The situation when a teenager who has no complaints and has no symptoms of ill health, suddenly after visiting a medical examination is informed that he has been found to have mitral valve prolapse (MVP), plunges many parents into panic. If you turn to the explanatory dictionary, the essence of prolapse is the protrusion or loss of an organ from its normal position.
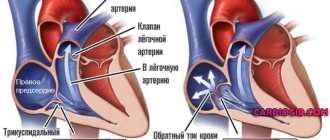
Thus, for the mitral valve, this means excessive bending of its leaflets into the cavity of the left atrium during ventricular contraction. With a high systolic force, conditions are created for the valve to open and lose its tightness, and some of the blood returns to the atrium through the gap between the leaflets.
The mechanism of pathology formation
The pathogenic phenomenon develops as a result of anatomical changes in a special structure that closes the lumen between the left atrium and the ventricle: the so-called mitral valve.
Essentially, it is a partition that prevents the reverse flow of blood. In a normal state, liquid connective tissue is released into the vessels and moves in a large circle throughout the body.
During the violation under consideration, prolapse of the valves is observed, that is, their protrusion into the atrium. The phenomenon of regurgitation occurs - reverse blood flow. This results in a decrease in the volume of fluid entering the systemic circulation, impaired hemodynamics and hypoxia of organs and tissues.
In the early stages, the process is not noticeable, which complicates diagnosis. As the deviation develops, there is a lack of functionality of the body structures, without the possibility of their radical restoration. The liver, kidneys, lungs, brain are under attack. Knowing the mechanism of development of the problem, it is possible to determine ways to overcome the process.
Complications
First of all, it is worth mentioning about mitral valve insufficiency, as a result of which the walls do not close tightly enough, which leads to the development of mitral regurgitation. This complication threatens the patient with the development of heart failure. Secondly, the patient may develop bacterial endocarditis. This complication is quite serious, since it is an inflammation of the endocardium, that is, the inner lining of the heart. This complication is characterized by a number of symptoms:
- increased body temperature;
- general malaise;
- heartbeat increased;
- pain in the joints;
- pinpoint hemorrhages on the skin;
- jaundice.
Another complication is the appearance of arrhythmia. As a result, prolapse of the left ventricle of the heart will bring a lot of problems to the patient, since the person will begin to suffer from frequent fainting and dizziness, lack of air and heartbeat disturbances. Prolapse of the cardiac neutral valve can lead to such a serious complication as a stroke. As you know, a stroke is a deviation in the blood supply to the brain. The consequences can be dire, including death. The occurrence of a stroke threatens people over 50 years of age.
Classification
According to the standard medical typing method, there are 3 or 4 stages of the disease, both are used. They are approximately equivalent, the second one is somewhat more carefully worked out.
Stage 1 (mild)
Characterized by minimal deviations from the heart and blood vessels. The amount of returning blood is approximately 10-15% of the total volume.
At stage 1, symptoms are completely absent, or the clinical picture is so poor that it is almost impossible to determine whether there are any problems. Signs are revealed only against the background of hard work and physical activity.
Recovery from minor prolapse is still possible and even probable; in general, doctors choose a wait-and-see approach; there are exceptions, if there are concomitant pathologies of the cardiac structures, delay is disastrous.
Stage 2 (moderate)
Regurgitation reaches 25% or more, symptoms are already present, but in small quantities, in addition, they are nonspecific.
It is impossible to say for sure what causes them to come to life: neurogenic problems, hormonal abnormalities or cardiac factors. Shortness of breath, chest pain and weakness. Here is the classic triad.
The prospects for a complete cure are worse, but you can keep the disease under total control and prevent it from progressing for many years, but the outcome is the same: sooner or later you will need surgery. The question of the advisability of immediate therapy is decided at the discretion of the cardiac surgeon in agreement with the patient.
Stage 3 (pronounced)
Accompanied by generalized hemodynamic disturbances. In addition to the complete clinical picture of the underlying condition, there are signs from distant organs and systems: liver, kidneys, cerebral structures in particular.
Regurgitation reaches 40% or more, this is already dangerous, cardiac arrest and death are possible. Treatment is surgical. Urgent or planned, after stabilization of the condition.
Stage 4 (terminal)
It is not always highlighted. Terminal stage. The disease rarely reaches this point because it is detected much earlier. The mortality rate is close to 100%, restorative measures are futile and cannot cope with anatomical disorders.
Grade 1 mitral valve prolapse with regurgitation is the most benign variant of the pathological process and the best moment to start therapy. Stage 2 is somewhat more difficult, but there are still chances for recovery.
Mitral valve prolapse: signs, degrees, manifestations, therapy, contraindications
One of the anomalies of cardiac development is mitral valve prolapse (MVP). It is characterized by the fact that its valves are pressed into the left atrial cavity at the moment when the left ventricle contracts (systole). This pathology has another name - Barlow syndrome, named after the doctor who first identified the cause of the late systolic apical murmur that accompanies MVP.
The significance of this heart defect has not yet been sufficiently studied. But most medical experts believe that it does not pose a particular threat to human life. Usually this pathology does not have pronounced clinical manifestations. It does not require drug therapy. The need for treatment arises when, as a result of MVP, a cardiac disorder (for example, arrhythmia) develops, which is accompanied by certain clinical manifestations. Therefore, the task of the cardiologist is to convince the patient not to panic and teach him basic muscle relaxation and auto-training exercises. This will help him cope with the emerging state of anxiety and nervous disorders, and calm his heart's excitement.
What is mitral valve prolapse?
To understand this, you need to imagine how the heart works. Oxygen-enriched blood from the lung enters the left atrial cavity, which serves as a kind of storage (reservoir) for it. From there it enters the left ventricle. Its purpose is to forcefully push all incoming blood into the mouth of the aorta for distribution to organs located in the area of the main blood circulation (great circle). The blood flow again rushes to the heart, but into the right atrium, and then into the cavity of the right ventricle. In this case, oxygen is consumed, and the blood is saturated with carbon dioxide. The pancreas (right ventricle) throws it into the pulmonary circulation (pulmonary artery), where it is re-enriched with oxygen.
During normal cardiac activity, at the moment of systole, the atria are completely freed from blood, and the mitral valve closes the entrance to the atria; no return flow of blood occurs. Prolapse prevents the sagging, stretched valves from closing completely. Therefore, not all the blood enters the aortic mouth during cardiac ejection. Part of it returns back into the cavity of the left atrium.
The process of retrograde blood flow is called regurgitation. Prolapse, accompanied by a deflection of less than 3 mm, develops without regurgitation.
Classification of PMC
Depending on how strong the regurgitation is (the degree of filling of the left ventricle with residual blood) they are distinguished:
1st degree
The minimum deflection of both sashes is 3 mm, the maximum is 6 mm. Reverse blood flow is insignificant. It does not lead to pathological changes in blood circulation. And it does not cause any associated unpleasant symptoms. It is believed that the patient’s condition with grade 1 MVP is within normal limits. This pathology is detected by chance. No drug treatment is required. But the patient is recommended to periodically visit a cardiologist. Sports and physical education are not contraindicated. Running, race walking, swimming, skiing and skating are good for strengthening the heart muscle. Figure skating and aerobics are useful. Admission to practice these sports at a professional level is issued by the attending cardiologist. But there are also limitations. The following are strictly prohibited:
- Weightlifting sports involving dynamic or static lifting of weights;
- Strength training sessions.
2nd degree
The maximum deflection of the sashes is 9 mm. It is accompanied by clinical manifestations. Symptomatic drug treatment is required. Sports and physical exercise are allowed, but only after consultation with a cardiologist who will select the optimal load.
3rd degree
The 3rd degree of prolapse is diagnosed when the valves bend by more than 9 mm. In this case, serious changes in the structure of the heart appear. The cavity of the left atrium expands, the ventricular walls thicken, and abnormal changes in the functioning of the circulatory system are observed. They lead to the following complications:
- MK insufficiency;
- Development of heart rhythm disturbances.
In grade 3, surgical intervention is required: suturing the valve leaflets or MV replacement. Special gymnastic exercises are recommended, which are selected by a physical therapy doctor.
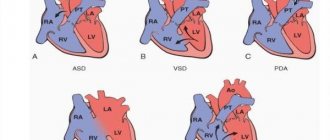
Based on the time of occurrence, prolapse is divided into early and late. In a number of European countries, including Russia, the classification of the disease includes:
- Primary (idiopathic or isolated) MV prolapse of hereditary, congenital and acquired origin, which may be accompanied by myxomatous degeneration of varying severity;
- Secondary, represented by undifferentiated connective tissue dysplasia and resulting from hereditary pathology (Ehlers-Danlos disease, Marfan disease) or other heart diseases (complications of rheumatism, pericarditis, hypertrophic cardiomyopathy, atrial septal defect).
