Lymphocytic leukemia is a malignant tumor that affects the cells of the lymphoid tissue that make up the lymph nodes and other internal organs. According to the international classification of diseases, the ICD-10 code is assigned to C91.
Cells found in the blood - leukocytes - are designed to protect the human body from diseases and form immunity. In lymphocytic leukemia, a blood test shows that the lymphocyte has mutated and changed its structure. Gradually, the accumulated mutated cells begin to displace healthy ones and, when the number exceeds, a decrease in immunity is noted. At the last stage of the disease, the blood test includes 98% of atypical cells and 2% of healthy ones.
Classification of the disease
Before selecting therapeutic measures, chronic lymphocytic leukemia, like other diseases, is classified depending on the results of a diagnostic study. The classification of a pathological condition involves the identification of types and forms of the disease based on the identified nature of its course and stage of development.
The most common in global oncohematological practice is the Rai classification, which is based on the degree of risk of chronic lymphocytic leukemia:
- Short. This group includes 2 stages of the disease: 0, precancerous, noted when isolated peripheral blood lymphocytosis is detected, and stage 1 is assigned if lymphocytosis is accompanied by lymphadenopathy.
- Intermediate. This risk group also includes 2 stages of the disease – II, characterized by an enlarged spleen (splenomegaly) or liver (hepatomegaly) and III, in which chronic lymphocytic leukemia is accompanied by severe anemia. The changes that characterize any of the intermediate-risk stages are not directly related to enlarged lymph nodes.
- High. It is noted at the IV, final stage. It is considered the most dangerous, because lymphocytosis is accompanied by thrombocytopenia, which in most cases leads to death.
Read here: Types of classifications of lung cancer
The J. Binet classification of chronic lymphocytic leukemia involves dividing the disease into 3 groups:
- A – the pathological condition originates in the bone marrow or peripheral blood, with the involvement of one or two lymphatic areas and the absence of concomitant pathologies.
- B – oncology is accompanied by damage to more than three lymphatic areas, among which are the spleen and liver.
- C – simultaneously with the development of lymphocytic leukemia, patients are diagnosed with thrombocytopenia or anemia.
But most often, classical staging of the disease is used to prescribe treatment.
Chronic lymphocytic leukemia is divided in clinical practice into the following stages:
- Initial. Lymphocytes in the peripheral blood are slightly increased, the size of the liver and spleen practically does not differ from the norm, and there are no clinical symptoms. Treatment of the disease at this stage is not required. All assistance to the patient consists of dynamic monitoring.
- Expanded. The main manifestations of the disease appear, which become more and more pronounced as the disease progresses. At this stage, specific, quite aggressive treatment is necessary.
- Terminal. The final stage of the disease, during which thrombocytopenia and anemia occur. Often, as a complication, lymphoblastic leukemia develops, an acute form of the disease arising from immature blood cells.
Decoding the results
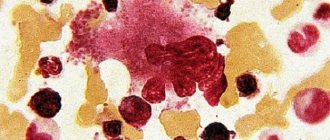
Lymphocytic leukemia blood test indicators are noted very quickly, since both biochemical and general analysis studies the number of leukocytes, only an inexperienced laboratory technician can miss atypical cells. Chronic myeloid leukemia blood picture will be noted in the general analysis - an increase in the total number of lymphocytes in the blood more than 5x109/l indicates a high probability of the disease. Sometimes, lymphoblasts and prolymphocytes can be detected in the analysis.
If you conduct a general blood test regularly, you can note increasing lymphocytosis, during which other cells that are part of the leukocyte formula will be displaced. At later stages of myeloid leukemia in children (CML) and adults, thrombocytopenia develops, and half-destroyed lymphocyte nuclei are found in the biomaterial, which in medicine are called Humnrecht's shadows.
A biochemical blood test can reveal disturbances in the functioning of the immune system, which is one of the most obvious signs of the development of a disease such as cellular chronic lymphocytic leukemia. At the initial stages of the disease, significant differences from the norm in blood biochemistry are not observed, but hypoproteinemia and hypogammaglobulinemia gradually appear. As the disease progresses, abnormalities in liver tests may occur.
