The membrane of the fertilized egg provides nutrition and protection to the baby while in the womb. There is a flow of nutrients, vitamins, and oxygen through the vascular bed of the placenta. The membrane is a hemoplacental barrier.
According to statistics, four out of a thousand pregnant women have an abnormal location of the placenta. What does such a diagnosis mean and why is it bad? What factors influence the pathological attachment of a child's seat? How to diagnose marginal displacement of the placenta? Can pathology be prevented or not? What are the consequences of placenta presentation for delivery?
Normal location of the placenta
The chorion transforms into the placenta only at the 12th week, but its final maturation occurs only at the sixteenth. Afterwards, the development of the placenta continues until the 36th week. This organ is designed to provide the baby with oxygen, all the necessary substances and microelements. However, ideal conditions for normal development of the placenta are not always created.
Interesting fact: according to statistics, about 15% of women experience pathological placental attachment.
All types of placenta previa are a pathology and require constant monitoring by a doctor.
The physiological norm is considered to be a condition when the placenta is attached to the fundus of the uterus or in areas that are close to its lower part: the front or back wall. If deviations exist, the organ may join the pharynx.
The pharynx is the opening in the uterus that connects it to the vagina. It protects the uterine area from infection.
Based on the location of the placenta, the following types of presentation can be diagnosed:
- complete (the placenta completely covers the uterine os);
- low (the placenta is in close proximity to the pharynx, the approximate distance is 4–5 centimeters);
- lateral (the uterine os is partially covered by the placenta);
- marginal (the placenta touches the pharynx only at the edge).
Interesting fact: there is a theory that gravity plays a significant role in choosing a place for attachment of the fertilized egg. If the expectant mother prefers to sleep on her right side, then it is attached to the right side of the uterus and vice versa.
What is placenta
The placenta appears in a woman only during pregnancy. With childbirth, she comes out with the baby. Popularly, this organ is also called the place of birth and the placenta. Its main task is to provide the baby with all the necessary elements.
In fact, the placenta has many functional responsibilities:
- protective;
- nutritious;
- hormonal;
- trophic.
And yet, the main task of this organ is to protect the fetus from negative environmental conditions. When everything is fine, there are no pathologies, then the baby’s development in the womb occurs as determined by nature.
What is marginal placenta previa and marginal presentation along the posterior wall?
Marginal placenta previa is a pathology that occurs when the upper segment of the uterus turns out to be unsuitable for the implantation of the fertilized egg for a number of reasons, and it attaches lower. However, the embryonic organ can “migrate” during gestation. A change in the location of the placenta occurs due to a change in the structure of the lower segment of the uterus and due to the lengthening of the upper uterine segment. Typically, the “migration” process begins in the 6th week and is completed by the 34th week of pregnancy. In this case, it is not the placenta itself that moves, but the underlying myometrium (the submucosal layer of the middle muscular layer of the uterine wall) shifts. “Migration” of the embryonic organ occurs from bottom to top. If after the 34th week the edge of the placenta still touches the internal os of the uterus, then we can talk about the marginal attachment of the placenta.
Interesting fact: marginal placenta previa after the 32nd week is typical for only 5% of pregnant women. However, they still belong to the risk group, since the percentage of perinatal mortality increases in this case by 25%.
Marginal presentation of the placenta along the posterior wall is an indicator that the organ will not leave the internal os in most cases. This position will contribute to the successful completion of the cesarean section, since the placenta is not injured during the incision. The posterior wall is not elastic and is little subject to change, so the likelihood of “migration” of the embryonic organ is low. Regional presentation along the anterior wall is more dangerous, since the organ in this case is subjected to serious stress, and there is a risk of mechanical disruption of the integrity of the placenta. In this case, there is a high probability that in the later stages of gestation the placenta will take a normal position.
Placenta previa often leads to persistent bleeding. The latter are more expected in later stages of pregnancy. This is due to the active formation of the lower segment of the uterus. The placenta is capable of correctly performing the task assigned to it only when it is located normally.
Important: during pregnancy, it is imperative to monitor the location of the placenta, its thickness and structure using ultrasound. It is advisable to carry out the first no later than the 13th week. The thickness of the organ can only be determined at the twentieth.
Types of choreon presentation
There are several classifications of the described obstetric pathology. The following is generally accepted:
- complete placenta previa -
the case when the internal os is blocked by lobules of the placenta, that is, it “passes” from one uterine wall to another, and the fetal membranes are not detected during vaginal examination (another name is central presentation);
- incomplete placenta previa or partial presentation - in this case, the placenta does not completely cover the internal os and is divided into 2 subtypes:
- lateral presentation - when 1 or 2 lobules of the placenta are presented and the fetal membranes are palpated (roughness is determined);
- marginal presentation - in this case, the extreme portion of the placenta is located in the area of the internal os, but does not extend beyond it;
Separately, it is worth highlighting low placentation or low placenta previa during pregnancy.
Low placentation is the localization of the placenta at a level of 5 or less centimeters from the internal os in the third trimester and at a level of 7 or less centimeters from the internal os in pregnancy up to 26 weeks.
