Violations of normal heart rate are conventionally divided into two groups. The former do not pose a particular threat to life and health until a certain point. Their treatment allows for delays and lengthy clarifications.
The latter do not involve any delays, since there is always the possibility of cardiac arrest. What’s worse, it’s impossible to predict when the fatal event will happen in a day, a week, a year.
Ventricular fibrillation is one of these threatening phenomena. Accordingly, therapy must be started immediately, and it is often impossible to radically correct the situation non-invasively. Even implantation of a defibrillator does not provide a 100% guarantee of survival.
The essence of the pathological process is a disruption of the normal conductivity of the atrioventricular node. This is a special accumulation of cardiomyocytes that transport electrical impulses further along the cardiac structures, in particular the ventricles.
As a result, the organ begins to contract chaotically, without a clear pattern, separately. The efficiency of blood ejection drops significantly. The less liquid connective tissue is pushed into the large circle, the more likely the patient will die.
Flutter and ventricular fibrillation: symptoms and treatment
Ventricular fibrillation and flutter are life-threatening heart rhythm disturbances that are essentially chaotic contractions of sections of the ventricular myocardium.
With fibrillation, the rhythm is irregular, and with ventricular flutter, the appearance of regular electrical activity of the heart remains. However, with both types of arrhythmia, there is hemodynamic inefficiency, that is, the heart does not perform its main function: pumping. The outcome of such rhythm disturbances is usually cardiac arrest and clinical death. Ventricular fibrillation is usually accompanied by contractions of individual groups of muscle fibers of the heart with a frequency of 400 to 600 per minute, less often - from 150 to 300 contractions. During ventricular flutter, individual sections of the heart muscle contract at a frequency of about 250–280 per minute.
The development of these rhythm disturbances is associated with the mechanism of re-entry, or re-entry. The electrical impulse circulates in a circle, causing frequent contractions of the heart muscle without its normal diastolic relaxation. With ventricular fibrillation, many such re-entry loops appear, which leads to complete disorganization of myocardial contractility.
Ventricular fibrillation and flutter can occur as a consequence of other heart rhythm disturbances, as well as for “non-arrhythmic” reasons.
The development of such a severe complication may be a consequence of recurrent stable or unstable ventricular tachycardia, frequent polymorphic and polytopic ventricular extrasystoles. Bidirectional ventricular tachycardia with long QT syndrome, paroxysmal fibrillation or atrial flutter against the background of Wolff-Parkinson-White syndrome can transform into such a disorder. Ventricular fibrillation and flutter can occur as a side effect of cardiac glycosides and some antiarrhythmic drugs. In this case, arrhythmia develops against the background of electrical instability of the myocardium.
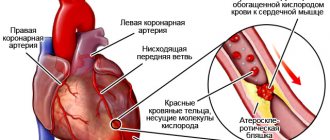
In 25% of cases, the development of ventricular fibrillation and flutter is not preceded by ventricular arrhythmias. These conditions can develop during acute coronary insufficiency, including myocardial infarction. It is believed that undiagnosed atherosclerosis of the main coronary arteries is one of the most common causes of flutter and ventricular fibrillation.
These pathologies are often found in patients with left ventricular enlargement due to various reasons (aortic stenosis, cardiomyopathies). Complete atrioventricular and nonspecific intraventricular block also predispose to the development of these arrhythmias. Other causes may be electrical trauma, hypokalemia, severe emotional stress, accompanied by intense release of adrenaline and other catecholamines. Anesthetic overdose, coronary angiography and hypothermia during cardiac surgery can also cause such severe complications.
Often the development of such rhythm disturbances is preceded by sinus tachycardia in combination with the release of adrenaline. Therefore, ventricular flutter and fibrillation are one of the main causes of sudden death in young people, particularly during sports.
Harbingers of the development of such rhythm disturbances may be short-term episodes of loss of consciousness of unknown origin associated with ventricular extrasystole or paroxysmal ventricular tachycardia. Ventricular fibrillation can also be preceded by painless myocardial ischemia, manifested by an unreasonable decrease in exercise tolerance.
At the beginning of paroxysm of ventricular flutter, several contractions with high amplitude are recorded on the electrocardiogram, then frequent irregular contractions of the myocardium occur. Gradually, the waves of contractions become more rare, their amplitude decreases, and eventually the electrical activity of the heart fades away. Usually the duration of such an attack is up to 5 minutes. In rare cases, sinus rhythm may then return on its own.
3–4 seconds after the development of ventricular flutter, the patient feels dizzy; after 20 seconds he loses consciousness due to severe oxygen deprivation of the brain. After 40 seconds, tonic convulsions are recorded once.
Flutter and fibrillation of the ventricles are accompanied by cessation of the pulse in the large arteries, severe pallor or cyanosis (blueness) of the skin. Agonal breathing occurs, which gradually stops in the second minute of clinical death. 60 seconds after the onset of the attack, the pupils dilate and stop responding to light. Involuntary urination and defecation are possible. In the absence of help, after 5 minutes irreversible changes in the nervous system develop and death occurs.
Causes of pathology
Fibrillation and ventricular flutter occur due to the pathology of impulse transmission through the myocardium.
These rhythm disturbances are successive stages of the development of one process. In ICD-10 (International Classification of Diseases, 10th revision) they are classified under one heading. Dysfunction of the cardiac pathways can occur as a result of:
- large scar (consequence of myocardial infarction);
- focal post-infarction cardiosclerosis;
- coronary heart disease;
- acute myocardial infarction;
- cardiomyopathy with severe hypertrophy of cardiomyocytes;
- dilatation (stretching of the walls) of the heart chambers;
- arrhythmogenic cardiomyopathy;
- myocarditis (inflammation of the heart muscle);
- valve defects;
- severe intoxication (including alcoholism).
