To identify pathologies of the gastrointestinal tract, various examination methods are used.
Ultrasound diagnostics, fibrogastroduodenoscopy, computed tomography, magnetic resonance examination are prescribed strictly according to indications. If for some reason the listed methods cannot be carried out or they turn out to be uninformative, the patient is prescribed fluoroscopy of the stomach with contrast.
This examination is carried out in the X-ray room of a hospital or clinic; it involves a small dose of radiation. The patient must know how the procedure will take place and how to properly prepare for it.
What is a barium stomach x-ray?
Since the stomach is a hollow organ with thin walls, X-rays “transit” through it, giving virtually no image on the screen. Therefore, a contrast study method was invented, which has been successfully used to this day.
The metal barium, or more precisely its salt, barium sulfate, was used as a contrast agent. It has a high ability to absorb X-rays, and when it fills the stomach, its inner surface bordering with barium is contrasted.
Entering the stomach, the barium suspension penetrates the folds of the mucous membrane, ulcerative defects, fills various protrusions of the wall (diverticula), and bends around the polyps and tumors present on the mucous membrane. This creates a picture of the shape and volume of the stomach, and the “geography” of its inner lining. In addition, it is possible to monitor the nature of peristalsis - the contraction and relaxation of the muscles of the gastric wall, when the narrowing and expansion of its lumen occurs.
Barium sulfate is safe, it does not dissolve, is not absorbed, passes unchanged through the entire intestine and is excreted along with its contents.
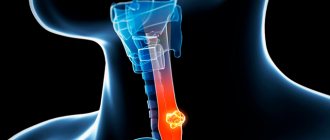
X-ray diagnostics of the esophagus and stomach
This examination allows you to assess the condition and functional capacity of the stomach and esophagus based on studying the image on x-rays. Ingestion of a barium mixture, which tends to accumulate in the mucous membrane of organs, provides their detailed visualization. When a barium solution passes through the gastrointestinal tract, it will be easy for a diagnostician to recognize pathological changes in their shape and structure.
By noting the time of movement of the barium suspension through the digestive tract, the doctor will be able to draw a conclusion about stenosis (narrowing) or obstruction of any part of the system.
Determining the presence of esophageal stenosis by barium passage rate
There are several techniques for performing fluoroscopy of the stomach and esophagus. Depending on the indications and existing symptoms, the diagnostician chooses the most informative one. Research methods are divided into traditional, Trendelenburg examination and double contrast.
As a rule, X-rays of the gastrointestinal tract are done in the morning to relieve the patient from the discomfort associated with prolonged fasting. After carrying out all the necessary measures to clean the organs being examined, the patient drinks a barium solution in the X-ray room and is placed on a functional table.
Traditional fluoroscopy technique
This technique involves the patient lying down on a lowering table. During the diagnostic process, if there is a need for tight filling of the examined organs, additional intake of barium mixture may be required. During the procedure, the patient is asked to change body position, which allows the doctor to obtain information about all parts of the organs being studied - pharynx, esophagus, diaphragm, stomach, etc.
The doctor evaluates the overall picture and takes targeted photographs from different angles. The contours of the shadows are the inner surface of the organ. To ensure that the barium is evenly distributed, the patient is first placed in a horizontal position. The mixture does not stay in the esophagus for long - when you exhale, the esophageal sphincter relaxes and the solution enters the stomach.
It envelops the walls of the stomach, fills the cavities between the folds and makes it possible to visualize them. Better distribution of the solution inside the stomach is facilitated by stroking movements with your hands with slight pressure. They can be performed either by the patient himself or by the medical staff present. This technique lasts approximately 40 minutes. During the examination, the patient may experience attacks of mild nausea, which quickly pass without leading to vomiting.
After the procedure, barium sulfate is released naturally, thereby discoloring the stool. Given the potent astringent effect of barium, the patient may be constipated. Therefore, after diagnosis, to speed up the elimination of barium sulfate, you should drink at least 1.5–2 liters of water, which will ensure that the body quickly gets rid of both the drug and disturbances in peristaltic activity.
If stools have not returned to normal over the course of several days, you should definitely notify your doctor about such disturbances and receive recommendations for solving problems with restoring intestinal function. Do not delay your visit to the doctor under any circumstances to minimize the risk of intestinal obstruction!
Diagnostics using Trendelenburg
The main purpose of this technique is to visualize a diaphragmatic hernia. An important point in this examination is to place the patient on his back with the pelvis elevated at an angle of 45° in the so-called Trendelenburg position, in which images are taken. In this position, the intestinal loops and other gastrointestinal organs are shifted towards the diaphragm and are visualized using a contrast agent, providing the diagnostician with the opportunity to determine the presence of a diaphragmatic hernia. When this defect is present, the organs prolapse into the chest cavity.
A hiatal hernia protruding into the diaphragm is diagnosed using the X-ray contrast method
Diaphragmatic hernia when using the Trendelenburg technique is determined by direct signs:
- change in the X-ray shadow of the heart;
- airiness under the diaphragm;
- darkening of the pulmonary field near the cavity;
- the lumen in the lateral photograph is round in shape;
- change in shadow shape when breathing;
- filling a separate cavity with contrast;
- the presence of gastric folds in the esophagus.
And also by indirect manifestations, characterized by: the absence of gas bubbles in the stomach contents, tortuosity of the esophagus above the diaphragm, displacement of the stomach to the lower third of the esophagus, rotation of the heart along the longitudinal axis, flattening of the vault and a decrease in the volume of the ventricles. This examination method is contraindicated for elderly and senile people with sclerosis and functional disorders of the heart and lungs.
It is also prohibited to carry out it in the presence of blood, pus, exudate and oncological processes in the peritoneum.
Double contrast
The technique involves conducting an examination using two contrasts - barium and gas. To do this, the patient is asked to drink a barium solution through a perforated tube, which allows him to simultaneously swallow air. Massage of the anterior abdominal wall promotes the distribution of the barium mixture, and the air ensures the straightening of tissue folds.
To relax the smooth muscles of the gastrointestinal tract and reduce peristalsis, antispasmodic drugs are administered. This technique allows you to obtain a complete picture of the esophagus and abdominal organs, which helps to identify various pathological processes, including oncology in the early stages.
