Flat epithelium
No more than 10 were found in the field of view
- Normally, squamous epithelium is present in the smear, since these cells are constantly renewed and exfoliated.
Found in large numbers, more than 10 in the field of view
– An increase in the number of epithelial cells in the smear is a sign of an inflammatory process in the vagina.
Not found
– In the absence of epithelium in the smear of the vagina and cervix, it can be assumed that the woman’s hormonal levels are disrupted and there is an insufficient amount of estrogen. This is also an indirect sign of atrophy of the vaginal mucosa.
Medical terms that scare you
Dystrophy or dystrophic epithelium - occurs with true erosion of the cervix or pseudo-erosion, which is also called ectopia. In a word, when there is a wound on the cervix. When it heals, cell degeneration will no longer be detected.
The medical term “metaplastic” is often present in the cytogram. Many people think that this indicates a malignant process. But no - metaplastic epithelium is a good smear result.
This indicates that the cells were taken exactly from the desired zone - the junction of two types of epithelium - from the endocervix (cylindrical) and exocervix (flat). These are the cells of the transformation zone, where atypia, precancerous or cancerous changes are most often found.
Acetowhite epithelium (ABE) is not an indicator that can be displayed on smears. ABE is visible during extended colposcopy after exposure of the cervix to acetic acid.
If there are pathological areas on it, the epithelium will begin to turn pale. Next, the doctor makes conclusions based on how quickly the whitening occurred, how bright it was, how long it lasted, whether it had boundaries, whether there was a sign of a ridge, etc.
If the reaction was not pronounced, most likely the women have chronic cervicitis (inflammation), HPV or LSIL (mild dysplasia). In case of severe ABE, HSIL is diagnosed - severe dysplasia.
In appearance, the cervix, even with severe dysplasia, can be quite healthy. And only the vinegar test shows what is not visible to the eye.
Not every gynecologist is a good colposcopist. An experienced specialist monitors the cervix during extended colposcopy after treatment with vinegar and iodine, literally without taking his eyes off, and makes very accurate diagnoses.
By the way, in some countries it is the vinegar test, and not the PAP test, that is a screening method for diagnosing precancer. If coarse acetic-white epithelium is detected, the woman is taken under control and treated.
Hyperplastic epithelium is usually synonymous with cervical canal polyp. Needs removal and histological examination.
Cells with signs of keratosis, keratinization - most often these words can be seen in the reports of women with suspected leukoplakia. But the same signs (features of epithelial cells) occur in precancer and cancer.
Pronounced reactive changes are an inflammatory process in the cervix.
Signs of mild dysplasia - lsil. If there are pronounced, deep changes, we are usually talking about HSIL - severe neoplasia, in which surgical intervention is necessary - conization of the cervix.
READ MORE: Do they take a smear during menstruation?
Koilocytosis is a feature of epithelial cells most characteristic of PVI (human papillomavirus, HPV). Viral infection.
Reparative changes in the epithelium are benign changes in cells, a variant of reactive changes (see above).
Degenerative changes are not cancer; they occur during a chronic or acute inflammatory process. In the same category, reactive changes include the following concepts: inflammatory atypia, squamous metaplasia, hyperkeratosis, parakeratosis.
Atypia, atypical changes - dysplasia (precancer) or malignant neoplasm.
Atypical squamous epithelial cells of unknown significance - asc-us. These are cells of unknown significance. The cytologist sees that they look unusual, changed, but cannot accurately determine what was the cause - inflammation, dysplasia, infection or irritation.
There is no need to be afraid of this formulation. It does not raise the doctor's suspicion of cancer. However, it is a reason to take smears from the cervix for HPV of high oncogenic risk (required types 16 and 18). And if they are detected, you need to undergo an extended colposcopy.
Proliferation of squamous epithelium - that is, proliferation or in medical terms - mitosis. Normally, this process proceeds slowly. Its purpose is to renew the upper layer of the cervical mucosa. During pregnancy, the process is more active, but normally moderate.
If, according to the results of scraping, proliferation is pronounced, then this happened for one of the following reasons:
- cervicitis (inflammatory process on the cervix);
- tissue trauma resulting from diagnostic curettage, abortion, difficult childbirth, conization;
- tumor growth - benign or malignant (cervical canal polyp, mild or severe dysplasia, cancer, papilloma).
That is, proliferation can be hyperplastic, inflammatory or post-traumatic.
Dyskaryosis is an enlargement of the cell nucleus. The cause is gynecological diseases (colpitis, cervicitis, vaginitis) or dysplasia.
https://youtu.be/NVDaCWstEp8
Staphylococcus aureus, cocci
Not found
– Normally, the absence of foreign flora is a sign of a high degree of vaginal cleanliness.
