Small intestinal cancer is a type of oncology that is not one of the common types. It accounts for no more than 3% of lesions from malignant tumors of the gastrointestinal tract. Symptoms and manifestations of small intestinal cancer in women develop much less frequently, and therefore the disease is mainly diagnosed in older men, that is, over 60 years of age.
Risk group
Etiology of the disease
The term “intestinal cancer” refers to a malignant tumor that affects the tissue of the intestine with mutagenic cells that begin to divide uncontrollably. Affected cells fill the area, disrupt its functioning, spread to adjacent areas, healthy tissues, and over time infect the entire body. In the absence of necessary treatment, intestinal pathology leads to death.
The length of the loop-shaped small intestine reaches 4.5 m. It consists of several sections: duodenum, jejunum, ileum. Each of them can develop a malignant tumor.
Intestinal cancer is a disease whose exact causes have not yet been established by medical science. There is a list of intestinal pathologies, damage to which provokes an increased risk of developing cancer. This:
- the presence of nonpolyposis hereditary colorectal cancer,
- celiac disease,
- congenital anomalies of the structure of the gastrointestinal tract,
- Crohn's disease.
One of the factors
Oncology of the small intestine can also occur under the influence of such factors on the human body:
- eating foods high in carcinogens,
- abuse of alcohol, nicotine,
- radiation exposure.
Most often, a malignant tumor begins to affect the cylindrical epithelium of the intestinal glands, and therefore, according to histology, it is classified as carcinoma. Predispose to the occurrence of intestinal disease:
- intestinal ulcers,
- BPH,
- chronic inflammatory processes in the intestines,
- diagnosis of diverticulitis.
An intestinal tumor almost always grows into the intestinal lumen, and in isolated cases it is exophytic. Oncology, which expands into the lumen, greatly narrows the intestine in a ring-shaped manner.
The loop of intestine, which is located above the site of narrowing, often expands and its muscles hypertrophy. With severe and long-term stenosis of the lumen, the loop in the intestine stretches, becomes thinner, and perforates, causing peritonitis. This is how patency is impaired due to intussusception.
Oncology rarely undergoes ulceration. It is characterized by metastases to the following organs:
- retroperitoneal and mesenteric lymph nodes,
- liver,
- abdominal region,
- lungs,
- adrenal glands,
- bones,
- dura mater.
As a rule, metastases from the intestines spread throughout the body with lymph.
A neoplasm in the intestine can grow together with a nearby loop of intestine, bladder, colon, female genitals, and enlarged regional lymph nodes.
Causes of small intestine cancer
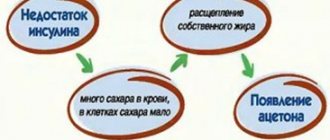
Malignant cells differ from normal cells of the body in their ability to undergo uncontrolled and endless division (in healthy cells the number of possible divisions is limited), loss of the ability to die naturally, and the possibility of spreading to neighboring tissues and organs and their destruction.
In the body of any person, mutations constantly occur that cause the appearance of malignant cells. But usually the immune system quickly detects them and destroys them before the tumor begins to grow. However, if, under the influence of some factors, too many altered cells are formed or the immune system does not recognize them in time, a malignant tumor appears.
Doctors do not have an exact list of the causes of small intestinal cancer. The only known risk factors that increase the likelihood of its occurrence are:
- Crohn's disease. This is a chronic inflammation of the small intestine. Under the influence of a long-term inflammatory process, the normal ability of the mucous membrane to recover is disrupted and its cells can become malignant.
- Celiac disease. With this disease, the body produces antibodies to the proteins of cereal plants - gluten. Immune compounds settle on the lining of the small intestine, causing inflammation. Chronic inflammation impairs the ability for normal mucosal regeneration.
- Familial adenomatous polyposis. This is a hereditary disease in which, due to an error in genes, many polyps form on the mucous membrane. Polyps themselves are benign formations, but over time they degenerate into malignant ones.
