Many people are interested in where the rectosigmoid colon is located. What diseases are associated with this area? Let's find out in this article.
Rectosigmoiditis is an inflammation of the distal regions of the large intestine, that is, the rectum and sigmoid colon. This disease can be acute and can also become chronic. The acute form of the disease is manifested by cramping pain, diarrhea, nausea, tenesmus, weakness, and, in addition, chills and hyperthermia. Against the background of chronic rectosigmoiditis, the pain is aching or pulling. In addition, false urges with diarrhea are observed, and intoxication syndrome is possible.
Diseases of the rectosigmoid rectum are diagnosed based on complaints, examination, rectal and endoscopic examination. Patients also undergo stool tests and a biopsy. Treatment involves following a diet, antibacterial therapy, symptomatic treatment and the use of local anti-inflammatory drugs.
So, where is the rectosigmoid colon located?
Anatomy
The rectosigmoid junction is the section of the rectum that is located fifteen centimeters above the anus. The human rectum extends from the anorectal junction all the way to the sigmoid colon.
The rectosigmoid region is located in the bony pelvis; this area is surrounded by muscles, organs of the genitourinary system, and, in addition, ligaments and various connective tissue structures. This section controls the natural mechanism of bowel movement. The human rectum is partially located extraperitoneally. Its proximal border is the rectosigmoid junction.
The rectosigmoid region consists, as a rule, of the mucous membrane, and, in addition, the submucosal layer. It is also formed by the muscular layer. Outside, it is covered with powerful fascia.
The mucous membrane of the rectosigmoid rectum is covered with columnar epithelium, which has a large number of goblet cells. This membrane, among other things, contains a lot of liberkühn glands, which consist almost entirely of mucous cells. It is for this reason that in the presence of pathological processes, copious amounts of various mucus are released from the rectum.
Blood supply in the rectosigmoid part of the rectum is carried out by the lower, and at the same time the middle and upper hemorrhoidal arteries. Of these, the superior artery is unpaired, and the remaining two are paired; they approach the rectum from the sides.
Basic information about rectosigmoiditis
What pathologies occur in the rectosigmoid colon?
Rectosigmoiditis belongs to the group of acute and chronic inflammatory pathologies of various origins that affect the rectum and sigmoid colon. Rectosigmoiditis is the most common type of colitis. It occupies a leading position in frequency among proctological pathologies. It is often diagnosed in adults. In particular, the likelihood of developing this disease increases between the ages of twenty and forty years and after fifty-five.
Etiology
The ethology of sigmoid colon polyps has not been fully studied, which is why effective preventive measures have not been developed. However, clinicians identify the following possible reasons for the formation of a rectosigmoid polyp:
- inflammatory processes in the gastrointestinal tract, which are chronic;
- disruption of intestinal microflora due to frequent food poisoning or chronic gastroenterological ailments;
- poor nutrition. In this case, it means following a diet that is poor in natural products, fiber, essential vitamins and minerals;
- abuse of alcoholic beverages and surrogates;
- genetic predisposition - according to statistics, 35% of patients with this diagnosis had the same clinical cases in their family history.
Rectosigmoiditis and its causes
Inflammation of the rectosigmoid colon occurs with specific and some nonspecific infections, and, in addition, against the background of inflammatory bowel diseases, in the presence of helminthiasis, nutritional disorders and as a result of stagnation of feces. Among other things, the cause of rectosigmoiditis may be poisoning by toxic compounds along with local disturbances in the blood supply. Also, the causes of this disease may be:
- Spread of inflammatory processes from neighboring organs.
- The presence of chronic diseases in the digestive areas.
- Diseases of the pancreas and liver.
- Conducting radiation therapy.
Infectious rectosigmoiditis can develop under the influence of pathogens. The nonspecific nature of the disease includes inflammation of the lower intestines in the presence of salmonellosis, dysentery, cholera and other similar infections with oral transmission. A specific type of rectosigmoiditis can be observed against the background of local infection with the causative agent of syphilis, gonorrhea and a number of other diseases that are sexually transmitted.
The parasitic nature of the disease of the rectosigmoid region can occur in the presence of giardiasis, ascariasis, enterobiasis and other helminthiases. The causes of alimentary rectosigmoiditis are the following factors:
- Alcohol abuse.
- Excessive addiction to spicy, and at the same time to salty and fatty foods.
The congestive form of the disease develops with constipation due to traumatization of the intestinal walls by excessively dense feces. The toxic nature of rectosigmoiditis can be diagnosed against the background of an overdose of certain medications, due to mushroom poisoning, and so on.
Sometimes this disease occurs as a result of the transfer of infection from nearby tissues and organs, for example, against the background of paraproctitis, vaginitis or urethritis. Rectosigmoiditis often affects patients who have other chronic diseases of the digestive system. For example, rectosigmoiditis can occur in the presence of gastritis, cholecystitis, diseases of the pancreas, gall bladder or liver. Among other things, the cause of rectosigmoiditis, as well as cancer of the rectosigmoid region, may be radiation therapy for oncological pathologies of the pelvis.
Functions
The sigmoid colon performs important functions for the body:
- The sigmoid colon contains beneficial microflora. It helps strengthen the immune system, participates in the synthesis of vitamins, and promotes the digestion of food debris that does not disintegrate under the influence of gastric and intestinal juices.
- Absorption of water and electrolytes. Numerous studies have proven that the most water and ions are absorbed in the sigmoid colon.
- Removal of feces. Normally, the rectum is empty. Feces accumulate in the sigmoid colon, and when it moves into the ampulla of the rectum, a reflex urge to defecate occurs.