Principles of treatment
If paroxysm of flutter or ventricular fibrillation is documented (for example, on the electrocardiogram monitor screen), a precordial blow to the lower third of the sternum can be used in the first 30 seconds. In some cases, it helps restore normal electrical activity in the heart.
Cardiopulmonary resuscitation should begin immediately, including restoration of airway patency, artificial respiration and chest compressions.
The main treatment method for ventricular fibrillation and flutter is electrical defibrillation. It is carried out by trained personnel using a series of electrical pulses of increasing energy. At the same time, artificial ventilation is performed. Drugs that stimulate the basic functions of the cardiovascular system are administered intravenously: adrenaline, lidocaine and others.
With correct and timely cardiopulmonary resuscitation, the survival rate is up to 70%. In the post-resuscitation period, lidocaine is prescribed to prevent ventricular arrhythmias, atropine, dopamine, and correction of disseminated intravascular coagulation syndrome and brain dysfunction is carried out.
Read also: Signs of pulmonary edema in cats
The question of further tactics is being decided. One of the modern methods of treating paroxysms of fibrillation and ventricular flutter is the installation of a cardioverter-defibrillator. This device is implanted into the chest and helps to recognize ventricular arrhythmias in time, while delivering a series of impulses that restore sinus rhythm. In other cases, implantation of a dual-chamber pacemaker is indicated.
Medical animation on the topic “Atrial fibrillation”:
Complications
It is vital that a person with ventricular fibrillation receives immediate care followed by treatment in a cardiac hospital. If this does not happen, an unfavorable outcome may occur within 30 minutes to 1 hour.
Complications of ventricular fibrillation include coma and impairment of neurological functions (intelligence, speech, memory, and others). They arise due to the death of brain cells during oxygen starvation, which occurs from the onset of an arrhythmia attack.
As a result of a serious condition and coma, the following may occur:
- aspiration pneumonia, caused by particles from the stomach entering the lungs;
- “stunning” of the myocardium, accompanied by a constant decrease in cardiac contractility;
- convulsive attacks.
With indirect cardiac massage, fractures of the sternum and ribs often occur. The doctor who assisted the patient should not be blamed for this. It is sometimes believed that such fractures are an indicator of effective resuscitation efforts.
What is ventricular fibrillation
Normal contraction of the heart muscle is ensured by bioelectric impulses. They are generated by the atrioventricular and sinus nodes. The impulses affect the myocardium, cardiomyocytes of the atria and ventricles, provoking the heart to push blood into the vessels. When the conduction of impulses is disrupted, arrhythmia occurs. Ventricular fibrillation is a condition in which chaotic movement of myocardial muscle fibers occurs. They begin to work inefficiently, with a frequency of 300–500 beats per minute. For this reason, urgent resuscitation of the patient is necessary.
The result of fibrillation is a rapid decrease in the number of heart contractions. The volume of ejected blood decreases along with blood pressure, which leads to complete cardiac arrest. If it is not started with the help of special resuscitation measures, the patient will live no more than 3–5 minutes. The arrhythmia cannot stop on its own, so artificial defibrillation is required.
Fibrillation often occurs due to cardiovascular pathologies. The main ones include:
- Complete blockade of the atrioventricular node.
- Cardiac ischemia.
- Complication of myocardial infarction.
- Cardiomyopathies – hypertrophic (thickening of the heart wall), dilated (enlargement of the heart chambers), idiopathic (impairment of the structure of the heart).
- Arrhythmias - ventricular extrasystole, paroxysmal tachycardia.
- Heart and valve defects (aneurysm, mitral valve stenosis).
- Acute coronary insufficiency (narrowing of large vessels).
There are less common causes of ventricular fibrillation. These include:
- Cardiomegaly (increase in heart size).
- Cardiosclerosis (scarring of the heart muscle).
- Brugada syndrome (hereditary ventricular arrhythmia).
- Myocarditis (inflammation of the myocardium).
- A sharp decrease in the volume of blood pumped out by the heart due to problems of unknown etiology.
The causes of ventricular fibrillation can be caused by processes not related to heartbeat disorders. They are shown in the table:
Electrolyte imbalance
Potassium deficiency leads to myocardial instability
Overdose of diuretics or cardiac glycosides
Severe poisoning with thiazide diuretics, narcotic analgesics, barbiturates
Coronary angiography, cardioversion, coronary angiography, defibrillation
Increased acidity levels in the body
There are factors that rarely provoke the development of fibrillation. These include:
- Hypo- and hyperthermia – hypothermia of the body and its overheating with sudden temperature changes.
- Dehydration – can cause bleeding and hypovolemic shock (rapid loss of large amounts of fluid).
- Injuries – mechanical in the sternum area, electric shock, blunt and penetrating.
- Hormonal imbalance due to thyroid pathologies.
- Chronic stress, excessive nervous tension.
Extracardiac factors
The hereditary factor plays a major role. There is more than just predisposition. Certain types of arrhythmia are passed on directly to descendants. This is, for example, Brugada syndrome. It has a genetic nature.
- Major blood loss. Leads to a drop in the level of nutrition of cardiac structures on the one hand, and on the other to a decrease in the amount of circulating liquid connective tissue.
- The same goes for dehydration. A critical level leads to cardiac arrest as a result of impaired myocardial contractility.
- Increased blood acidity. The so-called acidosis.
- Hyperthermia. A rise in body temperature above 39 degrees. Risks are determined in proportion to indicators. Numbers from 40 are considered extremely dangerous. Such levels must be brought down immediately. If the drugs are ineffective, call an ambulance.
- Hypothermia.
- Severe burns (second or third degree, also depending on the area of the lesion).
- Sudden changes in body temperature.
- Chest injuries affecting the heart. Fractures or bruises do not play a big role. After receiving an injury, it is mandatory to undergo an ECG and echocardiography (ECHOCG).
It is advisable to consult a specialized specialist. Any violations are grounds for hospitalization and careful monitoring of the patient.