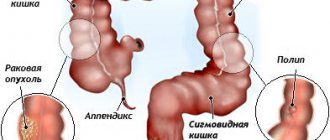
Oncological diseases detected using radiography
Indications and contraindications for the procedure
Indications for x-ray examination of the stomach are:
- chronic gastritis;
- suspicion of an ulcer ;
- suspected stomach tumor ;
- abnormalities in the development of the digestive system;
- diverticula;
- gastric obstruction (retention of contents or accelerated emptying);
- certain symptoms: heartburn, belching, vomiting, epigastric pain, loss of appetite and weight, anemia, periodic appearance of blood in the stool or periodic change in the color of the stool, resembling tar.
There are also contraindications when this study can harm health:
- During pregnancy and breastfeeding.
- Age up to 12 years.
- Acute inflammatory process in the abdominal cavity.
- Acute gastrointestinal bleeding.
- Suspicion of gastric perforation (foreign body, ulcer).
- The presence of an irreducible abdominal hernia (risk of strangulation when the intestines are filled with barium).
If previously these contraindications were relative, and x-rays were still performed for urgent indications, today there is no need for this; it is successfully replaced by FGDS - examination with an endoscopic probe.
How to prepare for an x-ray of the stomach and esophagus
As preparation for fluoroscopy of the stomach, only a specialized diet is used. It is necessary in order to free the gastrointestinal tract from undigested food particles, which can interfere with obtaining clear images or create “interference” in the area of X-ray action. In addition, in preparation for x-rays of the esophagus and stomach, it is necessary to exclude the possibility of gas formation in the digestive tract.
A few days before the procedure, it is important to exclude from the diet foods that take a long time to digest:
- vegetables with a lot of fiber and coarse fibers;
- fatty meats;
- smoked meats and marinades.
In preparation for examining the digestive tract using x-rays, products that promote gas formation are excluded from the menu: legumes, carbonated drinks and sweets, fermented milk drinks, cheese. Also, in preparation for an x-ray of the stomach, it is important to exclude foods that affect peristalsis. First of all, these are spices and alcohol.
On the eve of the study, you need to prepare with an enema or laxatives - the intestines and stomach must be completely empty. Therefore, on the eve of the procedure, stop taking food and water for several hours.
In preparation for the examination, it is important to consult with a radiologist regarding the use of certain medications. In most cases, doctors do not advise taking medications on the eve of the test. If the patient has a stomach ache, the doctor may allow you to take medications prescribed by the gastroenterologist during the preparation for the x-ray examination.
Important! During the period of preparation for x-ray of the gastrointestinal tract, it is not recommended to take antispasmodics, as they can cause short-term changes in peristalsis, as a result of which the diagnosis will not be accurate.
What can you eat before the test?
In order for the X-ray of the stomach to be accurate, it is important when preparing for an X-ray of the stomach and esophagus to give preference to easily digestible food prepared by boiling. You can drink herbal or green tea, coffee drink, cocoa, and compotes without restrictions.
Gastroenterologists recommend eating regularly and in small portions before an x-ray. The food temperature should be between 25 and 60 degrees Celsius.
In order for the preparation for the x-ray examination to go correctly, it is important to stop eating in time before the x-ray. Experts recommend avoiding eating in the evening, that is, 8-12 hours before the examination. The fluid intake should take place 2-3 hours before an x-ray of the esophagus and stomach is taken.
If the described measures are followed, the intestines should be empty by the time of the examination. If gastrointestinal diseases prevent this, patients prepare for x-ray examination through an enema.
When can you eat after the test?
After an x-ray of the esophagus and stomach has been taken, you can start eating immediately after diagnosis. However, it should be taken into account that a suspension of barium salt actively absorbs liquid, which can lead to the formation of fairly dense masses in the gastrointestinal tract. Under certain conditions, they can clog the intestinal lumen. To prevent this from happening, it is important to start eating mostly liquid foods after the x-ray, and to drink as much water as possible in the first hours.
Preparation rules
The only thing that is required of the patient is to come for the study on an empty stomach, including not drinking liquids. It is recommended not to drink alcohol or smoke during the day. The last meal and drink should be no later than 6 hours before the scheduled time of the procedure.
In other words, the stomach must be empty - this is the preparation of the patient for an x-ray of the stomach.
There are often situations when, as a result of diseases, the functioning of the digestive tract is disrupted, which is manifested by belching, vomiting, constipation, and bloating. In such cases, preparing the patient for an X-ray of the stomach includes a preliminary 3-day diet.
Dairy products, legumes, raw vegetables and fruits, carbonated drinks, spicy, fatty and fried foods are excluded.
If necessary, you need to do a cleansing enema and rinse the stomach if there is belching of food on the day of the study.
How to do an X-ray of the gastrointestinal tract
Before starting the diagnosis, the patient must take the following steps:
- Remove all jewelry containing metal, remove clothing and put on a robe.
- Remove dentures, if any, earrings and other items that may be in the X-ray area.
- Drink a certain amount of barium porridge (barium sulfate).
Further diagnosis is carried out as follows:
- The first sip of barium should not be large in volume. It will allow you to mark the affected areas, pronounced narrowing, which can serve as an obstacle to the advancement of the contrast agent.
- The patient must drink, following the doctor's instructions, the entire volume of barium suspension if the patency of the esophagus is satisfactory. A barium tablet or soft mixture is taken if areas of suspected dysphagia and small strictures need to be examined.
- The mechanics of intestinal contraction and relaxation (peristalsis) are studied as the contrast passes through the intestine.
- At the same time, the doctor examines the mucous membrane and determines its condition.
- At this moment, the radiologist watches on the fluoroscope monitor the progress of the barium suspension down the esophagus.
The average time for the initial procedure is about 40 minutes.
The video shows the fluoroscopy procedure from the author Akhat Kazhibaev.
Traditional diagnostics
Traditional diagnostics involve carrying out the procedure in the morning, with:
- food intake is allowed no later than nine hours before the start of the manipulation;
- cleansing enemas are done in the evening and three hours before the start of fluoroscopy.
The step-by-step technique of the procedure looks like this:
- The patient is placed on a special lowering couch in a supine position.
- If tight filling of the gastrointestinal tract is necessary, the patient drinks a contrast agent.
- During the manipulation, the subject changes the position of the body several times. The most informative position is considered to be on the back, with the pelvis located at an angle of 45 degrees.
- Traditional diagnostics allows for a detailed examination of all organs of the gastrointestinal tract, as well as the esophagus, diaphragm, duodenum and pharynx.
Trendelenburg study
Fluoroscopy, which is performed using the Trendelenburg method, is aimed at visualizing a diaphragmatic hernia. With this method, a person, immediately after taking barium, lies in a position, raising the pelvis by 45 degrees. This position allows the intestine to retract into the sternum, while the diaphragm enters the intestine through the lower esophageal opening.