A low location of the placenta is the most favorable option; bleeding during gestation and childbirth rarely occurs, and the placenta itself is prone to so-called migration, that is, an increase in the distance between it and the internal os. This is due to the stretching of the lower segment at the end of the second and third trimesters and the growth of the placenta in the direction that is better supplied with blood, that is, to the uterine fundus.
In addition, the presenting vessels are identified. In this case, the vessel/vessels are located in shells, which are located in the area of the internal pharynx. This complication poses a threat to the fetus if the integrity of the vessel is damaged.
Complications with marginal placenta previa
The placenta may return to its normal position closer to the third trimester. This does not happen in only 5% of women in labor. In this case, the following complications are possible:
- premature labor or the need for emergency termination of pregnancy;
- severe iron deficiency anemia;
- developmental defects and prolonged fetal hypoxia;
- placental abruption (marginal or central);
- rupture of the uterine body due to fusion of its walls with the placenta;
- perinatal fetal death;
- embolism (blocking of lumens) of blood vessels;
- heavy bleeding at the end of labor.
Video: placenta previa
Diagnosis of placenta previa - how is it determined?
- Obstetric external examination (note: height of the uterus, position of the fetus).
- Auscultation (in case of presentation, the noise of the placenta/vessels is usually noted directly in the lower part of the uterus near the placenta).
- Gynecological examination with speculum. Palpation determines complete presentation if there is a soft and large formation that occupies all the vaginal vaults, and incomplete presentation - when it occupies only the lateral or anterior vault.
- Ultrasound. The safest method (compared to the previous one). With its help, not only the fact of placenta previa is determined, but also the size, area and structure, as well as the degree of abruption, hematoma and the threat of miscarriage.
Causes of the pathological location of the placenta
Placenta previa can be caused by a variety of reasons and factors. The fertilized egg may differ in some features. The state of health of the mother and the processes occurring directly in the uterus play a major role. It is not possible to influence the place where the placenta is implanted by medical means; the process is uncontrollable. However, a woman is quite capable of minimizing potential risks.
Abnormalities of the ovum
The trophoblast (the outer cellular mass of the embryo), which is formed during the cell’s journey through the female reproductive organs, is the main assistant at the stage of attachment of the fertilized egg to the wall of the uterus. In the future, it is he who helps the fetus form the placenta. The membrane covering the fertilized egg may be too dense. In this case, successful implantation will not occur, even if the fertilized cell (zygote) is strong.
If you believe the statistics, then only healthy embryos, without genetic abnormalities, are able to properly implant into the uterine cavity. Embryos with congenital pathologies either do not undergo natural selection by the female body (the latter provokes miscarriage) or are implanted incorrectly.
Correct implantation of the fertilized egg can only occur if there is good tubal patency, the absence of abnormalities in the embryo and the fertile uterine mucosa
. In addition, the fertilized egg may not be active enough. If it does not promptly release a sufficient amount of enzymes that destroy the mucous membrane, then abnormal placentation may occur. While the egg is in the upper segments of the uterus, it does not have time to mature for implantation, and when the process is completed, it no longer has a choice and has to be attached lower.
Reasons related to maternal health
Once in the uterus, the fertilized egg begins to actively look for a place for implantation. Normally, it is attached to the upper layers of the uterus (most often the posterior wall or fundus is involved). However, this does not happen if the organ mucosa is damaged. Then the fertilized egg descends and implants into the lower segments of the uterus. There are many provoking reasons for this phenomenon, their list is as follows:
- bad habits;
- inflammatory processes occurring in the uterus;
- frequent births or a significant number of them;
- carrying out a curettage procedure or abortive intervention during pregnancy, as well as infection that may result from them;
- tumor development in the uterus;
- an abundance of scars on the body of the uterus;
- various anomalies of the uterine organ;
- endometriosis (a disease associated with the growth of internal cells of the uterus beyond the organ);
- too late first birth;
- hormonal disruptions and disorders;
- multiple pregnancy;
- concomitant diseases of internal organs. With pathologies of the cardiovascular system or circulatory disorders, congestion can form in the pelvic organs, as a result of which the fertilized egg cannot attach normally.
All the factors described above can negatively affect the course of pregnancy and fetal development.
Is it possible for the placenta to shift as the fetus and uterus grow?
The uterus gradually increases over time, because the child inside the mother’s womb grows and develops. The baby's place moves and may rise a little during pregnancy. Such a process cannot be stimulated from the outside.
To completely change the attachment of the placenta, there are no medications or any physiological methods or exercises. Surgical intervention to correct the placement of a child’s seat is also impossible.
The task of doctors in case of abnormal attachment of the placenta is to prevent ruptures and detachment of the fetal membrane, minimize the amount of blood loss during bleeding, and promote delivery naturally or by cesarean section. Treatment tactics for detected presentation include constant monitoring of the well-being of the woman and child.
Symptoms of marginal placenta previa
Regional placenta previa can be characterized by two types of symptoms: silent and severe. The first does not involve changes, so the woman is unable to respond to the ongoing process in a timely and correct manner. Violations can only be detected by ultrasound diagnostics.
If the location is abnormal, the placenta can tear away from the walls of the uterus and cause bleeding
With severe symptoms, the incorrect location of the embryonic organ is most often manifested by external bleeding. In addition, false contractions may appear at any time. It is the latter that lead to stretching of the uterus, separation of the placenta from its walls and rupture of blood vessels. Bleeding can also occur at a time when the organ opens much later than the uterine segment. The placenta exfoliates, which leads to disastrous consequences.