A large number of immature leukocytes should also alert the doctor. There are two forms of the disease - acute and chronic. Acute lymphocytic leukemia is characterized by an accumulation of immature white blood cells in the bone marrow and thymus gland. This stage occurs most often in children from 2 to 5 years old, much less often in adolescents and adults. As for the chronic form of the disease, it is characterized by the accumulation of tumor leukocytes in the bone marrow and lymph nodes. In this case, the doctor may note in the biomaterial an accumulation of leukocytes that are more mature, but nonfunctional. This form of the disease affects people after 50 years of age, as it develops very slowly, so it can hide itself in the body for years.
Causes of chronic lymphocytic leukemia
What can trigger the onset of mutation in maturing lymphocytes is still unknown, but the fact that there is no connection between chronic lymphocytic leukemia and ionizing radiation and carcinogenic factors has a scientific basis. Finding out the causes of this form of the disease, scientists came to the unequivocal conclusion that in order for chronic lymphocytic leukemia to arise in the human hematopoietic organs, a genetic predisposition is necessary.
From this, clinicians concluded that the risk group for developing this disease includes people with a family history of blood cancer. It is they who are recommended to undergo annual screening tests necessary for the timely detection of chronic lymphocytic leukemia.
Prevention
The development of chronic lymphocytic leukemia is not associated with any negative external factors. All available studies have not found provoking factors that would clearly lead to the onset or sharp progression of the disease. The only known cause of CLL in medicine is a hereditary factor. Thus, the most important thing that an elderly person can do is to undergo regular medical examinations in order to catch the disease at the initial stage and try to slow it down as much as possible.
Symptoms that suggest the development of a dangerous disease
Chronic lymphocytic leukemia is a slowly progressive form of the disease, so the onset of the disease often goes unnoticed. The main symptoms that accompany incipient chronic lymphocytic leukemia are characteristic of many other, often non-malignant, ailments.
In order not to miss the onset of the development of a dangerous disease, experts recommend paying attention to such signs that are not entirely specific to cancer of the blood, such as:
- susceptibility to infectious diseases;
- constant, often unexplained, fatigue;
- losing weight with a normal diet;
- excessive night sweats.
Read here: Brain tumor in children
Often in the early stages there is an enlargement of the lymph nodes, not accompanied by pain. The sizes of the spleen and liver remain normal. If left untreated, the disease begins to progress, as a result of which the accompanying symptoms become more pronounced.
In the advanced and terminal stages it is noted:
- significant deterioration in general health;
- temperature rise to critical levels;
- increased blood levels of creatinine and urea;
- severe thrombocytopenia and hemorrhagic syndrome.
The following signs may indicate the development of lymphocytic leukemia:
- vomit;
- severe headaches;
- meningeal symptoms.
The appearance of these signs is associated with the penetration of mutated cells into the soft membranes of the brain, which always occurs in the final stages of the disease.
Briefly about the disease
Leukemia is a group of malignant tumor diseases that affect blood cells.
Over time, malignant, atypical cells accumulate in the body, which for one reason or another have mutated and bring destruction to the body instead of support.
Lymphocytic leukemia affects lymphocytes , the basis of immunity; these cells, unlike other components of the blood, are mostly concentrated in the lymphatic organs (liver, spleen, tonsils, lymph nodes, etc.) - only about 2% of lymphocytes move throughout the body along with the bloodstream.
When brain cells are damaged, the term myeloid leukemia is also used.
Lymphocytes provide local immunity, and there are 3 types of lymphocytes, which supports the body's defense at all levels: protection against foreign proteins, destruction of affected cells and counteracting cancer cells.
Anna Poniaeva. Graduated from the Nizhny Novgorod Medical Academy (2007-2014) and Residency in Clinical Laboratory Diagnostics (2014-2016).Ask a question>>
The first reason to show increased attention to the condition of the body is the so-called lymphocytosis - an excess of the norm of lymphocytes in the blood. Each age has its own standard indicators. You can calculate the individual norm using the formula 1.2 – 3.5x109/l; in general, the content of lymphocytes in the blood of an adult should not exceed 40% of the total number of leukocytes of all types.
Watch a video about this disease
Diagnosis of oncological blood pathology
The appearance of alarming symptoms is the basis for visiting a specialist and conducting a number of specific diagnostic studies to confirm or refute the alleged diagnosis.
The program for diagnostic examination of patients with suspected chronic lymphocytic leukemia consists of the following activities:
- A general blood test to identify pathological changes in its qualitative and quantitative composition.
- Ultrasound of the abdominal cavity, which reveals an increase in intraperitoneal lymph nodes, as well as the spleen and liver.
- Histological examination of external (cervical, parotid, axillary or inguinal) lymph nodes.
