Each tick bite causes justified and understandable anxiety in a person - whether this will be followed by infection with a deadly infection, namely encephalitis. Therefore, the signs of an encephalitis tick bite are of interest to most people who are bitten.
It is important to separate the symptoms of encephalitis from another, more common, but no less threatening, infection - Lyme disease, or borreliosis, which at first resembles encephalitis in its manifestations.
In any case, as soon as the first symptoms of illness appear in the affected person, you should quickly contact an infectious disease specialist - only there they will determine whether it is encephalitis and will provide the necessary assistance by giving an injection of immunoglobulin to prevent further development of the infection in the body.
It is especially important not to miss the very initial symptoms of an encephalitis tick bite, so that a person has the opportunity to neutralize the virus that enters the blood during the bite using immunoglobulin serum.
Immunoglobulin against tick-borne encephalitis
Why are encephalitis ticks dangerous and how to recognize them?
Encephalitis ticks pose a particular threat to human life, because they are carriers of a dangerous and serious infection.
The bite of this insect can damage the central nervous system, cause paralysis, brain damage and death. This is how a small bug can ruin a person's life.
It is impossible to determine purely visually whether a tick is infected. In order to find out the degree of danger, the insect itself must be taken to a special laboratory, where the appropriate analysis will be done.
Both tick individuals and tick larvae can be carriers of this infection. They acquire it during their life activity from infected animals.
Where to contact
If you suddenly notice signs of an encephalitis tick bite in a person or symptoms of an encephalitis tick bite in a dog, immediately contact a veterinarian or regular clinic. There you can get professional help and remove the insect using a safe method.
In addition, this way you will be sure that everything was done correctly and there is no threat of the virus spreading. In specialized institutions, the ticks are sent for examination, where, with the help of special tests, they will find out whether it was a carrier of encephalitis.
Signs and symptoms of an encephalitis tick bite
- The moment a tick bites into a person’s skin, it actually sprays a dangerous infection under the skin.
- At the initial stage, it only affects the bite site.
- After some time, harmful substances begin to enter the bloodstream.
- Once the entire body is affected, certain symptoms begin to appear.
The initial symptoms of infection are similar to those of the flu. The symptoms are very similar:
- The body temperature rises to 38 degrees.
- Muscle pain is observed.
- Chills.
- Headache and nausea.
It is much worse if the infection immediately enters the human brain. The symptoms in this case are much more serious and deplorable.
Symptoms may include paralysis of the neck muscles. Such signs may appear a week or two after the bite. At first, the patient may feel discomfort in the neck area and an unusual heaviness of the head. After this, the head simply falls onto the chest as a result of complete muscle atrophy.
Symptoms of infection may include frequent loss of consciousness, even hallucinations.
The course of the disease can be either mild or acute. Moreover, after the body copes with this disease, immunity is developed that can withstand repeated attacks of this infection.
Symptoms
It is important to know that the encephalitis tick is especially active in spring and summer. To find out if you have been bitten by this insect, remember the symptoms accompanying it. First, we propose to study the mechanism of spread of the disease. So, at first the signals of infection with the virus are invisible, a little later the lymph nodes are affected and the virus goes straight into the blood. Further, unfortunately, the encephalitis virus spreads further throughout the body, according to the blood circulation. If the immune system is weak, symptoms will be noticeable already on the third day, but it has been noticed that symptoms appear ten days after the bite.
Incubation period after a bite
The infection enters the human body directly through an insect bite. The incubation period can last up to 1-2 months, depending on the form and degree of danger.
It happened that the first symptoms began to appear in a person only after 2 months. Therefore, you should listen to your body very thoroughly. It is worth paying attention to various changes in the body, even the occurrence of a simple headache.
Forms of encephalitis after a tick bite
Infection with encephalitis from ticks is classified into several types, or forms:
- Feverish - This is a milder form in which the central nervous system is not affected. With this form, the following symptoms are observed:
- The temperature rises.
- Headache.
- Nausea.
- decreased appetite.
- Meningeal – with this form of infection, the central nervous system is partially affected. This form manifests itself in the following signs:
- The muscles of the back of the head become hard.
- Photophobia appears.
- The temperature rises.
- Strong headache.
- Vomit.
- Poliomyelitis is the most dangerous form, which can lead to complete paralysis of the neck and arms. The result of this form is disastrous - either disability or death.
Tick-borne encephalitis infection clinic
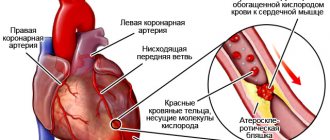
The virus, penetrating into the blood after a bite, multiplies in protective blood cells - macrophages. Then the stage of viremia begins, when new viruses enter the blood. After this, they follow to the regional lymph nodes, cells of the liver, spleen, blood vessels and multiply there again. Next, the viruses enter the motor neurons of the anterior horns of the cervical part of the spinal cord (as a result of which paresis and paralysis occur), into the cells of the cerebellum and pia mater.
The period from infection to the onset of clinical symptoms averages from 7 to 14 days. The severity of the disease depends on the type of bitten tick, the type of pathogen and the duration of blood sucking (the longer, the higher the likelihood of receiving a large dose of the pathogen). It is also known that the severity of the disease increases with the age of the patient.
In the acute period, a ring-shaped erythema may be observed at the site of tick suction. But the main clinical syndromes are general infectious, meningeal and focal.
In the prodromal period, the general infectious syndrome manifests itself in the form of the following symptoms:
- temperature increase,
- general weakness, lethargy,
- headache,
- nausea,
- Sometimes muscle pain occurs in the neck and shoulder girdle,
- feeling of numbness.
With a benign course, this period ranges from 3 to 5 days. In some cases, against the background of severe intoxication, meningeal syndrome occurs, and meningeal signs may not be pronounced, and changes can be observed only in the cerebrospinal fluid.