- Procedures performed to correct or identify the state of the cardiovascular system. Including coronography, defibrillation, EPI and other techniques. The probability of such an outcome is relatively small, but it exists.
- Intoxications of various types. Including alcohol, drugs, usually heroin or cocaine, antihypertensive and stimulant drugs (cardiac glycosides), also barbiturates and others. Heavy metal salts can play the same role, if not more.
- Insufficient amount of potassium in the body. Metabolic disorder leads to the development of early ventricular repolarization syndrome. Electrical activity becomes unstable.
It may be due to a group of pathological factors. In addition to those already mentioned, which cannot be corrected by the patient’s actions, there are also subjective ones.
These include smoking, consumption of alcohol, drugs, self-medication, excessive physical activity and others. Some are not of pathogenic origin, but also cannot be eliminated.
For example, being female (m/f ratio is defined as 1:4 or so) or age 45+.
Classification
Ventricular fibrillation is usually divided into 3 stages - primary, secondary and late. Primary fibrillation occurs 1-2 days after myocardial infarction. Electrical instability of cardiomyocytes is explained by acute ischemia. More than half of the cases of primary fibrillation are observed in the first 4 hours, 40% - within 12 hours after a heart attack, which is the main cause of mortality in patients with this pathology.
Secondary fibrillation develops due to lack of blood circulation in the left ventricle and is accompanied by cardiogenic shock. This stage is difficult to eliminate by defibrillation, while the primary stage passes after a single electrical impulse. Late fibrillation is observed 48 hours after myocardial infarction or at the 5-6th week of heart disease related to ventricular dysfunction. At this stage, the mortality rate is 40–60%.
Arrhythmia is characterized by symptoms identical to complete cardiac arrest (asystole). Signs of ventricular fibrillation:
- heart rhythm disturbance;
- weakness, dizziness;
- sudden loss of consciousness;
- frequent breathing or lack thereof, wheezing;
- pallor of the skin and mucous membranes;
- cyanosis (blueness of the tips of the ears, nasolabial triangle);
- pain in the heart, cardiac arrest;
- absence of pulse in large arteries (carotid, femoral);
- dilated pupils;
- complete relaxation or convulsions;
- involuntary emptying of the bladder and bowels.
Read also: Situational task of pulmonary edema
Arrhythmia begins suddenly, its appearance cannot be predicted. Signs of fibrillation determine the state of clinical death, when changes in the body are still reversible and the patient can survive. After 7 minutes of arrhythmia, oxygen starvation leads to irreversible damage to the cerebral cortex and the process of cell disintegration begins, i.e. biological death.
The mechanism of pathology development
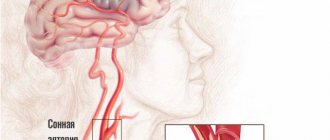
In the walls of the ventricles there are groups of cells capable of independently generating bioelectric impulses. With complete blockade of the atrioventricular node, this ability leads to the appearance of many isolated impulses circulating through the cardiomyocytes of the ventricles.
Atrioventricular block is the cause of ventricular fibrillation
Their strength is sufficient to cause weak, isolated contractions of individual groups of cells, but not enough to contract the ventricles as a whole and for a full cardiac ejection of blood.
The rate of ineffective ventricular fibrillation varies from 300 to 500 per minute, while the impulse does not weaken or interrupt, so the arrhythmia cannot stop on its own (only after cardiac arrest or artificial defibrillation).
As a result, the strength of heart contractions, ejection volume, and blood pressure rapidly drop, resulting in complete cardiac arrest.
Diagnostics
The likelihood of fibrillation is indirectly determined by signs of cardiac arrest or sudden death. This condition can be confirmed only using one diagnostic method - ECG (electrocardiography). The advantages of the study are the speed and possibility of carrying out the procedure anywhere. For this reason, resuscitation teams are equipped with cardiographs.
Ventricular fibrillation on ECG
An electrocardiogram records the main stages of fibrillation development. These include:
- Ventricular flutter or short (20 seconds) tachysystole.
- Convulsive stage - lasts 30–60 seconds, accompanied by an increase in contraction frequency, a weakening of cardiac output, and rhythm disturbances.
- Fibrillation – 2–5 minutes. Large, chaotic frequent flickering waves without pronounced intervals are observed. The P wave is also absent.
- Atony – up to 10 minutes. Large waves are replaced by small ones (low amplitude).
- Complete absence of heart contractions.
Other reasons
Less commonly, the development of this disorder can occur as a result of intoxication with cardiac glycosides, electrolyte imbalances, high levels of catecholamines in the blood, electrical injuries, chest injuries, cardiac contusions, hypoxia, acidosis, hypothermia. Also, ventricular tachycardia can be caused by some of the drugs, for example, sympathomimetics, barbiturates, narcotic analgesics, antiarrhythmics.
Another cause of flutter is cardiac surgery procedures. These include coronary angiography, electrical cardioversion, and defibrillation in the cardiology department.
Urgent Care
Before the arrival of the resuscitation team, the victim with fibrillation must be provided with emergency assistance. It involves carrying out resuscitation measures. First stage:
- You need to hit a person in the face if he loses consciousness. This will help bring him to his senses.
- Determine the presence of pulsation in the carotid or femoral arteries, observe whether there is movement of the chest.
- If there is no pulse or breathing, you should proceed to first aid.
The second stage consists of performing closed cardiac massage and artificial ventilation. The algorithm is as follows:
- Lay the victim on a flat, hard surface.
- Tilt your head back, clear your mouth of vomit, and remove your tongue if it is stuck.
- With one hand, pinch the victim's nose and blow air through the mouth.
- After insufflation, fold your hands crosswise and apply rhythmic pressure on the lower third of the sternum. 2 deep breaths, then 15 compressions.
- After 5-6 cycles of resuscitation, assess the condition of the victim - check for pulse and breathing.