Important: bleeding tends to occur at the most unexpected moment; the process cannot be predicted. It can form even during a night's rest. Its strength and duration cannot be predicted either.
Regional placenta previa can manifest itself in different ways. It all depends on the individual characteristics of the body. At the first sign of discomfort, consultation with a doctor is required.
Symptoms
The lower area of the uterus and the walls are constantly growing and stretching as pregnancy progresses and at the time of birth. The placenta does not have such elasticity. This causes its detachment, resulting in bleeding from the vessels of the uterus.
Therefore, the main symptom is sudden, painless, recurring light or heavy vaginal bleeding in the second half of pregnancy. Some women also experience contractions.1
Bleeding can be triggered by a variety of factors: physical effort, vaginal examination, sexual intercourse, coughing, hot bath or sauna, increased intra-abdominal pressure due to constipation.
If you experience any of the following symptoms, you should contact your doctor immediately:
- cramps or sharp pains;
- bleeding that recurs after several days or weeks;
- bleeding after sexual intercourse;
- bleeding in the second half of pregnancy.
Diagnosis of pathological locations of the placenta
The anomaly is detected by ultrasound examination. Using ultrasound, you can accurately determine the presence of pathology, the specific position of the placenta body and the location of its edges. Computer diagnostics gives an idea of the thickness of the organ and its size. An ultrasound can also record the distance from the lower edge of the placenta to the internal os of the uterus. This parameter is very important because it can tell you about potential risks and complications.
A bimanual examination of the vagina (assessment of the condition of the uterus, ovaries and pelvic tissues on a gynecological chair) is not advisable in order to prevent bleeding, which may ultimately cause premature birth. In a situation where it is impossible to perform an ultrasound, the doctor must carefully carry out the examination and draw conclusions.
Types of abnormal placentation
According to the location of the child's seat, they distinguish full, low, lateral, incomplete, and central presentation. The greatest danger to full pregnancy is complete occlusion of the pharynx. Central presentation is determined during a gynecological examination or ultrasound. With such a presentation, natural childbirth is impossible; a caesarean section is required.
Low presentation means that the exit from the uterus is not blocked. The baby's place does not reach the pharynx, but is located at a distance of less than 7 centimeters from the cervical canal. Such placentation has the most favorable prognosis. Natural childbirth is possible.
Partial marginal attachment means incomplete overlap of the internal canal of the cervix by the placenta. The clearance is too narrow. The newborn's head will not fit through it, which means the baby will not be able to exit through the genital tract.
Lateral and marginal placenta previa are determined during a vaginal examination and confirmed during an ultrasound examination. With lateral presentation, the placenta partially covers the exit from the uterus. When the edge is located next to it, without blocking the entrance. There is also partial attachment along the posterior and anterior wall with incomplete, low presentation.
Treatment
It is impossible to cure marginal placenta previa in the truest sense of the word. There is only an opportunity to promote the “migration” of the embryonic organ or to prevent the situation from getting worse. In order to reduce pressure on the vaginal vessels and the lower edge of the placenta, a woman is recommended to use a special bandage . A pregnant woman in such a situation is contraindicated in physical activity and stress, which can lead to surges in blood pressure. Sexual contact should also be avoided.
If a pregnant woman is diagnosed with placenta previa, it is recommended to wear a bandage
An exercise will help reduce pressure on the lower edge of the placenta: a woman is recommended to stand on both hands and feet on the floor 3-4 times a day. You need to stay in this position for several minutes. In this way, it will be possible to somewhat stretch the anterior wall of the uterus and achieve some upward movement of the placenta. The exercise may be especially effective in the second trimester.
In order to reduce pressure on the lower edge of the placenta, a woman is recommended to stand on all fours for a few minutes 3-4 times a day.
Drug treatment may include vitamin therapy, taking antiaggregation (suppressing the adhesion of blood cells) and vascular drugs in doses that are safe for the health of the mother and fetus.
Most often, women diagnosed with marginal placenta previa are hospitalized at 24 weeks. The hospital carries out procedures and preventive measures, such as:
- tocolytic therapy. A pregnant woman is prescribed medications to reduce the number of uterine contractions. This effect is possessed by: Ginipral and Partusisten. They are administered to the expectant mother by drip or intramuscular injection;
- prevention of fetoplacental insufficiency. A pregnant woman is prescribed vitamin complexes and medications designed to improve blood circulation: Curantil, Trental or Actovegin;
- prevention of anemia. A woman is prescribed drugs that increase the level of hemoglobin in the blood;
- taking antispasmodics. Women are prescribed suppositories with papaverine, Magne-B6, No-shpa or magnesium sulfate. Therapy is aimed at reducing the tone of the uterine organ;
- prevention of premature birth. If there are risks due to placental abruption, additional treatment is carried out with corticosteroids: Dexamethasone and Hydrocortisone. This is necessary to prevent breathing disorders in the baby.
How does pregnancy proceed with established placenta previa?
- Period 20-28 weeks . If the presentation is confirmed on the 2nd ultrasound, and there are no symptoms, then a regular examination of the expectant mother by her gynecologist-obstetrician is sufficient. Usually, additional drugs are prescribed to reduce the tone of the uterus. If there is even spotting, hospitalization is required.
