Recently, an increasing number of children are becoming ill with reactive pancreatitis. The reason for this is the increase in the number of products containing preservatives, dyes, and flavor enhancers. These are all kinds of crackers, nuts, chips, juices and sweet drinks from the store chain. The disease manifests itself in the form of spasms in the pancreatic ducts.
Enzymes produced in the pancreas itself cannot enter the gastrointestinal tract and begin to digest the gland itself. The disease occurs abruptly, sometimes even instantly, as a reaction of the little person’s body to various infections, such as respiratory disease, respiratory viral infection, intoxication due to ingestion of stale food. The pancreas may react to antibiotic treatment, the consequences of abdominal trauma, and negative psycho-emotional stress.
A little about pathology
In the process of evolution, the open system of the human body acquired numerous protective and adaptive reactions of variable orientation and mechanism of action. Inflammation is one of them, perhaps not the way a person would like it to be, therefore, until a certain period in the development of science, it was interpreted as a disease. Practical medicine has interpreted the inflammatory reactions of the pancreas or liver as an independent disease, but in fact it is a protective-adaptive mechanism triggered by the threat of disturbances in physiological homeostasis.
I.I. Mechnikov gave a definition of this process that was somewhat different from the then traditional understanding. He noted the important role that inflammatory reactions play in preventing the negative consequences of destructive factors and at the same time their pathological nature:
- As soon as an open system detects damage of any etiology (trauma, toxic effects, the result of individual disturbances in the functioning of an organ or system), it triggers a mechanism formed in the process of evolution.
- Regardless of the patient, changes in blood vessels, hemorrhagic fluids and tissues begin in his body, aimed not only at destroying the pathogenic agent, but also at restoring the damaged area.
- Conventionally, inflammation is divided into septic, caused by the presence of infection, and aseptic (reactive), developing for no apparent reason. It can be perceived as a reaction to changes that have occurred in the immediate vicinity of the site of invasion.
- In any case, the goal of its development is to eliminate the source of the lesion and the factors that provoked it. Sometimes this is impossible, and then the source of damage is limited and rejected, and it does not matter whether it is of foreign origin or is its own area, transformed beyond recognition.
The inflammatory process is launched to destroy the damaging factor and the consequences of its pathological dynamics. But in its development in the body there are positive and negative sides, therefore, in the understanding of general pathology, it is not just a negative localized phenomenon, with all the corresponding signs. It affects both the place of localization and the entire organism as a whole, threatens the organ and helps the system survive, in the process of eliminating the foreign and its demarcation (fencing, restrictions on distribution) it damages its own.
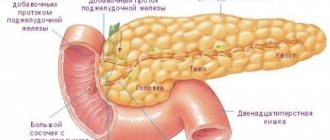
Where is the tail of the pancreas located?
The gland has a head, body and tail. The head of the pancreas is located in the fold of the duodenum. The body is presented as a prism with 3 sides, and the tail is the final, narrowest part of the pancreas, the final organ. Like the pancreas, the parenchyma of the tail has a glandular structure, and there are certain properties. The parenchyma is presented by acini and islets of Langerhans.
The acini is a simple working part of the pancreas that has different cells with enzyme-forming activities. An individual lobule has its own primary excretory channel with vessels; its cells produce a number of types of enzymes that are involved in the breakdown of fats, proteins and carbohydrates.
Endocrine work behind the islets of Langerhans. They are located in the middle of the acini, and include a variety of cell types that synthesize hormones. Unlike enzymes, hormonally active elements penetrate instantly into the blood and begin to act.
The tail of the organ is elongated, reminiscent of a pear, its top is slightly raised. In the area of the tail there is an excretory canal, the duration of which is 13-16 cm, it runs throughout the entire gland. It spreads to the leading side of the peritoneum from the side and falls on the left side under the rib somewhere in the middle of the component from the urinary process to the navel. The tail area is adjacent to the kidney on the left, the spleen, and the adrenal gland.
The development of inflammation and its causes
Reactive changes in the liver and pancreas in a child are the result of the development of an inflammatory process that affects one or the other gland (liver, pancreas) or even both at once. Since the term “reactive” is sometimes replaced by the definition “aseptic”, it is assumed that an infection of the pancreas or liver - bacteria, viruses or infections - is not involved in the formation of inflammation and its negative consequences.
However, it always presupposes a certain reaction of the body (both pathogenic and adaptive), and occurs as a response to the action of one or more provoking factors (sometimes called pathogenic or phlogogenic).