Symptoms of MVP
The first and second degrees of MVP are most often asymptomatic and the disease is discovered by chance when a person undergoes a mandatory medical examination. In grade 3, the following symptoms of mitral valve prolapse are noted:
- Weakness and malaise appear, low-grade fever (37-37.5°C) persists for a long time;
- There is increased sweating;
- Headache in the morning and at night;
- There is a feeling that there is nothing to breathe and the person instinctively tries to absorb as much air as possible, taking a deep breath;
- Emerging pain in the heart is not relieved by cardiac glycosides;
- A stable arrhythmia develops;
During auscultation, heart murmurs are clearly audible (mid-systolic clicks caused by high tension of the chords, which were previously greatly relaxed). They are also called slamming valve syndrome.
When performing a heart ultrasound with Doppler, it is possible to detect reverse blood flow (regurgitation). MVP does not have characteristic ECG signs.
Video: MVP on ultrasound
1st degree, 13-year-old boy, vegetation at the ends of the valves.
Etiology
It is believed that two reasons play a decisive role in the formation of PMC:
- Congenital (primary) pathologies transmitted by inheriting the abnormal structure of the fibers that form the basis of the valve leaflets. At the same time, the chords connecting them to the myocardium gradually lengthen. The sashes become soft and stretch easily, which contributes to their sagging. The course and prognosis of congenital MVP are favorable. It rarely causes complications. There were no cases of heart failure. Therefore, it is not considered a disease, but simply attributed to anatomical features.
- Acquired (secondary) cardiac prolapse. It is caused by a number of reasons, which are based on the inflammatory-degenerative process of connective tissue. Such processes include rheumatism, accompanied by damage to the mitral valve leaflets with the development of inflammation and deformation in them.
MVP therapy
Treatment of mitral valve prolapse depends on the degree of regurgitation, the causes of the pathology and the complications that arise, however, in most cases, patients do without any treatment. Such patients need to be explained the essence of the disease, reassured and, if necessary, prescribed sedatives.
Of no small importance is the normalization of work and rest, adequate sleep, and the absence of stress and nervous shock. Despite the fact that heavy physical activity is contraindicated for them, moderate gymnastic exercises and walking, on the contrary, are recommended.
Among the medications, patients with MVP are prescribed:
- For tachycardia (rapid heartbeat), it is possible to use beta-blockers (Propranolol, Atenolol, etc.);
- If MVP is accompanied by clinical manifestations of vegetative-vascular dystonia, magnesium-containing drugs (Magne-B6), adaptogens (Eleutherococcus, Ginseng, etc.) are used;
- It is mandatory to take vitamins B, PP (Neurobeks Neo);
- Grade 3 and 4 MVP may require surgical treatment (suturing the leaflets or valve replacement).
MVP in pregnant women
MVP develops much more often in the female half of the population. This is one of the most common heart pathologies detected during mandatory examination of pregnant women (echocardiography, cardiac ultrasound), since many women, having grade 1-2 MVP, may not have been aware of their existing anomaly. Mitral valve prolapse may decrease during pregnancy, which is associated with increased cardiac output and decreased peripheral vascular resistance. During pregnancy, in most cases, prolapse proceeds favorably, but pregnant women more often experience heart rhythm disturbances (paroxysmal tachycardia, ventricular extrasystole). MVP during gestation is often accompanied by gestosis, which can lead to fetal hypoxia and growth retardation. Sometimes pregnancy ends in premature birth or labor weakness is possible. In this case, a caesarean section is indicated.
Drug treatment of MVP in pregnant women is carried out only in exceptional cases with a moderate or severe course with a high probability of arrhythmia and hemodynamic disturbances. It is accompanied by four major syndromes.
Autonomic-vascular dysfunction:
- Chest pain in the region of the heart;
- Hyperventilation, the central symptom of which is an acute lack of air;
- Heart rhythm disturbances;
- Feeling chills or increased sweating due to decreased thermoregulation;
- Gastrointestinal (gastrointestinal) disorders.
Vascular dysfunction syndrome:
- Frequent headaches; swelling;
- Decreased temperature in the extremities (icy hands and feet);
- Goosebumps.
Hemorrhagic:
- The appearance of bruises with the slightest pressure,
- Frequent nose or gum bleeding.
Psychopathological syndrome:
- Feelings of anxiety and fear
- Frequent mood changes.
In this case, the pregnant woman is at risk. She should be observed, treated and give birth in specialized perinatal centers.
An expectant mother diagnosed with stage 1 MVP can give birth naturally under normal conditions. However, she must follow the following recommendations:
- She should avoid prolonged exposure to heat or cold, in stuffy rooms with high humidity, where there are sources of ionizing radiation.
- It is contraindicated for her to sit for too long. This leads to stagnation of blood in the pelvis.
- It is better to relax (read books, listen to music or watch TV) while reclining.
A woman who has been diagnosed with mitral valve prolapse with regurgitation should be monitored by a cardiologist throughout her pregnancy so that developing complications are recognized in a timely manner and measures are taken to eliminate them in a timely manner.
Complications with MV prolapse
Most complications of mitral valve prolapse develop with age. An unfavorable prognosis for the development of many of them is given mainly to older people. The most serious complications that pose a threat to the patient’s life include the following:
- Various types of arrhythmias caused by dysfunction of the autonomic-vascular system, increased activity of cardiomyocytes, excessive tension of the papillary muscles, and disruption of atrioventricular impulse conduction.
- MK insufficiency caused by retrograde (in the opposite direction) blood flow.
- Infectious endocarditis. This complication is dangerous because it can cause rupture of the chords connecting the MV to the walls of the ventricle or separation of part of the valve, as well as various types of embolism (microbial, thromboembolism, embolism with a valve fragment).
- Neurological complications associated with cerebral embolism (cerebral infarction).
Prolapse in childhood
In childhood, MV prolapse occurs much more often than in adults. This is evidenced by statistical data based on the results of ongoing research. It is noted that in adolescence, MVP is diagnosed twice as often in girls. Children's complaints are of the same type. Basically, this is an acute lack of air, heaviness in the heart and chest pain.
The most common diagnosis is grade 1 anterior leaflet prolapse. It was detected in 86% of examined children. Stage 2 disease occurs in only 11.5%. MVP III and IV with degree regurgitation are very rare, occurring in no more than 1 child out of 100.
Symptoms of MVP manifest themselves differently in children. Some people practically do not feel abnormal heart function. In others it manifests itself quite strongly.
- Thus, chest pain is experienced by almost 30% of adolescent children who have been diagnosed with MVC (mitral valve prolapse). It is caused by various reasons, among which the most common are the following:
- chords that are too tight;
- emotional stress or physical stress leading to tachycardia;
- oxygen starvation.
- The same number of children experience heart palpitations.
- Often teenagers who spend a lot of time at the computer, preferring mental activity to physical activity, are prone to fatigue. They often experience shortness of breath during physical education classes or when doing physical work.
- Children diagnosed with MVP often exhibit neuropsychological symptoms. They are prone to frequent mood swings, aggressiveness, and nervous breakdowns. Under emotional stress, they may experience short-term fainting.
During the examination of the patient, the cardiologist uses various diagnostic tests, through which the most accurate picture of MVP is revealed. The diagnosis is established when noises are detected during auscultation: holosystolic, isolated late systolic or in combination with clicks, isolated clicks (clicks).
The disease is then diagnosed by echocardiography. It makes it possible to determine functional deviations of the myocardium, the structure of the MV leaflets and their prolapse. The defining signs of MVP according to EchoCG are the following:
- The MK valves are enlarged by 5 mm or more.
- The left ventricle and atrium are enlarged.
- When the ventricle contracts, the valves of the MV bend into the atrium chamber.
- The mitral annulus is dilated.
- The chords are elongated.
Additional signs include:
- Aneurysm of the septum between the atria;
- The aortic root is dilated.
The x-ray shows that:
- The pattern of the lungs is not changed;
- Bulging of the pulmonary artery arch is moderate;
- The myocardium looks like a “hanging” heart with reduced dimensions.
The ECG in most cases does not show any changes in cardiac activity associated with MVP.
