The pancreas (PG) performs two important tasks in the body: the production of a special secretion involved in the digestion of food and the production of the hormone insulin, which is responsible for the absorption of glucose.
pancreatitis in a child
Pancreatitis in children is an inflammation of the tissues of the pancreas and secretion ducts. Disturbances in the functioning of such an important organ lead to serious consequences, so parents need to know how to detect the disease in order to promptly seek medical help.
Causes of inflammation
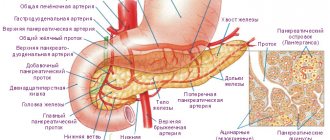
The pancreas or pancreas has an oblong structure and includes a head, body and tail. The parenchyma consists of glandular tissue and ducts.
An enlarged gland can be caused by a number of reasons:
- Congestion accompanied by impaired blood flow.
- Plasma enters the intercellular substance of tissues, which causes edema.
- Violation of the outflow of pancreatic juice into the lumen of the duodenum.
- Growth of pathological neoplasms.
The causes of inflammation of the pancreas must be taken into account when selecting therapy.
Pancreatitis is a pathology whose development can be influenced by many factors. Usually the occurrence is due to systemic diseases, unhealthy diet - the predominance of fatty foods in the diet.
As already mentioned, with pancreatitis the pancreas suffers. It is located next to the stomach, its functions include the production of various groups of enzymes to facilitate the digestion process and absorb the maximum amount of substances necessary for the body.
Pancreatitis provokes inflammation of the pancreas tissue, which causes a failure in the production of enzymes. This negatively affects the digestion process, causing serious harm to the child’s health.
Important!
Lack of treatment can lead to irreversible consequences - inflammation of the gland tissue can completely destroy its structure.
Principles of proper nutrition
The main rule in treatment is the correct diet for pancreatitis:
- exclusion of pancreatic irritants from the diet;
- food is cooked by steaming, baking;
- all food consists of a porridge-like substance (ground);
- reduce consumption of fatty foods and carbohydrates;
- increased frequency of eating up to 6-7 times a day, in small portions.
On the first day after an attack of pancreatitis, strict abstinence from eating food for 2-3 days is recommended. During this period, it is allowed to take decoctions of rose hips, chamomile, and mineral water without gases.
Only after passing the threshold of exacerbation of pancreatitis by hunger, you can gradually begin to consume dietary foods and food.
The necessary diet for pancreatitis helps restore the functioning of the pancreas and speeds up recovery.
Classification of pancreatitis
In children, the disease is classified into forms - acute and chronic. Pancreatitis is considered chronic if it lasts for more than six months. The acute form provokes swelling and catarrhal inflammation of the gland tissue. In especially severe cases, hemorrhages occur, which provoke necrosis of gland tissue.
The nature of the changes occurring in the tissues of the gland divides pancreatitis into:
- acute edematous;
- hemorrhagic (with hemorrhages);
- purulent;
- fatty pancreatic necrosis.
Typically, the causes of pancreatitis in children are nutritional disorders. Being under constant load, the gland tissues lose their properties and begin to degenerate, reducing their activity.
In children over 7 years of age, chronic pancreatitis of a latent or recurrent nature is usually diagnosed. The acute form is less common in children.
Depending on the origin, pancreatitis can be:
- primary;
- reactive, occurring against the background of inflammation of other organs;
- hereditary.
Diet for the treatment of pancreatitis
Nutrition in the treatment of pancreatitis is extremely important. At the beginning of treatment, the baby is prescribed a complete fast for a period of 1–3 days, during which he is allowed to drink only warm, non-carbonated mineral water. After this, the patient is transferred to a special diet. During the period of fasting, the child's gastric juice is constantly removed, as it provokes the release of enzymes in the pancreas.
porridge when dieting
After the end of the three-day fast, the child is gradually given food: first liquid porridge, then vegetable soup or puree, compotes and jelly. Food is given five to six times a day, in small portions and heated. Then eggs are gradually introduced in the form of a steam omelet, boiled meatballs and fish. All food is served in highly chopped form.
About a month after the start of treatment, the diet is expanded: fermented milk products, bread, sour cream, vegetable and butter are given. The food is served whole.
diet 5
For six months after the end of treatment, the child is kept on a diet that excludes foods that irritate the gastrointestinal tract: rough food, pickles, smoked foods, soda, fatty and fried foods.