In a child or an adult, reactive changes in the endocrine (pancreas) and (or) exocrine gland (liver) occur not only under the influence of phlogogen. This is a process launched to destroy, eliminate or limit (localize, demarcate) negative phenomena. Timely correction and proper treatment can even eliminate the destructive consequences of its action. In a child, reactive changes occur under the influence of:
- physical factors - tissue injury by any means - electric current, high temperature, radiation, hypothermia;
- chemical compounds with phlogogen properties - acids of any origin, waste or products of metabolic reactions, constituent components of natural biological fluids that have undergone changes - bile secretion, urine, salts, excreta, enzymes;
- biological agents - fragments of necrotic tissue, own cells that have undergone destruction under the influence of pathogenic factors and are perceived by the immune system as objects for immediate destruction.
The pancreas and liver may undergo changes, against the background of which inflammation of the organs is possible under the influence of various factors - external and internal. Such changes are possible not only in adults, but also in children. Non-infectious exogenous are foreign cells that enter the body through blood transfusion, transplantation and even vaccination.
The list of endogenous non-infectious factors in this case is wider. Common biological reasons are products of tissue destruction, own opportunistic microbes, activated by low immunity. Chemical - the result of the pathological action of the accumulation of metabolic products. All this is the result of metabolic disorders.
Healing procedures
If parents notice that the baby is lethargic, refuses to eat, is capricious, or the teenager is losing weight, eating poorly, complaining of nausea and abdominal discomfort, you should immediately contact a specialist.
The doctor will prescribe the necessary treatment after clarifying the diagnosis and rule out diabetes mellitus, which often develops when the pancreas is damaged.
Detected pathological changes in the liver and pancreas tissue must be treated comprehensively. The following therapeutic regimens are used:
- antispasmodic drugs - eliminate pain, relieve spasm of the sphincters of the pancreatic ducts and gallbladder, improving the outflow of digestive juice and bile;
- enzymes to relieve pain and better digestion of food;
- antihistamines if changes occur as a result of food or drug allergies;
- detoxification measures.
This treatment regimen received positive feedback from specialists and patients.
Mandatory treatment is carried out for the disease, as a result of which the structure of the pancreatic parenchyma has changed. With a peptic ulcer or erosive gastroduodenitis, due to the anatomical proximity of the organs, the head of the pancreas is involved in the pathological process: it begins to enlarge, and pain appears. To avoid complications of the underlying disease and the reactive state of the pancreas, it is recommended to do all prescribed procedures, take medications and follow a diet.
Changes in the gland disappear when the condition of the organ that caused them is normalized. The prognosis is always favorable, since functions are slightly impaired.
Changes in the pancreas
In a child, reactive changes in the endocrine gland occur in many cases, but there are two ways of developing inflammation of the pancreas: the first is the consequences of a constantly present disease of the digestive organ (or organs), the second, outwardly more harmless, is a violation of the conditions of normal existence.
It is interesting that the second category also includes systematic deviations from the normal diet (untimely or containing food components that are not recommended at this age) and poisoning with toxic components (food, medicinal, environmental), constantly present or strong at one time.
The degree of speed of occurrence of reactive changes directly depends on the origin and strength of the negative impact, the reactivity of the organism itself and the characteristics of the tissues in which they develop:
- normal reactivity corresponds to the provoking factor - the inflammation is completely adequate and is called normergic;
- increased (hyperergic) reactivity usually proceeds violently and leaves behind significant consequences: tissue damage, severe inflammation, pronounced symptoms due to the addition of additional risks (for example, an allergen);
- hypoergic or reduced reactivity is typical for infants or children of the first years of life; the process of the inflammatory reaction in this case is insignificant and the changes are weakly expressed.
Reactive changes in the pancreas or liver in a child are classified as nonspecific conditions of secondary etiology that accompany other, negative (diseases). This statement of transformations that occurred under the influence of the inflammatory process is not a diagnosis. The more intense the effect of the phlogogenic factor, the higher the severity of the destructive effect in the pancreas or liver, and the more acute the inflammatory process.
Diet in complex therapy of disorders
For inflammation of the pancreas, a diet is recommended for the baby. This is one of the prerequisites for successful treatment. General nutritional rules include:
- exclusion of any irritating foods (smoked foods, salty and spicy, sweet, fatty, etc.);
- steaming all dishes (fried is completely excluded);
- eating food in whole and crushed form (for children under 3 years of age, food is ground both during the stages of exacerbation and during periods of remission);
- fractional meals (5–6 meals a day in small portions at time intervals of no more than 4 hours).
- warm drink (still mineral water, tea without sugar);
- mashed porridge;
- dairy products;
- vegetable soups, purees;
- fish;
- lean boiled meat (chicken, veal) or steamed cutlets.
Fresh vegetables, berries and fruits can be introduced into the diet about a week after the acute attack has stopped.
- baked goods, confectionery products;
- concentrated meat and vegetable broths;
- mushroom broths;
- fatty fish and meat;
- white cabbage in any form;
- fried foods;
- conservation;
- smoked and pickled foods;
- sausages;
- ice cream;
- carbonated drinks.