Heart valve prolapse in childhood often develops due to a lack of magnesium ions. Magnesium deficiency disrupts the process of collagen production by fibroblasts. Along with a decrease in magnesium content in the blood and tissues, there is an increase in beta-endorphin and an imbalance in electrolyte balance. It has been noted that children diagnosed with MVP are underweight (inappropriate for height). Many of them have myopathy, flat feet, scoliosis, poor development of muscle tissue, and poor appetite.
It is recommended to treat MVP with a high degree of regurgitation in children and adolescents, taking into account their age group, gender and heredity. Based on the severity of the clinical manifestations of the disease, a treatment method is selected and medications are prescribed.
But the main emphasis is on changing the child’s living conditions. Their mental load needs to be adjusted. It must alternate with physical exercise. Children should visit a physical therapy room, where a qualified specialist will select the optimal set of exercises, taking into account the individual characteristics of the course of the disease. Swimming lessons are recommended.
In case of metabolic changes in the heart muscle, the child may be prescribed physiotherapeutic procedures:
- Galvanization of the reflex segment zone, with intramuscular administration of thiotriazoline at least two hours before the start of the procedure.
- Electrophoresis with calcium for vagotonic disorders.
- Electrophoresis with bromine for sympathicotonic dysfunctions.
- Darsonvalization.
The following medications are used:
- Cinnarizine - to increase blood microcirculation. The course of treatment is from 2 to 3 weeks.
- Cardiometabolites (ATP, Riboxin).
- Beta-blockers - for MVP accompanied by sinus tachycardia. The dosage is strictly individual.
- Antiarrhythmic drugs for persistent arrhythmias accompanying grade 3 MVP.
- Vitamin and mineral complexes.
Herbal medicine preparations are also used: horsetail decoction (it contains silicon), ginseng extract and other drugs with a sedative (calming) effect.
All children with BMD should be registered with a cardiologist and regularly (at least twice a year) undergo examinations aimed at timely detection of all changes in hemodynamics. Depending on the degree of MVP, the possibility of playing sports is determined. With prolapse of the 2nd degree, some children require transfer to a physical education group with a reduced load.
Recommendations for playing sports
With prolapse, there are a number of restrictions for playing sports at a professional level with participation in important competitions. You can familiarize yourself with them in a special document developed by the All-Russian Society of Cardiologists. It is called “Recommendations for the admission of athletes with disorders of the SS system to the training and competitive process.” The main contraindication for intensive training of athletes and their participation in competitions is prolapse, complicated by:
- Arrhythmia recorded by Holter monitoring (24-hour ECG);
- Relapses of ventricular and supraventricular tachycardia;
- Regurgitation above grade 2, recorded on echocardiography;
- A large decrease in blood output - up to 50% or lower (detected by echocardiography).
All people with mitral and tricuspid valve prolapse are contraindicated in the following sports:
- In which it is necessary to perform jerk-like movements - shot put, discus or javelin throwing, various types of wrestling, jumping, etc.;
- Weightlifting, associated with lifting weights (weights, etc.).
Video: a fitness trainer’s opinion on MCP
Prolapse at military age
Many young people of military age diagnosed with mitral or tricuspid valve prolapse have a question: “Are they allowed to join the army with such a diagnosis?” The answer to this question is ambiguous.
With MVP of the 1st and 2nd degrees without regurgitation (or with regurgitation of 0-I-II degrees), which does not cause cardiac dysfunction, the conscript is considered fit for military service. Since prolapse of this type refers to the anatomical features of the structure of the heart.
Based on the requirements of the “Schedule of Diseases” (Article 42), a conscript is considered unfit for military service in the following cases:
- He should be diagnosed with: “Primary MV prolapse of the 3rd degree. Heart failure of functional class I-II.”
- Confirmation of the diagnosis by echocardiographic examination and Holter monitoring. They must register the following indicators: the rate of shortening of myocardial fibers during blood circulation is reduced;
- regurgitation flows appear above the aortic and mitral valves;
- the atria and ventricles have increased sizes, both during systole and diastole;
- blood ejection during ventricular contraction is significantly reduced.
But there is one nuance here. The condition called “Heart failure” is classified into 4 functional classes. Of these, only three can grant exemption from military service.
- I f.k. - the conscript is considered fit for service in the Republic of Armenia, but with minor restrictions. In this case, the decision of the military conscription commission may be influenced by the symptoms accompanying the disease, causing intolerance to physical activity.
- At II f.k. the conscript is assigned fitness category “B”. This means that he is fit for military service only in time of war or in emergency situations.
- And only III and IV f.k. They are given a complete and unconditional write-off from military service.
Mitral, tricuspid, aortic prolapse and human health
Heart valves are valves that regulate the movement of blood through the heart chambers, of which the heart has four. Two valves are located between the ventricles and the blood vessels (pulmonary artery and aorta) and two others are on the path of blood flow from the atria to the ventricles: on the left is the mitral valve, on the right is the tricuspid valve. The mitral valve consists of anterior and posterior leaflets. Pathology can develop on any of them. Sometimes this happens on both at once. The weakness of the connective tissue does not allow them to be kept in a closed state. Under blood pressure, they begin to bend into the chamber of the left atrium. In this case, part of the blood flow begins to move in the opposite direction. Retrograde (reverse) flow can occur with pathology of even one leaflet.
The development of MVP may be accompanied by prolapse of the tricuspid valve (tricuspid), located between the right ventricle and the atrium. It protects the right atrium from the return flow of venous blood into its chamber. The etiology, pathogenesis, diagnosis and treatment of PTC are similar to MV prolapse. A pathology in which prolapse of two valves occurs at once is considered a combined heart defect.
Small and moderate MV prolapse is detected quite often in absolutely healthy people. It is not dangerous to health if regurgitation of 0-I-II degree is detected. Primary prolapse of the 1st and 2nd degrees without regurgitation refers to minor anomalies of cardiac development (MARS). When it is detected, there is no need to panic, since, unlike other pathologies, progression of MVP and regurgitation does not occur.
The cause for concern is acquired or congenital MVP with grade III and IV regurgitation. It is a severe heart defect that requires surgical treatment, since during its development, due to an increase in the volume of residual blood, the left atrium chamber is stretched and the thickness of the ventricular wall increases. This leads to significant overload of the heart, which causes heart failure and a number of other complications.
Rare cardiac pathologies include aortic valve prolapse and pulmonary valve prolapse. They also usually have no significant symptoms. Treatment is aimed at eliminating the causes of these anomalies and preventing the development of complications.
***
If you have been diagnosed with mitral or any other heart valve prolapse, there is no need to panic. In most cases, this anomaly does not cause significant changes in cardiac activity. This means you can continue your normal lifestyle. Perhaps just once and for all to give up bad habits that shorten the life of even an absolutely healthy person.
Video: mitral valve prolapse in the program “Live Healthy!”
Features of hemodynamics
Partially the issue has already been addressed. As a result of the impossibility of complete closure of the valves of the anatomical septum, a reverse flow of blood occurs from the left ventricle into the corresponding atrium, from where the liquid connective tissue came.
As a result, the volume of circulation in a large circle is disrupted, depending on the stage, significantly or minimally. In any case, hemodynamics decreases at the level of the entire organism.
Hypoxia (oxygen starvation) increases gradually, first manifesting itself as pulmonary symptoms, then cerebral. Possible fatal complications. It all ends in multiple organ failure.
Bringing hemodynamics back to normal is the main goal of therapy. In the later stages of the disease, recovery and radical improvement are no longer possible. The effect is supportive, but at this stage he is severely disabled: he cannot not only play sports, but also perform everyday household duties, even walk.
For your information:
Against the background of numerous organic disorders, there is a high risk of death over the course of several months or years. It gets to the point where it becomes dangerous to correct mitral valve prolapse (abbreviated MVP), and the patient may not survive the operation.
What it is
Mitral valve prolapse (hereinafter referred to as MVP) is the most common valvular pathology of the heart.
The disease affects approximately 2.5% of the world's population. It is often found in children and adolescents. The predominant number of patients are women and girls. MVP is distinguished separately from valvular heart defects for two reasons. Firstly, the anomaly has a different nature of occurrence. Secondly, unlike heart defects, this pathology is benign, but can also have unpleasant consequences. Often a person does not know about its presence: MVP becomes an “accidental finding” during a medical examination or examination for another disease.
To understand the essence of this disease, it is important to understand the process of valve operation. The human heart has 4 cavities, or chambers. Normally, blood circulates in only one direction: from the atria to the ventricles, then to the large vessels (aorta and pulmonary artery). This is possible thanks to the synchronous operation of the valves, which open and close at the right time. Closed valves prevent regurgitation - the direction of blood flow in the opposite direction.
