origin or the mother herself has serious pathologies.
- If conception was the result of sexual contact with a blood relative.
The screening test does not pose any threat to the fetus or the pregnant woman, so refusing it is pointless, or at least unreasonable. After all, such diagnostic measures can detect violations that can be easily corrected at such an early stage. A biochemical screening test is carried out at the antenatal clinic at the patient’s place of residence absolutely free of charge.
Yolk sac examination
On the 15-16th day of pregnancy from the day of conception, the process of formation of the yolk sac begins. This “temporary organ” of the baby is examined by doing an ultrasound (1st trimester screening). The timing and standards for ultrasound examination should indicate its presence and size. If it has an irregular shape, is enlarged or reduced, then the fetus may have frozen.
The yolk sac is an appendage that is located on the ventral side of the embryo. It contains a supply of yolk necessary for the normal development of the baby. Therefore, checking what the norm is for ultrasound screening in the 1st trimester in comparison with the study parameters is very important for monitoring the progress of pregnancy. Indeed, at first (until the child’s organs function independently), this appendage performs the function of the liver, spleen, and is also used as a supplier of primary germ cells, which are actively involved in the formation of immunity and in metabolic processes.
How is an ultrasound examination performed at 12 weeks?
Diagnosis, carried out at the 12th week of pregnancy, can occur in two ways: transabdominal, by driving a sensor along the expectant mother’s belly, and transvaginal, by inserting a sensor into the vagina.
In some cases, in order to obtain a complete picture, diagnosis is carried out using two types of studies.
According to experts, if the first ultrasound screening occurs transvaginally, the results of the study will be more accurate. But this method does not eliminate the risk of infection and damage to organs such as the vagina and cervix.
Most often, screening ultrasound examination at 12 weeks is carried out using the transabdominal method. The second type of study is used only in certain cases: if the uterus is located deep enough or the pregnant woman is overweight (excessive fatness interferes with the process of establishing important indicators of fetal development by moving the sensor across the abdomen).
The duration of the procedure can be a minimum of 10 and a maximum of 30 minutes.
The role of biochemical blood test
When examining the condition of the embryo, the doctor looks not only at the results of ultrasound (1st trimester screening). The norms in it are just as important as in a blood test. Such an analysis, in addition to an ultrasound examination, is carried out to determine at what level specific proteins (placental) are located. The first screening is done in the form of a double test - to detect the level of 2 protein types:
- "PAPP-A" - the so-called pregnancy-associated plasma protein A.
- “HCG” is the free beta subunit of human chorionic gonadotropin.
If the levels of these proteins are altered, this indicates the possible presence of various chromosomal and non-chromosomal disorders. But identifying an increased risk does not mean that there is definitely something wrong with the embryo. Such results of screening of the 1st trimester, interpretation, ultrasound normal indicate that it is necessary to more closely monitor the progress of pregnancy. Often repeated testing no longer shows the risk of genetic diseases.
Screening test results
You must wait about three weeks for results.
Analysis indicators are expressed not in numbers, but in MoM, which means multiplicity in medicine. The median is the statistical average for the given marker. According to the norm, MoM should be within the range of 0.5-2.0. If, based on the tests, a deviation from the norm is revealed, it means that there is some pathology in the development of the fetus. Elevated hCG may indicate the following abnormalities: chromosomal developmental defects, multiple births, Rh conflict. Reduced hCG indicates an ectopic pregnancy, threatened miscarriage, or undeveloped pregnancy. An increase or decrease in AFP indicates probable chromosomal abnormalities. The sum and combinations of deviations in the proportions of hormones can also indicate the presence of pathologies. Let's say that in Down syndrome, the AFP indicator is underestimated, and hCG, on the contrary, is overestimated. The hallmark of an unclosed neural tube is increased levels of alpha protein (AFP) and decreased levels of the hormone human chorionic gonadotropin (hCG). In Edwards syndrome, the test hormones are reduced.
What is ultrasound screening and biochemistry of maternal serum
The first screening is carried out between 11 and 14 weeks after the baby is conceived. The main objective of the method is to check the fetus for the presence of any developmental pathologies.
This type of testing even reveals complications in pregnancy that the expectant mother might not have suspected due to the absence of symptoms, good health, etc. This test is not always performed on pregnant women; other groups of people often undergo it.