- Chest X-ray.
Important! In the early stages of the development of the disease, when not only there are no clinical manifestations of the disease, but also histological signs are not expressed, the appearance of the disease can only be suspected by chance, when performing a blood test and identifying changes in its composition. The doctor will be able to make the correct diagnosis, i.e., clarify that the patient is developing not a lymphoblastic type of pathological condition, but chronic lymphocytic leukemia, after a bone marrow puncture.
What therapy is used for this disease?
As mentioned above, lymphocytic leukemia in the vast majority of cases in elderly patients is a practically incurable and slowly progressive disease. However, treatment is not started immediately after the pathology is identified, especially in situations where the pathology remains stable.
When the progression of the pathological process is activated, leading to a significant deterioration in the patient’s medical condition and quality of life, standard chemotherapy protocols are used, including the complex use of alkylating drugs, nucleotide analogues and monoclonal antibodies.
Typical primary treatment regimen
The most typical and fairly effective regimen, which allows 80 percent of cases to achieve remission after initial use, is the use of a combination of rituximab, cyclophosphamide and fludarabine. Bendamustine is used as an alternative or adjunct to this practice.
As practice shows, a number of patients with active progression of the pathological process exhibit resistance to cytostatics. In this situation, the only effective method of reducing the risk of developing the terminal stage in the shortest possible time is allogeneic bone marrow transplantation. Maintenance treatment includes high doses of glucocorticosteroids and monoclonal antibodies such as alemtuzumab.
It is worth noting that regular intensive chemotherapy for people over 50 years of age is significantly hampered by the extremely poor somatic status of patients and the presence of a number of chronic diseases.
Therapy for relapses
In case of relapse of lymphocytic leukemia, the main direction of treatment is the use of targeted drugs based on tyrosine kinase inhibitors, as well as other highly selective analogues.
The new generation of experimental drugs, which are a separate class of antitumor immunomodulators with targeted effects, are currently not used in clinical practice, as they are in the final stages of testing.
The main methods of treatment practiced for this disease
It is quite difficult to completely rid a person of a disease such as chronic lymphocytic leukemia. Treatment of the disease is carried out using different methods, which are selected depending on the stage. Typically, the main therapeutic measures begin after the disease has entered an advanced, actively progressing phase. At this stage of development, treatment of chronic lymphocytic leukemia is carried out using drug therapy.
Chemotherapy for this disease is specific and involves the use of drugs from the following drug groups:
- Glucocorticoids. These medications are used as monotherapy for severe autoimmune complications. This treatment eliminates the development of a septic process that can provoke early death.
- Alkylating chemotherapy drugs (Cyclophosphamide, Chlorambucil). Chemotherapy with their help is allowed if a patient is diagnosed with a polymorphocytic form of pathology (Hairy cell leukemia), which is diagnosed very rarely.
- Monotherapy with Fludarabine. This drug is highly effective and is prescribed to the most severely ill patients, because allows you to achieve remission at advanced stages of the pathological process.
- Polychemotherapy regimens. Chemotherapy is usually prescribed with a combination of drugs according to the SOP regimen, which includes Prednisolone, Vincristine, and Cyclophosphamide.
Important! All medications intended to rid a person of chronic blood cancer should be prescribed only by a specialist. Self-medication for oncological lesions of the blood is strictly prohibited, as it can lead to irreparable consequences for the patient. It is also not recommended to treat a dangerous illness using folk remedies.
Radiation therapy is rarely prescribed, because exposure to radiation only alleviates the condition of a sick person for a short period of time. The main effect of ionizing rays occurs on the area of the lymph nodes, spleen and liver. Whole body irradiation is prescribed infrequently and only in the presence of certain medical indications, since the risks associated with it significantly exceed the possible positive effect.
Read here: Cancer of the antrum of the stomach: features of the disease
If there are no results of therapy, patients may be recommended a bone marrow transplant. This surgical intervention is considered the most effective treatment method, since in almost all cases it leads to a complete recovery of the patient. However, it is not possible for all patients with lymphocytic leukemia, and finding a suitable donor is very difficult.
Acute lymphocytic leukemia
Acute lymphocytic leukemia is a malignant type of lesion of the circulatory system, characterized by an increase in the number of lymphoblasts. The typical course of the disease is characterized by anemia, enlarged lymph nodes, constant bleeding, respiratory system disorder and damage to the central nervous system.