Research is prohibited:
- if you suspect peritoneal and intestinal cancer;
- with dysfunction of the heart and lungs;
- with the accumulation of pus, blood or exudate in the peritoneum.
Double contrast method
The double contrast technique is the only way to detect cancer at an early stage. This fluoroscopy method involves the injection of two contrast agents: barium and gas.
The manipulation is carried out as follows:
- The patient takes the barium sulfate solution while lying down through a special tube. At the same time, the subject swallows air.
- During the administration of the solution, the patient undergoes an indirect massage of the anterior wall of the abdominal cavity. This allows for uniform distribution of the contrast mixture.
- Antispasmodics, administered orally along with the solution, relax smooth muscles, suppress the gag reflex and contractions of the walls of the gastrointestinal tract.
The consequences of this method of fluoroscopy:
- diarrhea or constipation;
- stomach discomfort;
- Digestive problems.
How is the procedure performed?
First, the patient undergoes a survey fluoroscopy of the chest and abdominal cavity to identify gross pathology that could interfere with the study. Then primary contrast is performed. To do this, give 1 glass of barium suspension to drink, the study is carried out in a vertical position, distributing the movement of contrast with pressure from the brush. The shape, size of the stomach, and peristalsis are assessed.
For a more detailed study of the relief of the mucous membrane, the double contrast method is used, when a barium suspension is combined with gas. Sodium citrate, 10 drops of alcohol and antifomsilane are added to the mixture as a gas former. They give you 1/3 cup of the mixture to drink through a special tube with holes, through which gas enters and is swallowed, which enhances the contrast.
The study is carried out in various positions of the patient's body: lying on the back, on the right and left side, with the leg end raised (in the Trendelenburg position). This allows you to move the contrast to different parts of the stomach and conduct a more detailed study of them. If pathology is detected, a photograph of this area is taken. The duration of the procedure is 20-30 minutes.
Features of the procedure in childhood
For children, an X-ray examination of the stomach, due to the high dose of radiation, is performed only for urgent indications, when it cannot be replaced by another method. This happens when there is a suspicion of foreign leaks in the stomach, a suspicion of volvulus and obstruction. Barium suspension is used only in children over 10 years of age; in other cases, a water-soluble contrast agent (gastrografin and analogs) is used.
Since soluble contrasts contain iodine, a skin tolerance test is performed first to ensure that an allergic reaction does not develop.
X-ray as one of the first prescriptions for gastrointestinal pathologies
Because of its excellent diagnostic ability, x-rays have long been recognized as the number one study for suspected pathological processes in the gastrointestinal tract (gastrointestinal tract). Therefore, at the first manifestations, such as:
- pain in the chest or abdomen;
- difficulty swallowing;
- occasional belching or heartburn;
- vomiting for unknown reasons:
- disruption of the digestive process;
- blood particles in the stool (a sign of bleeding), the doctor recommends an X-ray of the esophagus and stomach.
X-ray examination of the stomach and other parts of the gastrointestinal tract is the process of visualizing the organs being studied using X-rays.
This diagnostic method is almost always prescribed in a number of the first tests, because x-rays of the stomach and esophagus show quite a lot of pathological changes, including:
- erosive and ulcerative lesions of the mucous membrane and underlying muscle layers;
- neoplasms of both benign and malignant nature;
- inflammatory processes localized in the duodenum;
- hiatal hernia;
- violation of motor-evacuation function;
- formation of pathological scars on the walls of the stomach and esophagus;
- obstruction of the entire digestive tract.
Thanks to an X-ray examination of the gastrointestinal tract, the doctor is able to detect until a certain time unknown causes leading to a particular pathology, and, if possible, choose the most appropriate therapy. And also evaluate the quality of functioning of the digestive system.
What can a stomach x-ray show?
What can the results of a stomach x-ray with barium or other contrast show? The diagnostic capabilities of the method are very wide; it allows you to identify the following diseases:
- inflammatory process (gastritis);
- the presence of erosions and ulcers;
- tumors;
- diverticula;
- scar changes;
- anomalies of shape and position;
- reduction and increase in volume;
- dysfunction of smooth muscles;
- presence of foreign bodies.
Often, radiography is a precursor method for performing FGDS, for example, when identifying a tumor. To clarify its nature, endoscopy with biopsy and histological examination is necessary.
List of contraindications
Not all patients are prescribed barium X-ray or fluoroscopy of the stomach. Here is a list of conditions in which the examination cannot be performed:
- The patient's serious condition.
- Pregnancy and lactation.
- Suspicion of bleeding in the stomach or intestines.
- Having an allergy to barium.
- Pneumothorax.
- Thyroid diseases.
You should not be afraid of the prescribed procedure - it will not cause you discomfort or pain. The radiation dose is low, however, repeat X-rays of the stomach can be done only after a year. X-ray of the abdominal cavity is an accessible, inexpensive, and very informative examination. However, only a doctor can prescribe it.
Interpretation of examination results
When deciphering the results of an x-ray of the stomach, the doctor writes a conclusion that reflects the norm and pathology. The anatomical position, shape and volume of the stomach, and the evenness of its contours are assessed. They can be changed, the stomach is deformed by scars or adhesions.
There is such an X-ray symptom as a filling defect, that is, when there is a polyp or tumor on the mucous membrane, and in this place barium flows around it, forming a concave contour inward. Another sign is a symptom of a niche, when, on the contrary, barium flows into a defect in the mucous membrane of an ulcer or into an existing diverticulum (protrusion of a section of the wall outward).
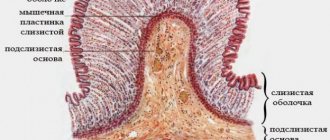
With double contrast, the relief of the mucous membrane is assessed - the nature and depth of the folds, their location. With hypertrophic gastritis, they are rough, thickened, with atrophic gastritis, on the contrary, they are smoothed out. The radial arrangement of folds in the area of ulcers or tumors is also characteristic.
The nature of the dynamics of the stomach and the state of its sphincters are also assessed. For example, in the Trenedelenburg position with the head end down, insufficiency of the sphincter of the cardia and reflux of stomach contents into the esophagus are detected. This is the so-called GERD - gastroesophageal reflux disease.
It is quite common and often causes diseases of the esophagus - Barrett's disease (metaplasia of the gastric epithelium into the esophagus) and cardiac cancer.