Kinds
A malignant tumor can form anywhere in the small intestine. Oncology is classified into exophytic and endophytic in accordance with the nature of tumor growth. ICD disease code C17 malignant neoplasms of the small intestine.
An exophytic tumor in the intestine grows inside the intestinal lumen. At the very beginning, it provokes stagnation of content in this department. After a certain time, stagnation turns into obstruction.
Endophytic neoplasms do not have clear boundaries. They begin to spread into the intestinal tissue, affecting its layers one by one, gradually affecting all the membranes. With further progression, oncology affects neighboring organs.
An endophytic tumor is more dangerous, and the prognosis for life expectancy and recovery in this case is negative. Intestinal diagnostics helps determine the exact nature of the tumor.
In accordance with the histological structure of tumor neoplasms, they are classified into the following types:
- adenocarcinoma is a tumor that affects the glandular tissues of the intestine; it does not often form in the intestine, mainly affecting the duodenum,
- carcinoid is a malignant tumor that is formed from epithelial cells, it mainly affects the small and large intestines,
- lymphoma is a rare type of ileal cancer,
- leiomyosarcoma is a malignant tumor that can reach large sizes, is detected even through the abdominal wall, and often provokes intestinal obstruction.
Carcinoid
Meckel's diverticulum (congenital ileal diverticulum).
During intrauterine development, the vitelline-intestinal duct (ductus omphalo-entericus) connects the intestinal tube with the vitelline (umbilical) bladder. By the 3rd month of intrauterine development, the vitelline-intestinal duct becomes obliterated and disappears, and the intestine completely loses its connection with the navel. If embryogenesis is disrupted, the vitelline-intestinal duct may remain open along its entire length, and then a fistula is formed, through which the contents of the small intestine are released out. In some cases, the vitelline duct is obliterated only near the navel, and no obliteration occurs near the wall of the small intestine. This leads to the formation of an ileal diverticulum, which was first described in detail by J. Meckel (Jr.) in 1809.
A Meckel diverticulum is a blind process of the intestine ranging from 1.2 to 10-12 cm in length. Typically, the diverticulum arises from the free edge of the intestine. The width of its lumen varies. With a narrow lumen, the diverticulum resembles a vermiform appendix. The wall of the diverticulum consists of three layers: serous, muscular and mucous membrane, which are a continuation of the same layers of the intestine and completely repeat their structure. Most often, the diverticulum lies free in the abdominal cavity, but in some cases it can be fixed to the abdominal wall or to the wall of the nearby intestine or its mesentery, which can cause intestinal obstruction. The blood supply to the diverticulum is provided by the vessels of the intestinal wall.
Clinical picture.
Meckel's diverticulum most often does not manifest itself clinically and is discovered accidentally during an X-ray examination of the intestine or during surgery on the abdominal organs. And only the development of a pathological process in the wall of the diverticulum itself becomes the cause of the manifestation of clinical signs of the disease. Among the pathological processes that occur in Meckel's diverticulum, diverticulitis and diverticulum ulcer should be highlighted.
The development of diverticulitis is promoted by stagnation of contents in the lumen of the diverticulum. The inflammatory process in the wall of the diverticulum can be acute or chronic according to the nature of its course. Acute inflammation can be expressed very differently - from minor serous infiltration of the diverticulum wall to significant changes in it, leading to the destruction of all layers of the wall and the development of peritonitis. The clinical picture of acute diverticulitis is essentially no different from the clinical picture of acute appendicitis. However, most authors note that with diverticulitis, abdominal pain is localized closer to the navel, and the clinical picture itself can be more pronounced - higher body temperature, more intense intoxication. However, these signs also occur in destructive forms of appendicitis. Therefore, if the surgeon, performing an operation for acute appendicitis, finds no changes in the appendix, he should always examine the terminal ileum so as not to miss the presence of diverticulitis.