In severe cases, when encephalitis or meningoencephalitis develops, patients experience delusions, hallucinations, agitation, and the person is poorly oriented in time and space. The patient is inhibited and may feel fear and apathy.
The patient's appearance is characterized by the following features: redness of the face, neck, conjunctiva, injection of scleral vessels, the tongue is covered with a whitish coating, the pharyngeal mucosa is often hyperemic. Abdominal bloating may occur. People often complain of photophobia, lacrimation, and blurred vision.
With diffuse cerebral symptoms, disorders of consciousness, epileptic seizures, respiratory and cardiac problems, signs of cerebral edema, pathological reflexes, as well as paresis of facial muscles and tongue may occur.
With focal cerebral symptoms, hemiparesis, paresis after convulsions, epileptic seizures, and, less often, subcortical and cerebellar symptoms quickly develop. Characteristic lesions of the cranial nerve nuclei. Occasionally, gastric bleeding with bloody vomiting is possible (as a consequence of a violation of the autonomic nervous system).
In some patients, after the prodromal period, a pronounced pain syndrome occurs in the neck and shoulder girdle with periodic muscle twitching, which indicates damage to the motor neurons of the anterior horns of the spinal cord. Weakness and numbness may suddenly occur in any limb, which will subsequently be accompanied by movement disorders.
Over the course of several days, and sometimes even weeks, against the background of elevated temperature and general cerebral symptoms, the intensity of flaccid paralysis of the cervicobrachial and cervicothoracic localization increases (hunched over, stooping, “proud” posture, hanging head on the chest).
Movement disorders can be mixed. For example, flaccid paresis appears on the upper limbs, and spastic paresis appears on the lower limbs. An increase in motor impairment is observed for up to 12 days. By the end of 2-3 weeks, atrophy of the damaged muscles is observed. Also, paralysis can begin in the reverse order - from the lower extremities to the muscles of the trunk and upper extremities.
All these manifestations can occur when infected with any type of tick-borne encephalitis virus, but with the Far Eastern variant, severe and pronounced damage to the central nervous system develops. The disease begins acutely, is very difficult to tolerate, and often ends in death and disability of the patient.
Clinical features of tick-borne encephalitis
The clinical feature of Central European tick-borne encephalitis is two-wave fever.
- Stage 1 corresponds to viremia (circulation of the virus in the patient’s blood). It is accompanied by nonspecific symptoms (fever, weakness, loss of appetite, muscle pain, nausea). In most cases, the person recovers. But in about 30% of cases, remission is observed (5-8 days), and then follows
- Stage 2 , which is characterized by damage to the central nervous system (meningitis, encephalitis).
It should be remembered that with nutritional infection (through milk), an enlargement of the liver and spleen is often observed.
Depending on which symptom complex prevails in a patient with tick-borne encephalitis, the following clinical forms are distinguished:
- febrile,
- two-wave milk fever,
- meningeal,
- meningoencephalitis,
- polio-like,
- polyradiculoneurotic.
After infection and the acute stage, the infectious process can become chronic in several forms (hyperkinetic, which is characterized by Kozhevnikov’s epilepsy; amyotrophic, when the activity of the pathological process is localized in the cervical-brachial girdle).
The virus can remain in active form in the central nervous system and, under favorable conditions, manifest itself after several months or years.
With tick-borne encephalitis, the development of complications is quite often observed. Most often they occur when infected with the Russian spring-summer subtype of the virus.
The most common complications include:
- cerebral edema with the development of cerebral coma,
- hemorrhages in the brain matter,
- gastric hemorrhages,
- Jacksonian or Kozhevnikov epilepsy,
- respiratory and cardiac disorders as a result of damage to the medulla oblongata,
- infectious-toxic myocarditis,
- paralysis
- and, as a consequence, disability of the patient.
Nonspecific complications include the addition of bacterial flora against the background of decreased immunity and the development of severe pneumonia with respiratory failure.
Diagnosis of tick-borne encephalitis
Laboratory diagnostics are used to confirm the diagnosis.
- Clinical blood test: decreased leukocytes and increased lymphocytes and monocytes.
- Clinical urine analysis: the appearance of protein and casts in the urine (with moderate severity of the disease and especially with severe disease).
- Cerebrospinal fluid - slight increase in lymphocytes and increased protein levels.
- Virological methods: isolation of the virus from the blood, cerebrospinal fluid (on the 5-7th day of illness), in cell cultures with further identification using the method of fluorescent antibodies.
- Serological methods: enzyme immunoassay, complement fixation reaction, passive hemagglutination reaction, neutralization reaction in paired sera taken at intervals of 2-3 weeks.
- Polymerase chain reaction: determination of viral RNA in the blood.
Treatment of patients with tick-borne encephalitis
Treatment of patients with tick-borne encephalitis is carried out in the infectious diseases department or in intensive care. Bed rest and a protein diet with a high potassium content are recommended.
Antiviral treatment consists of administering homologous immunoglobulin against the tick-borne encephalitis virus. The faster it is administered, the faster the clinical effect will occur. Its mechanism of action is due to the fact that the antibodies that are part of the drug neutralize the effect of the virus (1 ml binds from 600 to 60,000 lethal doses of the virus), and also protect the cell from further penetration of the virus by binding to membrane receptors.
Also, for specific treatment, ribonuclease is used, which penetrates the membranes of the brain and inhibits the reproduction of the virus in the cells of the nervous system. In some cases, the administration of interferons in small doses is recommended.
Pathogenetic treatment is associated with detoxification (administration of saline solutions). If there is a risk of cerebral edema, glucocorticosteroids are administered. If breathing problems are noted, the patient is transferred to artificial ventilation. To combat hypoxia, hyperbaric oxygenation and sodium hydroxybutyrate are administered. For psychomotor agitation, lytic mixtures and sedatives (Seduxen, Relanium) are used. To treat paralysis, muscle relaxants are administered, as well as drugs that improve blood supply and trophism of brain tissue. To eliminate seizures, patients take anticonvulsant and antiepileptic drugs.