How to properly prepare for an examination
Preparation for a barium X-ray of the stomach should be done in advance. If everything is done correctly, you can get high-quality photographs, which is important for further treatment. Doctors recommend being on a special diet for at least two days. You should exclude from your diet foods that contribute to gas formation. You should eat porridge for a while, lean meat, boiled fish and eggs. Prohibited products are:
- Carbonated drinks.
- Cabbage in any form.
- Sweets.
- Milk and any dairy products.
- Buns, bread, pies, cakes.
It is important to note that an X-ray of the stomach with barium is taken on an empty stomach, so a person who is preparing for diagnosis should not eat food either in the evening or on the day of the X-ray itself. It is forbidden to chew gum, smoke or even drink water. According to all rules, the study should be carried out no less than eight hours after the last meal.
There are some cases when patients suffer from a lot of flatulence or severe constipation, in which case doctors recommend that before the study they completely cleanse the body with an enema, and only then will it be possible to perform an X-ray of the intestines with barium.
Before sending a patient for diagnostics, the doctor is obliged to check him for the presence of allergic reactions. Barium sulfate can cause allergies and not all patients are aware that it has a predisposition to allergic reactions. If the allergy is confirmed, then it will be possible to use another contrast substance for the study.
Harmfulness of radiography and adverse effects
X-ray examination of the stomach, especially with taking pictures, is associated with a certain dose of radiation to the body, and therefore has contraindications. However, one-time irradiation, carried out no more than once a year, is considered not dangerous for a healthy adult body.
An unpleasant consequence of the procedure is the accumulation of barium in the intestines and difficulty in emptying it. To prevent this from happening, it is recommended to drink a large amount of liquid immediately after the procedure so that the suspension does not form fecal “stones”; you can also take a saline laxative.
What is the difference between fluoroscopy and radiography?
To understand the subtleties of how fluoroscopy and radiography differ, it is enough to recall the features of these two subtypes of procedures from a scientific point of view:
- Radiography is a method that allows you to obtain a “flat” static image of all organs in the area of exposure to x-rays. Based on the results, an image is obtained that depicts the organs at a certain point in time.
- Fluoroscopy is a method that allows you to obtain visual information in dynamics, obtaining a “volumetric” image of the target organ, which is superior in contrast and resolution to the surrounding tissues.
Comparing these two types, we can conclude that fluoroscopy of the esophagus and stomach is more informative. However, this is not always the case: each method has advantages and disadvantages. For example, radiography produces a larger image that will show even minor changes, while fluoroscopy shows organs on a smaller scale. It is worth noting that the radiation exposure during fluoroscopy is slightly higher, and during radiography the radiation dose is several times lower, since it takes more time to trace the dynamic image.
Important! In terms of the methodology, both procedures are practically the same, but their results look different.
How is radiography done?
Before the examination, the patient frees the body from clothing and metal objects, and then lies down on a special table. First, he undergoes a regular X-ray of the esophagus and stomach, which allows him to see the gross pathologies of the organs being examined, and then an X-ray with contrast is performed. To do this, the patient is given about 150 ml of a contrast solution, which he drinks at one time.
Immediately after this, the doctor takes a series of photographs in different projections: lying on the back and side, as well as standing in the front and lateral projections. On average, x-rays of the esophagus and gastric pouch take about 5-10 minutes. The result is static images of the organ.
How is fluoroscopy done?
In terms of the sequence of actions, the technique for performing fluoroscopy of the stomach and esophageal tube is practically no different from radiography. The patient also frees the body from clothing and metal objects, after which he lies down on a special table or couch. When performing fluoroscopy of the stomach with barium, the patient first drinks a solution of the drug.
The main difference is that the procedure is performed using a trochoscope. This equipment allows you to obtain a digitized image of internal organs that are in dynamics. On it, the doctor can examine functional deviations in real time. For example, during fluoroscopy of the esophagus, the process of filling the tube with contrast, its penetration into the stomach, and the return of the solution during reflux are visible.
As in the previous case, fluoroscopy is performed in several positions so that the doctor can visualize the abnormalities from several viewing points. This is the so-called polypositional fluoroscopy, in which the patient is first in a supine position, then on his side, after which a series of images is taken in a standing position.
This study lasts about 25-40 minutes. To reduce the radiation dose to the patient’s body, digital fluoroscopy is used.
Research price
The price of an X-ray examination of the stomach in Moscow varies from 1 to 5 thousand rubles, it depends on the level of the clinic, its location in the city, and the quality of the equipment used. The Moscow search engine service will help you choose a clinic where you can undergo an examination inexpensively; just enter the name of the study and select the desired region of the city. You can pre-register for the procedure at a convenient time.
There are clinics that do the test for free; it is also included in the compulsory medical insurance services; for this you need to have a doctor’s referral and an insurance policy.
What symptoms are revealed during the examination?
1. Change in the lumen of the organ (increase, decrease);
Narrowing of the lumen of a hollow organ occurs with endophytic (growing inward) or exophytic (growing outward) cancer. In the second case, it may be a tumor of another organ, compressing the stomach, duodenum or esophagus from the outside. On the x-ray we see a local narrowing of the lumen compared to the norm (measured with a ruler). Expansion of the lumen can occur with diverticula, for example: a change in the shape of the organ (deformation). The deformity can be congenital or acquired. The human stomach most often has the shape of a “hook”, but there are other options: “horn”, “snail”, “hourglass” with a constriction in the middle. 2. Violation of the position of the organ relative to others (displacement); Gastroptosis – prolapse of the stomach. In addition, the position of the organ can change due to hernias (diaphragmatic, abdominal wall), or injuries. On an x-ray we see, for example, the stomach projected onto the pelvic organs. 3. Violation of the integrity and structure of the organ wall, defects in organ filling, changes in the folding of the mucosa.
The “niche” symptom is the filling of a damaged area of the organ wall with a contrast agent. The symptom most often occurs with peptic ulcer disease. On the x-ray we can see intense darkening at the site of the defect in the organ wall.
Filling defect - a dark area in the image reflects the area where the contrast could not penetrate. It might be a tumor. Also, filling defects are characteristic of polyps and other neoplasms, radiolucent foreign bodies. The image shows a clear brightening against the background of darkening due to contrast. Thinning of the folds of the mucous membrane can occur with chronic atrophic gastritis - it is almost impossible to see them on an x-ray. Radial convergence of the folds of the mucous membrane towards the niche is a symptom of peptic ulcer disease. “Niche” is a darkening that protrudes into the wall of the organ.