- Period 28-32 weeks. The most dangerous period for both: with an increase in the tone of the uterus in its lower parts, the risk of detachment and serious bleeding increases with the small size and immaturity of the fetus. In case of marginal or complete presentation, a hospital is indicated.
- Period 34 weeks. Even in the absence of bleeding and severe fetal suffering, the expectant mother is advised to go to hospital until the birth. Only constant supervision by specialists can guarantee a successful outcome of pregnancy and childbirth.
Childbirth with marginal presentation
In a situation where special exercises did not help and the bandage did not give the desired effect, doctors decide on the safest method of delivery. This usually occurs at 36–38 weeks of gestation. If the ultrasound still indicates marginal placenta previa, the obstetrician-gynecologist may recommend early hospitalization.
If bleeding is mild or absent, then natural delivery is possible. In this case, when the cervix is dilated to three fingers, a prophylactic amniotomy is performed (opening the membranes of the fetal bladder).
If the cervix is dilated to 3 fingers and a diagnosis of marginal presentation is made, a woman is recommended to have a prophylactic amniotomy
Some obstetricians and gynecologists allow women to give birth on their own, even if there is bleeding. If the cervix is smooth and soft, then an amniotomy is performed before contractions, as a result of which the baby descends and is closely pressed against the entrance to the pelvic area, thereby retaining the detached lobules of the placenta. This will stop the bleeding. The woman is also prescribed the drug Oxytocin. It reduces the amount of blood loss during childbirth and speeds up the process, causing strong and frequent contractions.
When amniotomy is not effective, a woman with heavy bleeding is prescribed a cesarean section. In some cases, early surgical delivery (when the period is less than 36 weeks) is acceptable. In this case, not only the woman, but also the child is prepared for premature intervention by administering drugs that accelerate the formation of alveoli in the lungs. Ultrasound examination will help assess the maturity of the fetus and its readiness for childbirth.
Important: bleeding limits or completely eliminates the use of antiplatelet agents that help improve blood flow. Anemia can lead to poor maternal health or fetal hypoxia (lack of oxygen).
Photo gallery: childbirth with a diagnosis of placenta previa
If bleeding during placenta previa is mild or absent, then natural delivery is possible
If there is heavy bleeding and a diagnosis of placenta previa, the doctor may decide to perform an early surgical delivery.
When amniotomy is not effective, a woman with heavy bleeding and a diagnosis of marginal presentation is prescribed a cesarean section.
Caesarean section for pathology
C-section
in case of placenta previa it is carried out if there is:
- anamnesis in the form of diseases with a pronounced inflammatory nature;
- detection of polycystic disease or uterine fibroids;
- previous abortive interruption of the gestation period;
- multiple births
; - pregnancy at a late age;
- early surgical intervention with violation of the integrity of the uterus;
- systematic blood loss in a volume exceeding 0.2 l;
- complete low location of the amniotic sac;
- leg or pelvic
position of the fetus.
The above aspects serve as the basis for planned surgical intervention. If there are no indications for a cesarean section with placenta previa, natural delivery occurs. If there is a threat to the life of the expectant mother or child, emergency intervention is carried out.
Note!
It should be remembered that after surgery a woman still has the possibility of subsequent childbearing.
Diagnosis of pathology
Symptomatically, this pathology is often manifested by bloody vaginal discharge. Most often, these signs appear from the 28th week, it is during this period of pregnancy that the activity of the uterus increases. In the third trimester, the appearance of blood can be facilitated by physical activity, sexual intercourse, or after active movements of the fetus if it is in an incorrect position. The type of bleeding that occurs depends only on the degree of damage to the blood vessels. There can be either minor bleeding or heavy bleeding, which carries consequences. Bleeding occurs due to the fact that the uterus is actively growing; the blood vessels in such a placenta previa do not have time to adapt and placental abruption occurs. The pain syndrome may be mild or completely absent.
Diagnosis consists of examination by a gynecologist and ultrasound. During the scan, the doctor determines the location of the placenta and the degree of overlap of the uterine os, and of course the condition of the child, because any spasm of blood vessels in the placenta immediately affects his condition.
Sex with low placentation
As a rule, the doctor categorically excludes sex with a low-lying placenta.
But since there are several types of sex, pregnant women often wonder whether all types of intimate contact should be limited or just vaginal sex.
With low placentation, it is necessary to exclude any type of sex that:
- causes excitement, leading to a rush of blood in the pelvic organs;
- produces a direct physical effect on the vagina or rectum.
Thus, with low placentation, sexual rest is recommended for all types of sex.
Diagnosis of low placentation
An ultrasound will reliably reveal the fact of anomalies in the location of the placenta.
The location of the placenta is determined by ultrasound diagnostics. Also, based on the results of ultrasound and Doppler, the doctor will be able to determine whether there is a lack of nutrients (based on the size of the fetus and their age) and oxygen (based on blood flow assessment during Doppler).
That is why, if low placentation is detected, it is necessary not to neglect the doctor’s recommendations and attend consultations, as well as undergo examinations as often as recommended by the gynecologist leading the pregnancy.