We recommend reading:
Location and functions of the appendix
Disruption of the sigmoid colon leads to diseases. If the absorption function is impaired, a violation of hemostasis and vitamin deficiency occurs. And if the sigmoid colon inhibits the movement of feces, constipation occurs. The cessation of the inhibitory influence leads to diarrhea.
Symptoms of rectosigmoiditis
The acute form of the disease is characterized by a sudden onset with the onset of weakness; in addition, the patient may feel weak, a marked deterioration in health, hyperthermia, chills, nausea and vomiting. Patients suffering from rectosigmoiditis usually complain of intense cutting, cramping pain in the left side of the abdomen. In addition, diarrhea may be observed along with frequent tenesmus, accompanied by the release of a certain amount of feces, mucus and blood, among other things. Flatulence with a feeling of incomplete bowel movement may occur. During the initial stages of a rectal examination, a spasm may be detected, and subsequently a complete relaxation of the sphincter.
In the presence of chronic rectosigmoiditis, the clinical picture is usually less bright; exacerbation, in turn, can alternate with remissions of varying durations. Symptoms are usually caused by eating disorders along with alcohol abuse. During an exacerbation, patients suffering from rectosigmoiditis may complain of aching or nagging pain in the left half of the abdomen. Pain often radiates to the lower back and perineum. Against the background of bowel movements, the pain syndrome may intensify. Very often there is itching in the anus along with increased bowel movements, tenesmus and bloating. Spasms and relaxation of the sphincter are less pronounced than during acute rectosigmoiditis.
Diverticulosis of the sigmoid colon
Another fairly common disease of the sigmoid colon is diverticulosis. The main symptoms of a clinically pronounced uncomplicated disease are abdominal pain (from mild tingling to severe colic) and impaired intestinal function. Localization of pain, as a rule, occurs in the area of the sigmoid colon - in the left iliac region of the lower abdomen or above the pubis. Pain can also be triggered by eating.
A characteristic symptom is unstable stool. Diarrhea may alternate with constipation. In this case, the pain syndrome intensifies due to the prolonged absence of stool. Diverticulosis can occur in combination with irritable bowel syndrome. Possible nausea and vomiting. Sometimes accompanied by leukocytosis and fever.
Divertricular disease is the formation of sac-like hernia-like protrusions of the intestinal wall. In general, the disease is explained by the effect of periodically significantly increased intracavitary pressure on the weakened intestinal wall. These changes are usually age-related. Although there is an assumption based on genetic predisposition to the occurrence of the disease.
The disease, which occurs against the background of an abscess, threatens rapidly developing peritonitis, intestinal bleeding, anemia and other dangerous complications. Therefore, at the first signs, an urgent consultation with a gastroenterologist is necessary. During the diagnosis, the patient undergoes X-ray and endoscopic diagnostics.
The doctor prescribes conservative treatment with antispasmodics, anti-inflammatory drugs, antibacterial drugs and intestinal antiseptics. Complications require hospitalization and possibly surgery. In addition, the patient needs a mandatory diet. To prevent the disease, it is recommended to eat foods rich in plant fiber. They are also advised to exclude too spicy foods from the diet and not to abuse alcoholic beverages.
Diagnosis of pathology
The diagnosis of this disease is made by a proctologist taking into account complaints, pathological history and examination data of the anal area. In addition, the abdomen is palpated, a digital rectal examination is performed, sigmoidoscopy and a number of laboratory tests are performed.
Palpation of the abdomen of a patient suffering from rectosigmoiditis usually reveals pain that the patient feels in the left iliac region. During examination of the perianal zone, areas of maceration and irritation are often identified. A rectal examination may reveal spasms or relaxation of the sphincter along with swelling of the intestinal mucosa. There may be traces of mucus and blood on the glove. Sigmoidoscopy, as a rule, confirms the presence of inflammation in the patient, making it possible to determine the type and severity of inflammatory processes.
Based on blood tests, leukocytosis is detected along with an increase in ESR. A coprogram usually indicates the presence of blood and elements of the intestinal mucosa in the stool. Against the background of rectosigmoiditis caused by helminthiasis, pinworms with roundworms and other parasites can be found in the feces. With rectosigmoiditis, which develops as a result of infection, pathogenic organisms may be present in the fecal matter. In doubtful situations, a biopsy is performed during sigmoidoscopy. As for the final diagnosis, it is made taking into account the results of the histological examination. Now let's look at how a disease such as rectosigmoiditis is treated.
Diagnosis of the disease
Before starting treatment of the patient, it is necessary to clearly formulate the diagnosis. This is done by doctors of such specializations as therapy, gastroenterology, surgery, as well as specialists in infectious diseases. Which doctor will prescribe therapy depends on the causes and manifestations of the disease.
To begin with, it is important to carry out a differential diagnosis to distinguish inflammation of the sigmoid colon from pathologies of the digestive tract and other systems. Diseases similar in symptoms to sigmoiditis include dysentery, ulcerative colitis, cholera, dysbiosis and paraproctitis. In women, it can also be adnexitis, endometriosis, ectopic pregnancy and other pathologies. The following methods are used for diagnosis:
- examination and medical history collection by a qualified physician;
- palpation of the abdomen by the same specialist - to accurately determine the location of pain, which often makes it possible to immediately distinguish sigmoiditis from many other pathologies;
- general laboratory tests of stool and blood to determine the severity of the inflammatory process;
- sigmoidoscopy, which allows you to assess the condition of the intestinal mucosa, the area and shape of organ damage, and also exclude oncology;
- X-ray examination to diagnose intestinal obstruction;
- Ultrasound - helps to assess the condition of the intestines in general;
- endoscopic examination - examination of internal organs using an endoscope, etc.