Normal radiograph of the contrast-enhanced stomach
An X-ray of the stomach and duodenum with contrast in a standing position reveals: the stomach is hook-shaped, its size is not enlarged, the contrast agent is evenly distributed throughout its cavity, no kinks, filling defects, or thinning of the mucosa are observed. X-ray of a stomach ulcer
In the area of the greater curvature (the anatomical term is the part of the stomach, its convexity directed towards the spleen), a “niche” is clearly visible, from which the folds of the mucous membrane diverge radially. Ulcer of the greater curvature of the stomach. X-ray of gastric polyposis
On the x-ray we see a large number of filling defects (dark in color), round in shape, with clear and even contours. There are no signs of destruction of the mucous membrane. Multiple polyps. X-ray for stomach cancer
The lumen of the antrum (exit - closest to the duodenum) part of the stomach is significantly narrowed (funnel-shaped, circular - in a circle). The contours in the area of narrowing are unclear, torn, and there are significant filling defects. Cancer of the antrum of the stomach.
Reviews
Experts consider the method to be quite informative and relatively safe, fast, well tolerated by patients, and use it in combination with gastroscopy. These methods complement each other, and this “tandem” allows us to establish the most accurate diagnosis.
Judging by patient reviews, the procedure does not cause any inconvenience or pain. Many patients with chronic gastritis and ulcers prefer X-ray examination to the endoscopic method, which to a certain extent causes discomfort.
What is barium for x-rays?
It is common practice to use barium for X-rays of the stomach and esophageal tube, since hollow organs are not visualized well enough. This is a contrast agent consisting of a suspension of barium sulfate salts in drinking water. Externally, the solution looks like a milky-white liquid with a neutral chalky taste. When examining the stomach and esophagus with barium, specialists are able to examine in detail the internal outlines of the organs.
Important! When examining the stomach with barium, the drug is not absorbed, so the method is considered absolutely safe in terms of systemic effects on the body.
X-rays with contrast, in addition to better visualization of the internal contours and structure of the mucous membrane, make it possible to evaluate the peristalsis of organs and other aspects of their functioning. To conduct an informative study of the stomach, contrast is drunk immediately before taking a series of images.
Although barium is considered a safe compound by radiologists, patients may experience allergic reactions to barium sulfates. If this happens once, in subsequent studies a different contrast is used, most often iodine compounds.
Contraindications
There are no absolute contraindications for radiography. However, in some cases the procedure is undesirable for diagnosis.
- If the patient is in serious condition, conducting an examination may worsen the situation.
- Pregnancy. Especially the first trimester (weeks 1-12). To perform fluoroscopy during pregnancy, permission from a gynecologist is required. X-ray beams can be dangerous to the fetus.
- Allergic reactions to substances used for contrast have been detected.
- The presence of pus, fluid, or severe gastric bleeding may be contraindications for examination.
A repeat procedure is prescribed by the attending physician if necessary.
Research methods
There are several ways to study how to take an x-ray of the stomach.
- First way. On the day of the examination, an x-ray of the stomach is first taken. In this case, the use of contrast is not required. Involves taking a single-component image. Using this technique, it is possible to detect pustular formations, intestinal obstruction, and the presence of foreign objects in organs.
- Second way. Next, a fluoroscopy of the stomach with barium is performed. The patient is asked to take a contrast agent. Its taste is reminiscent of chalk, but it has a thick consistency.
Why is it necessary to perform the second examination method? The thing is that the stomach is a hollow organ. That’s why it has the ability to block X-rays. For the result to be correct, the contrast is taken in two stages:
The first dose involves taking a small sip. At this moment, the doctor evaluates the swallowing process, the passage of liquid through the esophagus. After this, the solution completely envelops the gastric walls. Then the doctor takes several pictures and captures the relief of the folds on the organ.
The second stage involves taking the remaining solution. This is approximately 100-150 milliliters. At this point, thanks to the passage of barium through the organ, the doctor can see the shape, location and size of the stomach. Tone and peristalsis are also assessed.
Pictures are taken in several projections, so the patient has to change position. One of these is the Trendelenburg pose. The medical table is tilted so that the patient's pelvis is higher than the head. This helps identify a hiatal hernia.
Alternative methods for diagnosing diseases of the upper gastrointestinal tract
FGDS procedure
Endoscopic examination (EGD) is the main way to detect gastric pathology. Preparation for it is similar to that before contrast radiography. FGDS allows you to examine the gastric mucosa, if any formations are detected, take material for a biopsy and even perform therapeutic manipulations (stopping bleeding from an erosion or ulcer). The study does not involve radiation, is performed quickly, and allows you to see the pathology with your own eyes.
However, like X-rays, FGDS does not allow us to examine the wall of the stomach: its thickness, structure, and the presence of tumors. The procedure is assessed by patients as unpleasant. It is extremely difficult for young children to perform FGDS. In addition, endoscopic examination cannot assess the shape of the organ, its location and functionality.
CT scan
CT is more informative than X-ray of the stomach with barium. The study allows you to see not only the cavity of the stomach, but also its walls, as well as adjacent formations: neighboring organs, lymph nodes. The latter is important for determining the extent of spread of the malignant tumor. However, like X-rays, CT involves irradiating the patient and does not allow examining intragastric pathology in as much detail as FGDS.
X-ray of the stomach in the Trendelenburg position
Contrast-enhanced X-rays of the stomach and esophagus can detect diseases such as hiatal hernia, ulcers or cancer. To increase the information content of an X-ray examination of the gastrointestinal tract, a polypositional study is used in the vertical, horizontal and lateral position of the patient.
For the diagnosis of paraesophageal (near the esophagus) hiatal hernia, the Trendelenburg position is important, since it increases intra-abdominal pressure.
X-ray of the stomach and esophagus according to Trendelenburg
An X-ray of the stomach is informative when barium sulfate is introduced into the organ cavity. For these purposes, the patient is given a glass of a solution of the substance to drink a few minutes before fluoroscopy (candling). Then, under the control of an X-ray television screen, the doctor observes the movement of barium through the esophagus, stomach and duodenum.
At the initial stages of examination, if a diaphragmatic hernia is suspected, the patient's Trendelenburg position becomes of great importance. It involves lifting the patient's pelvis at an angle of 35-45 degrees relative to the head. In this position, when the intestine prolapses into the chest cavity, the contrast is thrown into the intestine through the esophageal opening of the diaphragm and clearly outlines its contours.
The Trendelenburg position came to radiology from surgery, where it was used for convenient access to the colon during hernia operations. When using this position, the intestinal loops and omentum are shifted upward, which opens up rapid access to the pelvis.