Less than 10 detected in field of view
– a single amount of extraneous opportunistic microorganisms is normally acceptable if there are no signs of inflammation.
More than 15 were detected in the field of view, the entire field of view, leukocytes above 15 in the field of view
– The presence of a large number of cocci, leukocytes, inflammatory cells (key cells) is a laboratory indicator of purulent inflammation in the vagina or cervical canal.
Anatomical features
The cervix is the lower section of the uterus, which is the connecting link between the cavity and the vagina. Inside it is the cervical canal, which is the only way to communicate with the environment and the internal genital organs.
Since it is through the cervical tissue that infection can occur, it has a special defense mechanism. There are two pharynxes: the external one, which opens into the vaginal cavity, which is accessible to the doctor for examination, and the internal one, located at the junction with the uterine cavity. These structures are primarily needed not only to protect organs from viruses and pathogenic bacteria, but also for normal pregnancy.
https://youtu.be/642YpJJUeLA
The inside of the cervical canal is lined with epithelial glandular cells capable of producing mucus. By the appearance of the cervix, by its color and surface, as well as by the consistency of the mucus, the doctor can assume the presence of some pathology.
Sticks (Doderlein)
Not detected, cocci, gonococci, trichomonas, fungi, leukocytes more than 15
– the absence of rods is a sign of a severe disorder of the vagina, severe inflammation, with the displacement of vaginal lactobacilli by the pathogenic flora.
Found in small quantities, cocci, gonococci, trichomonas, fungi, leukocytes more than 15
– An insufficient number of rods is a sign of a severe disorder of the vagina, severe inflammation, with the displacement of vaginal lactobacilli by the pathogenic flora.
95% of all bacteria
– The natural microflora of the vagina is normally 95% or more of rods.
Possible pathologies
Cervical pathologies are one of the most common cases in gynecological practice. Diseases can develop for many reasons, the main ones include:
- congenital disorders;
- imbalance of the hormonal system;
- infections;
- inflammatory processes;
- damage during surgical operations.
Common symptoms of cervical pathologies are pain, atypical or even bloody discharge, as well as discomfort during sexual intercourse.
Structural anomalies
The first group of cervical diseases consists of anomalies associated with changes in the structure. They can be either congenital or acquired. In the first case, the pathology most often spreads to other parts of the woman’s reproductive system.
Structural abnormalities are associated primarily with changes in the patency or shape of the cervical canal. The main diseases include the following pathologies.
- The cervical canal has the shape of a funnel, which has developed as a result of improper arrangement of muscle fibers. It can occur during labor, which leads to difficulties in subsequent pregnancies. This pathology does not provide treatment.
- Atresia of the cervical canal is a complete obstruction or severe narrowing of the canal. It can be either a congenital anomaly or pathologies that develop during abortion or the formation of cancerous tumors. It is dangerous due to the accumulation of menstrual blood in the uterine cavity and the inability to conceive a child.
- The development of two canals is a congenital anomaly, which is a duplication of the genital organs. In this case, there is a possibility of a normal pregnancy and childbirth, so surgical intervention is a last resort.
Sometimes there are cases of enlargement of the cervical canal, which entails danger during pregnancy. This is due to an excess of male sex hormones in the body and the loss of the function of confining the fetus by the cervix. Most often, appropriate medications are prescribed to correct hormonal levels or a gynecological ring is installed. Often the structure of the cervix contains an excess amount of connective tissue; in such situations, the organ cannot withstand the mechanical pressure exerted by the fetus. The cervical canal begins to expand, and the cervix begins to shorten.
Candida
Not detected
– Yeast should not be present in the normal vaginal microflora.
Candida was detected above 104 CFU/ml, leukocytes more than 15 in the field of view, squamous epithelium more than 10 in the field of view
. – The presence of yeast-like fungi is a manifestation of candidiasis (thrush), or a concomitant laboratory indicator for inflammatory processes in the vagina. Candida is found as an opportunistic flora, and often accompanies viral infections of the cervix and vagina, STDs.
Functions
The main functions of the cervix include:
- barrier - the external os prevents the entry of viruses, microorganisms and bacteria into the uterine cavity, and also limits the movement of sperm to the egg (except for the period of ovulation);
- childbearing - the cervix is capable of strong stretching during the passage of the child through the birth canal;
- fertilization - mucus produced by the cells of the cervical canal in the middle of the menstrual cycle creates a favorable environment for sperm to penetrate into the uterus and further conception.
All of the above functions are important for a woman’s body, especially during pregnancy.