The criterion for discharging a patient who has suffered tick-borne encephalitis is complete normalization of the clinical condition and the possibility of outpatient treatment.
Consequences of a bite - illnesses after a bite
As already mentioned, ticks are carriers of dangerous infections, and this is not just about encephalitis. In any case, after a tick bite, even if the laboratory did not find any cause for concern, the necessary disinfection measures should be taken.
There are the following types of dangerous consequences after a parasite bite:
- Tick-borne encephalitis is the most dangerous disease that can lead to complete disability and even death.
- Lyme disease , which affects the central nervous system. The symptom of this disease is the appearance of a red spot on the body. It appears at the site of the bite. Over time, it can reach large sizes and gradually darken;
- Tick-borne spotted fevers.
- Hemorrhagic fevers - there are Crimean and Omsk types of fevers. It is characterized by kidney damage, the temperature rises, and internal hemorrhage is often possible;
- Ehrlichiosis monocytic.
- Ehrlichiosis granulocytic.
- Babesiosis.
- Tick-borne fevers of Kemerovo and others.
Why do people have different symptoms after an encephalitis bite?
The manifestations of infection may vary for each tick bite victim. This happens for various reasons.
- The main thing is what subtype of virus has entered the blood.
- The second is the general health and activity of the bitten person’s immune system; the weaker the victim’s health, the more severe the disease scenario.
- The third is the number of viruses that enter the bloodstream during a bite. This directly depends on the time the bloodsucker was in the body. This is why it is so important to remove the detected parasite immediately.
- The fourth is how early first aid was provided and immunoglobulin was administered. If the injection was given in the first 4 days, the injected antibodies can neutralize the virus, and the disease may not develop at all.
For your information! Symptoms also vary for each individual infected person due to which organ of the body is affected by the virus. It is customary for doctors to distinguish the febrile form from the meningeal and focal forms. Symptomatic therapy depends on this definition.
First aid
The very difficulty with a tick bite is that its bite cannot be felt. It is practically painless.
Therefore, you can detect it either after a thorough examination of your body, or if the tick has already reached an impressive size, which is almost impossible not to notice:
- The first step, if you happen to find a tick on your body, is to get rid of it immediately. If a person is far from civilization, where there is no possibility of receiving medical care, he will have to act independently, using available means.
- To remove a tick, you will need a tool like curved tweezers; if this is difficult, you can use regular tweezers or a regular thread. Before the tick extraction procedure itself begins, it is worth disinfecting the bite site. Then, prying the tick at the base, you should pull it out with a slightly rocking motion. Many people believe that in order to weaken the tick and make it easier to remove, the bite site should be anointed with sunflower oil. This is not worth doing. Yes, the tick will begin to choke and loosen its grip. But! At this moment, he will begin to choke and inject all the nasty stuff that he has accumulated.
- After the parasite has left the human flesh, the bite site should be treated. To do this, you should take brilliant green, and the skin around the bite should be treated with an antiseptic or hydrogen peroxide.
First aid when detecting a tick
If a tick is detected, first aid must be provided as quickly as possible! If during the examination it is discovered that an encephalitis tick has bitten, the first action should be to remove the parasite from the bite site.
It is necessary to remove the tick from the wound very carefully, since you need to get it out whole! If you pull sharply, the body may remain in the hands, and the infected proboscis of the tick may remain in the wound.
There are several ways to remove a tick from a wound:
- Pour oil into the wound, then the tick will have nothing to breathe, and you can safely remove the body.
- Disinfect the tweezers, carefully pick up the tick and remove it in a counterclockwise circular motion. The principle of operation is the same as in unscrewing nuts.
- When you don’t have tweezers at hand, you can wrap your hands in a cloth and twist it out of the wound in the same way.
- Apply alcohol to the wound. Ticks cannot tolerate alcohol vapors, so it will come out on its own.
A special device is sold in stores - a tick remover, which is convenient for picking up a tick and twisting it out of the wound.
Under no circumstances should you burn the parasite with vinegar or a cigarette while it is in the wound.
This action can provoke a greater risk of contracting an infection, since the tick will get scared and regurgitate back the blood that it has already sucked.
Once the tick has been removed from the wound, it is necessary to save it and immediately go to the hospital. There they will do an analysis to determine the virus and select the correct treatment after the bite. When you contact, the doctor vaccinates you with antibodies to encephalitis and prescribes additional drugs - antiviral drugs. Be sure to take a blood test for encephalitis after 10 days, then two weeks later - for immunoglobulins for encephalitis, and after three weeks - immunoglobulins for borreliosis.
Treatment after an encephalitis tick bite
When certain symptoms begin to appear after a tick bite, it is necessary to undergo a course of treatment. In general, monitoring of the patient's condition should continue for a month.
Many people believe that the most effective remedy after a tick bite is antibiotics. This is wrong. After all, a virus is not a bacterium, so taking antibiotics in an attempt to overcome a dangerous disease is simply pointless:
- The best remedy here would be anti-tick immunoglobulin . This drug is very expensive, this is due to the fact that its components include the blood of donors who have developed immunity to this disease.
- The patient is also prescribed various stimulants that help the body strengthen the immune system. As an example, you can take Anaferon.
- As a more preventative measure, you can consider some kind of diet.
- If we are talking about more severe consequences, such as inflammation of the brain or polyomelitis , then steroid hormones are often taken as therapeutic measures, among which prednisolone can be distinguished.
- If there are seizures of an epileptic nature , then take antiepileptic drugs, for example, Difenin or Phenobarbital.
In any case, the victim of a dangerous tick will not be able to permanently get rid of the consequences of this disease. Now the patient will need to be regularly monitored by a doctor.