Contraindications to Trendelenburg x-ray of the esophagus
X-ray of the esophagus in the Trendelenburg position cannot be performed if:
- pus, fluid, and blood in the abdominal cavity;
- tumors of the abdominal cavity and intestines.
Direct contrast radiographs of the esophagus
The Trendelenburg position negatively affects the functioning of the heart and lungs. With a prolonged stay with the pelvis raised, there is an increase in blood pressure, a change in the respiratory rate and pulse due to the pressure of the intestines on the chest cavity.
Photo of the radiograph: suspicion of a hernia of the paraesophageal part of the diaphragm in the left supradiaphragmatic region
In elderly patients (after 50 years), radiography of the esophagus is performed if a diaphragmatic hernial protrusion is suspected. With age, against the background of degenerative-dystrophic and involutional processes, the muscular system becomes weaker, so the likelihood of prolapse of the large intestine into the chest cavity increases.
Contrast radiography of the small intestine is performed as follows:
- The patient is placed under the X-ray television screen.
- He is given a sip of barium sulfate to drink from a glass.
- The progress of contrast is monitored by transillumination.
- As the barium approaches the cardiac opening of the diaphragm, the patient is asked to inhale and hold his breath.
- The doctor takes a picture of the esophagus.
- The person is then asked to turn sideways and the procedure is repeated.
- Next, they begin an X-ray examination of the stomach.
If colon prolapse is suspected through the esophageal diaphragmatic hiatus, the patient is placed in the Trendelenburg position. The method allows you to estimate the length of the esophagus, examine its peristalsis, and study the condition of the cardiac and pharyngoesophageal sphincter.
X-ray symptoms of hiatal hernia
X-rays of the stomach and esophagus show hiatal hernia based on the following symptoms:
- displacement of the heart shadow;
- increased airiness under the diaphragm dome;
- decreased transparency of the pulmonary field near the cavity formation;
- rounded clearing with constrictions (due to intestinal folds) on the lateral image;
- when swallowing barium in the patient's Trendelenburg position, the cavity is filled with contrast;
- the shape of the darkening changes with breathing;
- the presence of stomach folds in the area of the esophageal part of the diaphragm.
Indirect signs of a diaphragmatic hernia on an x-ray:
- No gas bubble in the stomach.
- The tortuous course of the esophagus in the supradiaphragmatic part.
- Movement of the stomach into the distal esophagus.
- Rotation of the heart along the longitudinal axis.
- Reduction in the size of the stomach and flattening of its arch.
In conclusion, I would like to note that radiography of the esophagus and stomach can be performed only in the absence of contraindications. Barium sulfate is a water-insoluble substance, so it does not dissolve when it enters the abdominal cavity.
Photo of an X-ray of the stomach: confirmation of a diaphragmatic hernia after contrast
Contraindications to X-ray of the small intestine:
- a through hole in the intestinal wall (perforation);
- purulent inflammation;
- foreign body in the lumen of the organ;
- allergy to barium;
- pregnancy.
An X-ray of the stomach in the Trendelenburg position should be performed not only if a diaphragmatic hernia is suspected. The pose allows you to clearly monitor the state of the gastroesophageal junction. It is used for all types of contrast radiography of the esophagus and stomach.
x-raydoctor.ru
Indications for the procedure
X-rays of the stomach are prescribed to patients for various purposes, which include:
- Making, confirming or refuting a diagnosis.
- Determining the causes of some symptoms.
- Evaluation of the results of surgical intervention.
Important! It should be noted that there are fundamental differences between the procedures of radiography and fluoroscopy of the stomach. The first method involves a snapshot of an organ, and fluoroscopy allows the doctor to study the dynamics of certain processes, observing them in real time. In the second case, several consecutive photographs are taken at once.
Symptoms that may lead to the appointment of an x-ray of the stomach are:
- painful sensations in the abdominal area of unknown origin;
- detection of obvious or hidden blood in feces;
- difficulty swallowing, impaired movement of food through the esophagus;
- loss of appetite, weight loss, sudden anemia;
- detection of compactions of unknown nature during palpation of the organ;
In addition, radiography and fluoroscopy methods are used to make, confirm or refute diagnoses of various diseases, defects and unhealthy conditions of the gastrointestinal tract. For example, radiography is most effective if the presence of foreign bodies in an organ is suspected.
After operations on the gastrointestinal tract, a fluoroscopy procedure is often prescribed to evaluate the results of the manipulations and ensure the normalization of internal processes.
Preparing the patient for a barium contrast x-ray
X-rays using contrast allow you to more accurately assess the size, shape, and functional state of the gastrointestinal tract, and fluoroscopy also allows you to trace the dynamics of the movement of substances through the esophagus and passages.
The barium mixture solution is a suspension that the patient drinks in small sips according to the instructions of the doctor performing the procedure.
Table 1. Step-by-step preparation for a barium contrast x-ray
The stomach is an important organ that is involved in the digestion process. It mixes and breaks down food. Gastric juice eliminates germs. Poor nutrition, bad habits, and inflammatory processes disrupt the normal functioning of the stomach.
X-ray of the stomach is a method of visual diagnosis in real time of diseases of the organ, using X-rays and a contrast agent. To maintain health, it is important to identify the disease in a timely manner and not allow it to progress.
When is an X-ray examination of the stomach prescribed?
A girl complains to the doctor about epigastric pain
X-rays with contrast allow you to diagnose a wide range of diseases and anomalies of the gastrointestinal tract. It is prescribed when symptoms appear indicating pathology of the upper digestive tract:
- Nausea and vomiting.
- Heartburn.
- Belching.
- Rapid weight loss (suspected cancer).
- Difficulty swallowing, pain when swallowing.
- Pain in the epigastric region.
X-ray of the stomach, therefore, is used when the rate of food evacuation decreases (for example, against the background of pyloric stenosis), the presence of foreign bodies, suspected oncopathology, peptic ulcer, hiatal hernia, inflammatory processes (gastritis).
The study is not safe for every patient. Contraindications to fluoroscopy and radiography of the stomach are:
- Pregnancy. The study can only be carried out for health reasons!
X-ray examination of the gastrointestinal tract is contraindicated for pregnant women.
- The patient's serious condition. The diagnostic procedure takes a long time and requires a change in body position, which can be difficult for weakened patients or patients who have suffered trauma.
- Contrast should not be used for some acute surgical conditions. Suspicion of ongoing gastric bleeding or perforation of an ulcer is a contraindication to swallowing barium. In case of perforation, only a plain film without contrast can be taken to detect gas in the abdominal cavity. In the picture it will be visible as a crescent-shaped area of clearing under the right dome of the diaphragm.