Treatment methods for rectosigmoiditis: main directions
Treatment of this disease is often conservative. As a rule, it includes the implementation of etiopathogenetic and symptomatic therapy.
Patients are prescribed a gentle diet to reduce irritation of the intestinal walls. Coarse fiber, too cold and too hot, spicy, smoked, fried and fatty foods are excluded from the diet. It is recommended to consume warm soups, and, in addition, dietary main courses that are steamed.
Against the background of the parasitic form of rectosigmoiditis, antiparasitic drugs are prescribed. If there is a radiation form of the disease, appropriate therapy is stopped, and if pathogenic bacteria are detected, antibacterial treatment is carried out.
For any type of rectosigmoiditis, cleansing enemas are used. Usually enemas are performed with a decoction based on chamomile, with the addition of fish oil, collargol solution or sea buckthorn oil. Sitz baths are also used along with suppositories with anti-inflammatory and regenerating effects.
Enveloping and astringent drugs may be prescribed. In the presence of severe pain, patients are prescribed antispasmodics, and against the background of flatulence, medications are required to reduce gas formation. In the presence of ulcerative rectosigmoiditis, hormonal therapy may be needed, which is usually carried out in the form of local remedies - suppositories or microenemas.
After eliminating the inflammatory process in the rectosigmoid colon, it is recommended to take medications that help restore the intestinal microflora. Provided timely and adequate treatment of rectosigmoiditis is carried out, the prognosis is usually favorable.
Treatment
Surgical intervention - this type of treatment is rarely used when tumors are detected in the sigmoid region or a strong bend.
Treatment with drugs is carried out under the supervision of a doctor. If the patient’s well-being worsens, hospitalization is carried out followed by surgical intervention. Depending on the nature of the inflammation, various medications are prescribed:
- Antibiotics – to eliminate inflammation caused by bacteria;
- Adsorbents – to remove toxins;
- Antispasmodics will eliminate intestinal muscle spasms;
- Means to reduce swelling;
- Enzymes for digesting food;
- Probiotics – to normalize microflora;
- Anti-inflammatory drugs.
The drugs are prescribed in the form of tablets or rectal suppositories and microenemas. In advanced cases, the patient is prescribed glucose drips.
Treatment of diseases lasts more than one month, and often requires a repeat course. During drug therapy, a mandatory condition is adherence to a diet.
Diet
It can prevent and cure intestinal diseases, it is prescribed to restore the body, stop inflammatory processes, and enrich the body with nutrients. For a favorable outcome of treatment, you must follow it. It is forbidden to eat fatty, fried and spicy foods, flour products (they can cause fermentation).
The diet includes: fresh fruits and boiled vegetables, dried fruits and compotes made from them, boiled lean fish, boiled or steamed dietary meat (rabbit, veal, chicken), bread containing coarse fiber (it will improve intestinal motility and speed up release).
All foods that can cause gas are excluded from the diet: cabbage, cucumbers and radishes, fried eggs, fatty broth soups and fresh bread, pasta and carbonated drinks, sausages or sausages, sweets, fresh vegetables, milk. During remission, nutritional requirements can be relaxed.
When you stop following the diet, the disease returns. The patient must watch his food throughout his life.
Unconventional methods of treatment
Along with medication, non-traditional types of treatment are used. If the diagnosis is confirmed, it is proposed to treat the disease with a decoction of chamomile, rose hips and plantain (herbs are sold at the pharmacy). Medicinal herbs are either used separately or a mixture of them is used.
Treatment of rectosigmoiditis
The type of treatment the patient can expect depends on the established cause and the diagnosis. Quite often, doctors prescribe conservative therapy using traditional methods. Based on the information received, treatment is carried out in a hospital so that the doctor can monitor the patient’s condition and respond in time to any changes. The patient is given etiotropic therapy and symptoms are eliminated. As part of this treatment, the following recommendations must be followed:
- If radiation damage to the intestine develops, it is necessary to stop the appropriate therapy or adjust the radiation dosage.
- Prescribing an antibacterial drug to reduce the influence of negative organisms.
- Prescription of probiotics used to normalize intestinal microflora.
- To combat spasms, the patient is prescribed antispasmodics.
- The use of infusion therapy is used to restore water balance in the body. This measure is used to reduce intoxication, and, in addition, helps with diarrhea.
- The use of special drugs to improve intestinal microflora and mucosal structure.
How is the treatment carried out?
Treatment of sigmoid colon takes place in a hospital or on an outpatient basis. Bed rest is advisable. In severe forms of diverticulosis, malignant tumors, and stenosis, the damaged area of the sigmoid colon is removed. In case of bacterial infection, an antibiotic is prescribed; intoxication is treated with infusions. You can supplement therapy with folk remedies, which are often used to treat intestinal diseases in children. The following basic medications are used in conservative therapy:
To treat the organ, you may need a probiotic – Linex.
- antibiotics (“Ampicillin”, “Tetracycline”);
- antispasmodics (“No-shpa”, “Spazmalgon”);
- probiotics (Linex);
- prokinetics (“Domidon”);
- saline solutions (Regidron);
- enzyme preparations (Creon);
The duration of the complex treatment course is about 3 months; repetition may be required to reduce the likelihood of relapse.
Diet features
Drug therapy does not bring results without adjusting the patient’s diet. The diet should not burden the intestines, so split meals 5-6 times a day are recommended. Products containing fiber and bran are shown. It is recommended to consume fresh and boiled vegetables, fruits and juices from them, steamed meat and fish dishes, dietary mucous soups, and low-fat cottage cheese. To avoid discomfort and bloating, limit spices, foods that cause gas (cabbage, legumes, radishes, mushrooms), coffee, carbonated drinks, processed foods, chicken eggs, baked goods and fatty foods. Be sure to have a sufficient amount of fluid, 8-10 glasses of clean water per day.