With MVP, its main function is disrupted. During the systole phase, when the left ventricle contracts, the valve leaflets cannot withstand the blood pressure and begin to protrude into the cavity of the left atrium. The main problem is that some of the blood returns to the left atrium. This is called regurgitation. All the ensuing adverse effects of MVP are associated with this process. Severe regurgitation can lead to disability.
Reasons for violation
Despite the fact that the mechanism of development of the pathology is well known, the exact factors in the development of the process cannot be named.
Presumably, the following points play a role:
- Congenital and acquired heart defects. They may be the result of intrauterine problems or a combination of circumstances. Peak detection occurs in the first years of life and adolescence. There are usually no symptoms as such, which makes these diseases deadly. The destruction of cardiac structures is ongoing, but there are no signs, the patient is confident in his own health. The result is a diagnosis made during an autopsy. There is only one method of prevention - regularly visit a cardiologist and carry out preventive examinations (ECG, ECHO) at least once a year.
- Metabolic disorder. First of all, changing the movement of potassium, magnesium and sodium partly. Deviations in ventricular repolarization occur, the heart does not work properly, and interruptions are noted. The cardiac structures themselves do not receive enough blood, and degenerative phenomena begin in all formations, including valves. In the long term, this is fraught with prolapse or other phenomena. Treatment is effective in the early stages.
- Heart attack. Acute necrosis of muscle tissue. Occurs against the background of acquired coronary insufficiency. The change is potentially lethal. Up to 60-70% of all patients die, many later, as a result of heart failure. It is easier to prevent such a condition than to cope with its consequences.
- Endocarditis and similar pathological processes of an infectious, toxic or autoimmune nature. A guarantee (so to speak) of preventing catastrophic complications, such as destruction of the atria, is urgent treatment in a hospital setting. Antibiotics, antivirals, and antihypertensive drugs are used.
- Infectious and inflammatory problems of the throat and upper respiratory tract. From classic tonsillitis to chronic tonsillitis and other processes in the paranasal sinuses. Caries, gingivitis, and gum changes also have an impact. It is not recommended to delay treatment; there is a risk of developing cardiac abnormalities.
- Ischemic disease. It is issued if the pathological process does not reach a certain critical mass for the formation of a heart attack. Requires constant, lifelong support, since there is a high probability of muscle layers stopping or dying.
Development factors require close attention. Knowing the features and probable moments of the formation of a pathogenic phenomenon, it is possible to determine approximate preventive measures.
Mechanism of development, diagnosis and treatment of aortic calcification
Have you been struggling with HYPERTENSION for many years without success?
Head of the Institute: “You will be amazed at how easy it is to cure hypertension by taking it every day...
Read more "
Calcium is the main building element in the human body, but its accumulation negatively affects health. If calcium is not excreted from the body, it begins to enter the blood. This provokes calcium deposition on the walls of blood vessels, including the aorta. Thus, calcification of the aortic valve occurs. This condition is dangerous because the largest vessel in the body loses its elasticity. Increased blood pressure can cause aortic rupture and instant death.
Development mechanism and reasons
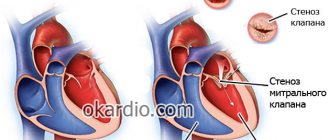
The disease spreads not only to the walls of the aorta, but also to the aortic valve of the heart. According to statistics, every fifth valve defect is caused by calcification. This acquired pathology of the aortic valve is also called true stenosis.
Aortic calcification leads to changes in the structure of the valve, fusion of the leaflets, which provokes its insufficiency. This phenomenon causes a sharp pressure drop to occur as blood flows from the left ventricle to the aorta. In the ventricular cavity, blood pressure is increased, but at the mouth of the aorta it decreases sharply. Because of this, the ventricular cavity loses its elasticity, and its walls hypertrophy. This phenomenon causes a weakening of the functions of the left ventricle and a decrease in the volume of blood ejected from it. The hemodynamic overload from which the left ventricle suffers extends to the atrium and the vessels of the pulmonary circulation.
Due to the accumulation of calcium in the body, a person may develop calcification of not only the aortic valve, but also the mitral valve. In this case, calcium is deposited on the annulus fibrosus of the valve. Many people with calcification do not have valve dysfunction, but they are at risk of developing mitral regurgitation, which occurs when blood flows from the left ventricle into the left atrium during systole.
The causes of excessive calcium accumulation in the blood are:
- Age: In older people, calcium is washed out of the bones and enters the blood.
- Kidney disease: The inability of the excretory system to remove calcium allows it to accumulate in the body.
- Increased absorption of calcium in the intestines.
- Disturbance in the process of calcium absorption by bone tissue.
- Diabetes.
- Heart defects.
- Obesity.
- Unhealthy Lifestyle.
- Heredity.
- Atherosclerosis.
- Rheumatic valvulitis.
Symptoms
With calcification of the valve apparatus, a person notices the following symptoms:
- shortness of breath;
- heart rhythm disturbance;
- heartache;
- episodes of loss of consciousness.
Severe valve calcification can cause an attack of cardiac asthma, or suffocation. A buildup of calcium on the inside of the aortic wall often causes it to rupture. Signs of this dangerous condition are:
- severe pain in the chest or abdomen;
- a sharp decrease in blood pressure and pulse;
- loss of consciousness;
- nausea and vomiting;
- paleness of the skin or its cyanosis;
- involuntary defecation (urination).
With such symptoms, a person needs emergency medical care.
Diagnosis and treatment
The presence of calcification of the aorta and aortic valve can be determined using the following methods:
- ultrasound examination of the heart;
- chest x-ray;
- cardiac catheterization;
- ventriculography;
- aortography;
- ultrasonography.
The research results are interpreted by the attending physician. After making a diagnosis, the specialist determines treatment tactics for the patient. Typically therapy includes:
- Taking calcium antagonists with a high concentration of magnesium: Verapamil, Tiapamil, Felipamina.
- Taking medications to stabilize blood pressure: Nitro-5, Sustonita, Arfonada.
- Taking diuretics: Veroshpiron, Furosemide.
If calcification provokes atrial fibrillation, the person is advised to take Digoxin. If there is a threat of developing heart failure or aortic rupture, the decision is made in favor of surgical treatment. For calcinosis, the following is carried out:
Why do you feed pharmacies if hypertension is afraid of the usual like fire...
Tabakov has revealed a unique remedy against hypertension! To reduce blood pressure while preserving blood vessels, add to…
- Replacement of the affected valve with an artificial one (if the aortic valve is affected).
- Aortic balloon valvuloplasty or bypass using a vascular graft (if the entire aorta is affected).
The development of calcification can be prevented with the help of folk remedies. They can be an effective addition to traditional therapy. But before taking folk remedies against calcification, you should consult your doctor.
Garlic is used to slow down the process of calcification. It helps normalize blood pressure, prevent atherosclerosis and dissolve calcium deposits on the walls of blood vessels. You can prepare an effective remedy at home:
- You need to take 300 grams of chopped garlic and pour a glass of vodka over them.
- The container with the workpiece is placed in a dark place for a week.
- For the first 5 days, the drug is taken three times a day, 1 drop. It is recommended to add the medicine to milk. Every day the number of drops is increased by 1 (for each dose). So, on day 5 a person should take 15 drops of garlic tincture.
- From the 5th day, the number of drops taken at a time is reduced by 1.
- From the 10th day you need to take 25 drops per day.
The course of treatment is 4 months with a 2-month break.
A remedy prepared according to the following recipe is considered effective:
- You need to take 100 grams of dry chamomile, birch buds and motherwort. Everything should be crushed.
- The herbal mixture should be poured with 0.5 liters of boiling water and left for 20 minutes.
- A glass of strained broth along with a teaspoon of honey is drunk before bed, and a second portion in the morning on an empty stomach.
During the treatment of calcinosis, you should limit the consumption of foods rich in calcium. It is also recommended to control body weight and prevent gaining extra pounds.
Symptoms and complaints of patients
Manifestations occur only in the later stages. There is no acute form of mitral valve prolapse, since the development of changes is gradual.
At the initial stages, the signs are minimal, the patient does not pay attention to them. As things get worse, catastrophic transformations occur.
An approximate list of symptoms:
- Moderate intensity of chest pain. They press, prick, burn. Discomfort radiates to the stomach, epigastric region, shoulder blade, and arms. It is extremely rare that the pain is severe; more often it is an indication of an emergency condition.
- Tachycardia. Constant sleep disturbances such as inability to rest at night. Possible nightmares. Fast contractions don't disappear at all. Gradually the patient adapts to his own condition.