For example, screening a group of children of the same age - the technique allows us to identify characteristic diseases for this age. Since it is usually prescribed only three times, women are scared if a specialist refers it for additional screening.
There is no reason to panic, because doctors refer for additional examination not because a pathology has been detected, but because there is a risk of its development. For example, screening is often prescribed for women over 35 years of age if family members have pathologies, if there was a frozen pregnancy or miscarriage in the past, etc.
What can distort the result
False positive results occur in the following cases:
- Artificial insemination.
- Excess weight increases the concentration of all hormones, while lack of weight decreases it.
- During multiple pregnancy.
- For diabetes mellitus.
- Even stress and fear of the procedure can affect the result, so you need to carry out the procedure in a calm state.
The doctor will explain to you all the normal indicators and tell you who to contact if something is wrong
Who is the examination recommended for?
Order No. 457 Min. Healthcare R.F. from 2000 says that screening examinations should be carried out for all pregnant women. Every woman has the opportunity to issue a refusal. However, such an act can only speak of the illiteracy of the expectant mother and indicate a negligent attitude towards her baby.
How many risk factors are there that are considered a reason for mandatory prenatal screening? The main reason for the examination is:
- age criterion: 35+;
- ending of previous pregnancies with miscarriage or fetal death;
- occupational hazards;
- diagnosing chromosomal pathologies in the fetus during a previous pregnancy or the birth of a child with intrauterine malformations;
- infectious diseases suffered at the beginning of pregnancy;
- taking medications prohibited for pregnant women;
- alcoholism, drug addiction;
- diseases transmitted by heredity, both in the family of the mother and in the family of the child’s father;
- close family ties between the baby’s parents.
Who needs screening
Some women believe that if they feel well, it is not necessary to undergo screening during pregnancy, especially since not all pregnant women register with a gynecologist in the first trimester. Thus, women especially at risk may give birth to a baby with physical and/or mental developmental disabilities. After all, if a chromosomal mutation is not detected in the early period of gestation, then the disease itself will not go away, and embryogenesis will further go along the wrong path and the moment will come when it is not possible to correct anything.
Therefore, regardless of the well-being of the pregnant woman, her age, the birth of previously healthy children, the presence of excellent living and nutritional conditions, screening during pregnancy is recommended at all stages of gestation. Even with a woman’s good health and unburdened heredity, deviations in embryogenesis can still occur. Despite this, a pregnant woman can refuse to be examined; no one will force her to undergo diagnostics.
Particular attention to screening during pregnancy should be paid to women at risk:
- expectant mothers 35 years of age and older, even if they have already given birth to healthy children. After this age period, the body begins to age, processes are launched in which the likelihood of chromosomal abnormalities in the fetus increases;
- a history or identification of signs of a frozen or ectopic pregnancy, miscarriage, risk of spontaneous miscarriage, premature birth;
- ARVI or other infection at the beginning of the gestational period;
- chronic infectious process, sluggish infectious diseases;
- stillborn children in the family or children with chromosomal abnormalities;
- close blood relatives of future parents who have been diagnosed with a genetic disorder;
- taking various medications, vaccinations, anesthesia for surgery immediately before conception and at the beginning of gestation;
- conception as a result of incest or violence;
- smoking, alcohol abuse, drug use;
- Rhesus conflict.
Screening during pregnancy does not pose any danger to the expectant mother and child, so research from the examination is unreasonable.
Baby development at 12 weeks
Many of the baby’s main organs have already developed, while some small structures continue to form. On average, a child's height is 80 mm and weight is approximately 20 grams. Doctors also note that the fetus has the following characteristics:
- heart rate is more rapid than in the third trimester and can be approximately 170 beats per minute;
— the child’s face no longer looks like a tadpole, but takes on human features;
- you can see eyelids, lobes, a little vellus hair (at the site of formation of eyebrows and eyelashes);
- most of the muscles have practically already developed, so the fetus moves all the time, and the movements are mostly involuntary and rather chaotic;
- the baby grimaces and clenches his hands into fists, you can see marigolds on his fingers;
- the child has already developed kidneys and almost formed intestines, red and white blood cells are observed in the blood;
— both hemispheres of the brain are fully formed, but the spinal hemisphere still “commands”;
- you can see who it is: a boy or a girl, but since the fetus does not always lie the way the mother and doctors want, you can make a mistake, so they speak more accurately about the sex at the 16th week.