Outside the phase of exacerbation of the inflammatory process in the wall of the diverticulum, symptoms of the disease, as a rule, do not occur. Meckel's diverticulum ulcers are rare. They develop like peptic ulcers. The ulcerative process progresses rapidly, which can lead to bleeding or perforation of the diverticulum wall.
Clinically, a Meckel diverticulum ulcer manifests itself as attacks of abdominal pain or intestinal bleeding. The type of blood released varies. Sometimes fresh blood is released, which has a bright scarlet color, sometimes old decomposed blood is released. This depends on the intensity of bleeding and the speed of removal of blood from the intestinal lumen. Abdominal pain can be very severe and usually occurs after bleeding. Sometimes a diverticulum ulcer is asymptomatic, and the first clinical sign of the disease is peritonitis that develops as a result of perforation of the diverticulum wall. The presence of an ulcer in the wall of the diverticulum is detected only during surgery. However, the presence of paroxysmal abdominal pain, preceded by bloody stools without mucus, especially in young men, should always cause the doctor to suspect the presence of a Meckel diverticulum ulcer and perform an X-ray examination of the intestine on the patient.
Treatment of diseases of Meckel's diverticulum.
Each disease associated with Meckel's diverticulum is subject to surgical treatment - it is necessary to perform a diverticulectomy. In cases where the diverticulum is involved in a pathological process localized in another organ, it should also be removed.
If a diverticulum is accidentally discovered during surgery for a disease of any abdominal organ, it must be removed if traces of a former or existing pathological process are found in it. If no pathological processes are detected in the wall of the diverticulum and its size is small, then it is considered inappropriate to complicate each operation in which it was discovered by removing the diverticulum.
If you find an error, please select a piece of text and press Ctrl+Enter.
Reasons for development
The reliable reasons that cause the formation of oncology have not been established. In accordance with the surveys and statistics, the risk of contracting pathology increases in the following situations:
- when diagnosed with a tumor of the small intestine in the immediate family of a person,
- with chronic infectious inflammation of the small intestine, which can destroy mucous surfaces,
- polyps in the intestine,
- oncology of other organs,
- radiation exposure,
- abuse of alcoholic beverages, smoking,
- constant inclusion in the diet of salted, dried, smoked foods, which contain a lot of animal fats, as well as frequent consumption of lard and fatty meats.
Polyps
Important! Most often, oncology of the small intestine is detected in men after 60 years of age.
Inflammation of the large intestine
Inflammation of the large intestine or colitis is an infectious disease of parasitic or intoxication origin. Colitis of the first degree is caused by damage to the mucous membrane of the walls during direct contact with the pathogen. Colitis of the second degree is a consequence of gastrointestinal pathologies: pancreatitis, gastritis, cholecystitis, etc. Rarely, inflammation of the colon has extragastric causes, such as allergic reactions.
Characteristic symptoms
A malignant tumor in the small intestine at the very beginning of the lesion does not provoke any symptoms. The first signs develop only at the stage when the course of the disease leads to a narrowing of the lumen in the affected area of the small intestine.
The very first symptoms that should alert a person and become a reason to visit a doctor include complex dyspeptic problems in the intestines:
- persistent nausea
- vomit,
- bloating,
- spastic pain in the epigastrium, in the navel area.
Also, in the first stages of tumor damage, patients experience the following characteristic manifestations:
- loose stools with tenesmus – false urge to defecate with pain, after which there is copious discharge of mucus,
- alternating diarrhea and constipation,
- intestinal obstruction of varying severity,
- pain during bowel movements.
Pain during bowel movements
Common signs of bowel disease include:
- rapidly increasing weakness
- frequent ailments,
- rapid fatigue even after light work,
- loss of appetite,
- sudden, seemingly causeless weight loss,
- low protein content in blood plasma,
- anemia,
- pale tint of blood and mucous surfaces that line the mouth and nasal cavity,
- frequent dizziness, headaches,
- persistent increase in body temperature to subfebrile.
In men and women, a tumor in the small intestine develops in the first stages of the lesion almost equally. But at the time of active progression and influence on nearby organs, some differences arise.