- Dizziness. Nausea. Indication of brain damage, remove pathological changes urgently with beta blockers (Anaprilin, Metoprolol). Possible vomiting. But it is of reflex origin, so relief does not come after the episode.
- Dyspnea. As a rule, against the background of a long course of the main process. Prolapse of the anterior leaflet of the mitral valve of the 1st degree is accompanied by such insignificant manifestations that it does not create a feeling of danger or discomfort, prompting the patient to visit a cardiologist. As it develops, shortness of breath becomes unbearable, the patient cannot perform daily duties, is unable to move, and sometimes even get out of bed.
- Arrhythmias. This symptom has been partially described. In addition to acceleration of contractions (paroxysmal type), fibrillations and group extrasystoles are possible, which can lead to cardiac arrest without prospects for resuscitation. It is impossible to prevent this, only as part of complex treatment of mitral valve prolapse.
- Feeling of constant fatigue, decreased performance.
- Fainting and syncope. Accompany the later stages. This is a bad sign because it indicates homodynamic disturbances when blood circulation in the brain weakens.
The clinical picture at stages 2-3, especially at stages 4, is bright, but not specific. There are no pathognomonic manifestations. Objective methods put an end to the question.
Frequent symptoms
Most people with “harmless” mitral valve prolapse, especially children and adolescents, have an asymptomatic course of the disease and nothing bothers them. Sometimes patients complain only of minor chest discomfort. I would like to note that the clinical picture may not correspond to the degree of pathology.
Symptoms of mitral valve prolapse:
- pain in the left side of the chest or behind the sternum: stabbing, pressing, squeezing, moderate intensity. The duration varies from a few seconds to a day. Pain can occur either during a strong experience or performing physical exercise, or spontaneously, for no apparent reason. Often the unpleasant sensation is accompanied by a feeling of lack of air, the appearance of cold sticky sweat, anxiety and even fear of death;
- dizziness due to low blood pressure;
- rapid heartbeat, sensations of “interruptions, rolling, freezing” in the chest;
- frequent pre-fainting conditions, in which a person experiences a feeling of lightheadedness and nausea, accompanied by flashing spots before the eyes and blurred vision;
- with severe and prolonged mitral regurgitation, signs of congestive heart failure are added - difficulty breathing, rapid onset of fatigue, swelling in the legs, especially in the evening, heaviness in the right side due to an enlarged liver.
Also, in people with mitral valve prolapse, often due to hereditary connective tissue disorders, I observe symptoms of autonomic dysfunction:
- constant pressure changes;
- fainting;
- increased sweating;
- neurotic disorders - such patients are usually anxious and suspicious, suffer from various phobias, hypochondriacal and obsessive-compulsive neuroses, they often invent non-existent diseases;
- “chilliness” and cold fingers and toes;
- increased sensitivity to cold;
- vegetative crises, better known as panic attacks.
How dangerous is the disease?
Common complications include cardiac problems. Basically, these are fatal abnormalities that cannot be treated in isolation.
- Heart attack. The most likely outcome. Characterized by acute circulatory disorders in muscle formations. Hence the intense clinical picture.
- Caridiogenic shock. A drop in blood pressure combined with a significant decrease in left ventricular output. A deadly complication. Mortality rate is almost 100%. Even lucky patients do not manage to live too long; within a few years, death is inevitable.
- Stroke. Acute malnutrition of the brain. It is dangerous not only in terms of mortality, but also in the likelihood of focal-type deficiency phenomena (speech, vision, hearing suffer first of all).
- Heart failure.
- Vascular dementia. It occurs relatively rarely against the background of the pathology under consideration.
Mitral valve prolapse is dangerous due to hemodynamic disturbances and threatens generalized hypoxia of all tissues and organs. Long-term course is associated with multiple failures.
Mitral heart valve prolapse
The most widespread in the modern world is mitral prolapse of the central heart valve. Most often, such prolapse is congenital in nature, so it occurs unnoticed by its owner. However, in some cases the patient may be concerned about:
- Interruptions in the functioning of the heart. This symptom can also occur in the presence of left heart valve prolapse. In this case, this means the appearance of a rapid heartbeat, a deviation in the rhythm of heart contraction, and so on.
- Pain in the heart and chest area. It is worth noting that pain sensations can differ from each other - be stabbing, cutting or aching.
- Symptoms of VSD, that is, vegetative-vascular dystonia. This includes headaches, stomach pain, shortness of breath, and the like.
- Fainting and loss of consciousness, which is especially typical for heart disease with mitral valve prolapse. Most often, such manifestations occur in stressful situations or when staying in stuffy conditions.
- Panic attacks, when a person is overwhelmed by fear.
Diagnostics
Examination of patients with suspected abnormalities in the functioning of cardiac structures is the task of a cardiologist or specialized surgeon.
The duration of diagnosis ranges from several days to a week, possibly more, depending on the main factor in the development of the process.
An approximate diagram is as follows:
- Interviewing the patient for complaints, as well as collecting anamnestic data. A crucial point that forms the basis of diagnosis, despite its apparent insignificance.
- Auscultation (listening to heart sounds). They are loud, their splitting is observed. In some cases chaotic. Systolic clicks are detected, caused by a sharp tension of the chords, which were previously relaxed - a direct indication of regurgitation.
- Measurement of blood and pulse pressure (the latter is calculated as the difference between the upper and lower levels). Also heart rate. As a matter of priority.
- Daily monitoring using the Holter method. Using an automatic programmable tonometer. Allows you to evaluate the functional activity of a muscle organ in dynamics, in conditions familiar to a person. Inpatient examinations of this kind are less effective.
- Electrocardiography. The main method. It is not aimed at identifying violations of the contractility of the myocardium and other structures. Load tests are carried out, but with great caution. Because complications are likely.
- Echocardiography. Or ultrasound. Visualization is shown in a short time, which makes the technique widespread and accessible to a wide range of patients. Used to diagnose organic abnormalities. As a rule, in this way either the consequences of mitral valve prolapse or the origin of the process are identified.
- Angiography of the coronary arteries. Blood flow normally should not lag behind.
- MRI or CT. In extreme cases.
If indicated, a consultation with an otolaryngologist or a nervous system specialist may be prescribed. As part of the advanced diagnostics, a general, hormonal, and biochemical blood test is performed.
Anatomy of the mitral valve
The mitral apparatus consists of the left atrium wall, annulus, leaflets, chordae tendons, papillary muscles and the wall of the left ventricle. The valve is located obliquely behind the aortic valve.
Left atrial wall
The left atrial myocardium extends to the proximal part of the posterior leaflet. Thus, enlargement of the left atrium can lead to mitral regurgitation as the mitral annulus is stretched. In this case, the anterior leaflet is not disturbed due to its attachment to the base of the aorta.
Mitral ring
It is a fibrous formation that connects to the valves. This hole is not solid, but D-shaped, the same shape that prosthetic valves are made of.
The normal diameter of the mitral annulus is 2.7 to 3.5 cm, and the circumference is between 8 and 9 cm
The border of the mitral annulus is posterior to the aortic valve, which is located between the ventricular septum and the mitral valve. The ring functions as a sphincter that compresses and reduces the surface area of the valve during systole, allowing complete closure of the leaflets. Thus, dilatation (widening) of the mitral annulus causes poor closure of the leaflets, which leads to mitral regurgitation.
Doors
The free edges of the valves have several recesses. Two of them, anterolateral and posteromedial, divide the valves into anterior and posterior. These commissures can be accurately identified by the insertions of commissural chordae tendons into the valves
Normally, the valves are thin, flexible, translucent and soft. Each leaflet has an atrial and ventricular surface.
- Front flap
It is located behind the root of the aorta and is attached to it, unlike the posterior leaflet. Accordingly, this leaflet is also known as the aortic, septal, large or anteromedial. The anterior valve is large and semicircular in shape. It has a free edge with or without small indentations. The two zones on the anterior valve are called coarse and transparent, according to the passing chordate tendons. These two zones are separated by a ridge on the atrial surface of the leaflet, which is the line of its closure. The ridge is located approximately 1 cm from the free edge of the anterior valve. Distal to the ridge is a rough area shaped like a crescent.
- Rear flap
Also known as the ventricular, lesser or anal leaflet. It is a section of the mitral valve that is located behind the two commissural areas. It has a wider area of attachment to the annular space than the anterior leaf. Divided into 3 scallops and 2 recesses or slits. The middle crest is larger than the other two (anterolateral and posterolateral commissural).