Adenocarcinoma and rectosigmoiditis
Adenocarcinoma is a malignant tumor that usually forms from glandular cells. This malignant formation can be located in different mucous membranes, internal organs or on the skin. But often the tumor is located in the rectosigmoid part of the intestine, which is its most common location. This is observed in ninety-five percent of cases. The tumor is often a complication of rectosigmoiditis. Next, let's take a closer look at what this adenocarcinoma is.
Classification
The following forms of development of such a pathological process are distinguished:
- hyperplastic polyp - formation no more than 0.5 centimeters, the risk of malignancy is extremely low;
- adenomatous polyp - a high risk of transformation into a malignant tumor, sizes vary from 1 to 3 centimeters;
- diffuse form - characterized by a multiplicity of polypous formations, the risk of degeneration into cancerous tumors is low.
In most cases, regardless of the form of the pathological process, polyps in the sigmoid colon are removed.
Description of the pathology
So, as we already know, the rectosigmoid junction is a section of the rectum that is located fifteen centimeters above the anus. Adenocarcinoma located in this area is also called a sigmoid colon tumor. During diagnosis using magnetic resonance imaging, the anus, as a rule, is not displayed; therefore, the area of tumor localization is determined by measuring the distance from the anorectal junction to the tumor itself.
Adenocarcinoma of the rectosigmoid colon tends to develop very quickly, and, in addition, is one of the most progressive types of cancer. Adenocarcinoma quickly forms metastases, accompanied by the most painful symptoms for the patient.
Diagnostics
The beginning of the diagnosis begins with an x-ray of the colon. First of all, polyps are detected. To conduct this examination, the patient takes barium orally, which will help the doctor see the edges of the tumor, shape and size.
A sigmoid colon polyp is a benign formation that consists of glandular epithelial tissue, very rarely transforms into a malignant tumor. Treatment, as a rule, is surgical, since recurrence of the disease is possible, and it is impossible to completely exclude malignancy of the tumor. Provided that therapeutic measures are started in a timely manner, the prognosis is favorable. There are no clear restrictions regarding gender and age, however, according to statistics, this disease is diagnosed three times more often in men.
According to the International Classification of Diseases, Tenth Revision, polyps of the sigmoid colon belong to the section “Other intestinal diseases” and have a separate code designation. The ICD-10 code is K55–63.
Symptoms
The main symptoms of a tumor of the rectosigmoid colon include the following:
- The occurrence of pain in the intestines.
- The appearance of blood in the stool.
- The occurrence of bloating with strong release of gases that have a pungent putrid odor.
- The patient’s complete refusal to eat along with loss of appetite.
- The appearance of lethargy, apathy, depression and unwillingness to live in a person. It must be said that such symptoms can be observed in the patient even before he knows his immediate diagnosis.
- Deterioration of complexion, and, in addition, of the skin throughout the body.
- The occurrence of vomiting, nausea, along with the stomach’s rejection of any food immediately after eating.
- Complete lack of interest in food along with aversion to various, previously very favorite smells.
- Lightning-fast weight loss, and at the same time loss of more than ten kilograms of weight in less than three months.
- The occurrence of bad breath along with belching of air before and after meals.
- The appearance of sticky skin and cold sweat.
- Clouded pupils and yellowness of the face.
Unfortunately, at the initial stage of development of a tumor of the rectosigmoid colon, symptoms are invisible or completely absent. In this regard, without an accurate preliminary diagnosis and without screening, it is difficult for the patient to suspect them on their own. The earlier adenocarcinoma is detected, the greater the patient’s chances of survival and the more comforting the prognosis will be. It is also worth noting that depending on the patient's health, age, race and gender, the propensity for rectosigmoid rectal cancer may be greater or lesser.
Buy online
Introduction
Sigmoid colon cancer occurs in 25-40% of the total number of patients operated on for a malignant tumor of the colon [1, 2, 13]. Despite the fact that radical surgery is performed in 50-70% of cases of colorectal cancer, locoregional recurrence develops in 10-25% of them [5]. Among the reasons for local recurrence of the disease, it is customary to single out incomplete resection, migration of tumor cells in the intestinal lumen and along the parietal peritoneum [9]. No less important and more justified from an etiopathogenetic point of view is the theory of tumor spread through the lymphatic system. Back in 1986, P. Quirke, based on a series of pathomorphological studies, published a work in which he described the possibility of colon tumors spreading through the lymphatic capillaries [15]. The significance of this pathway of disease progression and its impact on patient survival have been proven in a series of major studies [7, 8].
The main route of lymphatic drainage from the sigmoid colon is ascending - located along the branches and main trunk of the inferior mesenteric artery (IMA). The question of the extent of lymphadenectomy when the tumor is localized in the sigmoid colon remains controversial to this day. Despite the fact that a number of authors demonstrate a fairly high probability of involvement of the apical lymph nodes - more than 4-12% [7], there are still statements about the inappropriateness of performing such a large lymphadenectomy [17]. At the same time, when apical lymph nodes are affected by tumor metastases, the 5-year survival rate is 25.6% [10].
Today it is not disputed that the qualifications of the surgeon and the number of operations he performs for colon cancer are an independent prognostic factor. However, to date, sufficient data have not been accumulated to, like rectal cancer surgery, establish certain standards of surgical technologies in the treatment of colon cancer, in particular the sigmoid colon [16].