In women, during the process of tumor growth into the tissue of neighboring organs, the vagina is injured, and in males, the prostate is injured. When the disease affects the rectum and anal area, women and men complain of intense pain in the anus, in the area of the coccyx, sacrum, and lumbar spine.
Men are especially prone to urinary problems. This indicates tumor growth into the walls of the bladder. This process provokes a rise in temperature to high numbers, infection of the urinary tract in an ascending manner.
Important! Oncology can progress for a long time without provoking complaints at all, and first manifest itself only after the occurrence of serious irreversible complications.
A tumor of the small intestine is characterized by a gradual increase in symptoms, and therefore people do not take them seriously. Over time, the tumor grows and has a negative impact on the functions of neighboring organs. In this case, victims have complaints that indicate the following dangerous conditions of the intestine:
- intestinal ischemia,
- pancreatitis,
- obstructive jaundice.
In especially severe cases, serious disruptions already occur in the functioning of other organs that are located closer to the tumor - pancreas, liver, etc.
Anatomical and physiological data.
The small intestine begins from the duodenojejunal flexure (from the ligament of Treitz), located to the left of the II lumbar vertebra.
Its final part passes into the cecum, forming the ileocecal junction, which has a Bouginian valve, which prevents the passage of the contents of the large intestine to the distal parts of the small intestine. The total length of the small intestine in an adult varies from 5 to 7 m, and the diameter of its lumen is from 3 to 5 cm. About 2/3 of the small intestine is called the jejunum, and the remaining part is called the ileum, although there is no clear anatomical boundary between them. The loops of the small intestine are attached throughout their entire length to the mesentery, formed by two layers of visceral peritoneum, between which lymphatics, blood vessels and nerves pass in loose tissue. The small intestine is supplied with blood by 16-22 intestinal branches arising from the right semicircle of the superior mesenteric artery. These vessels form among themselves arterial arches of the first and second order in the thickness of the mesentery. Numerous short straight arteries extend from the latter to the intestinal wall. The veins of the small intestine unite into a large venous trunk, the superior mesenteric vein, which flows into the portal vein. The small intestine has dual innervation - parasympathetic and sympathetic.
The small intestine undergoes a complex process of chemical and enzymatic breakdown into the final products of proteins, fats and carbohydrates, which are absorbed through the large surface of the small intestine mucosa. Vola and electrolytes are absorbed in the small intestine. The described function of the small intestine has a significant impact on the constancy of the internal environment of the body and is characterized by great dynamism. All pathological processes that occur in the small intestine and lead to disruption of its normal function can quickly cause severe disorders of water and electrolyte balance and significant changes in metabolism.
Among the diseases of the small intestine that are most often encountered in clinical practice are terminal ileitis and Meckel's diverticulum.
Terminal (regional) ileitis was first described in detail by B. Crohn in 1932. As it turned out later, a pathological process identical to the one described by Crohn can be localized in any part of the gastrointestinal tract. However, it is most often found in the terminal small intestine. In the literature it is described under different names: terminal ileitis, Crohn's disease, regional ileitis, granulomatous enteritis (colitis), etc.
Etiology.
To date, the true cause of terminal ileitis has not been established. Some authors believe that the cause of the development of the pathological process in the terminal part of the small intestine is the presence of bacteria and viruses in it (infectious theory). However, the specific causative agent of this disease could not be found.
In 1936, Raichert put forward a theory according to which Crohn's disease occurs as a result of inflammatory blockade of the lymphatic vessels of the small intestine with the development of severe lymphostasis in its wall and mesentery (inflammatory theory). . Lannay caused granulomatous changes in the intestines of sensitized animals (immunological theory). However, it was not possible to prove the autoimmune genesis of Crohn's disease.
Pathological anatomy.