In parallel with the start of feeding, the child is prescribed enzyme preparations to help digest food. They should be taken for at least the first three months. Then, based on the test results, they are cancelled.
Reactive pancreatitis in children
In the case of reactive pancreatitis, the process is reversible; it is only necessary to identify and begin to treat the underlying disease in time. If left untreated, the disease progresses to true pancreatitis. Such problems are more common in children aged 10–14 years.
The etiology of reactive pancreatitis lies in existing foci of infection in other organs, which complicate the functioning of the pancreas. In addition to infectious diseases, the reactive form can be caused by taking antibiotics and other potent medications.
The latent form is not characterized by obvious clinical manifestations, but the relapsing type of the disease occurs in waves - exacerbations alternate with remissions. Exacerbation of inflammation of a chronic process, like acute pancreatitis, can be mild, moderate or severe.
Treatment with folk remedies
Reactive pancreatitis in a child cannot be cured without the use of medications. However, to relieve symptoms, you can resort to the help of recipes from traditional healers. Before starting a course of therapy, you should consult your doctor.
One of the popular products in the treatment of pancreatitis is royal jelly. It can only be used if the child is not allergic to honey. The duration of the course of therapy is 2-3 months. Then you need to take a short break for a few days. It is recommended to take royal jelly one teaspoon three times a day. It is better to slowly dissolve the sweet treat rather than swallow it whole.
You can also make homemade kvass from celandine. To prepare it you will need 3 liters of whey. If you cannot find it, you can replace it with plain water. The liquid must be poured into a vessel, add a teaspoon of sour cream and sugar. Pour half a glass of celandine herb into a gauze bag and place it in a jar of water or whey. You need to stir the kvass daily for two weeks. If you strictly follow the instructions provided, on the 10th day the drink should begin to foam. Take kvass for a week, a tablespoon three times a day.
Reasons for organ enlargement in children
Inflammation of the pancreas in a child can be caused by a number of pathological conditions:
- Closed abdominal injuries associated with a fall or other mechanical damage; against this background, an enlarged spleen can often be observed.
- Autoimmune disorders are malfunctions of the immune system, in which the body begins to produce antibodies to its own tissues, including the pancreas.
- Poisoning with chemicals , causing disruption of the digestive system. Against this background, an enlarged liver is often observed.
- Infectious processes in other organs.
- Chronic pancreatitis can be caused by improper treatment of the acute form of the disease.
- Growth of neoplasms in organ tissues , abscess, cyst, benign or cancerous tumor. Inflammation of the organ can be localized - for example, only the tail of the gland enlarges.
- Stomach ulcer , in which the integrity of the structure of the mucous membrane of the stomach or duodenum is disrupted. Over time, this leads to dysfunction of the pancreas and an increase in its size.
- Duodenitis is an inflammation of the duodenum that obstructs the outflow of pancreatic juice.
- Cystic fibrosis is a systemic congenital pathology that provokes damage to various glands, including the pancreas.
Important!
Identifying the main cause of pancreatic inflammation in children is a mandatory diagnostic measure. Further treatment will be based on these data.
Symptoms of the disease
https://youtu.be/VLz_sFK08BY
The symptoms of the disease are clearly expressed in older children, but in children they are subtle, sometimes even not manifested at all. The first sign of acute pancreatitis is severe pain in the lower abdomen that occurs suddenly. Sometimes children note that the area around the navel or the entire abdomen is painful.
In addition, reactive pancreatitis in children is characterized by the following symptoms:
- frequent vomiting that does not provide relief;
- increased body temperature;
- yellowing of the skin;
- very light-colored stool;
- rich color of urine;
- general anxiety, screaming and crying in babies, loss of appetite.
The child may also experience:
- fluctuations in blood pressure;
- bloating;
- frequent shortness of breath;
- secretion of sticky sweat.
In this situation, the correct reaction of parents is important. They should provide the child with peace and place a cold heating pad on the stomach, moving it slightly to the left. Do not feed under any circumstances! Call an ambulance!
Symptoms, signs of inflammation
Inflammation of the pancreas in children is usually mild. The younger the child, the less pronounced his symptoms of the disease.