Childhood is not a contraindication. However, it should be remembered that preparation for the study of such patients, the recommended volume of contrast agent, and the position in which the images are taken have their own characteristics.
The radiation dose for X-ray examination of the organs of the upper gastrointestinal tract (in particular, the stomach) is 0.1-0.8 mSv for digital and film radiography, respectively, 3.5 mSv for fluoroscopy.
How to prepare the body for the fluoroscopy procedure
A research method with a contrast medium that absorbs x-rays of varying intensities. From the images obtained, the doctor can evaluate the stomach - its shape, capacity, functionality, etc.
Preparatory measures for a healthy person include 2 tips:
- Do not eat for 4-6 hours before the procedure.
- The day before the examination, do not take medications, alcoholic beverages, or smoke.
For older people and people suffering from diseases of the gastrointestinal tract, it is recommended to prepare the body for the examination in advance. Compliance with the rules is the basis of high-quality diagnostics. 3 days before the fluoroscopy, follow these recommendations.
Preparing for the study:
- Dieting. The patient is prescribed a diet menu to “unload” the stomach and remove toxins. Proper nutrition reduces bloating and gas formation. Recommended menu: water porridge, fresh steamed dishes, dietary meat, lean fish. Exclude: fatty, spicy foods, smoked meats, marinades, mushrooms, legumes, cabbage, dairy products, bread, baked goods, confectionery, alcohol, carbonated drinks. The list of permitted products is discussed with the doctor.
- Cloth. It is recommended to do an enema to completely cleanse the body before starting the examination.
Be sure to clarify the rules for preparing the body for x-rays to conduct informative diagnostics. Neglecting the recommendations will lead to inaccurate or incorrect results and the procedure will need to be repeated. Before conducting the study, the doctor must familiarize the patient with what fluoroscopy involves, the purpose of the method, how it will be carried out, and what is needed for this. The procedure may be carried out for a fee.
What to do immediately before the procedure
X-ray of the stomach takes a lot of time and requires patients to carefully follow the doctor's instructions. Before the diagnosis begins, the person is given a barium suspension to drink. It has a viscous consistency and whitish color, and tastes like chalk. This substance is inert and does not cause any harm to the body. If the patient has a pronounced gag reflex, the doctor may suggest that he take a drug that relieves spasms (No-shpa, Spazmalgon).
The doctor will tell you which foods should be excluded from the diet before diagnosis.
Taking any medications without a doctor's prescription is highly discouraged. After such preparation, the patient is brought to the X-ray machine and the position of the equipment is adjusted according to the patient’s height. The examination is carried out in a standing position. Next, the person is asked not to move and hold his breath for a while so that the picture is as clear and informative as possible.
After this, the specialist takes a series of x-rays in various projections, after which he develops them on a special film and delivers the finished result. Preparatory measures for a survey radiography of the abdominal organs are extremely important to obtain a high-quality image, which will be the key to a correct diagnosis and timely treatment.
Double contrast in the study of the stomach and intestines
The gastrointestinal tract can suffer from many pathologies, and standard fluoroscopy methods cannot always give a complete picture of what is happening. In some cases, the doctor may see the need for double contrast fluoroscopy. It is carried out with the same barium suspension, but the patient needs to drink it through a special perforated tube, which allows air to enter the stomach.
Massaging the anterior abdominal wall promotes better distribution of barium along the walls of the stomach, and the air entering it ensures the straightening of the folds. If it is necessary to study the large intestine, a contrast agent is injected into it through an enema. Special preparation is required before the study. Prescribing a diet during fluoroscopy of the large intestine is also desirable, as when examining other parts of the gastrointestinal tract.
Indications for an X-ray of the intestine and preparation for the procedure
The diagnosis is prescribed by a gastroenterologist or oncologist. The following symptoms may be the basis for prescribing research:
- loose and frequent stools with a change in color to black;
- pain in the intestinal area;
- chronic constipation;
- the appearance of blood or pus in the stool.
Intestinal examinations require careful and high-quality preparation; the doctor will tell you about all its nuances. The quality of the resulting images depends on how thorough the preparation for the procedure is. This is all the more important, since during the procedure the body will receive radiation exposure, and repeated diagnostics will not be possible soon. It should be remembered that a week before the procedure you should give up smoking and alcohol.
General rules for preparing for gastric fluoroscopy for patients
The stomach x-ray procedure is considered simple and does not require special preparation from the doctor or patient. There are, however, rules that must be strictly followed to obtain objective data and successfully carry out the procedure:
- The patient takes his last meal at least 12 hours before the procedure.
- On the day of the x-ray, you should stop taking medications, inhalations, smoking, and chewing gum.
- 2-3 days before the study, you should follow a gentle diet, excluding any foods that contribute to gas formation.
- On the eve of the procedure, it is recommended to do a cleansing enema.
- If obstruction of the pyloric part of the gastrointestinal tract is established, then immediately before the study the patient is prescribed lavage using a probe.
- The patient should give preference to loose clothing that does not contain metal parts.
- Immediately before the procedure, you must get rid of any jewelry, dentures, or excess clothing.
Compliance with the above rules will allow you to achieve maximum effect from the stomach x-ray procedure
Negative effects of X-rays
Long-term strong and weak ionizing radiation affects all living organisms, especially their DNA. Therefore, it is necessary to inform your doctor about the number of x-ray examinations performed in a given year to avoid unwanted radiation exposure.
The X-ray method allows you to see the condition of human organs without surgical intervention. The essence of the method is simple - a beam of X-rays passes through the tissues of the body and leaves a negative image on a light-sensitive screen or special film. The quality of the image depends on the ability of the area being examined to transmit x-rays. Examination of hollow organs, such as the stomach and intestines, is difficult due to the fact that X-rays pass through them unimpeded, leaving no visual imprint. An element such as barium, or rather one of its compounds, came to the rescue.
Barium sulfate is a contrast agent that absorbs X-rays well. It is not dangerous for the human body, since it does not dissolve in the acidic environment of the stomach and, accordingly, is not absorbed into the blood. The contrast agent is taken orally and examined as it passes through the gastrointestinal tract.
Methods for X-ray diagnostics of the stomach and intestines using a contrast agent
In the study of the stomach and intestines, two diagnostic methods are used: fluoroscopy and radiography.
Radiography - obtaining an x-ray image depicting the object of study. The image can be examined many times, passing it on to various specialists. However, a flat image does not show the functional state of the organ.
Fluoroscopy allows you to see internal organs on a screen and track their functioning in real time.