Crohn's disease is characterized by the occurrence of significant inflammatory infiltration of the affected segment of the gastrointestinal tract, in particular the terminal segment of the ileum, the wall of which takes on a bluish-purple color, becomes thickened and rigid, which makes it possible to clearly detect it against the background of a healthy intestinal wall. The most pronounced changes affect the submucosal layer of the intestinal wall, which leads to a narrowing of the intestinal lumen and difficulty in the passage of intestinal chyme. Ulcers appear on the surface of the intestinal mucosa.
There is pronounced swelling of the intestinal mesentery, which seems to “float” onto the surface of the intestine. In the thickness of the mesentery, noticeably enlarged lymph nodes are found. In the chronic course of the disease, the intestinal loops in the area of development of the pathological process stick together and form a tumor-like conglomerate.
Clinical picture.
There are acute and chronic stages of the disease. In the chronic version, Crohn's disease can be asymptomatic for a long time or manifest itself as cramping abdominal pain, loose stools and general weakness.
In the acute period of the disease, which is characterized by a rapid onset, diarrhea, excruciating pain in the abdomen (in the navel or right lower quadrant), often cramping in nature, vomiting, fever, and an increase in the number of leukocytes in the blood come to the fore. In some cases, tension in the muscles of the anterior abdominal wall or Shchetkin’s symptom appears - Blumberg. This clinical picture often simulates an acute disease of the abdominal organs (acute appendicitis, perforated ulcer, etc.). With severe swelling of the intestinal wall, symptoms of intestinal obstruction may appear with retention of stool and gases. The true picture of the disease is often revealed only during laparotomy.
Serious complications can occur with Crohn's disease, which include bleeding into the intestinal lumen, the formation of abscesses in the abdominal cavity and enteric fistulas.
Diagnosis of terminal ileitis is quite difficult, especially in the acute period of the disease, since the symptoms of acute ileitis are very similar to the symptoms of many acute diseases of the abdominal organs. In the stage of chronic inflammation, the diagnosis of terminal ileitis can be made based on the clinical picture. X-ray examination of the small intestine while monitoring the passage of barium suspension through it can be of great help in diagnosing the pathological process. On radiographs (Fig. 67), it is possible to detect an oblong narrowing of the lumen of the terminal ileum, where the contrast agent appears in the form of a lace (the so-called “lace” symptom). However, it should be noted that an accurate diagnosis of terminal ileitis can only be made after histological examination.
Rice. 67. X-ray picture of terminal ileitis. The narrowed area of the dysgainic ileum has irregular contours.
The diagnosis of terminal ileitis can be helped by histological examination of a lymph node taken during laparoscopy.
Treatment.
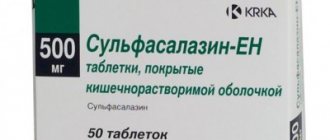
Terminal ileitis with an uncomplicated course of the pathological process is subject to conservative treatment. The use of cortisone and its derivatives, as well as ACTH, has a good effect. It should be noted that cortisone therapy does not provide long-term remission of the disease. In recent years, a combination of cortisone and sulfonamide drugs (salazopyrine, sulfasalazine, salazopyridazine) has been used to treat terminal ileitis. In the acute period of the disease, the prescription of antibiotics is indicated - norfloxacin, ciprofloxacin, ceftriaxone, metronidazole. The administration of anti-immune drugs (imuran) gives a positive result.
If there is no effect from conservative therapy and if complications of the disease occur, surgical treatment should be resorted to, which consists of resection of the affected areas of the intestine within healthy tissues along with the mesentery and hyperplastic lymph nodes. Most often, with terminal ileitis with a sharp narrowing of the intestinal lumen, it is necessary to perform a right hemicolectomy. If a complication of terminal ileitis occurs, the nature of the surgical intervention depends on the localization of the pathological process and the general condition of the patient. The number of disease relapses after surgical treatment of Crohn's disease, according to various authors, reaches 50-80%, especially after early operations.
Degrees
- 1st degree. At this stage, the diameter of the tumor does not exceed 2 cm, it does not extend beyond the boundaries of the small intestine and does not grow into the tissue of nearby organs, and no metastases have yet formed.
