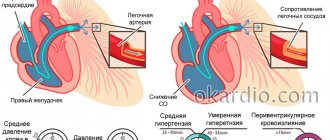
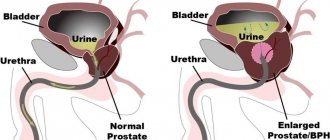
BPH (benign prostatic hyperplasia, Prostate adenoma) is a benign growth of gland tissue, an increase in its volume. The enlarged gland compresses the urethra passing through it, causing urination problems - this is the main symptom of the disease.
Benign prostatic hyperplasia is detected in 20% of men 40 years old, 70% - 60 years old, 90% - 80 years old. The main reason for the development of BPH is a change in the hormonal background of a man (a decrease in testosterone levels with age).
Prevalence in the world
Perhaps adenoma is one of the most common diseases in men who are emerging from a young age. So, in Russia, almost every second man over 45 years old is diagnosed with this disease, in the USA - every third.
If a man is lucky enough to live to the age of 80, then the incidence rate corresponds in this case to a year of life, that is, 80% of men at this age suffer from adenoma. It is generally accepted that at the age of 60 years, 44% of men have certain complaints and symptoms, and according to morphological studies, some signs occur already by the age of 30.
Throughout the civilized world, the incidence is gradually increasing, but it is due to the fact that men have begun to live longer. The incidence of prostate adenoma increases at a rate of approximately 2% for each year of life. It is interesting that among the Negroid race this disease is less common than among the white population, but among residents of China and Japan, on the contrary, prostate adenoma is diagnosed more often than in Europe.
Stages of development
There are several stages in the development of the disease, at each of which the corresponding symptoms will appear:
- The first degree of the disease is characterized by impaired urination. Urine is retained in the bladder, hence the frequent urge to go to the toilet.
- Second degree - urine comes out in a thin stream, and it is not completely eliminated, so there is discomfort after urination. This phenomenon provokes kidney disorder.
- At the third stage of the disease, paradoxical ischuria develops - overcrowding of the bladder in the absence of the urge to urinate. Urine is constantly dripping from the urinary canal, as it is significantly dilated. This condition is life-threatening.
Causes and development
The prostate gland is heterogeneous in structure. It has three different zones that perform different functions. In some of these zones, nodular centers are formed, in which the structure of the epithelium is disrupted. Gradually, this tissue begins to increase in volume, compressing the urethra, which passes through the prostate gland. As a result, the urethra is deformed and its angle of inclination changes. And most importantly, the lumen of the urethra narrows. Instead of being round, it becomes flattened and slit-like.
As a result, the so-called infravesical obstruction is formed. If we translate this complex term into Russian, then everything is very simple: this is “subvesical compression.” After all, the prostate lies under the bladder, and it is there that the urethra is compressed by hyperplastic prostate tissue.
Important risk factors for prostate hyperplasia are:
- a decrease in the production of male sex hormones in the testicles with age, as well as an increase in the concentration of estrogen in the blood plasma;
- stimulation of changes in the epithelium causes an increase in the blood level of the enzyme 5-alpha reductase, which affects the conversion of testosterone;
- One of the most important risk factors for the development of prostate adenoma is prostatitis. Chronic, advanced and untreated prostatitis almost often leads a man to a diagnosis of benign prostatic hyperplasia, and this is in the best case. In the worst case, it could be urosepsis (you can read about it in this article) or.
Treatment of BPH
Before proceeding to intensive therapy, it is necessary to undergo diagnostics, which, for inflammation of the prostate gland, includes transrectal ultrasound to measure the prostate and identify the features of its structure, cystoscopy for internal examination of the bladder and urethra, uroflowmetry in the form of a series of tests. The transrectal method can accurately record the volume of the inflamed prostate gland and finally determine the diagnosis. General doctor's recommendations for BPH are presented below:
- At the initial stage, it is necessary to restore systemic circulation and ensure the natural outflow of urine through medication. Additionally, give up bad habits, eat right and lead an active lifestyle.
- At the second stage, the clinical picture becomes more complicated and surgical treatment may be required. If the doctor suspects urethral obstruction, surgery followed by a rehabilitation period cannot be avoided.
- The third stage of prostate BPH is complicated and can only be treated with radical methods. Conservative therapy is ineffective. Recommended resection of the prostate gland requires a long rehabilitation period.
Medication
If the prostate gland is inflamed and hurts, you need to consult a urologist. The specialist, after studying the patient’s complaints and instrumental diagnostics, recommends gentle conservative methods with a sustainable therapeutic effect. More often, doctors prescribe representatives of the following pharmacological groups:
- 5-alpha reductase blockers recommended for the patient with an enlarged prostate volume of more than 40 ml: Finasteride, Proscar, Dutasteride, Avodart;
- alpha blockers to reduce the severity of anxiety symptoms and acute pain syndrome: Terazosin, Doxazosin, Tamsulosin;
- Phosphodiesterase inhibitors effectively relieve symptoms of erectile dysfunction: Tadalafil, Cialis.