How to properly prepare for an examination
No special preparation is required before the first screening during pregnancy. Mommy should come to the hospital at the designated time. Do not worry, as negative emotions can affect the reliability of the results.
Reviews indicate that the procedure is absolutely painless and cannot harm mother and child. Before donating blood, you should not eat or drink various drinks. No special diet required. You can only drink plain water, no more than one glass.
Why is an ultrasound performed at 12 weeks?
The peculiarity of the first 12 weeks of pregnancy is that during this period all the main organs and systems of the baby are formed, but the fetus is not yet protected by the placenta from the influence of negative factors coming from outside.
An ultrasound at week 12 shows how the baby is developing and whether its parameters correspond to the gestational age. However, the main goal of the study is to identify developmental disorders. At this stage, genetic abnormalities can be detected.
Ultrasound also allows you to record:
- location of the fetus in the uterus;
- number of expected babies;
- condition of the placenta and reproductive organs of the mother;
- placenta attachment site;
- quantity and quality of amniotic fluid;
- successful pregnancy;
- expected date of birth.
If a woman does not know the exact date of her last menstruation (for example, with an irregular cycle), ultrasound can determine the gestational age with great certainty.
As already mentioned, the first screening makes it possible to see abnormalities in the development of the fetus, so that the mother can make a decision about the further fate of the pregnancy. If serious abnormalities are detected, doctors may interrupt the pregnancy process. Early diagnosis reveals the following fetal pathologies:
- disorders in the formation of the nervous system;
- Down's disease;
- Patau syndrome;
- Shereshevsky-Turner syndrome;
- Brahmann-Lange disease;
- Edwards disease.
Monitoring the condition of the placenta, uterus and intrauterine fluids is also important. If deviations are detected, treatment is prescribed to allow the woman to maintain the pregnancy and bear a healthy baby.
First trimester screening
As already written above, it is carried out no earlier than the eleventh, but no later than the thirteenth week. It is during this period that the so-called embryonic period of fetal development ends, and the fetal period begins.
This means that the embryo turns into a fetus, and organs begin to develop, like those of a full-fledged human being. During this period, pathologies or abnormalities can be identified.
Of course, only a specialist will correctly interpret the screening results, but expectant mothers can at least learn in general terms what to expect and what some indicators may mean.
Who is referred for first trimester screening?
You can refuse screening, but doctors do not advise it
All pregnant women are referred, but this procedure can be refused. Doctors do not recommend refusing, as this is a negligent attitude towards the baby’s life. The following groups of women should also be examined:
- over 35 years old;
- there were unsuccessful attempts to give birth - a frozen fetus, a miscarriage;
- those who work in production and may come into contact with harmful substances;
- who gave birth to a child with disabilities in the past;
- during the first weeks, those who had an infection;
- taking medications prohibited for the first trimester;
- those suffering from alcoholism or drug addiction;
- when there is a threat of miscarriage;
- if there are pathologies in the family.
How the study is performed
There is a special medical worker - a sonologist, who carries out the procedure. At this time, there are two options - abdominal and transvaginal examination. They prefer the second one, as it is more reliable.
There are machines for home ultrasound
The woman is asked to undress to the waist and lie on the couch with her legs bent. Then a thin sensor in a condom is inserted into the vagina. It will be moved to fully examine the fetus, this may cause discomfort, but not pain. After the procedure, some discharge may appear on the underwear, perhaps a little bloody.
This is normal, no need to worry. Ultrasound of the abdominal area does not give reliable results at this stage, but if it is chosen, the woman is asked to lift her clothes to expose her stomach. Then you will have to wait for the results - in public hospitals for up to five days. After this, you need to donate blood for analysis.
Cost of 1st trimester screening
It is known that not even all government agencies are ready to provide such a service free of charge. Blood biochemistry alone exceeds one and a half thousand rubles, and you also have to pay for the ultrasound procedure itself. Each clinic sets the cost differently, but it is unlikely to be less than two thousand rubles.