Diagnosis of encephalitis
The diagnosis of “tick-borne encephalitis” is made only after a comprehensive examination of the patient. It is necessary to differentiate the disease from disorders with similar symptoms - tumors of the central nervous system, Lyme disease, typhus, encephalitis of other origins and even influenza.
At the first stage, the doctor collects the necessary endemic data and draws up a clinical picture. To do this, the specialist interviews the patient about visiting places of possible infection, obtains information about the patient’s health status and the presence of certain symptoms of tick-borne encephalitis.
Further diagnostics include:
- spinal puncture followed by analysis of the cerebrospinal fluid to examine for the presence of central nervous system disorders, purulent inflammation and bleeding;
- serological study;
- virological method.
The decisive factor in making a correct and timely diagnosis is the molecular biological study of the insect. Therefore, if the parasite was removed from the body independently, it is necessary to immediately place it in a glass container with holes for ventilation and transfer it to specialists for analysis for encephalitis.
Prevention
The best way to prevent a tick bite is to protect yourself as much as possible from this parasite.
To protect yourself from a tick bite, you should take the following precautions:
- When hiking in a forest or forested park area, the presence of open areas on the human body should be reduced to a minimum. Clothes must have long sleeves, trousers or trousers must be tucked into shoes, which are also chosen as high as possible. The head must be hidden under any headdress such as a headscarf.
- When going into the forest, you should apply appropriate anti-tick medications to your skin.
- When in a forested area, you should choose the middle of the path to move and avoid tall bushes or plants.
- After a person leaves a potentially dangerous area, he must immediately check his clothes and the clothes of his loved ones for the presence of this parasite. After all, the tick does not immediately dig into the skin; it can crawl and choose the best place for itself within a few hours, that is, the bite can still be avoided. The main thing is to be vigilant.
- You should not be allowed to bring into your home grass or flowers picked from the forest. Clothes worn in the forest area should also be checked for the presence of dangerous parasites.
- As a preventative measure, you can turn to vaccination, which consists of three stages. Vaccinations are given after 4, 6 and 12 months. You can administer immunoglobulin before visiting a potentially dangerous area. While walking in the forest area, you should take 1 tablet of iodantipyrine.
- Before going into the forest, you can be fully armed. This means that it is worth taking all the necessary preparations that are used to disinfect the bite. You need to make sure that you have tweezers with you, which, if anything happens, can be used to remove the parasite. Taking care of the future, it is also necessary to have a container in which the tick will be delivered to the laboratory. Currently, pharmacies sell entire kits that include all these components.
Precautionary measures
The very first rule among all precautions is to get vaccinated against encephalitis! Having protected yourself with the vaccine, you can safely wander through the forest at any time. It is especially important to take this rule into account during periods of particular activity of ticks - in spring and summer. The news often reports regions with an increased incidence of encephalitis due to tick bites. Therefore, if you live in one of the regions with this problem, get vaccinated!
We recommend reading:
Composition of a travel first aid kit: what to take
A few more rules:
- wear light-colored clothing so that the insect is visible;
- cover your head with a scarf, hat or cap;
- keep ticks away from your body, tuck your pants into your socks and wear rubber boots on top;
- choose long sleeve shirts or turtlenecks;
- apply tick repellent;
- carefully examine yourself and the animals.
Tips and tricks
So, to summarize:
- As recommendations, we can recommend precautionary measures when staying in a forest or city park area. When in the forest you only need to wear the right clothes, which will leave as few places as vulnerable to tick bites as possible.
- Even if the company that goes to the forest, leaving home, did not take care of purchasing the necessary sprays and ointments against insect bites , this is not a problem. Currently, such drugs are sold at any gas station that you will probably come across along the way.
- You can also treat the clothing itself, which you plan to wear in the forest, with special preparations containing acaricides, because these substances can kill ticks. After walking, it is worth examining not only yourself and your loved ones, but also animals that are more susceptible to bites from these parasites.
- It is worth remembering that you can pick up a tick even in your own garden. Therefore, summer residents, or residents of private houses with their own gardens, are in a special risk zone. To eliminate risks, it is worth mowing the grass and ridding your garden plot of unnecessary tall bushes.
- If you plan to have a picnic in the forest, and such occasions are especially popular in the summer, you should choose a safe place to rest. It is best to sit on a sandy surface, or choose a dry forest.
If you adhere to all of the above measures and follow the recommendations, you can protect yourself from sad consequences. Sometimes it is impossible to foresee everything.
If it happens that a tick has nevertheless burrowed into a person’s skin, there is no need to be lazy; you should definitely consult a doctor and get the necessary advice and an algorithm for further actions. You can save yourself from serious consequences, the main thing is to be vigilant in time.
General description of the disease
Tick-borne encephalitis is classified as a natural focal disease that occurs in certain areas. The carriers of the pathogen are wild animals, in this case the encephalitis tick. The main foci of tick-borne pathology are Siberia and the Far East, the Urals, the Kaliningrad region, Mongolia, China, some areas of the Scandinavian Peninsula and Eastern Europe. Every year, about 5–6 thousand cases of encephalitis tick infection are registered in our country.
The severity and form depend on the immunity of the bitten person, the amount of virus in the body, the number of bites, and also on geographic location. Experts divide the encephalitis tick virus into 3 subspecies: Far Eastern, Siberian and Western. The most severe forms of the disease occur after a tick attack in the Far East, with a 20–40% fatality rate. If an encephalitis tick attack occurred in the European part of Russia, the chances of avoiding complications are much higher - the mortality rate here is only 1-3%.
Spread of tick-borne encephalitis in the Russian Federation
What types of ticks carry encephalitis?
Nature is not only a great place to relax and a source of inspiration. It is there that we face great danger in the form of small blood-sucking parasites. They can be found everywhere: in the grass and on the leaves.