- 2nd degree. At this stage of the progression of the malignant tumor, it grows a little more, begins to extend beyond the boundaries of the intestinal wall and affect nearby organs, but there are no metastases. At this stage, the pathological process often involves the cecum, large intestine, and more specifically its part - the sigmoid colon.
- 3rd degree - the tumor increases greatly and can send metastases to the lymph nodes near the small intestine, but distant metastases have not yet been observed.
- 4th degree - the tumor has already affected tissues located nearby and provokes multiple metastases to distant systems and organs.
Oncology of the small intestine is characterized by metastasis to the following organs:
- abdomen,
- liver,
- ovaries,
- lungs,
- pancreas,
- bladder,
- adrenal glands,
- pelvic organs,
- lymph nodes in the retroperitoneal region.
Prognosis and prevention of small intestinal cancer
The prognosis for small intestinal cancer is serious, since due to minor and vague symptoms, the diagnosis is usually made too late, when the tumor has already spread beyond the intestine.
Prevention of small intestinal cancer has not been developed. It should be noted that with celiac disease, following a strict diet and preventing exacerbations significantly reduces the likelihood of developing a malignant tumor.
[1] Scottenfeld D. et al. The epidemiology and pathogenesis of neoplasma in the small intestine. Ann, Epidemiol. 2009.
Diagnostics
To make a correct diagnosis, the doctor conducts a comprehensive examination of the patient’s condition. It includes several methods to increase the accuracy of the results:
- Clinical method. The patient is interviewed, visually examined and palpated to establish the circumstances of the development of the disease and the location of the malignant tumor. If the tumor is large, then it can be detected already at this stage of diagnosis.
- Laboratory method. Diagnostic tests are carried out to detect anemia, increased ESR, abnormalities in liver tests, and digestive disorders. The presence of indicators of intestinal cancer in the blood - tumor markers - is also checked.
- Ultrasound.
- Endoscopy. Capsule and laparoscopic techniques are implemented.
- X-ray with the introduction of a contrast agent. This method allows you to establish the localization of the tumor and diagnose the direction of its growth - into the thickness of the intestine, into the lumen.
- MRI.
Tumor markers in the intestines are produced in response to the aggressive influence of a malignant neoplasm on the body. They can be of two types. The first are organ-specific, which are produced by affected cells immediately after damage by pathology; in the normal state they are not present in the body. The second type is enzymes, hormones and other biological substances that produce remaining healthy cells.
Diagnostics
Symptoms of inflammation of the large intestine
Large intestine inflammation symptoms of acute colitis can occur quite violently. In this case it is observed:
- bloating;
- sharp pain;
- mucous discharge from the anus;
- painful urge to defecate;
- diarrhea.
Also, these symptoms are accompanied by vomiting, high fever, general weakness, and sudden weight loss. In this case, the patient must definitely consult a doctor and conduct a full examination of all parts of the large intestine, its lower and upper parts, and, if necessary, the entire gastrointestinal tract.
Upon examination, they may reveal:
- swelling of the intestinal mucosa;
- thickening and hyperemia of the affected areas of the intestinal wall;
- localization of large amounts of mucus and purulent discharge;
- formation of erosions and ulcers on the intestinal mucosa;
- minor hemorrhages;
- A clinical blood test reveals high levels of ESR and leukocytes.
There may also be other clinical pictures of the disease. For example, for two to three weeks a person may experience discomfort with diarrhea, turbulence in the stomach and flatulence.
. But since such problems are insignificant, he does not pay attention to them, does not consider them important and does not associate them with the occurrence of a serious disease of the colon. Thus, the acute form becomes chronic.
Treatment
Treatment of a malignant tumor in the small intestine depends on the degree of damage to the organ and the type of oncology. In approximately 2/3 of all cases, surgery is performed to remove cancer cells. This helps reduce the intensity of symptoms and increase the patient's life expectancy.