Chords
The cup tendons are small fibrous strings that arise either from the papillary muscles or directly from the wall of the ventricle, and are inserted into the valve leaflets or muscle. There are 2 types of chords, called true and false.
The normal average chord length is about 20 mm. The normal average thickness of the chordae is 1-2 mm.
- Commissural chords
They are called so because they are attached to the commissural areas located at the junction of the anterior and posterior leaflets. There are two types of commissural chordae. The postmedial commissural chords are inserted into the posteromedial area of the commissure; whereas the anterolateral commissural chordae insert into the anterolateral commissural region. Most of the main branches of the commissar chords are directed towards the center of the commissural areas.
- Valve chords
Attached to the front or rear doors. Two types of chordate tendons are attached to the anterior valve. The first are the rough chords, which are inserted into the distal part of the anterior valve, called the rough zone. The second are the chords, which are located in front of the insertion into the anterior valve.
The posterior valve has 3 types of chordal fibers. The first are the rough chords, which are the same as the rough chords of the anterior valve. The second are the basal chords, specific to the posterior valve.
Papillary muscles and the wall of the left ventricle
These two structures represent the muscular elements of the mitral valve. The papillary muscles usually extend from the apex and middle third of the wall of the left ventricle. The anterolateral papillary muscle is usually larger than the posteromedial papillary muscle and is supplied by the left anterior descending artery or the left peripheral artery. Pathological fusion of the papillary muscles can lead to mitral stenosis. On the other hand, rupture of the papillary muscle, usually a complication of acute myocardial infarction, leads to acute mitral regurgitation.
Video: Mitral Valve - Anatomy, Function & Area - Human Anatomy | Kenhub
Treatment
Mixed therapy. Depends on the stage.
Stage 1. For mild MVP, dynamic monitoring was provided. Doctors will not undertake to prescribe surgery until the condition worsens. Spontaneous regression or stagnation, stabilization of deviations at a certain level, is possible. In such a situation, supervision is not needed at all.
Effective lifestyle changes:
- Quitting smoking, alcohol, and bad habits in general.
- Normalization of diet. There are no specific recommendations for a universal plan; everything is possible, but in moderation. The menu is based on vegetables, fruits, cereals, dairy products and protein in various forms.
- Sleep 8 hours per night.
- Minimum stress.
Stage 2. Requires medication and, again, dynamic observation. Minimal signs of progression are the basis for surgical treatment.
Among the drugs:
- Antihypertensive drugs. Diverse in character. Prescribed by a doctor.
- Cardiac glycosides, but with caution. A heart attack or a stop in the functioning of a muscle organ is possible.
- Antiarrhythmic. Amiodarone, Hindin and others.
- Mineral complexes, preparations for replenishing potassium and magnesium.
Stage 3. Requires planned surgical treatment. Mitral valve replacement is used. This is the main technique in the advanced phase of the pathological process.
Before the intervention begins, it is recommended to normalize the patient’s condition; this can be done with the same medications. Monitoring of the situation is constant, every 1-2 months ECG, ECHO and objective routine assessment.
Stage 4. Has no prospects for cure. The care is palliative, the only chance of recovery is a heart transplant, but there are few donors, so the probability is almost zero.
Each phase requires its own approach. The later and more neglected, the more difficult it is; doctors are forced to show greater ingenuity.
Disruption
The cardiovascular system has a complex structure. It includes the heart with 4 chambers, blood vessels and valves. There are 4 main valves. One of them is aortic. It is located at the mouth of the aorta. It is the largest blood vessel in the human body.
The aorta begins the systemic circulation, which supplies blood to all organs except the lungs. The valves are formed from the inner layer of the heart and ensure the movement of arterial blood in one direction: from the ventricles to the aorta and smaller arteries. The aortic valve has 3 leaflets. After ventricular systole, blood rushes into the lumen of the aorta, and the valve leaflets close. This prevents blood regurgitation. Aortic insufficiency is a heart defect in which during diastole (relaxation) of the left ventricle, part of the blood from the aorta returns back.
In most cases, this pathology is combined with defects of other valves and narrowing of the aortic mouth. Men suffer from this disease 3-4 times more often than women. Aortic insufficiency occupies 4% of the overall structure of heart defects. The disease does not appear immediately and can last for years. If left untreated, this heart defect progresses. Conservative therapy is effective only for minor disturbances in blood flow.
Forecast
The likely outcome can be determined after long-term observation. Much depends on the rate of progression and the stage of the pathological process. If we speak in numbers, then very roughly we can imagine the following calculation:
- Stage 1. Survival rate is 95%, even without treatment. But the probability of progression is 98%; with therapy or behavior changes, the phenomenon can be slowed down.
- Stage 2. 70%, mortality is minimal, but no longer zero.
- Stage 3. The chances of staying in this world are determined to be 30%; with therapy, it is slightly higher. The numbers change dramatically with successful surgery.
- Stage 4. The terminal stage has no cure at all. Mortality rate is 98%, the remaining 2% occurs in the next 6-8 months. Transplantation solves the problem only partially; multiple organ failure is observed. Therefore, there is almost no hope.
Early treatment, young age, good response to the use of drugs, a minimum of somatic pathologies, absence of bad habits, genetic predispositions, non-physical nature of the work. These are favorable prognostic factors.
How is blood flow disrupted?
The pattern of blood flow disturbances in aortic insufficiency is quite complex. Incomplete closure of the valve flaps leads to the following disorders:
- reverse flow of arterial blood from the aorta into the left ventricle;
- its overflow and stretching;
- expansion of the ventricular cavity;
- increasing the force of its contraction;
- increase in systolic output.
The load on the left ventricle increases. Even during diastole (relaxation) it is filled with blood. Normally, during relaxation, the volume of blood in it is no more than 130 ml, and during regurgitation of blood it reaches 400 ml or more. Prolonged work of the heart in such a rhythm leads to hypertrophy (increase in ventricular volume).
Over time, a mitral valve forms. Its development is associated with dilation of the left ventricle and impaired muscle function. During the compensation stage, the work of the left atrium does not change. In the later stages, diastolic pressure increases in this part of the heart. This is how hypertrophy of the left atrium develops.
Aortic disease often causes blood stagnation in the small circle. The consequence of this is an increase in blood pressure in the pulmonary artery and damage to the right ventricle. This is how right ventricular failure develops.
Signs
Symptoms of first-degree mitral prolapse are usually less severe, and in some situations may be completely absent. Most often, this condition manifests itself as pain in the left half of the chest, not associated with myocardial ischemia.
It can last for several minutes, or it can persist throughout the day. There is no connection with physical activity, but sometimes the pain syndrome is provoked by emotional experiences.
Other manifestations are:
- feeling of lack of air and inability to breathe deeply;
- heart rhythm disturbances (rapid or slow heartbeat, interruptions and extrasystole);
- frequent headaches accompanied by dizziness;
- loss of consciousness for no apparent reason;
- a slight increase in systemic temperature in the absence of infectious diseases.
Since MVP is quite often combined with vegetative-vascular dystonia, its symptoms may also occur.
Congenital prolapse
Congenital MVP begins to form in utero and, after the birth of a child, this pathology is combined with manifestations of vegetative-vascular dystonia. In most cases, heart disease does not manifest itself in any way, and all symptoms are caused precisely by disorders in the functioning of the nervous system.
Symptoms
Such children often experience episodic pain in the heart and chest. They can be caused by a disturbance in the functioning of the nervous system, and appear after stressful situations or emotional overstrain. The pain is tingling or aching in nature and is not accompanied by dizziness, shortness of breath or loss of consciousness. Sometimes they last a few seconds or minutes, but they can last several hours or even days.
A child with vegetative-vascular dystonia may experience sensations of “fading heart”, palpitations and headaches. These symptoms are not associated with cardiac dysfunction due to a defect in the mitral valve and have one characteristic feature: they appear and disappear suddenly and are never combined with dizziness or loss of consciousness.
Episodes of fainting with congenital MVP are extremely rare, and they are also caused by vegetative-vascular dystonia. Such fainting occurs in stuffy rooms or is associated with negative and strong emotions (sharp fright, fear). They are easily eliminated by patting the face and providing access to fresh air.
People with congenital MVP often have the following characteristic features in their physique:
- long and thin limbs;
- above average height;
- elongated face;
- skin hyperextensibility;
- joint hypermobility, etc.
Congenital prolapse can be combined with other pathologies that are caused by a defect in the connective tissue: myopia, accommodation disorders, flat feet, strabismus, etc.
Diagnosis and classification
The most effective diagnostic technique for congenital MVP is echocardiography. It allows you to determine not only the degree of protrusion of the valve leaflets, but also to calculate the volume of blood regurgitation.