Escherichia coli
Not found
– there should normally be no E. coli in the vagina
Detected, leukocytes more than 15 in the cell. –
E. coli in the vagina can be a component of opportunistic flora, and enter the vagina from the intestines. In the presence of a large number of leukocytes, and the absence of other infections, E. coli in the smear is considered the causative agent of the inflammatory process.
Found in single quantities -
E. coli in the vagina can be a component of opportunistic flora, and enter the vagina from the intestines. If there are no complaints, no treatment is required
Cytological examination of scrapings of the cervix and cervical canal
Interpretation of research results contains information for the attending physician and is not a diagnosis. The information in this section should not be used for self-diagnosis or self-treatment. The doctor makes an accurate diagnosis using both the results of this examination and the necessary information from other sources: medical history, results of other examinations, etc.
It should be remembered that the cytological research method, like any other laboratory research method, does not always provide comprehensive information for making a diagnosis. Only a clinician has the right to make a final diagnosis (based on a study of the anamnesis, observation of clinical manifestations and histological examination data).
The result of a cytological examination of the obtained biomaterial (imprint smears) can be presented by a cytologist in the form of: - description of the cellular composition; — descriptions of cellular composition and conclusions; — descriptions of the cellular composition and conclusions in a conjectural form; — descriptions of cellular composition and recommendations.
The form of the answer depends on a number of reasons: the adequacy of the cellular material (few cells, many blood elements, mucus), an incorrectly filled out referral for a cytological examination: the reason for the examination is not indicated (clinical diagnosis), the presence/absence of menstruation; it is not indicated where the material was taken from, the markings in the direction do not correspond to those on the glass, etc.
Interpretation of the result
Possibilities of cytological diagnosis of some diseases of the cervix and options for interpreting the results of cytological examination:
Endocervix. Normally, when cellular material is correctly obtained from the transformation zone (ZZ) - the junction zone of squamous and columnar epithelium - the smear contains cells of squamous and columnar epithelium without changes. Cytological conclusion: the obtained material contained cells of squamous and columnar epithelium without any features. The presence of a small number of metaplastic epithelial cells is an indication that the material is derived from ST. In the absence of the above description, the smear was not taken from the CT and it cannot be said that the patient does not have a risk of cervical cancer. Such smears are common in postmenopausal women and patients who have undergone cervical treatment that has moved the boundary line into the cervical canal. Depending on the patient’s medical history, this may be a reason to re-sample material.
The clinical diagnosis in the direction of polyps of the cervical canal, and the corresponding cytological picture allows the cytologist to give a conclusion; the cytogram corresponds to the clinical diagnosis of polyps of the cervical canal. If there is no clinical diagnosis, and the cellular composition is represented by large accumulations of columnar epithelial cells, the cytologist gives a descriptive answer with the assumption of hyperplasia of columnar epithelial cells or a polyp of the cervical canal.
Ectocervix. During reproductive age, the cellular composition of imprints from the vaginal part of the cervix is normally represented by squamous epithelial cells, predominantly of the superficial or intermediate type. The wording “in the obtained material there are squamous epithelial cells of the surface layers without any features” indicates that the obtained biological material consists of squamous epithelial cells of the surface and intermediate layers in various combinations in accordance with the phase of the cycle. At the beginning of postmenopause (normally), squamous epithelial cells of the intermediate layer are noted in the smear. In some women, throughout their entire subsequent lives, an intermediate type of smear is observed (squamous epithelial cells of the intermediate layer), sometimes with the presence of cells of the superficial layer, which is apparently associated with the function of the adrenal glands and active sexual life. The presence of squamous epithelial cells of the surface layer (estrogenic type of smear) in the preparation in the first 5 years of menopause should be alarming regarding ovarian neoplasms and uterine fibroids. Postmenopause is characterized by the presence of cells of the basal-parabasal layer (i.e., deep layers).
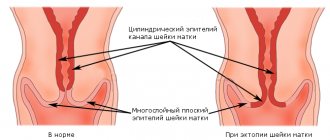
Erosion (ectopia) of the cervix. The concept of cervical erosion (true erosion) implies a defect in the mucous membrane of the cervix caused by various diseases (syphilis, traumatic injuries, consequences of radiation therapy, cervical cancer, etc.). The term cervical ectopia (pseudo-erosion) means displacement of the tall columnar epithelium onto the vaginal part of the cervix. Provided that there is a clinical diagnosis of “cervical erosion/ectopia” in the direction and correct collection of biomaterial from the ectocervix (cellular material is represented by squamous epithelial cells of all layers in various combinations, accumulations of columnar epithelial cells, elements of inflammation), the cytological conclusion has the following form of answer: the cytogram corresponds (does not contradict) the clinical diagnosis - cervical erosion.