Preparing for an ultrasound
At 12 weeks, the fetus is still small, so it is necessary to exclude all factors that interfere with visualization of the uterine cavity during the study. Since during this period the uterus has not yet risen high enough, gases accumulated in the intestines may prevent its examination. To eliminate them, you must stop consuming the following for 2 days before the study:
- smoked, canned, fried and fatty foods;
- seafood;
- cabbage;
- legumes and soybeans;
- peas;
- flour;
- white bread;
- sweets.
If on the eve of the examination there is a feeling of gas accumulation in the abdomen, the woman can take Espumisan. This drug is harmless to the fetus and quickly eliminates gas formation in the intestines.
Ultrasound at 12 weeks is performed using 2 methods: transvaginal and transabdominal. The second method requires that the patient's bladder be full. To do this, half an hour before the procedure you need to drink 500 ml of water or not empty your bladder for 2-3 hours. You need to bring your own diaper to the ultrasound room. Some clinics also require disposable gloves.
What should I show?
Thanks to the first screening, the expectant mother and the doctor will know exactly how the baby is developing and whether he is healthy.
Biochemical analysis of the 1st screening during pregnancy has certain indicators:
- HCG norm - detects Edwards syndrome when the levels are below the established values. If they are too high, then the development of Down syndrome is suspected.
- Plasma protein (PAPP-A) , the value of which is below established standards, indicates the fetus’s propensity for diseases in the future.
An ultrasound examination should show:
- how the fetus is positioned to eliminate the risk of ectopic pregnancy;
- what kind of pregnancy: multiple or singleton;
- whether the fetal heartbeat corresponds to developmental norms;
- embryo length, head circumference, limb length;
- the presence of external defects and disorders of internal organs;
- thickness of the collar space. With healthy development, this corresponds to 2 cm. If compaction is observed, then pathology is likely;
- condition of the placenta to eliminate the risk of dysfunction.
| Diagnostics | Gestation period | Indicators | Meaning |
| Ultrasound examination of the fetus. Depending on the intrauterine location, the following is carried out: - through the skin; - transvaginally. | From 10 to 14 weeks | The coccygeal-parietal size shows the maximum distance from the back of the head to the tailbone of the fetus. | Allows you to accurately determine the duration of pregnancy and confirm the presence of pathology. |
| The thickness of the collar space (neck fold in which fluid accumulates). | What matters is not the actual presence of fluid (all embryos have it), but its quantity. | ||
| Determination of the length of the nasal bone. | If the nasal bone is not visualized and the thickness of the neck fold is increased, then the likelihood of developing Down syndrome is high. | ||
| Heart rhythms. | 147-171 beats per minute. | ||
| Biparietal head size is the distance between the extreme points of the crown in the fetal skull. | Helps determine the presence of fetal pathologies and confirm calculations of the moment of conception. | ||
| Biochemical (hormonal) analysis, in which venous blood of the expectant mother is taken in an amount of 10 ml | From 10 to 13 weeks | Chorionic gonadotropin, which detects pathologies of the placenta, Edwards syndrome and Down syndrome. | A decrease in the level of hCG in the blood during pregnancy or a slowdown in its growth indicates the risk of spontaneous miscarriage or the development of an ectopic pregnancy. |
| Protein A, a protein produced by the placenta. | The interpretation of the 1st trimester screening is indicated in Mohm units. With MoM from 0.5 to 2.5, the indicators are considered normal. |
A comprehensive examination, the results of which are shown by the first screening performed, makes it possible to detect various genetic pathologies. If a serious illness is confirmed that threatens the quality of life and health of the unborn child, then parents are offered to terminate the pregnancy artificially.
To accurately confirm the diagnosis, the woman undergoes a biopsy and puncture of the amniotic membrane to obtain amniotic fluid and examine it in the laboratory. Only after this can we confidently say that the pathology exists, and a final decision can be made about the further course of the pregnancy and the fate of the child.
How does Screening Ultrasound differ from regular ultrasound?
The procedure itself is no different. This can also be done using a sensor. Screening ultrasound is performed for early detection of fetal pathologies at a specific stage of pregnancy. If deviations are found, it is necessary to find out whether treatment is possible.