Methods for contrasting the stomach with barium
Contrasting is the process of penetration of barium sulfate into the esophagus and stomach after taking a specialized solution. The solution is prepared immediately before the procedure.
To fully understand the state of the organ and its work, several contrasting methods are used:
- Primary contrast. Along with the stomach, the condition of the esophagus is usually diagnosed. After several sips of the contrast agent, fluoroscopy or a series of images in several projections begins.
- Double contrast. This method is necessary to assess the structure and relief of the inner surface of the stomach. To do this, prepare a special solution from barium sulfate and drugs that pump gas into the stomach. The air environment straightens the folds of the stomach, and barium makes them clearly visible on the screen or image.
During the study, a number of images will be taken in different projections to assess the condition of the stomach and make an accurate diagnosis.
Description of the fluoroscopy method
Contrast fluoroscopy is one of the methods for accurately diagnosing a number of diseases of the stomach, duodenum and esophagus; the duration of the examination is 20-30 minutes. Purpose of the procedure:
- Detection of stomach pathologies;
- Included in the comprehensive diagnosis of ulcers, tumors, enteritis;
- The structure of the mucous membrane is studied;
- Detection of gastrointestinal motility disorders.
The patient first takes an x-ray of the stomach organs to identify and evaluate pathological changes. The fluoroscopy procedure is performed by introducing a contrast agent. Use:
- Water-barium suspension;
- Double contrast (air and water-barium suspension).
Types of contrast agents: Barium, iodine, helium and other substances are used as contrast media to better reflect the x-rays of the scanned tissue, resulting in better visibility and quality of the resulting image.
Examination of the abdominal cavity using this method is painless and does not cause any discomfort. The patient is given a liquid with barium to drink in a volume of 200-600 ml (a white contrast agent that tastes like calcium). Before the procedure, be sure to remove all metal objects (hairpins, pins, chains).
Contrast enhancement (contrast enhancement) allows for a more accurate visual analysis of pathologies of the abdominal organs. The patient can observe the process in real time, the data is projected onto the monitor.
During the examination, the patient must take different body positions:
- Horizontal;
- Vertical;
- Oblique;
- You will need to roll over onto your right side (left), stomach and back. This is done to ensure even distribution of the contrast agent.
The patient takes a water-barium suspension and the filling of the abdominal organ is monitored on the monitor. The doctor takes the necessary photographs (photos in black and white). They are displayed on the screen. The examination reveals the anatomical features of the stomach, the anterior and posterior walls of the organ, and the condition of the duodenum. In a hospital setting, it is preferable to carry out diagnostics using the double contrast method.
After the procedure, the doctor warns the patient about possible consequences (bloating, possible abdominal pain, changes in the color of stool, nausea, vomiting). Be sure to report these symptoms to your doctor.
How does this happen
The study is carried out only on an empty stomach, after preliminary preparation of the patient. In the X-ray room, the patient takes off his clothes and puts on a special gown. Be sure to remove all jewelry and notify your doctor if there are metal inserts in your body. After this, the laboratory assistant takes a survey photograph in a standing position; further process is possible only after the first photographs. This is necessary to eliminate the possibility of internal bleeding, organ ruptures, and acute obstruction. The resulting photos are examined by the doctor; if there are no contraindications, contrast is performed.
A mixture is prepared in the laboratory: a solution of water and barium sulfate. The subject takes a few sips of the drink. It tastes and smells like chalk and does not cause any unpleasant sensations. After entering the esophagus, the barium mixture covers the mucous membrane of the gastrointestinal tract, and the esophageal tube becomes clearly visible on the screen. For subsequent examination of the stomach and duodenum, the patient drinks the remainder of the solution - 200-250 ml. The fluid fills the organs and they are better visible in the image; ulcers, neoplasms, deformations, and narrowings are easily visible.
To get a complete picture, the patient is placed on a table and a series of photographs are taken. Diagnosis is carried out in direct, lateral and oblique projections. To do this, the patient is asked to change his position several times.
After receiving the data, the radiography procedure is considered complete. In some cases, an x-ray of the lower intestine is needed, then the process is repeated a few hours later, when the barium enters the large intestine.
Once the radiologist has enough information, he will write a report and describe the images. Sometimes this takes several days, sometimes the patient can receive results after 30-60 minutes. With this data, he goes to the doctor who referred him for examination. The attending doctor will be able to establish a diagnosis and determine treatment, or, at best, determine that there are no diseases or complications.
What does a fluoroscopy of the stomach show?
X-ray with contrast allows not only to detect the presence of pathological changes in organs in the digestive system, but also to track the dynamics of the development of the disease and the effectiveness of therapy.
What pathologists does an x-ray of the stomach reveal:
- ulcers - contrast is distributed unevenly, fills niches;
- reduction or increase in the volume of the stomach cavity;
- tumors, polyps, or a predisposition to their occurrence;
- deformation or displacement of the walls of organs or the stomach itself relative to other organs - pathology develops with a hernia of the diaphragm or abdominal wall;
- violation of the lumen of the stomach, duodenum - this pathology occurs when a malignant tumor develops inside or outside the organ;
- foci of inflammation.
Fluoroscopy in the Trendelenburg position is performed if a diaphragmatic hernia is suspected.
X-ray helps detect stomach ulcers
Performing fluoroscopy
After the patient is fully prepared for the study, he drinks barium, the amount of which in the standard procedure is 250 ml. Gradually washing the gastrointestinal tract, contrast gives the radiologist the opportunity to examine the condition of the mucous membranes, identify their defects by the degree of filling with contrast, and find out the time required for the onset of the absolute filling phase.
After this, the phase of “tight” filling begins. At this time, the doctor receives the following information:
- stomach size;
- form;
- location of all digestive organs;
- displacement and structure;
- extensibility and contractility.
Ulcer niche
Here you can determine the specific location where the ulcer or tumor is located. If there is a suspicion of a tumor, additional examination will be required, since X-ray methods do not allow determining the type of tumor - whether it is benign or malignant. Standard fluoroscopy may not detect some pathologies.
To obtain more information, fluoroscopy of the esophagus and stomach in the Trendelenburg position may be prescribed. The patient fixes the pelvis in an elevated state of 45 degrees - this position allows you to clearly diagnose a hiatal hernia. In addition, the doctor often asks the person to lie on his side, or take a different position, depending on the characteristics of the suspected disease.
Immediately before fluoroscopy, consultations are held with the participation of specialists:
- attending physician;
- radiologist;
- gastroenterologist.
If necessary, doctors of other specialties also take part in the preliminary examination.