Closed heart massage is performed rhythmically, but without sudden movements, so as not to break the ribs of a person with fibrillation. You should not try to deliver a precordial blow to the heart area unless you have special skills. Emergency care must be provided in the first 30 minutes of the onset of arrhythmia and before the arrival of medical specialists, who should be called before resuscitation begins.
Forecast
About a quarter of patients survive resuscitation. Half of them die within the first year from the moment of discharge if radical treatment is not carried out.
The operation can significantly improve the outcome. It is recommended to ask your doctor what you can expect. Too many variables.
Usually the survival rate is 50-60% for 5-10 years, sometimes more. Positive and negative factors are taken into account: addictions, age, gender, general health, history of somatic pathologies, and others.
Treatment of ventricular fibrillation
Sudden cardiac arrhythmia cannot be treated. You can prevent fibrillation in some heart diseases by installing a pacemaker or cardioverter defibrillator. Therapy involves providing first aid to the victim and using special resuscitation equipment:
- Defibrillation is the restoration of heart rhythm using electrical impulses of varying strength and frequency.
- Carrying out artificial ventilation of the lungs - manually using an Ambu bag or through a breathing mask with a ventilator.
- The use of drugs for cardiac resuscitation - Epinifrine, Amiodoron.
Consequences and complications
Since fibrillation is a borderline condition, it is impossible to avoid negative consequences after rhythm restoration. Various cardiac arrhythmias and circulatory disorders are always a consequence of hypoxia.
Any patient, after the attack has stopped, is under the supervision of a cardiologist and requires periodic inpatient treatment. Antiarrhythmic and other medications are prescribed for life.
Complications that occur immediately after defibrillation and cardiopulmonary resuscitation are as follows:
- Skin burns in the area affected by defibrillator electrodes.
- Rib fractures after chest compressions of the heart muscle.
- Aspiration pneumonia.
- Pneumothorax.
- Thromboembolism.
- Cardiac dysfunction.
- Arrhythmia, including atrial fibrillation.
- Brain disorders, including various types of encephalopathies.
Sometimes, as a result of the death of brain cells, patients' motor functions are impaired and the functioning of internal organs suffers.
Ventricular fibrillation: causes, stages and emergency care in case of clinical death
One of the main causes of sudden death during myocardial infarction is ventricular fibrillation, in which the cellular structures of the heart muscle work chaotically and arrhythmically, without performing a pumping function. A fatal condition occurs much more often in the first 4 hours after acute cardiac ischemia, and the only effective treatments are primary resuscitation and the use of a defibrillator. But even timely and professionally performed therapeutic measures are not always able to bring a sick person back to life: atrial and ventricular fibrillation in the vast majority of cases (90%) leads to an irreversible condition - biological death.
Prevention
It is difficult to prevent ventricular fibrillation because it is impossible to predict. An attack always occurs suddenly, so preventive measures should begin much earlier and are aimed at eliminating the occurrence of pathologies of the cardiovascular system.
The first and main rule that will help keep your heart and blood vessels healthy is giving up bad habits. Smoking and alcohol cause severe blows to the cardiovascular system, this must be remembered. It is necessary to promote the abandonment of bad habits in the family, because not a single child will believe the propaganda against smoking and alcohol if his parents like to spend evenings with a glass of wine and cigarettes.
Reasonable physical activity is the best exercise machine for the heart and blood vessels. Remember the famous academician Amosov, who retained the ability to operate on patients at the age of 80 - he walked up to the 8th floor every day and went for daily jogs. Speaking about physical activity as reasonable, we also want to prevent excessive zeal in sports. In recent years, the popularity of bodybuilding has grown among young people; in pursuit of a beautiful body, young people independently and uncontrollably increase physical activity, combining this with a certain, not very healthy diet. Sports nutrition of questionable quality, dietary supplements that are not confirmed by quality certificates, need to be removed from your life. After all, everyone knows the term “athletic heart” and what this pathology leads to. Exercise, active recreation with the whole family, daily walks are the best option for reasonable physical activity.
Try not to get into stressful situations. It is clear that it will not be possible to completely exclude them, but at least you can avoid provoking them. Try to get enough sleep, do not overload yourself with supposedly urgent matters - plan your work and rest correctly.
Pay attention to your diet. Nutrition is the most important aspect of a healthy life, no doubt about it. When purchasing groceries, pay attention to vegetables, fruits, fish, nuts, and dairy products. Save smoked delicacies and kebabs for the festive table. Monitor the amount of liquid you drink, pay attention to what you drink. The best option is water, herbal tea, fruit drinks prepared with your own hands. A bad option is juice from a box, sweet compote, soda and endless coffee. Eat often, but little, the volume of food per meal should not exceed 200 ml.
Take care of your health. This is especially important if your family already has patients with a diseased heart or blood vessels. Monitor your blood pressure daily and periodically take biochemical blood tests to check your potassium and cholesterol levels.
If you suffer from chronic heart disease, be sure to take your medications methodically. Do it as prescribed by your doctor; creative approaches to taking medications are unacceptable. Do ECGs regularly and see a cardiologist. Follow medical recommendations carefully and methodically.
If you have coronary heart disease or arrhythmia, do not neglect planned hospitalization. It is a periodic stay in the hospital that will help to conduct a detailed examination, pass clinical tests, adjust treatment, and receive new useful recommendations from a cardiologist. Intravenous drip infusions of drugs to strengthen the myocardium will help avoid sudden attacks.
Try to be in the fresh air more, this will help avoid hypoxia, which is harmful to the heart and blood vessels. Live with positive emotions, smile more often, be friendly. And the heart will be healthy.
Did you like the article? Save it!
Still have questions? Ask them in the comments! Cardiologist Mariam Harutyunyan will answer them.