Ixodid ticks (Ixodidae) are carriers of the causative agent of tick-borne encephalitis, a disease that mainly affects nerve cells in the human body. These may be brain structures, peripheral innervation, or radicular nerve endings in the spinal cord. Science knows about 650 species of these arachnids. In our latitudes, two species pose the greatest danger: taiga and dog.
Every year, about 2.5 thousand Russians become infected with the encephalitis virus.
Taiga tick
A small spider from 4 to 6 mm, belonging to the order Arthropods. Most often it can be found in the forests of Siberia, the Urals, and the Far East. Due to the fact that over the last century there has been a sharp warming of the climate, the usual habitat of the taiga tick has expanded. Today it can increasingly be found in Belarus, the Baltic countries and south-eastern France. Taiga ticks are carriers of Lyme disease and tick-borne encephalitis.
Dog tick
This type of tick is widespread in the European part of Russia, as well as in the countries of Central and Northern Europe. At the end of spring and beginning of summer there is a peak in the number of their bites. The dog tick is similar to a taiga representative of the family, and by external signs it is almost impossible to distinguish them from each other. Today it is quite often found in summer cottages and garden plots, at camp sites, and in places where dogs are kept. A humid microclimate and the presence of a host are the main conditions for survival.
Contrary to popular belief, ticks very rarely fall from trees. More often they live in grass, soil and fallen leaves.
Ticks are the main carriers of viral encephalitis. But you cannot judge by the appearance of a tick whether it is infected or not. This can only be detected in laboratory conditions. The source of the disease is both the bloodsucker itself and its larvae. The cause of tick infection can be considered to be its previous activity on a sick animal.
How do Ixodid ticks reproduce?
The female tick lays about 15 thousand eggs after drinking blood. But not everyone will reach the adult stage; this largely depends on natural conditions. The end result is usually only a few dozen individuals. The clutch matures within a few weeks.
Incredibly, ixodid ticks feed only 3-4 times during their entire life, which lasts several years: in the larval stage, in the nymph stage, and a couple of times as adults.
The larva feeds once. Small warm-blooded animals become her victims, since it is difficult for her to get to the top. The feeding process can last for 2–3 days, and then the larva becomes a nymph (an adult without sexual maturity). The individual spends the winter in this state. With the onset of spring, the nymph is ready to hunt, and larger animals become its victims. In this state, it matures to the imago stage (adult sexually mature individual) within a year. Unlike females, sexually mature males need from 30 minutes to several hours of preliminary saturation to be able to mate.
Ticks are able to sense the proximity of a person or animal at a distance of 5–10 m. It is for this reason that parasites are found in large quantities on paths and roads.
Video: one tick - two diseases
Prevention of encephalitis
Prevention of tick-borne encephalitis in areas where the disease is endemic must be regular and thorough.
Prevention in adults
Measures to prevent encephalitis can be specific and nonspecific.
Specific measures include vaccination of the population in areas unfavorable for tick-borne encephalitis. Vaccination promotes the development of lasting immunity to the disease.
Vaccination against encephalitis for adults is carried out depending on the season according to a standard (three injections) or accelerated schedule (two injections).
With standard vaccination , the first dose of the vaccine is administered in the fall, and revaccination is repeated after 1-3 months and after 12 months. Then repeated revaccinations are carried out every 2 years.
Vaccination according to an accelerated schedule is carried out in the spring, when ticks are already active. After the first dose, the second is administered 14 days later. During the period of developing immunity, it is recommended to avoid contact with insects.
Contraindications to vaccination are the same almost everywhere:
- chronic non-infectious diseases in the acute stage (diabetes mellitus, stroke, stage 2 and 3 hypertension, tuberculosis and others);
- allergic reactions during exacerbation;
- acute reaction to previous vaccine administration;
- infectious diseases;
- pregnancy;
- intolerance to vaccine components.
Prevention of encephalitis in humans can be non-specific - this includes the use of special anti-tick clothing, repellents in nature, and mandatory inspection after visiting forested areas.
Emergency prevention of encephalitis is carried out in the presence of a bite. As protective measures, administer 3 ml. anti-tick immunoglobulin with a titer of at least (1/160) to destroy the virus. The drug is administered only in a hospital setting. Yodantipyrine and rimantadine are also used to increase the effectiveness of emergency immunization.
Prevention in children
Prevention of tick-borne encephalitis in children has the same principles as in adults.
- Vaccination against tick-borne encephalitis is given to children after examination by a pediatrician from 12 months in endemic areas. Vaccination is carried out only in a hospital setting and a doctor’s conclusion about the absence of contraindications. Contraindications include infectious and non-infectious diseases in the acute phase, intolerance to vaccine components, acute reaction to previously administered vaccines, children under 1 year of age.
- Correct behavior in nature - use of protective clothing, regular inspection, use of children's repellents.
- As an emergency prophylaxis, children under 14 years of age are given 1.5-2 ml. anti-tick immunoglobulin and Anaferon is prescribed as an antiviral drug.
Activity of encephalitis ticks in Russia
Long-term observations of ticks have formed a clear idea of where insect habitats are mainly located. This allows doctors to calculate the density of bloodsucking insects and predict the scale of the problem in the current season.
The activity map of encephalitis ticks can also be useful for people who are far from science. This is a kind of practical guide that allows you to find out how active these parasites are in your region. Today, most of the territory of Russia is occupied by endemic (dangerous) zones for tick-borne encephalitis:
- Northwestern region (Leningrad region, Karelia, Arkhangelsk region),
- Central region (Tver, Yaroslavl, Vologda regions),
- Ural (Sverdlovsk, Perm regions),
- the southern part of Siberia (Krasnoyarsk Territory, Novosibirsk, Tomsk, Omsk, Irkutsk regions),
- Far East (Khabarovsk and Primorsky Territories).
Maps of the incidence of encephalitis are compiled on the basis of official data from the State Sanitary and Epidemiological Supervision of the Russian Federation on the maximum incidence for the current year.
What to do if you are bitten by a tick?