The purpose of the work is to develop and evaluate the oncological effectiveness of surgical interventions for sigmoid colon cancer that are justified from an anatomical and embryonic point of view.
Features of the structure of the mesentery of the sigmoid colon
To achieve successful surgical treatment of malignant tumors of this localization, it is important to know the anatomy of the sigmoid colon, the structural features of the mesentery and angioarchitectonics. The mesentery (mesocolon) of the sigmoid colon is usually understood as a package of integrative tissue with lymph nodes and vessels, limited by two layers of the parietal peritoneum. The mesentery is clearly visualized by upward traction of the middle third of the sigmoid colon. However, it must be remembered that the base of the mesentery is located in the projection of the aorta - at the origin of the NBA. This is clearly demonstrated by mobilizing the lateral surface of the mesocolon in the sigmoid colon (Fig. 1).
Figure 1. Mobilization of the lateral surface of the sigmoid mesentery. The line marks the transition of the peritoneum from the mesentery to the lateral wall of the pelvis. The problem is that the lateral layer of peritoneum, covering the mesentery of the sigmoid colon, passes to the lateral abdominal wall, where it is called the parietal peritoneum, while the mesocolon remains covered with its own fascia of the colon. With its dorsal surface, this fascial layer is adjacent to the renal fascia, due to which fixation of the mesentery is ensured, which is sometimes falsely perceived as its base and, accordingly, leads to a significant reduction in the volume of surgical intervention.
Despite the fact that the angioarchitecture of the sigmoid colon is quite diverse, there are more or less constant variations in the structure of the vessels. The main source of arterial blood supply is the NBA. Its mouth is located on the anterior surface of the infrarenal aorta and is located between the two lumbar splanchnic nerves, above the superior hypogastric plexus and below the lower horizontal part of the duodenum (Fig. 2).
Figure 2. Orifice of the inferior mesenteric artery. 1 - duodenum; 2 - superior hypogastric plexus; 3 - inferior mesenteric artery. The length of the NBA trunk varies from 4 to 7 cm [6].
N. Michels et al. [13] based on the results of a study of 500 cadavers, it was found that in most cases the NBA is divided into two branches: ascending and descending. In Russian literature, the ascending branch of the NBA is often called the left colic artery. This is not entirely true, since the ascending branch does not go horizontally to the left half of the colon, but follows upward, where it connects with the left branch of the middle colic artery, providing the so-called intermesenteric circulation (between the superior and inferior mesenteric arteries) [18]. It should be noted that a variant of the structure periodically occurs in which there is another additional short vessel connecting the ascending branch of the NBA and the middle colic artery [11]. The arteries that provide direct blood supply to the descending colon are branches of the ascending trunk of the NBA. A less common variant of the structure is in which there is a trifurcation of the NBA and the middle branch is the sigmoid artery. The arterial blood supply to the sigmoid colon is carried out by 2-4 sigmoid arteries, which in most cases are branches of the superior rectal artery; less often, the first sigmoid artery is a derivative of the ascending branch of the NBA [11]. Not reaching 2-3 cm from the intestinal wall, the sigmoid arteries form arcade vessels, the branches of which directly provide blood supply to the intestinal wall. Venous drainage from the sigmoid colon occurs through the inferior mesenteric vein into the splenic vein basin. The inferior mesenteric vein, in turn, is formed by the union of the superior rectal, sigmoid and left colic veins.
Surgery technique for sigmoid colon cancer
Surgical treatment of tumors of the sigmoid colon is based on compliance with modern principles of oncosurgery, among which the main ones are removal of the tumor within the intestinal fascia and treatment of the lymphatic collector, which is potentially dangerous for metastasis. The order of the stages of the operation is of great importance in ensuring oncological effectiveness: first, the feeding vessels are isolated and ligated, then the intestine is crossed, and only after that the tumor is isolated. This principle is called no-touch (translated from English as “not touching”), and its oncological effectiveness has been shown in a number of studies [20].
In accordance with the principles listed above, we have proposed a modified technique for the surgical treatment of sigmoid colon cancer, including para-aortic lymphadenectomy with skeletonization of the feeding vessels and complete mesosigmoidectomy.
The boundaries of lymph node dissection are the lumbar splanchnic nerves on the medial and lateral sides, the lower horizontal part of the duodenum and the superior hypogastric plexus above and below, respectively. The scope of lymphadenectomy may be increased if lymph nodes above the aorta that are suspicious for metastases are detected.
The fundamental point is to accurately identify the layer between the fascia covering the aorta and the fascia proper of the sigmoid colon. After this, a vascular bundle remains on the index finger of the operating surgeon’s left hand, consisting of branches of the NBA and a package of lymph nodes. Another equally important advantage of this technique is to prevent accidental damage to the left ureter, which remains inferior.
A dissection of the peritoneum medial to the sigmoid colon in the cranial direction is carried out to the lower horizontal part of the duodenum, continuing the incision along it in the lateral direction. Next, the actual removal of the lymph nodes located in the area of the mouth of the NBA is performed. The para-aortic tissue is removed so that both lumbar splanchnic nerves remain on the aorta. The visceral branches of the left lumbar splanchnic nerve, running in the direction of the trunk of the NBA, are cut off sharply. The next technique is the actual skeletonization of the NBA barrel. To do this, it is necessary to enter the space above the adventitia of the vessel. As a rule, we use a harmonic scalpel or scissors for this purpose. Further dissection is carried out in the resulting layer in the caudal direction until all the main branches of the NBA are visualized. The technique of skeletonization is not technically difficult and is not accompanied by bleeding.