Ivan Grekhov
Graduated from the Ural State Medical University with a degree in General Medicine. General practitioner
Causes of ventricular arrhythmias
Under normal conditions, the muscular system of the heart contracts simultaneously, rhythmically and synchronously, obeying the sinus node, which is the pacemaker. Ventricular fibrillation and flutter are always asynchronous and unproductive work of muscle fibers and cardiomyocytes, requiring a large amount of oxygen and energy. The lack of coordinated contraction of the myocardium stops vital blood flow in the human body. Ventricular fibrillation, the causes of which must be sought in the ischemic pathology of the heart muscle, leads to the death of the human body. The main causative factors of pathology include:
- large-focal myocardial infarction;
- heart failure;
- post-infarction cardiosclerosis;
- cardiomyopathy (dilated and hypertrophic);
- myocarditis;
- severe forms of rhythm disturbance and impulse conduction;
- acute oxygen deficiency;
- severe hypothermia of the human body;
- metabolic disorders associated with a sharp deficiency or excess of the minerals potassium and calcium;
- toxic effects of poisons and large doses of alcohol;
- drug overdose.
A separate idiopathic variant of ventricular fibrillation is distinguished, when the cause of unexpected clinical death in an apparently healthy person cannot be determined. A possible causative factor may be genetic changes in cardiomyocytes that contribute to the occurrence of ventricular disorders.
Read also: Extrasystoles are normal
The risk of sudden death associated with the occurrence of ischemia of the heart muscle and ventricular fibrillation increases against the background of predisposing and contributing factors:
- lack of regular physical activity;
- smoking;
- overeating with the development of obesity;
- prolonged and excessive consumption of strong alcoholic beverages;
- high blood pressure without adequate correction;
- diabetes;
- atherosclerosis.
Sudden death is a tragedy that can be prevented by following the principles of a healthy lifestyle and regularly visiting a doctor to identify the first signs of cardiac pathology.
Classification of ventricular flutter
During the development process, heart diseases such as ventricular fibrillation and flutter go through four stages:
The first is the tachysystolic stage of ventricular flutter. The duration of this stage is a maximum of two seconds. It is characterized by frequent, coordinated heartbeats. On the ECG, this stage corresponds to 3-6 ventricular complexes with a sharp high-amplitude fluctuation.
The second stage is convulsive ventricular tachyarrhythmia. Its duration is from 15 to 50 seconds. It is characterized by frequent, local contractions of the myocardium of an irregular nature. The ECG reflects this stage in the form of high-voltage waves of varying magnitude and amplitude.
The third stage is the stage of ventricular fibrillation. The duration of this stage is 2-3 minutes. It is accompanied by multiple irregular contractions of individual zones of the myocardium, having different frequencies.
The fourth stage is atony. This stage develops approximately 2-5 minutes after ventricular fibrillation occurs. The fourth stage is characterized by small, irregular waves of contractions, an increasing number of areas that have stopped contracting. The ECG is reflected in the form of irregular waves, the amplitude of which gradually decreases.
Cardiologists distinguish between ventricular fibrillation and flutter according to their clinical development. So, there are constant and paroxysmal forms. In this case, flutters of the second form can be recurrent in nature, that is, they can be repeated several times during the day.
Stages of a deadly condition
The mechanism of development of ventricular fibrillation is due to multiple impulses from different parts of the heart, which trigger a series of uncoordinated contractions passing through 4 consecutive and short stages:
- Atrial flutter – rhythmic contractions lasting no more than 2 seconds;
- Large-wave ventricular fibrillation (convulsive stage) - chaotic contractions of different parts of the heart, lasting about 60 seconds;
- Myocardial fibrillation (stage of small-wave contractions) – up to 3 minutes;
- Atony of the heart.
Ventricular fibrillation, the treatment of which depends entirely on the timely provision of emergency care, leaves a person with little chance of survival. After 30 seconds from the moment of atrial flutter, the patient loses consciousness, after 50 seconds a typical convulsive state occurs. At the end of 2 minutes, breathing stops and clinical death occurs. The only option to start the heart and restore the rhythm is effective resuscitation with the use of a defibrillator at the stage of large-wave contractions, which is only possible in a hospital setting.
Emergency measures
The algorithm of actions in a hospital setting consists of sequentially performed resuscitation measures:
- Primary
- assess the person’s condition (pulse in the carotid arteries, presence of breathing, pupil reaction);
- call for help from personnel who will prepare resuscitation equipment;
- prepare the airways;
- blow air into the lungs (artificial respiration);
- ensure blood circulation (indirect cardiac massage);
- perform defibrillation (3 shocks).
The lack of effect indicates persistent changes in the heart muscle that require intensive therapy.
- Secondary
- pulmonary intubation with artificial ventilation;
- introduction of drugs into the vascular system;
- repeated discharges.
Electric shocks from the defibrillator are optimally administered within the first 5 minutes of resuscitation. Delay sharply reduces the effectiveness of the method: every minute of delay reduces the chances of recovery from reversible death by 10-15%. After 10 minutes from the onset of fibrillation, any emergency measures are useless.
Typical symptoms
Regardless of the cause, all symptoms of cardiac fibrillation are manifested by signs of rapidly developing clinical death:
- loss of consciousness;
- tonic contractions of body muscles (convulsions) with involuntary urination and defecation;
- cyanosis of the skin;
- dilated pupils in the absence of reaction to light;
- cessation of arterial pulsation;
- frequent and noisy breathing, which stops after 2 minutes from the onset of the attack.
The classification of deadly ventricular arrhythmia divides the pathology into 2 types:
- primary (idiopathic);
- secondary (arising against the background of cardiac pathology).
In the first case, clinical death occurs unexpectedly, in the second, the symptoms of heart disease indicate the risk of sudden death, which allows for effective prevention and helps prevent an attack. However, timely cardiac resuscitation of idiopathic atrial and ventricular fibrillation is more effective (sometimes a single defibrillator pulse is sufficient to restore cardiac rhythm) than emergency care when stopping an initially diseased heart.