If, after a trip to the forest, you stripped naked, examined your body and found a tick embedded in your skin in some area, then you need to take a number of measures:
- Remove the tick immediately . To do this, you can use tweezers or a special “handle” with a loop at the end, which is sold in pharmacies. Before removing, lubricate the tick with Vaseline or oil. This will cut off its access to oxygen, which will make it easier to remove the insect. Pull out the tick slowly, then you do not risk leaving its head in the body.
- Place the insect in a jar . This measure is necessary for conducting the survey. Doctors will conduct a test to understand whether the tick was a carrier of the virus or not. Only in this way will it become clear whether an infection has occurred.
- Hospitalize the patient . The person is placed in the infectious diseases department, where he is prescribed intensive treatment.
- After laboratory tests of the tick, the infectious disease doctor will prescribe preventive medications - human anti-encephalitis gamma globulin.
The most common areas of tick bites are:
- armpits;
- groin;
- inner thighs;
- neck.
Unfortunately, emergency therapy is effective only in 60% of cases. Therefore, it is advisable to avoid being bitten at all. To do this, every person must follow simple recommendations, especially if he often spends time outdoors and goes to the forest.
We previously wrote about the consequences of borreliosis after treatment.
Such measures include:
- Wearing a special protective suit . The overalls fit snugly to the body and are fully tucked in. The fabric of such a suit is impregnated with a solution that repels insects. There is a protective hood and cuffs, as well as tick traps (special inserts that prevent ticks from moving along the body).
- Take a shower. Ticks are attracted to the smell of sweat. To avoid attracting them to you, wash yourself before going out and use antiperspirant.
- Use of repellents (preparations against insects). Before going into the forest, treat your protective suit with anti-tick aerosol. Do not use the drug on the body. Make sure that the aerosol does not get on the mucous membranes of the mouth or nose.
- Get vaccinated against tick-borne encephalitis . In many Siberian cities, school-age children are forcibly vaccinated against this virus. The vaccine is injected under the shoulder blade or into the shoulder. The procedure is recommended for children aged 4 years and older (imported vaccines are allowed from the age of twelve months). Revaccination is carried out every 3-5 years. The vaccine protects in 95% of cases.
Symptoms and consequences
As soon as a carrier of the causative agent of encephalitis has visited a person’s body and feasted on his blood, infection occurs. The virus enters the blood and, quickly traveling through the circulatory system, ends up in the central nervous system. On the second or third day, it is already detected in the brain tissue.
The most pronounced symptoms appear on the fourth day. The incubation period lasts two to three weeks. The main signs indicating human contact with a carrier of the causative agent of encephalitis include:
- General intoxication.
- Severe headaches.
- Weakness and apathy.
- Feverish condition.
- Nausea transforming into vomiting.
A person bitten by a tick looks very tired, sleepy and lethargic.
Extremely dangerous
What ticks carry encephalitis? Some insects cause a condition called tick paralysis in humans and animals. The bite of these carriers of the causative agent of encephalitis also provokes the development of many dangerous diseases.
On the territory of the Russian Federation, you should be especially wary of the dog tick and the taiga tick.
Consequences
In addition to tick-borne encephalitis, dangerous diseases caused by a tick bite include:
- tick-borne typhus;
- spotted fever;
- Lyme disease;
- tularemia;
- granulocytic anaplasmosis;
- monocytic ehrlichiosis.
Treatment of encephalitis
It should be kept in mind that if there are any signs of complications, it is necessary to seek specialist medical help and, if necessary, receive hospital treatment.
Once a specialist has made a specific diagnosis, steps must be taken to relieve symptoms. To treat the symptoms of encephalitis, the following are used:
- antipyretics;
- anticonvulsants;
- anti-inflammatory;
- antibiotics.
In severe cases, the patient may be taken to intensive care. Separately, the question arises that the many reasons that may underlie brain inflammation require an individual approach in each case.
For example, if it is confirmed that it is viral encephalitis caused by the herpes virus, treatment with antiviral drugs can be started. Treatment must be carried out under strict medical supervision. Often in such cases, anticonvulsants are also used to limit seizures.
Among the drugs that are primarily prescribed for encephalitis after infection with the herpes virus is acyclovir. The drug is an antiviral medicine that is specifically intended for the treatment of herpes zoster. It is also recommended for people with reduced immune capacity, at increased risk of infection, due to other circumstances or diseases, such as after a transplant.
The vaccine will help prevent tick-borne encephalitis and many other diseases, so do not neglect vaccination.
From whom can you get encephalitis?
Ticks are a very widely represented subclass of animals; there are tens of thousands of species, but only a few of them are dangerous to humans. To avoid danger, you need to remember well which tick carries encephalitis and what it looks like.
Different subtypes of tick-borne encephalitis virus are transmitted by ixodid ticks:
- Taiga tick (Far Eastern, Siberian subtype)
- Dog tick (European subtype TBE)
The Far Eastern subtype is the most dangerous, it is characterized by the highest mortality rate.
By the way, not everyone knows that you can become infected with encephalitis not only through a tick bite, but also from the previous carrier of the causative agent of encephalitis - through raw goat and cow milk. Such cases are very rare, but do not ignore this information! Especially considering that, unlike a tick bite, you can completely control the risk of infection through milk and easily prevent it. Outside the carrier’s body, the virus is no longer so tenacious and is completely destroyed if the milk is boiled.
Be vigilant and attentive, study the epidemiological situation in your region, and your outdoor recreation will not be spoiled by the fear of encountering ticks.
Diagnosis and treatment
To detect encephalitis, it is necessary to conduct a blood test. However, the result will not be obtained immediately after the bite. The disease will be confirmed only after 2 weeks. The most reliable way to diagnose pathology is lumbar puncture. Material for research is collected between the processes of the 3rd and 4th lumbar vertebrae. The cerebrospinal fluid is then sent for analysis. The results obtained are compared with established standards. The study will be ready in a week. There are a number of other methods that allow you to get the final result faster. The list includes:
- counter immunophoresis;
- fluorescent antibodies;
- PCR.