What not to do
Pregnant women with low placentation must be constantly monitored by a doctor. If you follow his recommendations exactly, everything will be fine. What you shouldn't do:
- worry. Modern medicine successfully treats pregnant women with low placental attachment. In 90% of cases, a woman gives birth to a healthy baby. Moreover, 60% of births are carried out naturally, and only 40 - by cesarean section;
- have sexual intercourse. Sex at any stage can damage the organ and lead to detachment. This only applies to women with low placenta previa;
- play sports, do abdominal exercises, lift weights, walk a lot. Decide what is more important, an active lifestyle or the health of the child;
- do douching and any other vaginal manipulations so as not to harm the pregnancy;
- worry, get nervous, get irritated. This will lead to an unhealthy emotional atmosphere and aggravate the condition. Develop stress resistance;
- travel on public transport, visit places with large crowds of people. They can push there, which will cause even greater prolapse of the organ;
- Ignore the doctor's recommendations and do not go on conservation when necessary.
You have to be patient
If the presentation is low, the woman is advised to place a pillow under her legs so that they are higher than the level of the body. This will help the placenta quickly find its place.
Low placentation is not a disease, but a special condition. The situation requires, first of all, not treatment, but correction. Much depends on the mood of the pregnant woman, her actions, and how accurately they correspond to the advice of doctors.
Preventive measures will help to avoid anomalies. These include:
- prevention of infectious and inflammatory diseases, their timely treatment;
- maintaining a healthy lifestyle: proper nutrition, adherence to work and rest schedules, avoiding alcohol and tobacco abuse;
- protection against unwanted pregnancy, so that there is no history of abortion;
- performing a caesarean section only in cases where there are vital indications;
- performance of gynecological manipulations and operations in trusted clinics by experienced doctors.
How dangerous is the pathology?
The danger of the pathology is the possible termination of pregnancy. With complete placenta previa, the risk of premature birth increases.
Many women develop hypotension due to blood loss and changes in vascular tone. Such patients are indicated for hospitalization to maintain pregnancy and prevent blood loss. During treatment, drugs are prescribed that reduce the tone of the uterus and reduce muscle contractility.
From 4-5 months, a woman can develop gestosis. It is manifested by increased blood pressure and edema. In this condition, the blood circulation of the uterus and baby is disrupted, and kidney function slows down. Because of this, protein is lost. The disease is diagnosed by its content in the urine. With central or other placenta previa due to gestosis, the patient’s condition is aggravated. In particular, recurrent bleeding is likely because clotting is impaired. This makes it very difficult to stop him.
When the placenta somewhat blocks the pharynx, blood supply and oxygen supply to the baby become difficult. Because of this, the child lags behind in development. If the placenta detaches, it will not grow back. This part does not take part in saturating the fetus with nutrients and other substances.
Due to the pathology, the child’s position also changes. Sometimes it is located across the abdomen. When it begins to move in this atypical position, the uterus becomes overstretched, leading to detachment. Childbirth in this case occurs by caesarean section. At the same time, doctors take into account how the child is positioned.
Features of childbirth
Bleeding is dangerous not only for the woman, due to the development of iron deficiency anemia, but also for the child. With this pathology, there is a partial disruption of oxygen access to the fetus, which leads to its hypoxia. With prolonged hypoxia, antenatal fetal death may occur, or after birth this condition may affect the physical and mental development of the child.
When such a diagnosis is made, and the due date approaches, every woman wonders whether she will be able to give birth herself. If there is no bleeding, labor is good, the woman’s condition is satisfactory, then such childbirth can be carried out through the natural birth canal, only with early opening of the membranes. But if any complications arise, then it is necessary to reconsider a cesarean section.
Diagnostics
The sooner doctors identify such a feature of pregnancy as the location of the placenta on the anterior wall, the easier it will be to prevent complications. Expectant mothers should undergo all examinations at the appointed time. Diagnosing the condition is not difficult. Without an ultrasound examination it is impossible to make an accurate diagnosis. Only an ultrasound scan of pregnant women gives a complete picture of the location of the fetus and possible risks. Doctors make the final verdict based on the results:
- gynecological examination;
- palpation of the abdomen;
- Ultrasound.
Symptoms and complications
Vaginal bleeding is a complication of placenta previa and its main symptom. In the case of complete presentation, heavy bleeding begins already in the second trimester and can occur periodically until childbirth.
Why does bleeding occur with placenta previa? In order to answer this question, you need to understand how the placental tissue is attached to the body of the uterus.
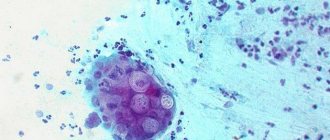
Placental tissue consists of villi - formations filled with conducting vessels. Some villi grow together with the uterus, others are immersed in the mother’s blood, which fills the so-called intervillous space (thickening of the endometrium in the place where the placenta is attached). Blood enters this space from small arterial vessels, the walls of which are partially destroyed by enzymes secreted by placental villi.
This entire complex mechanism works to ensure exchange between the organisms of mother and child: nutrients and oxygen come from the mother’s blood, and the placenta removes waste products from the fetus.
The child receives nutrition from the placenta through the umbilical cord, namely two arteries and a vein passing through it.