ALL is an oncological formation that is widespread among preschool children. In children, the primary appearance of the disease is observed; in adults, it appears as a complication after chronic lymphocytic leukemia. Prognosis for recovery in a child is ambiguous, since the pathology is characterized by relapses.
Causes
The etiology of the disease is based on scientists' assumptions about possible risk factors. The disease occurs due to the formation of rapidly multiplying cells. Genetic disorders that cause pathological changes arise in the womb.
People exposed to radiation are also at increased risk.
Radiation exposure from radiotherapy, which eliminated a tumor of another type, or exposure to an X-ray machine can also contribute to the development of pathology. The risk of developing acute leukemia increases when a pregnant woman comes into contact with certain groups of toxic substances.
Symptoms
The disease is characterized by rapid development and varied symptoms. The most common onset of the disease is symptoms: elevated and low-grade fever, weakness, signs of intoxication, discomfort and a feeling of fullness in the abdomen, frequent pain. As well as nosebleeds, swelling of the legs, skin rashes, and aching joints.
Groups of symptoms form syndromes that lead to malfunction of internal organs:
- anemic syndrome – characterized by low-grade fever, pre-fainting, fatigue;
- hyperplastic – internal organs increase in size;
- hemorrhagic - hemorrhages in skin areas appear in the form of small dots and large plaques;
- pain syndrome – due to intoxication of the body, pain and aches in the joints are felt.
Damage occurs to the skeletal system, brain, cranial nerves, digestive organs, and kidneys. There is a possibility of leukemic infiltration of the ovaries.
Cancer can also lead to a condition called myelogenous leukemia, which attacks bone marrow stem cells.
Diagnostics
The diagnosis is formulated using the results of OAM and biochemical blood tests. A mandatory research method is a myelogram. It is used to take a smear from the bone marrow for further examination. An increased ESR, anemia and leukocytosis are detected in the blood. The myelogram result indicates the presence of blast cells. To track the oncological process, a spinal puncture is prescribed. Using this method, the state of the nervous system is monitored.
Based on the results of the study, the patient is assigned a risk group and treatment is prescribed. An ultrasound is performed to examine the spleen and liver, to track the size and extent of the lesion. X-rays help identify the spread of metastases.
Additional diagnostics are carried out by immunophenotyping. It makes it possible to determine the immunophenotype of blast cells of bone marrow tumor formation. This helps to reliably diagnose pathology, divide patients into risk groups and prevent possible relapses.
Differential diagnostics are also carried out, excluding all possible variants of the disease and helping to make the correct diagnosis.
Treatment
Chemotherapy is used to treat ALL. There are regional, combined and intrathecal chemotherapy.
Carrying out a chemotherapy procedure
With regional chemotherapy, the drug substance is injected into the internal organs. Combination therapy involves the administration of several anticancer drugs. In intrathecal therapy, drugs are injected directly into the spine if there is a tumor in the spinal cord. In this case, the patient is additionally treated with intramuscular injections.
Chemical therapy has 3 stages:
- The induction stage is characterized by the introduction of a substance into the body in order to achieve the first remission. During the induction stage, cancer cells are destroyed. The duration of treatment is 2 weeks.
- At the consolidation stage, the remaining cells are destroyed. For this purpose, drugs are administered through a vein.
- The reinduction phase lasts several years to maintain remission and eliminate the possibility of relapse. During maintenance therapy, antibiotics are used.
Tolerance to chemotherapy is personal. The use of antitumor drugs has quite serious consequences for the body. This is due to the active decay of malignant cells, which lead to the formation of a large number of metabolic products, which causes intoxication of the body. Also, due to the low level of white blood cells in the blood, the likelihood of contracting infections is high. Therefore, it is important to follow the principles of patient care in clinics: complete isolation, frequent wet cleaning of the room, use of sterile clothing for medical staff.
If after 33 days of therapy there is no improvement or early relapses occur, the patient is prescribed a bone marrow transplant.
Internal and external radiation therapy are used when the tumor has spread to the spinal cord. It is used in the form of radiation radiation in the area of tumor formation or the introduction of a special substance into the tumor tissue.
Treatment of acute lymphocytic leukemia in children and adults is most effective in foreign countries. A clinic in Israel can help ensure a favorable outcome of treatment. The country's doctors use high-quality drugs and modern technologies in their practice.
Possible complications and consequences
It is not chronic lymphocytic leukemia itself that poses a threat to human life, but its complications.