Symptoms of fibrillation
The clinical presentation of the condition varies slightly depending on who gets it. The following differences occur here: the absence of any circulatory pathologies in myocardial diseases and the severity of the patient’s condition with chronic cardiac pathologies.
Ventricular tachycardia
Ventricular fibrillation (VF) that occurs in a patient without identified circulatory disorders is considered to be primary. The condition may be preceded by ventricular tachycardia or frequent group and multiple extrasystoles.
The beginning of an attack is always violent. The first symptom is severe weakness and dizziness, which increases rapidly and leads to loss of consciousness within 20 seconds. Then convulsions develop and involuntary urination occurs. The skin and mucous membranes acquire a characteristic pale color.
The patient's breathing is impaired, even to the point of stopping (apnea), there is no reaction of the pupils to light, it is impossible to listen to heart sounds or feel the pulse, and there is no blood pressure. After a few seconds, death occurs.
A secondary form of VF develops in severe chronic patients with pulmonary congestion. The symptomatic picture is similar to the clinic of cardiogenic shock. The patient suddenly turns blue or pale and loses consciousness. The skin becomes covered with cold, sticky sweat, and oliguria develops. If apnea does not occur immediately, breathing is characterized by an abundance of moist, bubbling wheezing, and then disappears. Further, the clinical picture develops in the same way as with the primary form.
Important: If cardiac and respiratory activity is not restored within 4 minutes after ventricular fibrillation, the treatment is considered ineffective. Irreversible changes occur in the central nervous system and death occurs.
Diagnostic criteria
In addition to typical symptoms, in hospital conditions the state of clinical death is determined by ECG signs of ventricular fibrillation:
- with atrial flutter on the monitor, the doctor will see frequent and rhythmic waves with a contraction frequency reaching 300 per minute;
- against the background of convulsions in stage 2, large non-rhythmic waves appear with a frequency of about 600 contractions;
- flicker appears on the ECG in small waves, the frequency of which can reach 1000;
- in the final stage, rapid attenuation of the waves and cessation of cardiac activity occur.
Electrocardiographic signs help to quickly assess the situation and make a decision to provide effective assistance, but only in a hospital setting. In ordinary life, you should focus on external symptoms in order to immediately begin emergency measures. Early cardiopulmonary resuscitation and the use of a defibrillator are the most important and mandatory methods of treating clinical death.
What is ventricular flutter?
A similar phenomenon is disorganized electrical activity of the myocardium, which is characterized by frequent and rhythmic contraction of the ventricles. The frequency of such contractions exceeds 200 beats per minute. It can also develop into fibrillation (flicker), which will be frequent, up to 500 beats, but irregular and erratic ventricular activity.
In the cardiology department, specialists classify fibrillation and flutter as dangerous arrhythmias that can lead to ineffective hemodynamics. In addition, they are the most common causes of arrhythmic death. According to epidemiological data, fibrillation and flutter most often occur in individuals whose age ranges from 47 to 75 years. A characteristic feature is that they occur three times more often in men than in women. In 70-80% of cases, the cause of sudden death is ventricular fibrillation.
Symptoms and signs
You can suspect VF in a person based on characteristic signs:
- in 5 sec . the person becomes dizzy and weak;
- in 20 sec . the patient loses consciousness;
- after 40 sec . from the onset of the attack, the patient experiences characteristic convulsions: the skeletal muscles begin to contract once tonically, and at the same time defecation and urination occur involuntarily;
- in 45 sec . from the onset of ventricular fibrillation, the pupils dilate and reach their maximum size after 1.5 minutes.
The patient sometimes has time to complain about:
- strong heartbeat;
- dizziness and weakness;
- heartache.
External signs include:
- pallor of the skin and mucous membranes;
- rapid breathing, shortness of breath;
- loss of consciousness;
- absence of pulsation in large arteries.
Doctors have 4 minutes to restore heart rhythm . If this cannot be done, then irreversible changes begin in the body.
Find out more about the disease from the video:
Treatment measures
Emergency care for ventricular fibrillation is carried out according to a protocol, which indicates the algorithm of the measures to be performed. The first thing they do is check for pulsation in the large arteries, and if there is none, then proceed to CPR (cardiopulmonary resuscitation). First you need to make sure that the airways are clean, and if they are blocked, remove the foreign body.
Next they practice a precordial blow, which is applied to the lower third of the sternum. In some cases, such manipulation leads to the resumption of the cardiac mechanism. If this does not happen, then perform indirect cardiac massage and artificial ventilation. If it is not possible to restore the heart rhythm in this way, then specific measures are taken.
The resumption of the functional activity of the cardiac system is carried out in intensive care wards using a defibrillator, which applies electric pulse discharges to the heart area. Electric discharges of increasing energy are produced (from 200 to 400 J). If fibrillation reappears or persists, then administer Adrenaline every 3 minutes, alternating with shocks with a defibrillator.
Treatment of ventricular fibrillation after stopping the attack and to prevent their recurrence in the future can be carried out conservatively, as well as using surgical intervention. Often, patients are fitted with a pacemaker, which maintains a normal heart rhythm when the patient is prone to developing serious arrhythmias that cause fibrillation.
Classification of species
Experts distinguish 3 types of VF after heart attacks: primary, secondary and late. Although discussions regarding the classification of this disease are still ongoing.
Primary fibrillation occurs 1-2 days after a heart attack. It shows that the myocardium is characterized by electrical instability, which resulted from acute ischemia.
About 60% of primary VF occurs within 4 hours, 80% - 12 hours after a heart attack. Such fibrillation often leads to sudden death. With left ventricular failure and cardiogenic shock, secondary VF sometimes develops in people who have suffered a myocardial infarction.
If fibrillation began 48 hours after a heart attack, it is called late. About 40-60% of people who experience this disease die. In most cases, such fibrillation begins 2-6 weeks after a heart attack. More often it developed in those people whose anterior wall of the heart was damaged.