So, we see that the placenta literally fuses with the uterus . Time passes, the fetus develops, and the uterus increases in volume: this is especially noticeable in its lower part, where the pharynx is located, that is, exactly where the placenta is attached in the case of central presentation. Since the placental tissue is low-elastic, it “does not have time” to stretch after the rapidly enlarging uterus.
Partial placental abruption occurs . The connection is broken, and the vessels begin to bleed into the uterine cavity, pouring out from the genital tract with profuse bleeding, followed by spotting.
Usually, the first time this happens is when the woman is at rest or sleeping at night. As a rule, there is no pain during bleeding - this distinguishes it from bleeding during self-termination of pregnancy, when cramping pain in the lower abdomen is possible.
Closer to 30 weeks, bleeding can be caused by sex , other physical activity, or even an examination in a gynecological chair.
In addition to bleeding, women diagnosed with complete placenta previa may experience pain in the lower abdomen and lower back, uterine tone, and hypotension. Low blood pressure, in turn, is expressed in depression, weakness, drowsiness and dizziness.
If a pregnant woman has periodic, heavy bleeding in most cases, anemia . This condition is characterized by a decrease in hemoglobin levels and can lead to more serious complications during pregnancy.
The lack of oxygen in the mother’s blood (namely, hemoglobin carries oxygen from the respiratory system to all organs and tissues of the body) negatively affects the baby’s condition. As a rule, fetal development and growth retardation occur. Plus, this will affect the health of the already born child: with a high probability, he will also suffer from anemia in the first year of life.
Most likely, if there is heavy bleeding and a drop in the hemoglobin level of the expectant mother, the doctor will prescribe appropriate treatment, but she herself can additionally take care of her health by eating foods rich in iron and which have a positive effect on the level of hemoglobin in the blood:
- meat products, liver - with caution: it is rich not only in iron, but also in other vitamins, an excess of which can adversely affect the course of pregnancy;
- fruits: apples, pomegranates (be careful as they can cause constipation), peaches, apricots, dried fruits, etc.;
- berries; the richest in iron are blueberries, blueberries, as well as black currants and cranberries;
- vegetables and herbs: tomatoes, beets, pumpkin, dill, parsley, spinach, etc.;
- cereals and legumes: buckwheat, lentils, beans, peas;
- walnuts, dark chocolate.
In order for iron to be well absorbed, it is necessary to take it along with vitamin C (citrus fruits, broccoli, cranberries, pineapple), a sufficient amount of protein and not to consume black tea, coffee and milk at the same time as iron-containing foods, as they interfere with its absorption. It is necessary to ensure that constipation does not occur, which can cause bleeding. Read more about how to avoid this problem →
Associated complications
The central presentation itself and the bleeding it causes can cause other pregnancy complications, for example:
- premature complete placental abruption;
- premature rupture of membranes;
- delayed fetal development;
- the likelihood of incorrect fetal position (transverse, oblique, pelvic presentation);
- placenta accreta; they speak of accretion when the villi of the placental tissue have grown into the deep layers of the uterus, and the placenta cannot separate from it on its own during childbirth. In this case, doctors perform the separation manually, it is clear that this is fraught with critically severe bleeding, sometimes in such a situation there is only one way to save the life of the woman in labor - to remove the uterus;
- fetal hypoxia, the child actually lies on the placenta and with its movements can put pressure on it, pinching the vessels and impeding the access of oxygen.
Treatment of low placentation and features of the protective regime
As soon as the expectant mother learns about this diagnosis, the first questions she asks the doctor are whether it can be cured and whether the regimen needs to be changed. Let us consider these aspects in more detail.
Treatment of low placentation
To date, there are no drugs that can affect the placenta changing its location. Therefore, in the presence of this pathology, doctors always choose a wait-and-see approach. Or, if the placenta does not take the desired position, the method of delivery is adjusted as necessary. It is important to remember that low placentation in itself is not an indication for cesarean section.
Security mode
Due to the risk of uterine bleeding and placental abruption, doctors strongly recommend that a pregnant woman maintain a protective regime. You may have to be careful until birth.
The protective regime includes the following measures:
- Limit physical activity. It is necessary to cancel all sports activities. Only slow walking is allowed.
- Do not make sudden movements. The placenta, which is already under pressure, may not withstand the jerk, and then detachment will begin.
- Minimize travel, especially on public transport. Stress, shocks and sudden movements are something that is extremely undesirable with low placentation.
- Raise your legs while sitting. A slight elevation of the legs will increase blood circulation and help prevent fetal hypoxia.
- Strictly limit the weight of items picked up. Lifting weights is a very common cause of uterine bleeding. The maximum permitted weight is 2 kg.
- Rise from a lying position without jerking, using your arms and, if possible, not using your abdominal muscles.
The author of this article was also diagnosed with “low placentation” during pregnancy. I, frightened after the ultrasound, “surfed” the Internet and “tortured” the doctor - what to do, how to fix it. And the gynecologist gave me two very good, in my opinion, advice. The first of them was the words “mode without fanaticism”: yes, it is necessary to limit the load, not to make sudden movements. But this does not mean that you need to “hibernate” like a bear in winter. Because when you constantly lie in bed, the blood supply to the pelvic organs deteriorates, and this is dangerous for the baby, who, due to improper positioning, risks not receiving enough of the substances necessary for life. In addition, no ventilation of an apartment or house can compare with a walk in the fresh air. Only oxygenated blood can sufficiently transfer this same oxygen to a growing baby.