Important! Sometimes the operation has only palliative value, that is, it is performed with the sole purpose of alleviating the patient’s suffering.
When the operation is impossible or the tumor formation is sensitive to the effects of chemotherapy, it is performed. Chemotherapy drugs inhibit the growth of cancer cells, preventing them from multiplying and developing normally.
Radiation therapy is ineffective for small intestinal cancer, which is why it is not performed. This can take place immediately after or during surgery to improve positive results. Radiation therapy is also used when surgery is impossible for some reason.
After surgery is completed, the patient is advised to undergo rehabilitation to eliminate the symptoms of cancer and try to completely get rid of cancer cells. Your doctor may prescribe the following medications:
Chemotherapy
At the same time, radiation therapy is implemented. But all of the above procedures can cause a large number of side effects:
- poor health and weakness,
- nausea with vomiting,
- diarrhea,
- constant headaches,
- hair loss,
- disruption of hematopoietic processes,
- mouth ulcers,
- dysfunctions of the immune system.
Due to the fact that the patient’s body is difficult to tolerate treatment, he requires the organization of adequate nutrition, which presupposes compliance with the following conditions:
Rejection of bad habits
Important! In severe stages of the pathology, when surgery is not practical, only radiation and chemotherapy are performed to relieve pain and other severe manifestations of oncology.
Treatment of inflammation of the lower colon
Treatment for inflammation depends on the specific diagnosis and severity. If a slight inflammation is caused by poisoning, then gastric lavage, taking various sorbents, drinking plenty of fluids and diet will help get rid of the problem in a few days
.
More serious diseases require a thorough examination and a professional approach to the treatment of the large intestine. Lack of proper balanced treatment can lead to dangerous consequences, including peritonitis.
We advise you to read: Is there swelling during ovulation?
For any form of colitis, it is necessary to follow a strict therapeutic diet, and especially if this is observed in pregnant women or in a newborn child. In this case, the doctor prescribes Diet No. 4
, which excludes from the diet foods that promote fermentation and rotting in the large intestine, irritating its mucous membranes: hot, salty, fatty, sweet, sour, fatty, spicy and dairy.
You should also temporarily avoid eating vegetables, fruits and berries. All food should be consumed only in liquid or thoroughly pureed form at a comfortable room temperature. This regimen must be followed throughout the entire treatment period and even after it. At the very beginning of the course of treatment (the first 1-2 days), it is better not to eat anything, and limit yourself only to drinking liquid in large quantities.
Therapeutic cleansing enemas
In case of inflammation of the large intestine, enemas are done only as prescribed by a gastroenterologist if it is necessary to cleanse the intestine of infectious components and its contents for direct delivery of therapeutic agents to the mucous membrane of the walls.
- Antiseptic enemas are made with infusions of chamomile, collargol and calendula. They help relieve swelling and soothe the intestinal mucosa, as well as remove pathological microflora locally.
- Enemas with sea buckthorn oil help rapid healing and restoration of the tissues of the mucous membrane of the large intestine.
Drug treatment of inflammation
Taking medications depends on the severity of the disease and its form and is prescribed only by a doctor after a complete diagnosis has been established.
- When pathogens such as viruses, infections, worms, and protozoan microorganisms are identified, antibiotics, antiviral and antiparasitic drugs, and sulfonamides are prescribed.
- If you have pseudomembranous colitis, you should stop taking antibiotics.
- To relieve spasms and pain, No-shpa, rectal suppositories and papaverine are prescribed.
- In case of poisoning, intoxication and infections, it is necessary to take drugs - enterosorbents, such as Polyphepan, Enterosgel and others.
In some difficult cases, surgery is required
: with perforation, peritonitis, necrotic processes, obstruction of the intestinal lumen, obstruction, expansion of infection to other tissues of the body. Also, indolent colitis that is not amenable to drug treatment and ulcerative colitis require surgical intervention.
In addition to medication and surgical treatment, patients are often prescribed radon mud baths, mineral water treatment, gymnastics, massage, and physiotherapy.
source