In other cases, an ultrasound may be prescribed to confirm or refute the diagnosis. It is also possible to conduct additional research at the request of the parents if during routine screening it was not possible to determine the sex of the child.
Factors influencing the development of chromosomal pathologies
Of course, biochemical and physical markers of chromosomal pathology make it possible to predict with a high degree of probability the risk of having a child with abnormalities. However, women who are just planning to have a child often think about preliminary factors that may influence the development of such deviations. There is a very good reason for concern, because according to statistics, for every 700-800 children, 1 child is born with Down syndrome.
To a certain extent, chromosomal mutations are influenced by heredity. For example, if the husband had relatives with Down syndrome in his family, the risk increases slightly. Although it has been precisely established that there is no direct transmission of the disease from generation to generation. Moreover, if a married couple gives birth to a sick child, they may well give birth to other healthy children. The risk, of course, increases, but is not absolute. Another interesting pattern is also observed. For example, if one of the identical twins is sick with diabetes, then the second one is also sick. But if the twins are dizygotic, then, as a rule, only one child is susceptible to the chromosomal mutation.
Scientists have also found that the risk increases if there is some serious disease in the family that is inherited. There is a pattern according to which diabetes mellitus, inherited, increases the risk of having a child with diabetes.
The age of the mother also greatly influences the possible birth of a child with chromosomal abnormalities. Therefore, doctors recommend having children as early as possible. After 42 years of age, the risk increases many times over. However, newborns with Down syndrome are also found in 20-year-old women in labor. The age of the father may also increase the likelihood of anomalies to a certain extent. Usually, if the total age of the couple exceeds 70 years, then during pregnancy it is worth undergoing a full examination for the presence of markers.
Radiation radiation, serious illness during pregnancy, and experiences can affect the birth of children with diabetes.
Of course, geneticists cannot determine the exact factors influencing the birth of children with disabilities. And it is unlikely that a woman who sincerely loves a man will refuse to conceive with him because of some genetic disease. But it is quite possible to try to have a child at an earlier age, before the age of 35.
What to do if you have unfavorable results
If the patient’s biochemical screening results show an increased likelihood of giving birth to a baby with severe anomalies, then it is extremely important for the mother not to become hysterical. Maintaining sobriety and clarity of mind as much as possible. It is necessary to understand how important it is to obtain accurate data about the baby’s pathology. If the importance is critical, then further examination is necessary to accurately confirm the diagnosis. To do this, mommy needs to make an appointment with a genetic specialist.
To be sure of the presence of genetic abnormalities, the specialist prescribes an invasive procedure, provided that the risk of having a sick child is very high - 1:100 or so. Before the 13th week, a biopsy of chorionic villi is performed. If there are serious risks, then it is better to undergo just such a procedure. Since other diagnostics that reveal the fetal genotype are carried out at a very late date.
Biochemical screening is by no means considered a mandatory procedure, but it is recommended for all patients in an interesting situation. Such a diagnostic study will help to detect probable abnormalities, which will allow timely termination of pregnancy (if absolutely necessary, when it is known for sure that the baby has severe genetic problems) or take measures to prevent abnormalities through competent, safe therapy.
Are there any standard indicators?
Of course there is! You can find out about them by doing studies such as ultrasound, screening (12 weeks). The norm will become known after the doctor examines the data. However, there are average medical indicators that are clearly established for each week of pregnancy. For example, β-hCG at 11-12 weeks should be from 200,000 to 90,000 mU/ml.
However, it should be borne in mind that screening of a 12-week pregnancy gives, of course, very high, but still not one hundred percent results, because each woman has her own body characteristics, which must be taken into account by the doctor. If there is more than one fetus, then it is more difficult to diagnose. They look at the indicators. If they are one and a half or two times larger, then we can conclude that there are 2 or more embryos. Each fetus has its own chorion and different hormone production. That is why the indicators are so high, and the expectant mother is sent for an ultrasound to confirm a multiple pregnancy.