The second advice the doctor gave me concerned a universal static exercise - the knee-elbow pose. It is universal in that it will be useful both in case of increased tone of the uterus, and in case of pathology of the location of the placenta, and even in the case of abnormal position of the fetus.
This exercise is unique for several reasons:
- reduces pressure on the uterine os and low-lying placenta;
- improves blood flow;
- changes the direction of gravity.
I performed this exercise 3-4 times a day for 15 minutes. After this, I had to lie down for 30–40 minutes.
As a result, following these tips, by the next screening I heard that the placenta had noticeably risen to a normal level. It is impossible to say exactly what exactly influenced her migration and whether anything influenced her at all. But one thing I can say for sure is that it didn’t get worse, and I did everything I could do to change the situation.
Photo gallery: features of the protective regime
With low placentation, it is necessary to rise without sudden movements from a position “on your side”, helping with your hands
When sitting on a chair or in a chair, your legs should be elevated to improve blood flow in the pelvic organs
Physical activity with low placentation should be limited to leisurely walks
Diagnosis of placenta appendage
How is this anomaly of placental development diagnosed? Typically, diagnosing this deviation is not difficult.
The diagnosis is usually made in the second half of pregnancy, if the patient complains of repeated bleeding from the genital organs, an examination is carried out by a gynecologist, during which the doctor identifies signs characteristic of this anomaly. Currently, abnormalities in the development of the placenta are most often detected by ultrasound.
It is worth noting that modern research methods make it possible to quite accurately determine the location of the placenta, so you should not neglect routine ultrasounds, especially in the second and third trimester of pregnancy. This will minimize the occurrence of complications. Ultrasound diagnostics allows you to track the development of the placenta throughout pregnancy.
I would like to note that the causes of bleeding can be not only abnormalities in the development of the placenta; pathological processes occurring in the vagina and cervix can provoke bleeding.
What complications can occur with partial placenta previa?
As mentioned above, the main complication of placenta previa is bleeding , which can occur during pregnancy and at the beginning of the labor process.
In the case of partial placenta previa, quite often there is a threat of miscarriage , which is caused by increased uterine tone, and one of the symptoms is pain in the lower back and lower abdomen.
Many pregnant women with this pathology of placental development suffer from hypotension - a persistently reduced blood pressure, which in turn reduces performance, weakness and a feeling of weakness appear, the frequency of headaches increases in the pregnant woman, and fainting is possible.
anemia may develop . A decrease in hemoglobin in the blood of a pregnant woman is dangerous because the symptoms of hypotension in this case intensify and manifest themselves more clearly.
Due to anemia, the fetus may experience a lack of oxygen, and this in turn may affect the development of the child, and growth retardation may occur.
Due to the incorrect location of the placenta, the fetus quite often occupies an incorrect position in the uterine cavity, which significantly complicates natural delivery.
Treatment of marginal and lateral placenta previa
Examination and treatment of pregnant women with bleeding in the second half of pregnancy is recommended to be carried out in a hospital setting . The choice of appropriate treatment is determined by a specialist after examining the pregnant woman’s birth canal, determining how the placenta is presented, and the doctor must also take into account the intensity of bleeding and the general condition of the pregnant woman and the fetus. To do this, an examination is carried out with mirrors and an ultrasound; the pregnant woman must pass the necessary blood and urine tests.
Most often, women with placenta previa are prescribed strict bed rest . In case of large blood loss, small dose blood transfusions may be prescribed. Pregnant women are prescribed tocolytic and antispasmodic drugs, as well as hormonal drugs that help normalize uteroplacental circulation, strengthen the vascular wall and increase blood clotting.
Quite often, women with abnormal placental development are prescribed sedatives, such as motherwort and valerian. Prevention of fetal hypoxia and endometritis is necessary. Laxatives are contraindicated for women with marginal and lateral placenta previa; if necessary, a cleansing enema may be recommended.
Treatment of marginal or lateral presentation without bleeding can be done on an outpatient basis . In this case, a regimen and diet are prescribed that must be strictly followed.
For women with partial placenta previa, it is recommended to limit stress, both physical and emotional, it is worth excluding sexual intercourse, more time is needed in the air, a pregnant woman should sleep for at least 7-8 hours, it is recommended to rest in the afternoon.
Diet for lateral and marginal presentation is also very important for the health of the pregnant woman. It is necessary to consume as many foods rich in iron as possible: buckwheat, apples, pomegranate juice, turkey and beef, etc.
With placenta previa, constipation, which can cause bleeding, is undesirable, so you should make sure that your diet includes foods rich in fiber.
It is necessary to consume enough protein so that iron is better absorbed. Pregnant women with partial presentation should take multivitamins.
If all recommendations for treatment, regimen and diet are followed, the risk of complications that can negatively affect the development of the fetus is minimal.
Behavior rules
The most important rule of behavior is that you are not allowed to be nervous in any case. Any stress now will not work in your favor, as it provokes contractions of the myometrium, and this can provoke bleeding, which is very undesirable. In fact, many things can now further stimulate bleeding. Therefore, follow simple rules:
- Avoid physical activity. Your ceiling is a very short walk. And don't lift anything heavier than a two-liter water bottle. And even then, only from table height to drink.