Cytological conclusion: the cytogram corresponds (does not contradict) the clinical diagnosis of cervical ectopia, which suggests the presence of squamous epithelial cells in the surface layers and accumulations of columnar epithelial cells in the obtained material.
Conclusion: a cytogram of endocervicosis occurs if, in the direction for cytological examination, the clinical diagnosis of cervical erosion/ectopia is not indicated, but morphologically, squamous epithelial cells and accumulations of columnar epithelial cells are noted.
It is not always possible to make a cytological diagnosis between superficial endocervicosis (cervical ectopia) and proliferating endocervicosis. A descriptive cytological response occurs when: - squamous epithelial cells and single clusters or single columnar epithelial cells are found in the material obtained from the ectocervix; — cellular material was obtained from the ecto- and endocervix and presented in one mixed smear; - strokes are not painted.
With healing endocervicosis, smears reveal a large number of metaplastic epithelial cells (metaplasia is the replacement of one type of epithelium by another). Metaplastic epithelium is a target for the action of the human papillomavirus - an area for the development of precancerous conditions. The presence of a small number of metaplastic epithelial cells in cervical smears is an indicator of a normal physiological process.
Histogenetic mechanisms of replacement of columnar epithelium with squamous epithelium: - progression of squamous cell transformation - direct ingrowth of native epithelium under the columnar epithelium. As squamous epithelial cells develop and mature, the endocervical cells move upward, degenerate, and finally slough off. A similar process is observed during reepithelialization of true cervical erosion healing; - squamous metaplasia - proliferation of undifferentiated reserve cells of the endocervical epithelium and their partial transformation into fully mature squamous epithelium. The first stage of the process is the appearance of reserve cells, followed by reserve cell hyperplasia, followed by differentiation into immature squamous epithelium, and at the final stage, mature squamous epithelium is observed.
Leukoplakia of the cervix. When using the cytological method for diagnosing simple leukoplakia (benign lesion of the cervix, underlying disease), hyperkeratosis is revealed, i.e., in the material obtained from the ectocervix, layers (clusters) of squamous epithelial scales were found (there is no nucleus in the cytoplasm of the cell), separately lying squamous epithelial scales, dyskeracites . If there is a clinical diagnosis of cervical leukoplakia, the cytological report notes that the picture does not contradict the clinical diagnosis of cervical leukoplakia. In the absence of a clinical diagnosis of cervical leukoplakia, depending on the available material, the cytologist gives a descriptive answer, possibly with a recommendation to exclude cervical leukoplakia. Single scales of squamous epithelium have no diagnostic value. Leukoplakia with atypia is not always detected by the cytological method, which is explained by the presence of squamous epithelial scales on the surface of the stratified squamous epithelium, which prevent the production of cellular elements. It is necessary to conduct a morphological examination of a cervical biopsy specimen.
Cervical dysplasia. Dysplastic changes occur in the stratified squamous epithelium of both the exocervix and endocervix. As a rule, changes begin at the junction of squamous and columnar epithelium. Dysplasia can simultaneously develop in several areas of the cervix and cervical canal, often the changes are expressed to varying degrees. Spectrum dysplasia (CIN) is not a single disease. There are two biological entities of the process: a productive human papillomavirus infection and a cancer precursor.
Dysplasia-I (mild dysplasia, CINI) is one of the least reproducible cytological diagnoses. Often dysplasia-I is difficult to differentiate from reactively changed epithelium. It is not always possible to make a differential diagnosis between dysplasia III (severe dysplasia, CIN-III) and intraepithelial cancer by cytological examination.
Cytological conclusion: Dysplasia - I (weak, CIN-1); Dysplasia -II (moderate, CIN-II); Dysplasia -III (severe, severe, CIN-III). If the received material contains cells with signs of malignancy, the cytologist gives a conclusion about the cytogram of the malignant neoplasm and, if possible, specifies the form of cancer.
Inflammatory processes of the cervix. Inflammation - a cellular reaction (at the site) - is represented by degeneratively changed epithelium, proliferative changes of a reparative, protective nature, inflammatory atypia. In an acute nonspecific inflammatory process, a pronounced leukocyte infiltration (many neutrophilic leukocytes) and incomplete phagocytosis are noted in the smear. The composition of the epithelial cell population may change. Cytological conclusion: cytogram of ecto-/endocervicitis. In subacute and chronic inflammation, eosinophils, lymphocytes, macrophages/foreign body type cells (multinucleate macrophages) join - cytological conclusion: cytogram of chronic ecto-/endocervicitis. Acute inflammatory processes are more often observed in the age group of 20 - 24 years, chronic processes and their consequences occur in women 25 - 34 years old.