Doctors distinguish between 2 types of fibrillation. If the rhythm of contractions is correct, and their number does not exceed 200-300 per minute, then we are talking about ventricular flutter. With abnormal rhythm and contraction frequency from 200 to 500 per minute. talking about flickering.
Symptoms and diagnostic methods
As noted above, ventricular fibrillation occurs in the same way as complete cardiac arrest, so the symptoms will be similar to those with asystole:
- In the very first minutes, loss of consciousness occurs;
- Spontaneous breathing and heartbeat cannot be detected, it is impossible to feel the pulse, severe hypotension;
- Widespread bluish discoloration of the skin;
- Dilation of the pupils and loss of their reaction to a light stimulus;
- Severe hypoxia can cause convulsive syndrome, spontaneous emptying of the bladder and rectum.
Ventricular fibrillation takes the patient by surprise; it is impossible to predict the time of its occurrence even in the presence of obvious predisposing factors on the part of the heart. Due to the complete cessation of blood flow, within a quarter of an hour the victim loses consciousness; by the end of the first minute from the beginning of the fibrillation paroxysm, tonic convulsions occur and the pupils begin to dilate.
By the end of the first five minutes of arrhythmia, irreversible processes begin in the central nervous system, which ultimately predetermine an unfavorable outcome: clinical death turns into biological death in the absence of resuscitation measures.
Clinical signs of cardiac arrest and sudden death may indirectly indicate the likelihood of ventricular fibrillation, but this condition can only be confirmed using additional diagnostic methods, the main one of which is electrocardiography. The advantages of an ECG are the speed of obtaining results and the possibility of performing it outside a medical institution, therefore a cardiograph is a mandatory attribute not only for intensive care units, but also for line ambulance teams.
Ventricular fibrillation on an ECG is usually easily recognized by a doctor of any specialty and an emergency paramedic by characteristic signs:
- Absence of ventricular complexes and any teeth, intervals, etc.;
- Registration of so-called fibrillation waves with an intensity of 300-400 per minute, irregular, varying in duration and amplitude;
- No isoline.
ventricular fibrillation on ECG
ventricular fibrillation and its difference from ventricular tachycardia on the ECG
Depending on the magnitude of the waves of random contractions, large-wave ventricular fibrillation is distinguished when the force of contractions exceeds 0.5 cm when recording an ECG (the height of the waves is more than one cell). This type characterizes the onset of arrhythmia and the first minutes of its course.
As cardiomyocytes deplete, acidosis and metabolic disorders increase, the large-wave type of arrhythmia turns into small-wave ventricular fibrillation, which, accordingly, characterizes a worse prognosis and a greater likelihood of asystole and death.
Clinical and electrocardiographic data allow ventricular flutter and fibrillation to be recognized. The ECG picture of ventricular flutter is characterized by regular, rhythmic waves of almost the same amplitude and shape, resembling a sinusoidal curve with a frequency of 200-300 per minute; absence of an isoelectric line between waves; absence of P and T waves.
In the case of ventricular fibrillation, continuously changing shape, duration, height and direction of waves are recorded with a frequency of 300-400 per minute, the absence of an isoelectric line between them. Ventricular flutter and fibrillation should be differentiated from massive pulmonary embolism, cardiac tamponade, paroxysmal ventricular tachycardia and supraventricular arrhythmias.
Preventative measures for fibrillation
Preventive measures for ventricular fibrillation must be taken for persons suffering from myocardial pathologies that can disrupt the rhythm of heart contractions.
To treat arrhythmia, it is necessary to take antiarrhythmic medications that will correct the functioning of the heart valves and normalize the heart rhythm.
If there is a high risk of fibrillation, it is recommended to implant a pacemaker.
3Diagnostics
Ventricular fibrillation on ECG
The electrocardiographic picture of ventricular fibrillation has characteristic features that distinguish it from other rhythm disorders - atrial fibrillation (AF), ventricular flutter, etc. Let's touch on the main points and ECG characteristics of ventricular fibrillation.
- Rhythm. In VF, despite the work of the pacemaker, the myocardium as a whole is not able to obey it, so each fiber is excited chaotically. Therefore, unlike a normal ECG, the rhythm is not sinus and is irregular.
- Heart rate. As mentioned above, there are no effective cardiac contractions of the myocardium. Only flickering waves of contraction of individual fibers can be traced. On an ECG, the frequency of such waves reaches 500-700 per minute.
- Absence of ventricular complexes. Ventricular complexes (qrs complexes) are not visualized, as is the case with atrial flutter on the ECG. Only waves are visible, which initially have a height of up to 5 mm, and then gradually decrease, eventually turning into a horizontal isoelectric line (asystole, cardiac arrest).
Question 98. Ventricular fibrillation and flutter, causes, diagnosis, emergency therapy
Experts determine ventricular fibrillation by external signs. If the doctor is near the patient during the onset of the attack, he will diagnose:
- increased heart rate;
- lack of rhythm;
- difference between heart rate and pulse;
- no difference between I and II heart sounds;
- wheezing in the lungs.
Competent resuscitation measures can save a person. If the attack occurred outside the hospital, you must call an ambulance. A person’s complaints, sudden fainting and characteristic convulsions can be used to suspect VF.
Before doctors arrive, it is recommended to do the following:
- Make sure that a state of clinical death has occurred.
- It is necessary to “start” the heart: in the absence of a defibrillator, a sharp blow is given to the sternum.
- In cases where the heartbeat is not restored, artificial respiration and cardiac massage begin. If resuscitation is carried out by 1 person, then for 2 insufflations he makes 15 rhythmic pressures on the sternum.
Causes of development and risk factors
About 75-80% of sudden deaths that are caused by cardiac problems occur due to VF. This disease occurs in both young and old people.
The risk group includes those patients who have suffered sudden circulatory arrest. Unexpected death affects 10-30% of such patients.