The most common consequences of this type of blood cancer are:
- Increased infectivity (susceptibility to infectious lesions). This feature that accompanies the disease is noted in many patients. The appearance of this complication contributes to the fact that patients diagnosed with chronic lymphocytic leukemia may develop septic lesions, in most cases leading to blood poisoning and death.
- The development of extensive internal and external bleeding, which in most cases cannot be stopped due to poor blood clotting, which also leads to untimely death.
- Severe anemia. This complication impairs the functioning of the cardiovascular system and increases the chances of developing heart attacks.
But the greatest danger comes from acute lymphoblastic leukemia, which has joined lymphocytic leukemia. When such a complication occurs, the sick person has virtually no chance of further life.
Reasons for appearance
The causes of the occurrence and development of the disease are:
The above factors lead to the occurrence of the disease. Cell mutation occurs when they begin to divide uncontrollably. The disease can develop for years, but a complete cure cannot be achieved.
The disease causes enormous harm to the body, from which it is not possible to fully recover. Modern medicine can stop the development of the disease and alleviate the patient's condition . However, there is a high probability of complications and exacerbation of pathology.
Treatment of patients is carried out under the strict supervision of a doctor. In the later stages of the disease, the patient is placed in a hospital for examination and more serious monitoring of his well-being.
Lifespan
Chronic lymphocytic leukemia belongs to the category of incurable diseases of an oncological nature. But at the same time, this pathology may have a fairly favorable prognosis, which is associated with a long (10-15 years) period of its development. During this time, characterized by an asymptomatic course, in most clinical cases an accidental diagnosis occurs, after which productive treatment of chronic lymphocytic leukemia becomes possible, ending with the onset of long-term remission.
But in a quarter of cases, the disease is aggressive in nature and tends to progress rapidly, which makes the prognosis completely unfavorable, since death can occur in the coming months after the disease is diagnosed.
Statistics according to the Rai classification show the following life expectancy for chronic lymphocytic leukemia:
- Stages 0–II, with adequately selected treatment, give a person a chance of extending life to 5–20 years.
- Stages III–IV, despite the therapy, reduce life expectancy to 3–4 years.
- When blood cancer is aggravated by bone marrow failure, death can occur within 2-3 months after diagnosis due to the development of secondary oncological pathologies, which usually have a more aggressive course.
Main symptoms
One of the stages in the development of plasma disease is the uncontrolled proliferation of atypical cells.
The leukemic form of leukemia has the following stages in its course:
- blood stem cell degeneration or initiation;
- uncontrolled growth and reproduction;
- an increase in the number of atypical cells;
- spread of the tumor beyond the bone marrow or metastasis.
Chronic b-cell lymphocytic leukemia causes the patient to develop the following symptoms:
- general weakness;
- irritability;
- brokenness;
- weight loss;
- lack of appetite;
- temperature increase;
- enlarged and painful lymph nodes;
- necrotizing stomatitis;
- blue-red plaques on the skin;
- joint inflammation;
- damage to the mucous membranes;
- bleeding from the gums and nose;
- causeless hematomas;
- prolonged wound healing;
- difficult to stop even minor bleeding;
- anemia;
- hair loss;
- pale skin;
- increased heart rate;
- susceptibility to bacterial or viral infection;
- frequent colds;
- pustular skin lesion.
Stages of occurrence
To select the most optimal treatment methods, as well as to determine the prognosis of the disease, several stages of chronic lymphocytic leukemia are distinguished. At the very beginning of the development of the disease, only lymphocytosis is detected in the blood laboratory. On average, patients with this stage live more than 12 years. The degree of risk is considered minimal.
At stage 1, lymphocytosis is accompanied by enlarged lymph nodes, which can be determined palpably or instrumentally. The average life expectancy is up to 9 years, and the risk level is intermediate.
During stage 2, in addition to lymphocytosis, when examining the patient, splenomegaly and hepatomegaly can be determined. On average, patients live up to 6 years.
At stage 3, hemoglobin sharply decreases, and persistent lymphocytosis and an increase in lymph nodes are observed. The patient's life expectancy is up to 3 years.
When stage 4 occurs, thrombocytopenia is added to all these manifestations. The degree of risk in this case is very high, and the average life expectancy of patients is less than one and a half years.