After identifying the main branches of the NBA, they begin to identify the vein of the same name. When the trunk of the vein is detected, the incision is continued above it in the caudal direction to the level of the intersection of the latter with the ascending branch of the NBA. In this way, a packet of fiber located between the initial part of the NBA and the inferior mesenteric vein is isolated.
Having completed the above stages of the operation, the surgeon must decide on the expected volume of intestinal resection and the level of vessel intersection.
The further course of the surgical intervention is determined by the location of the tumor and the anatomy of the vessels. If the tumor is located in the proximal third of the sigmoid colon, resection of the left parts of the colon is performed. The resection boundaries are marked 10 cm distal and proximal to the tumor. The ascending branch of the NBA and the first sigmoid artery are selectively crossed. This volume of resection and treatment of the feeding vessels makes it possible to ensure adequate blood supply to the middle and distal third of the sigmoid colon and to form a descendosigmoid anastomosis, ensuring the oncological effectiveness of the operation (Fig. 3).
Figure 3. Resection of the left colon. Here and in Fig. 4 and 5: a - operation diagram, b - intraoperative photograph.
If the tumor is located in the middle third of the sigmoid colon, segmental resection of the sigmoid colon is performed with the intersection of all sigmoid arteries and preservation of the upper rectal and ascending branches of the NBA (Fig. 4).
Figure 4. Segmental resection of the sigmoid colon.
If the tumor is located in the distal third, distal resection of the sigmoid colon is performed with the intersection of the IMA immediately after the ascending branch departs from it (Fig. 5).
Figure 5. Distal resection of the sigmoid colon.
The inferior mesenteric vein is always crossed in one place - immediately below the lower horizontal part of the duodenum. Tactics regarding the type of vessel intersection can be presented as follows: vascular trunks located in close proximity on both sides of the tumor are subject to intersection, with obligatory skeletonization of large branches of the vasculature.
To restore the natural course of the intestine, a double-row end-to-end anastomosis is usually formed using a hand suture or a circular stapler.
Material and methods
In the department of coloproctology with pelvic floor surgery of the Russian Scientific Center for Surgery named after. acad. B.V. Petrovsky, from February 2006 to September 2011, gained experience in treating 43 patients with stage I-III sigmoid colon cancer. The study did not include patients in whom distant tumor metastases were detected before surgery or intraoperatively. The average age of patients was 64.9±9.7 years (age range 31-83 years). The ratio between men and women was 30:13. In 10 cases, due to the prevalence of the tumor process, combined surgical interventions were performed: resection of the bladder (n=4), ureter (n=2) and small intestine (n=4). Depending on the location of the tumor, the following surgical interventions were performed: 9 patients with cancer of the proximal third of the sigmoid colon underwent resection of the left parts of the colon, 13 patients with the tumor located in the distal sigmoid colon underwent distal resection of the sigmoid colon. When the middle third of the sigmoid colon was affected, 21 patients underwent segmental resection of the sigmoid colon with the intersection of all sigmoid arteries and preservation of the ascending branch of the NBA and the superior rectal artery.
In order to assess the safety of the proposed surgical interventions, indicators of the intraoperative period (duration of surgery, volume of blood loss, frequency and nature of intraoperative complications) were analyzed. In addition, each removed specimen was subjected to pathomorphological examination with morphometry, in which the length of the removed specimen, the distance from the proximal and distal boundaries of the tumor to the corresponding resection lines, and the length of the vascular pedicle were measured. All lymph nodes were mapped in relation to arterial vessels, i.e. lymph nodes located along the marginal vessel (first order), along the main vascular trunks (second order) and apical (third order) were examined separately.
In the postoperative period, all patients underwent regular examination according to the monitoring program for patients with colorectal cancer, which included ultrasound of the abdominal organs, CT scan of the chest and abdomen, colonoscopy at 3, 6, 9, 12 months and then every 6 months.
Oncological outcomes were assessed by the incidence of disease recurrence and cumulative overall survival, as well as disease-free survival (local and distant) using the Kaplan-Meier method. We conducted a univariate analysis of factors influencing survival. The following parameters were set as factors: lymph node involvement in order, stage pT4, degree of tumor differentiation.
Results and discussion
Immediate results
To perform interventions with skeletonization of feeding vessels, an average of 206.2±73.0 minutes is required, although the stage of skeletonization and para-aortic lymphadenectomy itself took an average of 28±9 minutes (16-38 minutes). The average blood loss was 271.1±93.1 ml.
Complications of the early postoperative period occurred in 2 (4.5%) patients, both required re-intervention: bleeding from the marginal vessel of the reduced colon after distal resection of the sigmoid colon in one and bleeding in another patient, who had previously undergone a combined distal resection of the sigmoid colon. for locally advanced cancer with invasion into the bladder (the source of bleeding was not found, sanitary relaparotomy was performed). The length of hospital stay after surgery was 11.8±6.1 days. There were no deaths.
Results of pathological examination
When analyzing morphometric parameters, the following data were obtained: the length of the specimen was 24.7±11.4 cm, the length of the vascular pedicle was 12.1±3.4 cm.
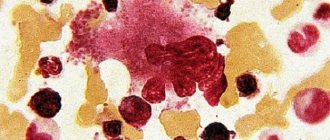
The histological structure of the tumor was designated as poorly differentiated adenocarcinoma in 5 (12%) cases, well differentiated in 4 (9%) and moderately differentiated adenocarcinoma in 34 (79%) cases. Tumor growth within the muscular layer of the intestinal wall was determined in 7 (16%) patients, growth beyond its limits in 26 (60%), tumor invasion of the serous membrane or presenting organs in 10 (24%) patients.