The degree of prolapse is determined by the size of the mitral valve protrusion:
- 1st degree – up to 5 mm;
- 2nd degree – up to 9 mm;
- Grade 3 – 10 mm or more.
If necessary, other diagnostic methods may be prescribed:
- ECG;
- Holter ECG;
- chest x-ray;
- clinical blood and urine tests;
- blood biochemistry.
Treatment
In most cases, congenital MVP does not require cardiac treatment. Such patients need to undergo control echocardiography 1-2 times a year and be observed by a cardiologist. Children with this structural feature of the heart are recommended to play outdoor games, swimming, and engage in physical education or light sports. The decision to engage in serious physical activity or sports that require serious stress is made individually.
In case of severe anxiety, headaches, palpitations and other signs of vegetative-vascular dystonia, observation by a neurologist is recommended, who may recommend taking medications to normalize the functioning of the nervous system. In most cases, all these symptoms can be smoothed out by taking herbal sedatives (Persen, Novo-passit, valerian preparations, etc.). In addition to such drugs, medications or dietary supplements with magnesium may be prescribed (Magnerot, Doppelgerts active magnesium + B vitamins, Magnesium B6).
If significant blood regurgitation is detected, which is accompanied by shortness of breath, severe weakness, headaches and increased pain in the heart during physical exertion, the cardiologist may prescribe a set of medications to normalize the functioning of the heart. The need for such therapy will be determined strictly individually.
Diagnostics of MVP
A doctor can suggest a violation in the valve system during a routine examination or based on the patient’s complaints. At the appointment, during auscultation, the therapist hears so-called noises. They occur when blood flows back into the ventricle.
In some cases, noises are not a sign of pathology, but require additional examinations.
The doctor will prescribe:
- Cardiac ultrasound is a simple and non-invasive procedure. Allows you to determine the degree of valve sagging and regurgitation. With significant tissue dysplasia, a defect or damage to the right heart valve may develop.
- X-ray – to determine the linear dimensions of the heart.
- ECG and daily monitoring of cardiac activity - to determine persistent changes in the rhythm of contractions.
- Bicycle ergometry - for prolapse of II and III degrees to identify the response to increased physical activity.
Ultrasound of the heart helps to identify the degree of MVP.
When making a diagnosis, consultations with a neurologist and rheumatologist are indicated. During the examination, heart defects, inflammatory diseases of the endocardium and pericardium, and pathologies of a bacterial nature should be excluded.
Treatment of prolapse
If objective symptoms - changes in heart rhythm, shortness of breath, pain - do not bother the patient, then drug or surgical treatment is not indicated.
Drugs
If there are pronounced signs of prolapse at the initial stage of therapy, the doctor will prescribe drugs from the following groups:
- Sedatives – valerian root extract, Fitosed, Persen, Novo-passit.
- Cardiotrophics - Riboxin or potassium and magnesium aspartate - have an antiarrhythmic effect and contribute to the saturation of heart tissue with oxygen. Vitamin complexes are indicated.
- Beta blockers are drugs that block adrenergic receptors. This reduces the frequency and strength of heart contractions during arrhythmia. In cardiology, Propranolol, Atenolol, Tenolol are used. Dosages are selected individually and may differ from those recommended by the manufacturer. Common side effects include a sharp decrease in heart rate, a decrease in blood pressure, the appearance of paresthesia and a feeling of coldness in the extremities.
Phytosed is a sedative
Prosthetics
Indications for surgical treatment are severe insufficiency of the valve system, with pronounced fibrous tissue changes, and the appearance of areas of calcification. It is considered an operation of desperation and is performed only if drug therapy is impossible or ineffective.
During preparation for surgery, an ECG, X-ray examinations, phonocardiography to assess the intensity of murmurs and heart sounds, and ultrasound of the organ are performed. Preventive antibiotic therapy is indicated.
The purpose of surgery is to replace the mitral valve with an artificial or natural prosthesis. This is a broadband operation with the patient connected to a life support system. This allows hearts to be excluded from the circulatory system during excision and installation of medical equipment.
The surgeon works on a cooled heart. After revision and installation of the valve in the anatomically correct position, air is removed from the heart chambers, tissue is sutured layer by layer and the patient is disconnected from the artificial circulation system.
Important!
The rehabilitation period is long and can range from 2 to 5 years. Patients with an artificial prosthesis take lifelong medications to reduce the risk of thrombosis. The lifespan of such a valve is limited and after some time repeated surgery may be required. The individual characteristics of the heart may not satisfy the throughput of the prosthesis.
Folk remedies
Traditional medicine in the treatment of mitral valve deflection is used only in consultation with a cardiologist. They will not cure the disease, but have a sedative effect, relieve anxiety attacks, and improve the trophism of the heart muscle.
- Mint decoction - buy herbal raw materials in pharmacies, but you can also grow it at your own dacha. For 5 g of dry leaves you will need 300 ml of boiling water. Pour in and leave for 2 hours. For 1 dose you will need 1 glass of the prepared decoction. Take 3 times a day.
- Pour a mixture of hawthorn, motherwort and heather flowers in equal proportions with boiling water at the rate of 1 teaspoon of dry raw materials per 250 ml. Take one glass of decoction in small portions throughout the day.
- St. John's wort decoction - classic proportions - for 5 g of plant material, 250 ml of boiling water. Take 100 ml 3 times a day 30 minutes before meals.
- Motherwort herb – calms, normalizes cardiac activity. For 4 teaspoons of raw materials you will need 1 glass of boiling water. Simmer in a water bath for 15 minutes. Take 100 ml 3 times a day before meals.
Motherwort decoction normalizes cardiac activity
Physical exercise
A sagging mitral valve is not a contraindication to physical activity. Moderate sports and active games, on the contrary, improve the condition of the child and adult.
A patient with stages I and II can play sports without restrictions in the absence of the following situations:
- episodes of arrhythmia, loss of consciousness due to changes in the rhythm of cardiac activity;
- the presence of episodes of tachycardia, flutter, and other changes during a stress test or daily ECG monitoring;
- mitral insufficiency with backflow of blood;
- history of thromboembolism;
- death of a relative with a similar diagnosis during physical activity.
Allowed to play sports with I and II degrees of MVP
With grade 3 prolapse, sports, except exercise therapy under the guidance of an instructor, are prohibited until surgical correction of the condition.
Valve prolapse is not a contraindication to pregnancy and natural childbirth. But you should inform your gynecologist about your condition.
Diet
There is no specialized diet for patients with sagging heart valves.
Doctors recommend introducing magnesium-rich foods into your diet:
- legumes;
- oatmeal;
- almond.
Oatmeal is rich in magnesium
It is mandatory to take vitamin complexes prescribed by a cardiologist.
For adult patients, it is recommended to exclude alcoholic beverages and tobacco.
Symptoms of pathology
Manifestations of the defect are divided into pulmonary, cardiac and general.
General symptoms:
- Decreased performance.
- Insomnia.
- Weakness.
- Forced sitting position.
- Pale skin combined with cyanosis.
Pulmonary symptoms:
- Dyspnea.
- Difficulty noisy exhalation.
- Cough for no apparent reason.
- Tendency to respiratory diseases.
- In later stages - hemoptysis.
Heart symptoms:
- Frequent heartbeat.
- Cardialgia.
- Reduced blood pressure.
- Atrial fibrillation.
- Ascending edema of the lower extremities.
Features of the skin
The first manifestation of the defect is pale skin . As hypoxia progresses, acrocyanosis develops - blue discoloration of the lips, earlobes, and fingertips. In the stage of decompensation, cyanosis becomes widespread, and bluish discoloration of the mucous membranes occurs.
A specific symptom is characteristic - “mitral face” - pronounced pallor of the face combined with a crimson blush on the cheeks and cyanosis of the lips. Despite the presence of these symptoms, a diagnosis is not made based on skin changes.
Causes of hemoptysis
The appearance of blood streaks in the sputum is due to cardiogenic pulmonary edema.
Developing pulmonary hypertension underlies spasm of microvasculature vessels - capillaries, arterioles and venules.
Microvascular spasm further aggravates hypertension , resulting in damage to the vascular walls. Through damaged vessels, blood begins to flow into the lung tissue. During the process of self-cleansing of the lungs, blood mixes with mucus and is coughed up by the patient (hemoptysis).
Heart rhythm disturbance
The disease is characterized by early onset of arrhythmia. Rhythm disturbances are caused by hypertrophy of the venous ventricle and left atrium , as a result of which the heart chambers cannot contract simultaneously. The following types of arrhythmias are distinguished:
- Atrial fibrillation.