Treatment
Treatment tactics for lymphocytic leukemia are determined based on existing signs of development and stage and laboratory tests. Treatment of benign lymphocytic leukemia can be reduced to observation, diet, or periodic herbal treatment. For prolymphocytic lymphocytic leukemia, massive drug treatment and a radical change in diet are carried out. In some forms of chronic lymphocytic leukemia, the main condition is good nutrition and treatment with folk remedies, carried out at the request of the patient and in agreement with the attending physician. But with lymphocytic leukemia, which is accompanied by rapid growth of atypical lymphocytes, damage to lymph nodes and internal organs, chemotherapy and even sometimes removal of the spleen are necessary. At this stage of lymphocytic leukemia, folk remedies are unlikely to improve the condition.
Nutritional Features
All patients with chronic lymphocytic leukemia need a rational distribution of rest and work schedules, as well as proper nutrition. Animal products should predominate in your usual diet, and fat consumption should also be limited. Consumption of fresh fruits, herbs, and vegetables is required.
For anemia, foods high in iron will be useful to normalize hematopoietic factors. You should regularly add liver to your diet, as well as vitamin teas.
Carrying out diagnostics
To make a diagnosis of chronic lymphocytic leukemia, a blood test is performed first. At the initial stage of the pathology, the clinical picture may change somewhat. The severity of leukocytosis largely depends on the stage of the disease.
Also, during the course of chronic lymphocytic leukemia, blood tests reveal a lack of red blood cells and hemoglobin. Such a disorder can be caused by tumor cells displacing them from the bone marrow. The level of platelets in the initial stages of the disease often remains within normal limits, but as the pathological process develops, their number decreases.
To confirm the diagnosis, examination methods such as:
- biopsy of the affected lymph node;
- bone marrow puncture;
- determination of immunoglobulin levels;
- cellular immunophenotyping.
Cellular examination of blood and bone marrow allows one to determine immunological markers of the disease in order to exclude the occurrence of other diseases and make a prognosis regarding its course.
What are the risk factors for developing chronic lymphocytic leukemia?
No specific environmental factors or factors associated with exposure to chemical or physical agents have been identified in the origin or development of this disease. If any of your family members have had lymphocytic leukemia, it is recommended to undergo regular preventive examinations and blood tests, because the risk of contracting the same disease increases 3 times. The earlier the diagnosis is made, the greater the likelihood of successful treatment. The risk of CLL increases significantly with age. Thus, there are about 30 new cases per 100,000 inhabitants aged 80-85 years.
Use of medications
Reviews about chronic lymphocytic leukemia in fifty percent of cases are positive, since with proper treatment the patient’s well-being can be normalized. Many patients say that chemotherapy in the initial stages can significantly prolong life and improve its quality.
In the absence of concomitant diseases, if the patient is under 70 years of age, a combination of drugs such as Cyclophosphamide, Fludarabine, and Rituximab is generally used. In case of poor tolerance, other combinations of drugs can be used.
For older people or those with concomitant diseases, more gentle combinations of drugs are prescribed, in particular, Obinutuzumab with Chlorambucil, Rituximab and Chlorambucil, or Cyclophosphamide with Prednisolone. If the disorder persists or relapses, patients may have their therapy regimen changed. In particular, this could be a combination of Idelalisib and Rituximab.
Very weakened patients with severe concomitant diseases are prescribed mainly monotherapy, in particular drugs that are relatively easily tolerated. For example, such as Rituximab, Prednisolone, Chlorambucil.
What kind of disease
Lymphocytic leukemia refers to one of the forms of oncology of hematopoietic tissues, which originates in the bone marrow and then spreads to the blood and immune system. The pathology occurs more often in men in the age group over 50 years (chronic form), as well as in children (acute form).
The development of a malignant process can be provoked by:
- hereditary predisposition and genetic disorders;
- pathologies of the immune system;
- negative effects of chemicals;
- receiving high doses of radiation;
- some types of viruses;
- intestinal infection;
- some medications;
- psycho-emotional stress state.
Life forecast
Chronic lymphocytic leukemia is a disease that cannot be cured, but has a satisfactory prognosis. The aggressive course of the disease with possible death is 15%. In other cases, life expectancy is 15-20 years from the moment of illness. The patient can live a full life, while following clinical recommendations - systematically examined, maintain a healthy lifestyle, improve nutrition and eliminate alcohol. A prerequisite is a constant diet.
Acute lymphocytic leukemia has a high probability of unfavorable prognosis. Statistically, children respond better to treatment. After treatment, 70% of children experience a 5-year period of remission. Adults undergo remission in 40-45% of cases. Children with a diagnosis can apply for disability and receive cash benefits.