As soon as the screening is carried out (12 weeks), the normative values are immediately checked against the data obtained in order to calculate whether there are any pathologies. For these purposes, doctors use a special coefficient called MoM. It is calculated using a certain formula: the amount of the hormone that was determined based on the screening results is divided by hCG (corresponding to the norm during this period of pregnancy). The result should be one (this is ideal). Well, based on the results of all the studies, they judge whether to include the expectant mother in the risk group with chromosomal abnormalities or not. It is worth noting that even if this suddenly happened, this is not a final verdict, but only one of the probabilities. Therefore, other indicators are compared and only after that some conclusions are drawn. They review the entire screening of a 12-week pregnancy: ultrasound, hormones, TVP, and may prescribe a repeat study in the second trimester.
The PAPP-A protein is responsible for the immunity of the pregnant woman, and it also helps the placenta work. Since the threshold boundaries are clearly established, its deviations are extremely undesirable. The thing is that such “jumps” in indicators indicate not only a possible miscarriage, but also such terrible anomalies as Down syndrome, de Lange syndrome, etc. The following numbers are considered normal: from 11 to 12 week - 0.7-4.76; from the 12th to the 13th week - 1.03-6.01.
What is a screening examination and what does it include?
Screening is a set of medical procedures aimed at identifying and preventing the development of various diseases. This examination is carried out not only for women expecting babies, but also for other segments of the population.
Perinatal screening is carried out three times throughout the pregnancy and includes:
- Ultrasound, which helps to see how the baby develops in the womb.
- Taking venous blood to determine the level of the hCG hormone and PAPP-A protein.
How is the examination carried out?
The first screening during pregnancy, how it is done, is decided by the doctor based on the specified gestational age. Contact of the sensor with the body is facilitated using a special glycerin-based gel, which is applied to the skin. The uterus with the existing amniotic fluid actively conducts sounds.
This allows you to study the development of the fetus, listen to its heartbeat, and record pathologies of organs and systems. The awkward position of the fetus in the uterus can make a comprehensive examination difficult. In this case, the woman needs to provoke the child to change position with light active movements.
The examination is carried out in 2 stages:
Ultrasound examination:
- Transabdominal method of procedure. It is absolutely painless, but not accurate enough.
- Transvaginal method. It does not require special preparation, a full bladder. However, gas-forming foods should be avoided. The examination of the fetus and uterus is of better quality than the transabdominal method, since it is performed inside the woman’s body. The downside is the discomfort when inserting the sensor into the vagina.
Test for hormones hCG, PAPP-A. If high risks of fetal pathology are detected, additional examination of amniotic fluid and placental cells is prescribed.
Should I do it?
The first perinatal screening is recommended by the Ministry of Health for all pregnant women, but is not a mandatory procedure. That is, if the expectant mother refuses tests, doctors will not force her to donate blood or do an ultrasound.
But is it worth giving up? In no case, because such an examination will help warn future parents about possible developmental problems in their baby, such as Down's or Edwards' disease, various defects in the structure of the nervous system and other pathologies that may subsequently lead to the death of the child or his birth with a disability.
Early detection of genetic pathologies will help doctors develop a treatment plan for the baby and, if not completely cure the disease, then at least relieve the symptoms as much as possible.
If the results of the examination reveal fetal pathologies that are incompatible with normal life, then doctors will refer the woman to terminate the pregnancy for medical reasons. It is better to give birth to a healthy child, but later than now to a baby who is not capable of a normal existence.
The following categories of pregnant women are especially recommended to undergo first perinatal screening:
- under 18 and over 35 years old - it is at this age that there is a high probability of miscarriage or the development of congenital defects;
- previously had a history of frozen pregnancy, spontaneous termination (miscarriage) or stillbirth;
- already having children with genetic disorders;
- having hereditary diseases or pathologies in their pedigree;
- working in hazardous industries;
- taking medications dangerous to the fetus (fetotoxic drugs);
- at the beginning of pregnancy, those who have had infectious diseases (including influenza, ARVI);
- having bad habits (alcohol, smoking, drugs);
- became pregnant as a result of a consanguineous relationship.
For the categories of women listed above, undergoing the first perinatal screening is mandatory, since all these factors are likely to cause deviations in the proper development of the child.
For other women, undergoing the first screening is not mandatory, but doctors still recommend undergoing this examination to make sure that everything is fine with your baby.
Are there false indicators during the first screening?