- Lie down more . Moreover, preferably with a pillow under your feet and on your back.
- Watch your diet . Now you and your baby need hemoglobin, so eat buckwheat, pomegranates, apples, blueberries, beets, pumpkin, walnuts, dark chocolate. In moderation, of course.
- Avoid going to crowded places to avoid contracting a common cold or seasonal flu.
- Stay as close to your medical facility as possible , even go to the store for chocolate with an exchange card. Traveling to other cities is out of the question.
- If there is any bleeding, immediately notify your obstetrician-gynecologist , especially if it is heavy.
The whole point is that this pathology cannot be treated . But if you follow all the rules, there is a chance that in a couple of weeks an ultrasound will show that the baby’s place has “migrated” closer to the bottom of the uterus. In some cases, the patient is doing so well that until the moment of delivery the internal os is completely open, and natural childbirth does not present any problems. But in other cases, the woman herself will not be able to give birth.
Risks and impact of low placentation on pregnancy
Low placentation can lead, in severe cases, to placental abruption.
The condition of a low placenta is not as obviously dangerous as previa, but it also carries significant risks:
- Since the growing fetus puts pressure on the uterus, it begins to “oppress” the baby’s place. And this is fraught with uterine bleeding and, in extreme cases, placental abruption.
- Nature has designed it so that the blood supply to the bottom of the uterus is better than from below. Thus, the fetus, attached to its lower part, risks not receiving vital nutrients and oxygen.
At the same time, it must be remembered that this diagnosis is not final. After all, the baby’s place can change its location several times during pregnancy. This process is called “placental migration.”
Where should the placenta be located?
The most ideal option for placing the placenta in the uterine cavity is to attach it along the back wall in the upper part of the uterus, closer to the bottom. The fact is that the walls of the uterus are designed in such a way that as the fetus grows, they stretch very much. However, they do not stretch evenly.
The uterus is designed in such a way that stretching occurs mostly along the anterior wall . It becomes thinner and more extensible, while the back wall remains dense and is much less susceptible to stretching.
That is why nature prescribes the attachment of the fertilized egg to the posterior wall, because the placenta, unlike muscle tissue, does not have the ability to stretch. Thus, the placenta, fixed to the posterior wall, experiences significantly less stress, which is not at all beneficial for it.
So it turns out that the back wall is an ideal option for the attachment of the fetus, and then the development of the placenta.
Placenta location options
For various reasons, the fertilized egg can attach not only to the upper part of the posterior wall of the uterus, but also to other parts of it. Quite often there is a side mount: to the right or left of the back wall. In some, also not very rare cases, the placenta is attached to the anterior wall of the uterus.
All of these options for the location of the placenta are not considered a pathology, although in such cases there is a deviation from the ideal location intended by nature. Women with a lateral placenta, as well as with a placenta attached to the anterior wall, most often carry and give birth to children naturally without complications. Of course, among them there are also those who are faced with various pathologies, but, as a rule, they have other reasons for complications.
Of course, the placenta, located on the anterior wall, is subject to somewhat greater loads due to the constant stretching of the walls of the uterus, fetal movements, and maternal actions. To some extent, this increases the risk of damage to the placenta, premature detachment, and so on. The direction of placental migration may also change.
Due to the constant stretching of the muscles of the uterus, the placenta can gradually descend too close to the os of the uterus, and sometimes even block the exit from the uterus to the birth canal. If 6 centimeters or less remains between the edge of the placenta and the cervical os, they speak of low placentation, but if the placenta partially or completely blocks the exit from the uterus, this pathology is called placenta previa.
However, low placentation and placenta previa can be caused by a number of other reasons, which will be discussed later. Presentation along the posterior wall is much less common than along the anterior wall. We have already discussed above why this happens.
Symptoms of low placentation
The greater the distance from the placenta to the uterine os, the less likely it is that any symptoms of low placentation will appear. When the baby's place drops low, even to the point of presentation, signs similar to the symptoms of miscarriage appear:
- pulling pain in the abdomen;
- lower back pain;
- blood discharge is red or brown.
If abdominal pain can be safe and indicate a sprain, then bleeding is a very dangerous symptom, which requires immediate consultation with a specialist managing the pregnancy or an emergency doctor.
Causes
The reasons that cause placenta previa are divided into the following groups:
- caused by the general condition of the pregnant woman;
- due to the characteristics of the fetus.
In the first case, when the pathology is caused by the general condition of the woman, the most common reasons include the following:
- Operations that the pregnant woman has previously undergone (uterine curettage, fibroid removal, cesarean section).
- Endometrial pathology.
- The woman had several births with complications.
You can also consider factors such as the presence of uterine fibroids or endometriosis, congenital anomalies of the structure of the uterus, pregnancies with multiple pregnancies, and endocervicitis. The risk of placenta previa increases with each subsequent birth.
When considering the second case, when the pathology of the placenta is caused by the characteristics of the fetus, specific processes can be indicated. For example, this may be a problem with normal troboblast implantation if enzymatic processes do not appear in a timely manner, and the process of attachment of the fertilized egg is disrupted. This point should be considered only when the embryo descends to the lower part of the uterus.