The average number of examined lymph nodes in the specimen was 26.4±18.2. The average number of examined first-order lymph nodes was 10.9±1.4, second-order - 7.7±3.1, third-order - 5.9±0.8. First-order metastatic disease of the lymph nodes occurred in 20.5% of patients. Damage to intermediate lymph nodes (second order) was diagnosed in only 1 (2.3%) case. Two patients had apical lymph node involvement (4.6%). Both of these patients were operated on for a locally advanced tumor of the sigmoid colon.
Long-term results
All patients included in the study were followed up. The median follow-up was 39.35±13.1 months.
During the study period, 4 (9.1%) patients died. In 3 (6.8%) cases, death was due to progression of the underlying disease, in 1 - acute violation of coronary circulation. Based on pathomorphological examination data, all patients who died from tumor progression were diagnosed with stage pT3. In one of three observations, there was damage to the pericolic lymph nodes (second order). The average time to death associated with tumor progression was 18.1 months. The overall cumulative 3-year survival rate in the selected group of patients was 90.1%.
During monitoring, 2 patients were diagnosed with metastatic lesions of the lungs and liver; they are currently receiving chemotherapy at their place of residence. None of the observations to date have revealed signs of local relapse of the disease. The disease-free cumulative 3-year survival rate was 81.4%. Univariate analysis did not reveal factors significantly influencing survival (see table).
It is traditionally believed that resection interventions for sigmoid colon cancer are well developed technically and are simple to perform. Factors that contribute to support this opinion include relatively high cancer-specific survival rates, the short period of time required to master the standard procedure, and the widespread belief that the technique is well known and does not need further improvement. However, even after surgical interventions performed radically from the surgeon’s point of view, the rate of locoregional relapses reaches 10-25% [5].
There is no description in the literature of a standardized operation for sigmoid colon cancer based on clearly defined anatomical-embryological relationships. The scope of lymphadenectomy is usually designated as para-aortic with high ligation. However, there is no description of clear anatomical boundaries of dissection. High ligation of the NBA may involve crossing the vessel both in the immediate vicinity of the aorta and 1-2 cm from it or before the origin of the left colic artery. The problem is that the length of the NBA can reach 7 cm [6]. Thus, there are no clear anatomical landmarks for the intersection of the vessel and the volume of lymph node removal.
It should be noted that the intersection of the NBA immediately after its departure from the aorta and para-aortic lymphadenectomy are not identical concepts, since the actual intersection of the NBA does not require removal of lymph nodes in the para-aortic region. Defining clear boundaries for para-aortic lymph node dissection, based on an understanding of the structure of this area, is extremely important.
The main argument for refusing to perform para-aortic lymphadenectomy is the risk of developing genitourinary disorders in the postoperative period associated with damage to the autonomic nerves located in this area. Meanwhile, in colon cancer surgery, techniques for performing nerve-sparing operations are well known. By analogy with total mesorectumectomy, the dissection layer in nerve-sparing para-aortic lymphadenectomy lies along the elements of the autonomic nervous system, and the boundaries of the removed lymph node package are determined by the lumbar splanchnic nerves and the hypogastric plexus. Thus, the statement that para-aortic lymphadenectomy cannot be performed without removing the autonomic nerves, in our opinion, is misleading.
Analysis of our own material showed that the frequency of damage to apical nodes does not exceed 4%, while C. Maurer demonstrates damage to apical lymph nodes in 10-12% of cases [12]. This is a strong argument in favor of performing para-aortic lymphadenectomy, since the main reason for the development of local relapse is incomplete removal of tumor disseminates of the mesentery of the sigmoid colon, which can be represented by affected lymph nodes [3, 14, 15]. Removal of lymph nodes of this location is often accompanied by the intersection of the IBA at the point of its origin from the aorta, which in turn leads to a significant expansion of the scope of the operation due to impaired blood supply to the left half of the colon. The technique we propose for skeletonization of the feeding vessel allows us to remove the necessary package of lymph nodes while maintaining the blood supply to the intestine and perform segmental resections. Expanding the scope of the operation to left-sided hemicolectomy for a tumor of the sigmoid colon is not justified oncologically, since the risk of damage to the pericolic lymph nodes at a distance of 10 cm from the edge of the tumor is present in no more than 2% of cases [19].
Consequently, segmental resection of the mesentery of the sigmoid colon is not an oncologically justified operation, and the approach to the treatment of sigmoid colon cancer requires revision. In our practice, the most obvious clinical model demonstrating the need for sanitation of the para-aortic region are patients who underwent obstructive resection for sigmoid colon cancer in other medical institutions and came to us with the goal of restoring the natural course of the intestine. During reoperation in most of these patients, a package of apical lymph nodes is identified in the para-aortic region, located in the part of the mesentery of the sigmoid colon, covered with peritoneum on both sides. In such a situation, there are often affected lymph nodes in the area of the base of the mesentery of the sigmoid colon, diagnosed during reconstructive interventions (Fig. 6, 7).
Figure 6. Package of para-aortic lymph nodes (history of segmental resection of the sigmoid colon). 1 - proximal stump; 2 - distal stump; 3 - tumor metastasis in the area of the apical lymph nodes.
Figure 7. Removal of tumor recurrence in the area of the apical lymph nodes. a - relapse in the area of the sigmoid artery.
Figure 7. Removal of tumor recurrence in the area of the apical lymph nodes. b — view after removal of the relapse: 1 — inferior mesenteric artery; 2 - inferior mesenteric vein; 3 - superior rectal artery; 4 - the ascending branch of the NBA.
To prevent local relapse of the disease, it is equally important to observe the correct isolation of the affected organ within the fascia of the colon - mesocolonectomy [4, 8]. The effectiveness of combining para-aortic lymph node dissection and the principle of complete mesocolonectomy is demonstrated by the absence of local recurrence of the disease in our study.