During the first screening, false indicators are sometimes encountered. This is due to the following provoking factors:
- Excess weight in a pregnant woman.
- Tendency to dystrophy.
- Fertilization using IVF.
- Bearing two or more fruits.
- The presence of diabetes mellitus in a woman.
- Threat of miscarriage.
- Incorrect determination of the gestational age of the baby.
- Anxiety during the examination, stress and nervous shock.
It often happens that with an unfavorable prognosis from doctors, a woman gives birth to an absolutely healthy child. This is explained by the imperfection of the technology used for examination and the human factor. When performing a blood test in a laboratory, the quality of the result may be affected by spoiled reagents or violation of the rules for handling biological material.
In some cases, screening gives a negative answer to the presence of various pathologies in the fetus, but the couple ends up with a baby with genetic abnormalities. These cases relate to diagnostic errors and are a real test for parents. When planning a pregnancy, parents should understand the importance of the first screening examination. The procedure is free, painless and affordable.
Detection of chromosomal abnormalities in the fetus in the early stages makes it possible to begin timely treatment or artificially terminate the pregnancy.
When is the first screening carried out and why?
Correctly calculating the gestational age helps determine not only the expected date of birth. It is necessary to plan the first screening. By the beginning of the 11th week, the embryonic period of development ends. Formed organs, limbs, facial bones appear, and the nervous system is formed.
Screening of the first trimester of pregnancy is carried out at the end of the term. The acceptable period for completing the study is 13 weeks and 6 days.
It is useless to carry out screening earlier than these dates: the picture of pathologies may be distorted and will not lead to the detection of pathologies.
Carrying out the procedure
The duration of the procedure is from 10 to 30 minutes. The speed of the procedure depends on the location of the fetus in the uterus, the need to examine the female genital organs, and abnormalities identified during the study.
Before the examination, the specialist fills out a special questionnaire, which includes general information about the mother, the presence of genetic diseases in the family, and the expected date of conception. This information is necessary for subsequent evaluation of the data obtained.
Transvaginal (internal) ultrasound involves examining the mother's genital organs and the uterine cavity by inserting a device sensor into the vagina. Before the procedure, the instrument is treated with an antiseptic and a condom is put on it. To conduct the study, a woman needs to lie on her back and bend her knees slightly.
Transabdominal (external) ultrasound is also performed in a lying position, but the device’s sensor is moved over the pregnant woman’s abdomen. In order to prevent air from penetrating between the skin and the instrument, a special gel is applied to the woman’s stomach. Regardless of the method of implementation, a correctly performed procedure should not cause discomfort to the patient.
The classic ultrasound method is transabdominal. The transvaginal research method is chosen in the following cases:
- If a woman is overweight, folds on the body prevent a high-quality examination through the skin.
- Suspicion of the development of pathologies of the genital organs. If a pregnant woman has signs of inflammation of the appendages, the formation of a cyst in the ovary or fibroids, examination through the skin will not give accurate results.
- Isthmic-cervical insufficiency was diagnosed. Since the vaginal sensor is located closer to the cervical canal, it will allow a better assessment of the degree of development of the pathology.
In some cases, research is carried out in two ways. This is necessary when, during a transabdominal examination, difficulties arise in determining certain indicators. This is possible if:
- the child is positioned in such a way that it is not possible to assess the parameters of the collar zone;
- During the examination, the first method revealed formations in the uterus that were poorly visible;
- it turned out that the placenta or fetal membrane is attached low.
Ultrasound does not harm the baby or the mother, so performing the procedure in several ways is acceptable. After the examination, the woman is given a conclusion with which she must visit a doctor.
Research results: transcript
First of all, when interpreting a screening ultrasound, attention is paid to the location of the fetus to exclude ectopic pregnancy. It is very important to determine the size of the uterus. The general condition of the fetus is assessed. After this, the size of the unborn child is measured, and the condition of the internal organs is assessed (the activity of the cardiovascular system, the location of organs). In addition, at this time it is already possible to find out the gender of the unborn child, although this will not yet be as accurate as possible.
Decoding
To ensure that the assessment of prenatal screening results is error-free, the latest computer programs are used, customized to work in a specific laboratory. Therefore, it is recommended that all screening studies be carried out within the same medical institution. Combined screening has the highest accuracy of predictions, when the results of ultrasound diagnostics are assessed in relation to the biochemistry data of maternal blood serum.