Following a strict diet will help to quickly stop an acute attack and normalize the functioning of the pancreas, and also prevent repeated exacerbations.
Main reasons for development
A variety of conditions can cause reactive changes in a child’s pancreas - diseases of the digestive system (gastritis, colitis, gastric ulcer), hepatobiliary system - hepatitis of any etiology, pathological processes in the gall bladder (cholecystitis) and bile ducts, congenital metabolic pathologies, hormonal disorders level. The process of changes in organ tissue under the influence of secondary inflammation is sometimes called reactive pancreatitis, but reactive changes are a more correct term, indicating the secondary nature of the pathology.
Predisposing factors can be not only diseases of the gastrointestinal tract and gastrointestinal tract (located nearby), but also diseases of the respiratory system. Despite the fact that the reactive process is considered aseptic, it can be triggered by an infection accompanied by acute inflammation - influenza or pneumonia, sore throat, pharyngitis.
In newborns, this condition is most often caused by congenital developmental anomalies or metabolic disorders. Older children are at risk of falling into the category requiring immediate care after blunt trauma to the abdominal cavity, constant consumption of fast food and sugary carbonated drinks with flavors and preservatives.
Pain, disturbances in normal digestion with a standard set of symptoms - from belching, nausea and vomiting to fever and general intoxication - are often mistaken for the consequences of banal food poisoning. But if you show the child to a specialist who will prescribe laboratory and instrumental tests, the true reason will be revealed. Timely diagnosis will allow you to eliminate reactive changes without any special consequences. It is enough to eliminate the cause and undergo the prescribed treatment so that the child’s condition returns to normal.
Symptoms
Parents should find out in a timely manner that their child has impaired pancreatic function. Indeed, in the event of the formation of stones, an abscess or a tumor, it is very important to provide the child with medical assistance in a timely manner. Even a normal reaction to poor nutrition can be dangerous. An increase in the size of the pancreas may be associated with a decrease in the production of enzymes necessary for digestion. This may negatively affect the functioning of the stomach, intestines or liver.
Therefore, it is very important to notice the symptoms of pathology in time. If the child can already speak, he may say that he feels nausea, a bitter taste in his mouth, or pain or a burning sensation in his stomach. There are also external symptoms: colic, bloating, vomiting, weight loss, weakness, pallor, fever and bowel dysfunction. The baby's stool becomes liquid and very greasy. It is difficult to wash off and a film may be visible on its surface. And due to the fact that the breakdown of proteins and carbohydrates is impaired, it emits a particularly unpleasant odor.
What do reactive changes in the pancreas look like?
The main diagnostic method is ultrasound, but additional laboratory diagnostic methods are also needed to interpret it. The symptoms of pancreatitis and reactive changes are approximately the same - the gland becomes granular and the level of echogenicity increases. In case of inflammation of the pancreas, the organ increases in size.
Determination of reactive changes in the acute course is carried out by symptoms - characteristic clinical manifestations. In a chronic process, the main indication of the presence of the condition is general blood and urine tests, stool tests for digestibility and elastase, and urine and blood tests for amylase.
If a child has sleep disorders, complete with lack of appetite, lethargy and inertia, which are unusual for age, it is likely that there are some problems in his body that have caused changes in the pancreas. Only timely examination and correct treatment will help to avoid a negative scenario.
How to return the gland to normal size
To understand this issue, you will need the help of a gastroenterologist. If you are sure that your child has an enlarged pancreas, then start giving your baby mineral alkaline water more often.
If you feel pain, apply cold to this place (as a rule, it is located just to the left of the navel). If the pain is severe, call an ambulance. The doctor will choose treatment tactics based on diagnostic data. There are 2 types of therapy: conservative and surgical.
Approximate scheme of the treatment process:
- Secretory activity is suppressed with the help of proton pump inhibitors. Histamine receptor blockers are administered and hormones are prescribed.
- To reduce swelling, apply a cold heating pad to the sore spot.
- To correct the functioning of the pancreas, enzyme preparations are prescribed.
- Parenteral nutrition is possible, i.e. injections with vitamin components are given.
- An operation to eliminate inflammation or dead tissue.
Since the pancreas is often enlarged due to pancreatitis, in this case it is advisable for the child to fast for a while. At this time, various nutrient solutions can be introduced into the body.
If you prescribe a diet, it will be called table No. 5, which provides nutrition aimed at restoring the functioning of the pancreas. This diet provides for the following food intake rules:
- Lean meat should be either boiled or steamed.
- Dairy products are not fatty.
- Porridges cooked in water, except millet. Over time, the water can be gradually replaced with milk.
- Boiled or steamed vegetables.