If the patient has encephalitis, treatment will depend on the symptoms. They can vary significantly. Even people who have previously been vaccinated need to see a specialist. During the acute period of the disease, bed rest is prescribed. The patient is admitted to the hospital. There he should remain until the symptoms disappear. Additionally, you must follow a diet. It is developed individually. It depends on the degree of damage to the liver and gastrointestinal tract. Additionally, it is recommended to take ascorbic acid. It is required to improve the functioning of the liver and adrenal glands.
Anti-encephalitis immunoglobulin is used to combat the disease. The positive effect is noticeable within one or two days. After its administration, a decrease in temperature to normal is observed, meningeal symptoms become less pronounced, and the general condition of the patient improves. Sometimes anti-encephalitis immunoglobulin is replaced by:
- leukinferon;
- homologous polyglobulin;
- reaferon;
- serum immunoglobulin;
- ribonuclease.
Vitamins, sodium chloride and glucose are used to combat the effects of toxins. All substances are administered intravenously. For some types of pathology, additional treatment methods are prescribed. If the disease has not affected the cranial nerves and there is no disorder of consciousness, the doctor will prescribe the use of prednisolone. At the same time, a gentle diet and potassium salts are prescribed.
What is encephalitis?
What is encephalitis? This term is used in relation to the inflammatory process occurring in the substance of the brain. The causes and forms of its manifestation are very diverse. Let's look at them all:
- According to localization, the following types are distinguished:
- General cerebral.
- Focal - itself is divided into the following areas:
- Frontal lobe.
- Temporal lobe.
- Parietal lobe.
- Occipital lobe.
- The presence of affected areas of the meningeal membranes:
- Isolated.
- Meningoencephalitis.
- For reasons of occurrence:
- Infectious: viral, bacterial, fungal.
- Autoimmune – an attack of the immune system on its own cells. This includes demyelizing encephalitis and leukoencephalitis.
- Post-vaccination (post-vaccination) – a complication after vaccination.
- Toxic – severe poisoning.
- According to the area of the affected brain, the following types are divided:
- Cortical.
- Subcortical.
- Stem.
- Cerebellum.
- According to flow forms:
- Spicy.
- Chronic.
- Other types of encephalitis:
- Epidemic (Economeau's disease, encephalitis A, lethargic) - provoked by a filterable virus transmitted by airborne droplets.
- Tick-borne (spring-summer, taiga) is an infection transmitted through ticks. Forms of development of this type: Febrile - fever, mild neurology.
- Meningeal - pain in the head, stiff neck, inability to straighten the legs when lying on the back.
- Meningoencephalic – fever, delirium, hallucinations, twitching, paresis, psychomotor agitation, epileptic seizures. Deadly form.
- Poliomyelitis - atrophy and paralysis of the muscles of the arms and neck: the head hangs, the arms fall.
- Polyradiculoneurotic – damage to peripheral nerves, their tingling and numbness.
- According to the development mechanism, it happens:
- Primary is damage to the brain itself.
- Secondary - brain damage - a symptom or complication of another disease.
- According to the presence of complications:
- Complicated.
- Uncomplicated.
go to top
Diseases that can be transmitted through a tick bite
There are also a number of diseases that ticks can carry. And if they bite, they can infect a person.
- Viral encephalitis, which is described above.
- Lyme disease (in other words, tick-borne borreliosis) may occur. It is of a chronic nature. However, in case of illness, a person is not contagious to others.
- Tick-borne typhus. In medicine, this is a whole complex of diseases that are caused by spirochetes. Not typical for our latitudes.
- Q fever. The disease is transmitted from animal to human by the same tick, which bites both victims.
- Hemorrhagic fever (common in Crimea).
Biology of Ixodidae
Ixodid ticks (pasture or forest ticks) are small arachnids that spend part of their life on the host’s body and feed on the blood of humans and animals. Ticks have a small head, eight legs, a small body, and a sharp harpoon-shaped proboscis for sucking blood. They orient themselves using the organs of touch and smell, and are able to sense a warm-blooded organism at a distance of up to 10 meters.
The most voracious individual is the female, because she needs nutrients for the development of eggs. Having sucked blood, the female increases in size a hundred times, becoming like a large shiny droplet. But be careful - an awkward movement, and the abdomen may burst, and its contents may splash into the eyes or a wound on the body. Males are not so bloodthirsty - after all, they do not need to take care of their offspring, they just need to feed themselves and fertilize the female.
From an epidemiological point of view, female ticks will be the most dangerous. After sticking for several days, they, together with saliva, inject a large number of viral particles into the human blood.
Why are ixodid ticks dangerous for humans?
Horror stories about ticks have a real basis - you can become infected with such a terrible disease as borreliosis or encephalitis. How can a person become infected? It is enough to take a walk in nature, pick up a tick, the bloodthirsty creature will find a secluded place, pierce its head almost completely into the skin and drink and suck for ten to twelve days, if a person does not notice it earlier, or accidentally catches it, tearing off its bloody abdomen. But the job has already been done - the tick bite has triggered the mechanism of infection transmission.
True, not every close encounter with a tick can cause encephalitis; the animal must have this insidious active virus in its saliva. The number of bites from an encephalitic animal increases the risk of developing the disease, although sometimes one bite is sufficient. Timely vaccination and a sufficient level of antibodies are a guarantee that the disease will not develop. How ticks become infected, where the virus comes from, and the transmission mechanism is studied by the science of epidemiology.
How do ticks become infected?
The source of infection is mouse-like rodents (shrews, voles, shrews), moles, hares and other small animals. Epidemiologists have counted more than 200 animals that are natural reservoirs of the encephalitis virus. Natural foci of tick-borne encephalitis are the taiga regions of the Far East, the forest zone of Russia from Kaliningrad to Sakhalin.