In 2010, the results of a multicenter study were published, the purpose of which was to evaluate the effectiveness of high ligation of the feeding vessel together with mesocolonectomy for colon cancer. The high 5-year cumulative survival rate (89%) [21] underscores the oncologic efficacy of this approach in the treatment of colon malignancies. This is confirmed by the results of our study, in which the overall 3-year cumulative survival rate was 90.1% and the 3-year cumulative disease-free survival rate was 81.4%.
Thus, resection of the sigmoid colon with para-aortic lymphadenectomy and skeletonization of the feeding vessels is the operation of choice for patients with cancer of this location. The proposed operations are absolutely justified from the point of view of oncological radicalism, since they involve removal of the tumor en bloc with the mesenteric fat-fascial package and apical lymph nodes. Analysis of our own results indicates the safety of this type of surgery from the standpoint of intra- and postoperative complications. However, to scientifically substantiate the proposed surgical interventions, it is necessary to continue studying long-term results and conduct a prospective study with randomization according to the type of intervention performed.
Main causes of adenocarcinoma
The causes of adenocarcinoma of the rectosigmoid region may be the following:
- Two or more close relatives have had this type of cancer.
- Lack of fiber in food, and, in addition, consumption of raw plant foods.
- The presence of weak peristalsis.
- A person's strong addiction to meat foods, especially pork.
- A person's complete lack of physical activity.
- Having obesity and overweight along with diabetes.
- Passion for smoking and alcohol in large quantities. It is worth noting that alcoholics have several times higher chances of developing this type of cancer than people who drink alcohol in moderation.
- The presence of inflammatory diseases of the stomach or intestines.
- Presence of chronic dysbacteriosis.
- Passion for promiscuous sexual intercourse.
How is rectosigmoid colon cancer treated?
Diet for sigmoiditis
It is necessary to treat intestinal diseases while following a therapeutic diet. Its goal is to reduce the load on the intestines during an inflammatory disease, while maintaining normal motility.
Avoid foods that are difficult for the digestive system: fatty foods, fried and smoked foods, salty and sour foods, spicy foods, caffeine-containing drinks, alcohol. It is necessary to exclude baked goods and sweets, as they increase fermentation. Recommended:
- low-fat fermented milk products;
- rice;
- boiled or steamed vegetables;
- boiled potatoes;
- lean meat and fish, steamed;
- liquid soups with low-fat broth.
In case of acute illness, it is enough to adhere to the diet until complete recovery. Chronic inflammatory process requires constant adjustment of diet.
Treatment of this pathology
The main treatment for this cancer is surgical resection. It can be complete or partial. In addition to the area affected by cancer, regional lymph nodes are also removed. Tissue samples from nearby lymph nodes must undergo histological examination for the presence of cancer cells.
But the situation becomes more complicated if the tumor of the rectosigmoid junction is inoperable. When surgery is not possible, a small section of intestine is completely removed to form a colostomy (this is a special tube for removing digestive waste).
Another method of treating cancer of the rectosigmoid colon is radiation therapy, which can be postoperative or preoperative. The first may be needed if the cancer has spread to the walls of the abdomen and the area behind the peritoneum. The time for postoperative radiation treatment is two weeks after surgery.
Chemotherapy is used for rectosigmoid adenocarcinoma in combination with other treatment options. Chemotherapy drugs include Fluorouracil, along with Capecitabine, Oxaliplatin, Tegafur and others. The course of treatment is usually about three months.
How long do people live with stage 4 sigmoid colon cancer?
Oncology develops over several years. Due to the absence of symptoms, cancer is detected in an advanced form. What adversely affects the patient’s life expectancy. Doctors recommend doing a full examination of the entire body every year. If you have discomfort in the large intestine or gastrointestinal disorders, you should consult a doctor.
In the presence of a stage 3 tumor, cancer cells affect a large area of the organ, which is an obstruction of the large intestine. The following symptoms appear in the patient, namely:
- severe pain;
- vomit;
- nausea;
- body temperature is kept within 37 – 38 degrees;
- prostration.
These factors develop into diarrhea and constipation. If such symptoms are detected, it is urgent to contact a specialist for further examination.
Nowadays, it has become very fashionable to use traditional methods of treatment. Before using self-medication, you must obtain consent from your doctor. Correctly calculate the dosage and course of therapy. If there are side effects, you should refuse this type of treatment. Herbal medicine has a number of contraindications. When used correctly, traditional methods will significantly improve the general condition of the patient.
During oncology therapeutic procedures, it is imperative to adhere to a balanced diet. Bad habits, if any, should be eradicated. Don't give up during the healing process. After all, a positive-minded person always believes in the chance of recovery. A pessimistic mood has a detrimental effect on health. A weak body also requires regular walks in the fresh air. For sigmoid colon cancer with liver metastases, the prognosis is made individually. It all depends on the condition of the body and the overall volume of the tumor.
Sigmoid colon cancer, even after the appearance of a polyp, the disease may not manifest itself, this is due to the subtleties of the structure of the sigmoid colon
Oncological disease in any form poses a danger to human health and life. If we talk about the intestines, among malignant neoplasms the most common tumor is the sigmoid colon. At the end of the article, we will offer you a statistical prognosis for stages 2, 3 and 4 of sigmoid colon cancer, but first we suggest you familiarize yourself with what its symptoms are, how to diagnose cancer and what treatment methods exist.
Sigmoid colon cancer is not called the silent killer for nothing. Even after the polyp appears, the disease may not manifest itself. This is due to the subtleties of the structure of the sigmoid colon.