- If it’s tea, it’s not strong, with a small amount of sugar. It is also recommended to drink rosehip decoction.
- Fruits baked without adding sugar and honey.
- Bread in the form of crackers or dried in the oven.
- Biscuits.
Important information: How to restore the functioning of the pancreas in case of chronic pancreatitis
Spices and sugar should be present in minimal quantities. Fatty, smoked, fried and spicy foods are prohibited. You should not eat sour fruits and berries, as well as the following vegetables - garlic, radish, radishes, onions. Sweets in the form of candies, chocolate, and cakes are also excluded. If you eat even a little of all these forbidden foods, the pancreas will enlarge again.
Liver pathologies
Changes of this kind in children are observed much less frequently than in adults, but they can pose a greater degree of risk due to the functional immaturity of the organ before a certain age. As in the case of the pancreas, pathological transformations are the result of factors located outside the gland itself, but having a direct impact on its condition.
Aseptic inflammation can be a consequence of variable diseases or disturbances of normal functionality, including a consequence of an infection located in another segment. Therefore, by reactive hepatitis we mean the result of the destructive action of inflammation occurring outside the liver, affecting its structural segments.
Depending on the main provocateur, reactive changes in the liver can affect its vascular network and parenchyma. In this case, more significant damage is possible. In a child, reactive changes can progress quickly and lead to serious consequences. The reason for this will be the immaturity of the exocrine gland. But there are much fewer reasons for the development of pathology in a child than in an adult - such statistics are explained by more careful monitoring of the baby’s condition and the absence of chronic diseases.
In this case, jaundice appears slightly or is absent altogether. Pain symptoms and dyspeptic symptoms are not much different from other liver pathologies. The course of changes can also be asymptomatic, and laboratory tests reveal only subtle deviations - the presence of bilirubin fractions and liver transaminases. No structural changes were found in the parenchyma.
Prevention of pancreatic diseases in children
To prevent a child from having problems with the pancreas, it is necessary to establish a proper diet from an early age, ensure proper sleep, and walks in the fresh air. These preventive measures have received good feedback from specialists who have been involved in the treatment and prevention of digestive diseases for a long time.
If there is the slightest disturbance in the child’s condition, you should immediately consult a doctor. This will make it possible to avoid severe complications and long-term treatment.
Bibliography
- Ostrovsky A.G., Karashurov E.S. Rare diseases of the pancreas: Textbook. Petrozavodsk, 1988
- Sokolov Yu.Yu. Diagnosis and surgical treatment of duodenopancreatobiliary anomalies in children. Abstract of the dissertation. Moscow, 2002
- Nutrition of a healthy and sick child. Under. Ed. V.A. Tutelyan, I.Ya. Konya, B.S. Kaganova. M. Publishing House "Dynasty", 2007
- Sokolov Yu.Yu. Surgical tactics for pathology of the organs of the biliopancreatoduodenal zone in children. Collection of scientific works. M. 1997, Issue 1, pp. 11–43.
Danger of condition
Reactive changes in the liver in a child are difficult to differentiate from other common pathologies of the organ - hepatitis, viral and toxic. The main task of diagnosis and the condition for the success of therapy is to determine the secondary nature of the condition and treat the main provoking factor. Once it is eliminated, the organ's ability to self-regenerate will allow it to successfully restore its function in the early stages. The cause of the inflammatory process in the pancreas can be changes in the structure of the liver, but the opposite is also possible.
The development of changes in the exocrine gland can occur for various reasons. Their list is no less wide than in the case of damage to the endocrine gland. Reactive changes can be the result of diseases of any segment of the GBS and digestive system, endocrine and infectious nature, oncological process, toxic effects (external or as a result of taking medications), burns, liver injuries, hereditary anomalies and systemic pathologies. Until the underlying cause of liver inflammation is discovered, there is always a risk of progression, complications and even death.
Treatment
Moderate reactive changes usually do not require separate special therapy. Usually everything returns to normal after the treatment of the underlying disease of the gastrointestinal tract, which led to disruption of the pancreas, is completed.
Severe diffuse changes in the parenchyma of the gland are treated in a hospital setting under constant medical supervision. Therapy includes antispasmodics (No-shpu, Papaverine) to reduce pain, enzyme preparations (Pancreatin and others), as well as vitamins and minerals. The child may also be prescribed antihistamines to relieve allergy symptoms, which, if present, may worsen the child's condition.
A prerequisite for recovery is a strict diet. In case of severe pain and vomiting, the child is given 1-2 days of therapeutic fasting, and then food is introduced gradually. The diet excludes fried and fatty foods and dishes, carbonated drinks, cocoa and chocolate, smoked and canned foods, and pickled foods. Vegetable soups, porridges, jelly, compotes with a low sugar content, fresh vegetables and fruits are useful.