The acute form of the disease is expressed by sharp paroxysmal pain (it can be relieved), often of a girdling nature, which radiates to the hypochondrium and spine. In addition, pancreatitis is characterized by lack of appetite, nausea, increased gas formation, diarrhea and vomiting.
Subfertile temperature, pale skin, dry mouth, and coating on the tongue are observed. With tissue necrosis, the temperature rises sharply, obvious signs of intoxication and intestinal paresis appear. The development of a collaptoid state is possible.
Kinds
Each type of disease has its own distinctive signs and course characteristics.
Spicy
The acute form of the disease often occurs in children 10-12 years old. The patient may develop purulent-necrotic lesions of the pancreas. Sometimes treatment is only possible through surgery.
Pain in this form of pancreatitis is girdling in nature, but can also be localized in the umbilical region.
Sometimes the patient feels back pain. In children, the functioning of the gastrointestinal tract is disrupted, diarrhea and flatulence occur. Children lose their appetite. A white coating appears on the tongue. Blueness of the limbs and face may occur. Body temperature rises.
Chronic
In the chronic form of the disease in children, the signs are mild or practically absent.
The chronic form of the disease in a child most often develops due to poor nutrition.
The pancreas is destroyed gradually. The chronic form of the disease most often develops with poor nutrition.
Useful video
Video about symptoms (where it hurts, what can cause a breakdown):
Symptoms of the chronic form depend on the duration of development of the pathological process, the stage and form of the disease, the degree of damage to the pancreas and other digestive organs. The child is bothered by periodically occurring aching pain in the right hypochondrium, which is aggravated by eating disorders, after physical exertion or stress.
The attack can last from several hours to several days. Children suffering from this form of the disease have no appetite and periodically suffer from heartburn, nausea, and vomiting. Constipation replaces diarrhea. There is weight loss.
Important!
Complications of pancreatitis in children are quite dangerous - false cyst, pancreolithiasis, peritonitis, pleurisy, diabetes mellitus.
ethnoscience
Along with traditional methods, the baby is also treated with non-traditional means. In the chronic form of pancreatitis, children have to constantly be given medications that do not have the most beneficial effect on the body due to their side effects. Natural remedies, if used successfully, will not only be a good help, but even replace taking medications, supporting the pancreas weakened by the disease. In the long term, this will have a beneficial effect on the child’s health.
herbs for pancreatitis in children
A good addition to drug treatment and a special diet will be various herbal decoctions, vegetable juices and mineral water. There is also a special recipe for jelly that effectively relieves inflammation in pancreatitis.
The list of herbs that can help with pancreas problems is quite large: chamomile, St. John's wort, horsetail, licorice root, and so on. However, it is recommended to use infusions from these herbs only after consultation with a gastroenterologist and herbalist. Some plants affect the production of enzymes, while others are only suitable for children from a certain age.
Therefore, to clarify the composition of folk remedies that are given to a child, a doctor’s consultation is needed in each individual case.
Diagnosis of the disease
The prognosis of treatment directly depends on the timeliness and correctness of diagnosis. After a visual examination and medical history, the doctor prescribes a series of examinations to confirm the diagnosis.
The child must have blood, urine and feces tested. The study will show whether there is inflammation in the body and indirectly confirm the development of pancreatitis in the child. An ultrasound examination of the abdominal organs and fibrogastroscopy will show a clearer picture. The conducted studies will help the specialist to reliably assess the patient’s condition and prescribe the necessary therapeutic measures. If treatment is necessary, the child may be hospitalized.
Diagnostics
To make a diagnosis, clinical examination data, complaints are used, laboratory (general clinical blood and urine tests, biochemical blood tests) and instrumental research methods are performed.
For instrumental diagnostics the following is used:
- ultrasound examination of the pancreas,
- angiography,
- contrast radiography,
- CT,
- MRI.
Treatment of the disease is carried out in a hospital setting. In the first days, food intake is excluded. This provides rest for the pancreas. Alkaline drinking is recommended, at a rate of 5 ml/kg. Only on the third day is a gradual transition to good nutrition (diet No. 5).
Treatment of reactive pancreatitis is predominantly symptomatic. Reactive pancreatitis in a child requires the prescription of vitamins and strengthening treatment. The diet is gentle, with the exception of fatty fried foods and smoked foods. In the acute stage, intravenous infusion therapy is performed. To relieve pain, antispasmodic treatment is used - spasmalgon, No-shpa.