- Ventricular tachycardia and fibrillation.
- Atrial flutter.
- Atrioventricular blockade.
- Extrasystole.
Pressure gradient
The pressure gradient is the difference in pressure between the left chambers of the heart. Normally, the pressure in the left ventricle is 33-45 mmHg, in the atrium - 3-6 mmHg.
With bicuspid valve stenosis, the pressure initially becomes equal in both chambers . As it progresses, the pressure in the atrium becomes greater than in the ventricle, on the basis of which the following classification of the defect is made:
- Slight stenosis (gradient is 7-11 mmHg).
- Moderate (12-20 mmHg).
- Significant (more than 20 mmHg).
The magnitude of the gradient also reflects the degree of pulmonary hypertension.
Clinical guidelines on mitral valve stenosis from the Ministry of Health of the Russian Federation can be downloaded from this link.
Symptoms of the disease and its treatment
severe fatigue; swelling of the legs and ankles; pain and shortness of breath when walking and lifting heavy objects; dizziness accompanied by fainting.
If such symptoms occur, you should immediately seek advice from a qualified specialist. He will help you understand why the heart valves are not working and develop the required course of treatment.
Initially, patients are prescribed conservative treatment methods. They are aimed at relieving pain, adjusting heart rhythm and preventing possible complications. Similar methods are prescribed after operations of the cardiovascular system; they help prevent relapses.
To determine a more effective treatment method, the doctor must take into account the severity of the disease, the patient’s age and all individual contraindications. Patients are prescribed medications that will increase the intensity of the heart muscle, and its functionality should improve.
General signs of mitral valve (MV) dysfunction are characteristic of many cardiovascular diseases, therefore, to make an accurate diagnosis, it is necessary to identify specific symptoms and conduct diagnostics.
With pathology of the mitral valve of the heart, symptoms may be as follows:
- malaise;
- dyspnea;
- heaviness in the chest;
- specific sound when listening to the heartbeat;
- swelling;
- fast fatiguability;
- pain in the heart area;
- nausea;
- cough, in severe cases - with bloody discharge.
The intensity of the manifestation of these signs depends on the type of disease and the degree of its neglect. Since many diseases are characterized by an asymptomatic course, to prevent the development of irreversible processes it is necessary to undergo an annual examination by a cardiologist, especially after 40 years.
If prolapse is detected during pregnancy?
Usually,
with mitral valve prolapse, they occur without complications, the child is born with normal body weight and at term.
During
a woman with mitral valve prolapse may be recommended echocardiography, which will clarify the volume of blood returning (
), and, accordingly, the degree of mitral valve insufficiency.
Complications of mitral valve prolapse during pregnancy and childbirth are extremely rare, but you should further discuss the risk of developing them during pregnancy.
or a cardiologist.
Changes in the mitral valve are detected during examination of pregnant women. Usually they were present since childhood, but did not bother and did not require any diagnostics.
The expectant mother should be reassured: prolapse does not threaten the baby or the course of pregnancy. It’s another matter if cardiac pathology, rheumatism or serious diseases are simultaneously detected.
In any case, obstetricians take these changes into account when planning labor and in the preventive treatment of a pregnant woman.
People with mitral valve prolapse should understand that the severity of recurrent regurgitation may vary throughout life. Therefore, it is necessary to undergo an annual examination and comply with the doctor’s requirements for preventive treatment of concomitant diseases.
Causes of the disease
The disease most often affects children 7–15 years of age and young people under 40 years of age, and the pathology is diagnosed more often in women. Heart valve defects are found in most cases in people suffering from any heart diseases (rheumatism, congenital defects) that have a genetic predisposition.
Mitral valve prolapse can be idiopathic or secondary. The idiopathic form of the disease occurs with congenital connective tissue dysplasia, structural anomalies of the valve apparatus (cusps, annulus fibrosus, chordae, papillary muscles), electrolyte disturbances, and disproportions of the valve-ventricular system.
Congenital defects develop against the background of a maternal hereditary predisposition, pregnancy complicated by intrauterine infections, or acute respiratory viral infections. Such pathologies include:
- Marfan syndrome;
- Ehlers-Danlos syndrome;
- pseudoxanthoma;
- arachnodactyly.
Secondary valve prolapse can be caused by coronary heart disease, systemic lupus erythematosus, vegetative-vascular dystonia, rheumatism, hyperthyroidism, mechanical trauma to the chest, myocarditis. These diseases cause prolapse, sagging, sagging, bulging and incomplete closure of the valve leaflets.
Prolapse occurs as a result of myxomatous degeneration of valve structures and nerve fibers of the heart. In the affected valves, a high level of type 3 collagen is detected, and diffuse damage to the cells of the fibrous layer is observed. As a result, the density of the valve leaflets decreases, degeneration progresses with age, and can lead to perforation of the valve leaflets and rupture of the chords.
The main reasons for prolapse of the mitral valve walls:
- violation of the proportions of the area, length and thickness of fragments of the valve apparatus;
- connective tissue defects leading to arching and stretching of the valve leaflets;
- disorders of functioning, neuroregulation, and functioning of the endocrine system.
Of no small importance in the appearance of symptoms of mitral valve prolapse are past infectious and viral diseases, vegetative-vascular disorders, damage to the central nervous system, metabolic disruptions, and lack of magnesium in the body.
Clinical picture
With SMC, clinical manifestations begin to worry the patient when the lumen of the fibrous ring narrows to almost twice its exit size. In this case, the sick person develops the following symptoms of the disease:
- dyspnea;
- cardialgia, which intensifies with physical exertion and anxiety;
- cough with hemoptysis;
- swelling of the lower extremities;
- acrocyanosis (blueness of the tip of the nose, lips, ears, etc.);
- the appearance of a “heart hump” - a characteristic protrusion of the anterior chest wall in the area of the projection of the heart;
- frequent attacks of atrial fibrillation;
- chronic bronchitis and pneumonia;
- general weakness, malaise, fatigue and loss of performance;
- the appearance of the symptom of “cat purring” (when, after physical exertion, placing your hand on the heart area, you can feel its rattling);
- On auscultation, a characteristic diastolic murmur and a third sound appear, which is called the “quail rhythm.”
In almost half of patients, mitral valve prolapse is asymptomatic and without harm to health, which indicates very small amounts of blood that leaks back into the atrium. For severe forms of MVP, the following clinical symptoms are characteristic:
- feeling of fear of death and constant anxiety;
- cardiac pain after physical exertion, in stressful situations, etc.;
- shortness of breath, rapid breathing;
- periodic dizziness, lightheadedness;
- increased fatigue;
- hyperthermia without manifestations of infectious diseases;
- sweating;
- tachyarrhythmia;
- During an auscultatory examination, the doctor determines the presence of a pathological systolic murmur in the patient and the appearance of a “quail rhythm” - the third tone.
Mitral valve insufficiency with significant regurgitation is manifested by a characteristic clinical picture:
- cardiac pain of aching and squeezing nature;
- shortness of breath at rest, which increases with a horizontal position of the body;
- the appearance of a cough with bloody sputum;
- swelling of the lower extremities, heaviness in the abdomen, hepatomegaly, ascites;
- acrocyanosis;
- swelling of veins in the neck;
- the appearance of a characteristic protrusion on the anterior chest wall in the area of the projection of the heart;
- hypertrophy of the left heart;
- attacks of atrial fibrillation;
- periodic trembling of the chest on the left;
- During an auscultatory examination, the patient is diagnosed with a murmur from the closure of the mitral valve, weakness of tones, and systolic murmur.
Symptoms
Symptoms of mitral valve prolapse vary from minimal (in 20-40% of cases none at all) to significant. The severity of symptoms depends on the degree of connective tissue dysplasia of the heart, the presence of autonomic and neuropsychiatric abnormalities.
Markers of connective tissue dysplasia include:
- myopia;
- flat feet;
- asthenic body type;
- high growth;
- reduced nutrition;
- poor muscle development;
- increased extension of small joints;
- poor posture.
Clinically, mitral valve prolapse in children can manifest itself:
- Signs of dysplastic development of connective tissue structures of the ligamentous and musculoskeletal system revealed at an early age (includes hip dysplasia, umbilical and inguinal hernias).
- Predisposition to colds (frequent sore throats, chronic tonsillitis).
In the absence of any subjective symptoms, nonspecific symptoms of neurocirculatory dystonia are detected in 20-60% of patients in 82-100% of cases.