The disease is characterized by spring-summer periodicity, with an increase in the activity of ticks, the number of infected people increases. Ticks become infected by feeding on the blood of these animals, often change 3-4 hosts, and have a complex life cycle:
- Fertile females lay a huge number of eggs, from which larvae develop.
- The larvae live on small animals, birds, and sometimes on large insects; before the onset of the next phase of development, they fall to the ground, turning into a nymph.
- A nymph is an immature tick that lives on large animals and humans; when fed, the nymph molts and also falls to the ground.
- After a while, the adult crawls onto blades of grass, sits with its paws spread, and waits for its “prey” - the owner.
Tick life cycle diagram
Adults live 3–4 months, die by autumn, only immature females overwinter.
Other forms of encephalitis
influenza encephalitis appears (another name is toxic-hemorrhagic encephalitis ). With this type of brain inflammation, neurological symptoms appear against the background of flu-like symptoms. The main symptoms of encephalitis are severe headaches, nausea, and dizziness . When moving the eyeballs, a person feels pain. Possible manifestations of pain in the back, muscles of the arms, legs, as well as at the exit points of the trigeminal nerve. Influenza encephalitis can cause anorexia and sleep problems.
Meningoencephalitis is characterized by paresis, paralysis, coma, and in some cases epileptic seizures may be observed . With acute encephalitis , which can develop approximately 3-5 days after the patient develops a rash, damage occurs mainly to the white matter, both the brain and the spinal cord. With the development of this form of encephalitis, the condition of patients worsens again, and body temperature increases. Symptoms of encephalitis in this case may be different. Thus, some patients complain of a general manifestation of weakness, drowsiness, which can lead to a coma. Other patients experience delirium and impaired consciousness, epileptic seizures, and may periodically remain in an agitated state. Paralysis, hemiparesis, damage to the facial and optic nerves are possible.
Encephalitis also occurs in patients with rubella and chickenpox. In this case, symptoms of the disease appear on days 2-8. Damage to the nervous system occurs. The onset of encephalitis is acute: paralysis, paresis, epileptic seizures, and hyperkinesis are possible. Coordination may be impaired, and in some cases the optic nerves may be damaged.
The herpes virus can trigger the development of herpetic encephalitis . With this disease, damage occurs to the cerebral cortex and white matter. Focal or widespread necrosis gradually develops. This type of encephalitis is considered a slow-growing infection due to the fact that the virus can persist in the body for a long time. The route of entry of the virus into the nervous system is hematogenous, as well as through the perineural spaces. The acute form of the disease is characterized by high body temperature, epileptic seizures, vomiting, headache and other symptoms. If necrotizing encephalitis develops, then catarrhal phenomena are present. After seven days, a sharp rise in body temperature occurs, and symptoms of damage to the nervous system, characteristic of other forms of encephalitis, appear. This form of encephalitis is especially severe in children.
The definition of “ polyseasonal encephalitis ” is used to define a group of encephalitis that has an unclear etiology. Most often, with this type of disease, cerebellar, brainstem, and hemispheric syndromes appear. With cerebellar syndrome, coordination and gait are impaired, and other disorders occur. With stem syndrome, changes in the functions of the facial, oculomotor and abducens nerves occur. Vestibular and bulbar disorders may occur.
Epileptic seizures, paresis, paralysis are a feature of the hemispheric syndrome. Serious disturbances of consciousness are also possible.
, toxoplasmosis encephalitis may occur . In its acute form, body temperature increases, pneumonia, conjunctivitis, myocarditis, skin exanthema, pharyngitis .
Are there other carriers?
The causative agent of tick-borne encephalitis can be transmitted not only by ticks. Another source of infection is wild animals and birds. Long-term asymptomatic viremia is sufficient for the spread of flavivirus through blood-sucking by a non-infectious parasite. Such viremia occurs in chipmunks, hares, squirrels, rats, foxes, and hedgehogs. Of the birds, carriers of the causative agent of tick-borne encephalitis are black grouse, wood grouse, hazel grouse, and woodpeckers. Birds, becoming infected and becoming guardians of the infection, can spread not only the virus itself, but also ticks. This is how new natural sources of disease are formed.
Treatment
When a patient is identified with TBE, his hospitalization in an infectious diseases hospital is mandatory. It is necessary to observe bed rest for the first time until signs of intoxication or severe neurological disorders disappear. Sometimes such patients may require observation in the intensive care unit, especially if breathing and consciousness are impaired.
The diet should be balanced, rich in vitamins from groups B (to improve the function of the nervous system) and C (antioxidant, also has antitoxic properties, daily dose up to 1000 mg).
How to act
When a person is bitten by a carrier of the causative agent of encephalitis, the first step is to remove the insect. You can do this yourself, but it is best to go to the nearest emergency room.
You need to pull out the insect as quickly and carefully as possible, because if you accidentally crush it, the risk of infection will increase significantly. It is noteworthy that in a place where human skin is different in thickness, the tick will be able to achieve its goal much faster.
If it was not possible to remove the tick completely and part of its body remains under the skin, you need to “arm yourself” with a needle, having previously disinfected it, and remove the “splinter”. The wound should be lubricated with a diamond solution or iodine.
When bitten by a carrier of the causative agent of encephalitis, the prognosis may be favorable. Absolute recovery occurs in the second or third week. Sometimes a person may suffer from neurotic disorders, paresis and atrophic paralysis.
What complications should you be wary of?
- edema-swelling of the brain followed by respiratory arrest and death. May develop approximately on days 4-6 of illness;
- hemorrhage in the brain against the background of complete well-being;
- gastrointestinal bleeding in the “milk” form;
- development of Kozhevnikov epilepsy, which persists for life;
- infectious-toxic myocarditis;
- Landry type malignant paralysis.