Infectious lesions of the cervix. Cytological features of smears for infectious lesions of the cervix depend on the pathogen and the duration of the inflammatory process.
Mycoplasma, ureaplasma and corynobacteria as the cause of inflammation are observed in a group of young women (under 20 years old). In the age group over 30 years old, anaerobic microorganisms occupy the first place among the causative agents of inflammatory processes in the genitals. Mixed infection increases the pathogenicity of each pathogen. In such cases, inflammation causes a pronounced tissue reaction, accompanied by epithelial damage, destruction and dysplasia. This leads to the development of not only colpitis and endocervicitis, but can play a significant role in the formation of cervical ectopia. Incomplete phagocytosis is noted (the phagocytic activity of leukocytes is suppressed). The cytological report indicates the type of flora with a recommendation to exclude a certain type of infection.
Bacterial vaginosis (BV) - (clinical diagnosis). In cytological preparations, BV is represented by key cells. If key cells are not found and the flora is cocco-bacillary, it is recommended to exclude the presence of Gardnerella (ureaplasma) in the cytological response; in the presence of mobiluncus bacilli, a recurrence of the pathological process after treatment is possible.
Genital herpes - the herpes simplex virus has a high tropism for epithelial and nerve cells. Relapses are mainly due to persistence of infection in the nerve ganglion. During a cytological examination of the obtained material, changes may be noted in the squamous epithelial cells that are specific to their damage by this type of viral infection: multinucleated cells of the “mulberry” type. Form of cytological response: signs of a viral infection were found in the material received. It is recommended to exclude the herpes simplex virus.
Human papillomavirus infection of the genitals. The human papillomavirus is capable of persisting for a long time in the basal layer of squamous epithelium, which determines the high frequency of recurrence of the process. The coincidence rate of cytological and histological diagnoses for condyloma was 42%: CIN-I - 56%, CIN III 74%. False-negative cytological responses are explained by the consequence of incorrect sampling of material - 90%, incorrect interpretation - 10%.
In addition, underdiagnosis in cervical smears may be associated with the presence of koilocytes in the deeper layers of squamous epithelium or the presence of a large overlapping number of inflammatory and flora elements. Cytological conclusion: signs of a viral infection were found in the material obtained. It is recommended to exclude human papillomavirus. Indirect changes characteristic of a viral infection: increased nuclear size, nonspecific multinucleation. Form of cytological response: the received material shows indirect signs of a viral infection. It is recommended to exclude the herpes simplex virus and human papillomavirus.
Trichomoniasis. An inflammatory reaction develops in the presence of a large number of protozoa. Proper patient preparation is important for a quality study. Discontinue the use of trichomonocidal agents 5 - 7 days before taking the material. The cytological specimen contains signs of acute/chronic inflammatory process, mixed flora, Trichomonas. Cytological conclusion: trichomonas colpitis.
Chlamydial infection. Chlamydia is tropic for columnar epithelium. Often found in women with cervical ectopia. In pregnant and menopausal women, signs of infection may be observed in the squamous epithelium. They can also be found in macrophages. Cytologically, the presence of intracellular specific inclusions is determined, which are more often detected with a fresh or untreated infection. Cytological forms of the response: cells with cytoplasmic inclusions were found morphologically similar to chlamydial infection. It is recommended to exclude the presence of chlamydial infection.
Squamous intraepithelial lesions (SIP) of the cervix are associated with significant qualitative and quantitative changes in the vaginal microflora. A deficiency of lactobacilli is observed in all patients with PIP, and an increase in representatives of opportunistic flora is noted. The cytological report indicates changes in the flora; if possible, a representative of the opportunistic flora is characterized. The presence of nonspecific vaginosis is noted.
Prognosis and prevention
The prognosis for treatment of the disease is favorable. Even in the acute period, the ability to work was preserved. Since patients who have had endocervicitis constitute a risk group for cervical cancer, they should be observed by a gynecologist at their place of residence with periodic colposcopy, cytological and bacteriological examinations.
The prognosis for endocervical stenosis depends on the causes of the disease, the timeliness of diagnosis and the correctness of the chosen treatment method. In most cases, correctly performed bougienage of the cervical canal and conization of the uterine cervix can completely restore the patency of the organ and reproductive function.
To prevent stenosis, it is recommended to plan pregnancy using modern contraceptive methods and avoid abortion, early diagnosis and adequate treatment of genital infections and tumor processes. An important role in preventing narrowing of the cervix is played by careful management of labor and the justified prescription of gynecological invasive procedures.