Methods and rules for treating illness, illness
Any therapy begins with finding out the causes of the disease. Sometimes it is enough to eliminate the provoking factor and pancreatitis will subside. Separately, congenital anomalies should be touched upon - this requires medical supervision of the child for many years.
One of the main reasons for the progression of inflammatory processes in the pancreas in adolescents is malnutrition - schoolchildren's pancreatitis. The main thing in the treatment of such a pathology will be a strict diet.
Nutrition for pancreatitis in children
Diet is an essential component of therapy. You need to know what to feed and what products to buy. It will help eliminate problems in all organs of the abdominal cavity and the pancreas as well.
Basic nutrition rules:
- fractional meals - 5-7 times a day in small portions;
- refusal of unhealthy foods: fast food, fizzy drinks, fatty, fried, salty, spicy, preservatives;
- a balanced diet, which includes various cereals, pasta, dairy products, lean meat and fish, vegetables and fruits;
- predominance of boiled and steamed food;
- eating not hot, but only warm food;
- fresh food for cooking.
Drug treatment
The diet will help reduce the load on the digestive organs. In addition, the doctor prescribes enzyme preparations that improve the digestion process:
- "Creon."
- "Festal".
- "Mezim forte."
These medications are taken with meals. Children may also be prescribed medications containing bifidobacteria, for example, Bifacil.
To alleviate the patient's condition, the following is prescribed:
- Pirenzepine, Famotidine.
- Pancreatin.
- No-spa, Mebeverine, children's Paracetamol.
In more severe cases, antibiotics are prescribed; antihistamines; drugs that help improve blood microcirculation; protease inhibitors.
Important!
Treatment comes down to following simple measures, the main thing is that the child understands the importance of these actions - this will benefit him not only now, but will also allow him to live fully in the future.
What to do with very young children
If the disease is diagnosed in a very young patient, the nutritional rules will be as follows:
- predominance of protein foods;
- cooking any porridge with water;
- vegetables and fruits should be heat treated.
Sometimes surgical intervention is necessary, for example, in cases where there are congenital anomalies in the pancreas. The decision to undergo surgery is made after a comprehensive examination and only if there are no results from conservative therapy.
Treatment of pancreatitis in children is often performed in a hospital setting. Only here doctors will be able not only to treat the baby, but also to monitor his nutrition, observing the dynamics of therapy.
Traditional methods of treatment
From time immemorial, potato juice has been considered one of the effective methods of treating pancreatitis. You need to grate 2-3 potatoes along with the peel and squeeze out the juice. Directions for use: 50 ml 2 times a day. The course of treatment is 2 weeks. Then a week break and repeat the course. An excellent addition to kefir is low-fat kefir, which is consumed 5-10 minutes after taking the main product.
Important!
Regular honey can protect you from many diseases. If the child does not have an individual intolerance to this product or diabetes, a good habit would be to eat 1 tsp. honey in the morning, diluted in milk or water.
It is necessary to take St. John's wort, motherwort, and immortelle inflorescences in equal proportions. 2 tbsp. Boil the collection for 10–15 minutes in 1 liter of water, let the broth brew for 2 hours, strain. The course of administration is 50 days, half a glass before meals.
A complex but very effective collection. You should take equal proportions of dry burdock root, buckthorn bark, plantain, blueberry leaves, dill and flaxseeds. Add dandelion root, knotweed and sage. The preparation method is identical to the previous remedy - for 1 liter of water, 2 tbsp. collection, boil for 10–15 minutes. The course of administration is 14–20 days, half a glass after meals.
Important!
Any treatment methods for very young patients must be agreed with a doctor, otherwise self-medication can lead to irreversible consequences.
If a child has an enlarged pancreas, it is necessary to first find out the causes of this condition, and only then begin therapy. Timely detected pathology will allow you to avoid surgery and cure the disease using conservative methods. Read also about bending of the pancreas in children.
Mechanism and reasons
Food that is crushed in the mouth, soaked in saliva, and then gastric juice, enters the duodenum. At this point, pancreatic juice passes into the intestine and completes the digestion process.
In the case when this does not happen due to swelling of the organ or spasm of the duct, enzymes are supplied in insufficient quantities, and symptoms of pancreatopathy (dyspancreatism) develop with transient swelling of the organ.