Fresh green salad is a must on the menu.
The indicators of double biochemical screening, which is carried out by a pregnant woman in the first gestational stage, are assessed exclusively in combination. If pathology is suspected, however, an ultrasound examination does not reveal any abnormalities, then the patient is recommended to undergo a repeat biochemical screening examination (if the timing does not interfere), or the examination is postponed for a second screening.
β-hCG
a similar hormonal substance is produced by the chorionic embryonic membrane. It is this hormonal compound that allows you to confirm the fact of conception using home rapid tests. In the first weeks of embryogenesis, β-hCG levels increase, reaching maximum values towards the end of this period. With the onset of fetal development, the hormonal level gradually decreases until approximately the middle of gestation.
At 10 weeks, the norm is 25.7-181.7 ng/ml, at 11 weeks – 17.3-130.2 ng/ml, at 12 – 13.3-128.6 ng/ml, and at 13 – 14.1-114.7 ng/ml. if there is an increase in the content of gonadotropic hormone, then there is a high probability of the fetus having Down syndrome. Also, an increased content of hCG towards the end of embryogenesis can be observed with multiple conceptions, diabetes in a pregnant woman, or with severe toxicosis.
Insufficient levels of chorionic hormone in 10-13 weeks are observed with ectopic gestation, an increased threat of miscarriage, with Edwards disease or with insufficiency of placental functions. Throughout the second half of gestation, gonadotropic chorionic hormone remains at the same level until delivery.
RARR-A
PAPP-A is a plasma protein that the body begins to secrete during pregnancy. It is produced by the outer embryonic layer during the period of penetration into endometrial tissue.
- Pregnancy-associated protein-A is responsible for immune responses during pregnancy, and also controls the full development and functionality of placental structures.
- The study of this protein is incredibly important for the early detection of disorders in the development of the baby. Even in the early stages, when ultrasound examination is not yet able to detect the problem, PAPP-A indicators may already indicate the presence of abnormalities.
- Normally, the content of PAPP-A at 10-11 weeks is 0.44-3.73 mU/ml, at 12-13 – 1.02-6.03 mU/ml, and at 13-14 – 1.46-8 .55 honey/ml.
- If the protein content deviates from the norm, this may indicate Down's pathology, the threat of spontaneous abortion or fetal fading, as well as Cornelia de Lange syndrome or underweight of the baby due to insufficient supply of nutrients.
It is important to undergo biochemical testing for PAPP-A before 14 weeks, since the results will be unreliable at later prenatal development. Protein A levels after 14 weeks in the presence of chromosomal abnormalities in the fetus are the same as in a pregnant woman carrying a healthy baby. Detected deviations of the PAPP indicator from the norm before 14 weeks should be regarded as a cause for alarm. Additional studies may be needed to clarify the diagnosis.
MoM standards
When the doctor receives the results, he calculates the MoM coefficient. This indicator helps determine the presence of deviations from the normal, average value. Typically, the MOM coefficient is about 0.5-2.5, and if the pregnancy is multiple, then up to 3.5. In different laboratory institutions, these indicators sometimes differ, since the level of protein-A and hCG can be calculated in other units. Therefore, the results should be interpreted only with a geneticist or other knowledgeable doctor.
Based on the test results, you can understand and see a lot
Using a special program that necessarily takes into account the pregnant woman’s unhealthy habits, diabetes, obesity, number of fetuses, natural conception, IVF or ICSI and other data, the risk of having a baby with genetic anomalies is calculated. A high risk level is considered less than 1:380.
For example, the conclusion states that the risk is high and amounts to 1:270. This indicator means that out of 270 patients, 1 woman gives birth to a baby with a similar abnormal genetic disorder. But there are situations in which the values differ slightly from normal, but the fetus will not have pathology. These include IVF, obesity, multiple pregnancy, diabetes and other factors.
So, with diabetes or obesity in girls carrying a child, hormones may be noticeably higher than the norm, and when carrying twins (triplets, etc.) or with in vitro fertilization, chorionic hormonal indicators will be increased, and PAPP-A may be at a lower level average.