The chance of experiencing VF in people who suffer from idiopathic dilated cardiomyopathy is 10%. Within 1 year after a major heart attack, the disease affects 5% of patients. For hypertrophic cardiomyopathy – 3%.
Fibrillation is characterized by random contraction of the muscle fibers of the heart. The stages of development of the disease quickly replace each other: the patient feels weak, loses consciousness, and his pupils dilate. About 2 minutes pass from the onset of the attack to clinical death.
In most cases, the cause of primary and other types of gastric fibrillation is a complication of myocardial infarction. Experts identify the following reasons for the development of VF:
- IHD of the heart (acute and post-infarction, coronary circulatory disorders);
- hypertrophic cardiomyopathy: death occurs in young people with excessive physical exertion;
- dilated idiopathic cardiomyopathy: fibrillation begins against the background of hemodynamic disorders in half of these patients;
- problems with the right ventricle (arrhythmogenic cardiomyopathy);
- different types of heart defects (the most common cause is aortic stenosis);
- specific cardiomyopathies;
- violation of the electrophysical characteristics of the myocardium.
The disease sometimes develops even in the absence of problems with the heart muscle. Risk factors that in some cases lead to ventricular fibrillation include:
- a sharp decrease in blood volume (this causes a drop in pressure and an increase in heart rate);
- severe poisoning (hypokalemia develops and cardiac excitability increases);
- hypothermia of the body;
- hormonal imbalance that arose due to pathologies of the thyroid gland;
- chronic stress or excessive nervous tension;
- overdose of drugs: diuretics or cardiac glycosides.
There are cases when the cause of ventricular fibrillation cannot be determined.
Symptoms
Ventricular fibrillation is a condition of the heart organ that poses a threat to human life. Fibrillation has pronounced symptoms, which are equivalent to clinical death.
During the period of ventricular arrhythmia, disturbances occur in the blood flow, biological fluid does not enter the system, which provokes a second-by-second increase in hypoxia of the brain, as well as all internal organs and systems.
Ischemia develops with every fraction of a second, leading to a person’s inability to move and, due to a lack of oxygen in the brain, to loss of consciousness.
Death occurs in 98%, and it occurs within a few minutes (up to 60 minutes) from the moment the first symptoms appear.
Symptoms of ventricular fibrillation:
- Disturbance in the rhythm of myocardial heart contractions;
- Headache - severe and sudden;
- The dizziness is quite severe;
- Cardiac arrest;
- Loss of consciousness;
- Lack of breathing, or breathing occurs intermittently;
- Sudden pallor of the skin;
- Cyanosis, which does not occur evenly over the skin (blue ears, lips, blue nose);
- The pulse cannot be felt in large-diameter arteries;
- The pupils dilate and there is no reaction to bright light;
- Body cramps;
- Completely relaxed and unresponsive body;
- Urination that occurs involuntarily (possibly defecation).
Signs of clinical death with fibrillation
The time of clinical death lasts from 4 minutes to 7 minutes. This is the time before irreversible consequences and destruction begin in the body.
If no help is provided during this period of time and the heart does not start working again, the body’s cells begin to disintegrate, which leads to the biological death of a person.
Ventricular fibrillation occurs suddenly and without preliminary symptoms. All the symptoms of fibrillation occur simultaneously and the patient no longer has the opportunity to change anything.
There is no way to predict the development of an attack of fibrillation; everything happens suddenly and quite quickly.
Due to the cessation of the flow of biological fluid into the bloodstream, a person experiences severe symptoms within 15 minutes in the form of dizziness, weakness and headache, and loses consciousness.
After he has lost consciousness, the most difficult period of paroxysm of ventricular fibrillation occurs.
By the first minute after the onset of clinical death, tonic convulsions occur, the pupils of the eyes begin to dilate.
The second minute of the coma stage is characterized by intermittent breathing, or its complete stop, the heartbeat does not appear, and the pulse in the large arteries is not audible. There is no way to measure blood pressure index.
Cyanosis of the nasolabial region appears, and cyanosis appears at the tips of the ears. The neck veins become engorged with blood and become very noticeable. The face takes on a puffy appearance.
Ventricular fibrillation on the ECG, depending on the time elapsed since the onset of the attack
By the end of the fifth minute of an attack of clinical death, irreversible processes of decay of the body begin. If resuscitation efforts do not occur, then the person experiences biological death.
It is possible to determine that the cause of clinical death is ventricular fibrillation using a portable cardiograph in an ambulance, and immediately begin to resuscitate the patient.
Rehabilitation
After ventricular fibrillation, the patient is monitored.
His condition is constantly monitored using a Holter ECG: this is done continuously for 1-7 days.
Treatment is aimed at preventing recurrence of attacks.
If patients experience fibrillation due to heart disease, then surgical intervention is performed. Surgeons can install a device that will correct the myocardial rhythm.
The radiofrequency ablation method is also used - this is the introduction of a special device that destroys the pathological focus of abnormal heart rhythm.
Drug antiarrhythmic therapy is also carried out. To prevent possible complications, anticoagulants are prescribed. They prevent increased blood clotting and reduce the likelihood of developing a heart attack. They also recommend products that improve metabolism and nourish muscles.
Features of the disease
Ventricular fibrillation (VF) is characterized by chaotic contractions of myocardial tissue.
Their frequency increases from 250 to 480 per minute. The movements of the ventricles cease to be coordinated. As a result, blood circulation stops and the heart stops. The ECG produces irregular and chaotic waves that vary in width, height and shape. At the beginning of the attack they are high-amplitude. This is the so-called large-wave fibrillation. Afterwards, the waves become low-amplitude and their duration increases. At this stage, the effectiveness of defibrillation decreases.
https://www.youtube.com/watch?v=HxldipUjVdE
Often this condition occurs as a complication of extensive myocardial infarction.