The reasons for the development of this pathology are:
- poor nutrition and consumption of heavy foods (fatty meat, spices), overeating;
- introduction of a new dish (spicy or meat);
- untimely or abrupt introduction of complementary foods to children under one year of age;
- children drinking grape juice;
- poisoning from poor-quality food or food allergies (including hereditary intolerance to a number of foods);
- abdominal injuries (bruises, blows, wounds);
- infectious diseases;
- ARVI, influenza;
- use in the treatment of certain types of medicines;
- chronic disorders of the liver, gall bladder, upper intestine;
- fibrotic changes or congenital abnormalities of the structure of the pancreas.
Important! All of these factors equally influence the formation of reactive pancreatopathy in people of any age. But due to the imperfection of the digestive system, it is children who suffer from it more often.
Prevention
As preventive measures against inflammation of the pancreas, it is recommended:
- a balanced diet, including all necessary micro- and macroelements;
- refusal of junk food;
- timely detection and treatment of pathologies of the digestive system;
- promptly identify and eliminate helminthic infestations in the body;
- when prescribing potent drugs, monitor the general condition of the child;
- use only high-quality and fresh products for cooking;
- do not overeat, so as not to overload the pancreas.
If you experience any symptoms of pancreatitis, you should immediately consult a doctor. This will help avoid many problems and prevent relapses of the disease in children. Self-medication can cause complications that will subsequently require additional treatment.
Consequences and complications
In the absence of timely treatment of reactive pancreatitis, the following consequences are possible:
- the disease will become chronic. The child will be forced to adhere to dietary nutrition constantly;
- a complication may be pancreatogenic diabetes mellitus, which affects blood vessels, kidneys and nerves. The disease leads to atherosclerosis;
- Exocrine pancreatic insufficiency occurs in children. With this pathology, the production of enzymes in the diseased organ decreases. Replenishment of missing enzymes occurs through the use of special medications.
Treatment of the disease
Treatment of pancreatitis in children is supportive care. There is no single drug or treatment to help the pancreas recover. If you experience severe pain, you can take a painkiller. Nausea and vomiting are treated with antiemetics.
If it is impossible to eat food in the usual way, the child is not fed, but fluid is administered through a vein to avoid dehydration. In terms of nutrition, you need a certain diet, starting with clear broths and ending with regular foods. The baby’s health returns to normal on the first or second day after the attack. But with more severe attacks, symptoms remain for a longer time. Then the child is fed through a feeding tube to prevent digestive upset.
Treatment for reactive pancreatitis in children is carried out only in the hospital, with bed rest. Treatment consists of three parts - drug treatment of the underlying disease, treatment of pancreatitis, and diet therapy. Only by following these three rules is a complete recovery possible.
Medicines that are necessary for treatment should be divided into several groups:
- painkillers that should be taken to relieve pain and stop an attack;
- enzyme preparations used to improve the digestive system. These drugs are divided into several subgroups: drugs containing enzymes and drugs containing bile.
To improve the effect of these medications, doctors advise using antacids that help reduce acidity.
Preventive actions
The main reason for the development of pancreatopathy in children is poor nutrition and overeating .
This leads to the fact that the pancreas cannot cope with the load and most of the food is not digested or absorbed. Simple rules will help prevent disease:
- eat often, but in small portions;
- drink plenty of fluids;
- refusal of fried and rough foods;
- eat only clean fruits and vegetables;
- Minimize the amount of seasonings and salt.
Let's imagine a sample menu for children 12 years old with problematic digestion:
- Breakfast - porridge cooked in water with milk, berry jelly.
- Second breakfast - steamed egg white omelet.
- Lunch – vegetable soup, boiled fish with mashed potatoes.
- Afternoon snack – baked apple with honey.
- Dinner – stewed vegetables with minced beef.
Following a diet will help prevent the development of the disease, as well as reduce discomfort in a child with pancreatopathy.
Hypofunction of the pancreas affects not only the child’s nutritional process, but also its formation. This disease causes nutritional deficiencies, which leads to weight loss and developmental delays . That is why it is so important to try to prevent the development of pancreatopathy or to begin treatment in a timely manner.
https://youtu.be/X9E_5wkywVE