Surgical
If the third stage of BPH of the prostate gland is diagnosed, what it is is determined by a detailed diagnosis. Effective treatment is carried out exclusively by surgical methods, the main goal of which is surgical removal of the adenoma and excision of the affected tissues involved in the pathological process. Here are the operations urologists prescribe in the hospital:
- Removal of BPH using the transurethral method involves instrumental excision of prostate tissue located along the urethra and compressing its lumen.
- Adenomectomy. The operation is performed under general anesthesia for large prostates and is accompanied by a long rehabilitation period.
- Prostatectomy. Partial excision of affected tissue with minimal side effects.
- Laser ablation causes compression of the urethra due to high heat and further “shrinking” of the prostate tissue surrounding the urethra.
Non-operative treatment methods
Conservative, minimally invasive and alternative methods of intensive therapy are highly effective only at the early stage of BPH of the prostate gland - what it is and how to act, the urologist will tell you in more detail after the examination. Here are the most popular procedures:
- cryodestruction;
- thermotherapy;
- transurethral needle ablation;
- introduction of prostatic stents into the area of narrowing;
- balloon dilatation of the prostate.
Postoperative period
Treatment for BPH is long-term even after surgery. The rehabilitation period includes proper nutrition, an active lifestyle and constant medical supervision. For example, the patient will have to completely eliminate fatty, salty and spicy foods, alcohol, while enriching the daily diet with fiber. In addition, you need:
- abandon harmful production;
- exclude physical activity;
- leave bad habits in the past;
- abstain from sexual intercourse for a month;
- Do not drive a car for 3–4 weeks.
Classification
There are many classifications of adenoma. But the simplest can be considered clinical, which is formed depending on the patient’s condition and complaints. There are three simple steps:
- compensation stage;
- incomplete compensation;
- decompensated stage.
The key mechanism here will be a gradual increase in bladder outlet obstruction, that is, compression of the urethra under the bladder. The bladder, of course, tries to overcome this obstacle. The bladder muscle, or detrusor, which contracts beyond our will and is controlled by the autonomic nervous system, resists with all its might. But, in the end, his strength ceases to be enough, and the contractility of the detrusor decreases.
All these stages are well reflected in three figures.
- The first stage is interesting because the bladder muscle becomes hypertrophied, it seems to be pumped up (after all, it is periodically loaded, like an athlete in the gym), and overcomes the obstacle.
The bladder empties completely, there are no problems, but there are already signs of bladder hypertrophy;
- The second stage is characterized by a constant load on the bladder muscle.
There is a depletion of his muscle strength, and, on the contrary, thinning of the muscle layer develops, hypertrophy gives way to hypotrophic changes. Imagine that an athlete trains around the clock, without rest, for many months in a row! Already the detrusor does not have enough strength to completely empty the bladder, and gradually more and more urine accumulates there, which is called residual urine. Let us remind you that normally there should not be more than 50 ml of liquid.
At this stage there are already symptoms of chronic urinary retention. As a result, the hydrostatic pressure inside the bladder gradually increases, and this leads to the fact that the outflow of urine from the kidneys begins to become difficult. But this does not happen immediately. At first, urine from the bladder, which cannot go down, goes “where it is easier.” In other words, it is thrown up into the ureters. The so-called vesicoureteral reflux occurs. The ureters gradually begin to stretch, and the pressure in them also gradually increases until it rises to the pelvis.
Already at this stage of the disease there may be signs of chronic renal failure. In addition, the constant presence of urine in the bladder is an excellent environment for the development of pathogenic microflora, the occurrence of cystitis, urinary infection, as well as conditions for the formation of stones in the bladder.
- What happens at the third stage? The muscle that pushes urine out, the detrusor, completely atrophies, and instead of completely emptying the bladder, as it should normally, it resembles a rag and does not work at all.
At this stage, the patient experiences total and complete urinary retention. A whole liter of urine or even more can accumulate in the bladder, all tissues of the bladder are stretched, and due to high pressure, urine begins to drip through the obstruction, and finally squeezes through the compressed urethra. This phenomenon is called “paradoxical ischuria”. Why paradoxical? Because there is urinary retention, but the urine, even drop by drop, comes out.
But a much more dangerous situation is that in an attempt to find the zone of lowest hydrostatic pressure, urine rushes upward. At this stage, the ureters and pyelocaliceal system of the kidneys have long been deformed and swollen. Bilateral hydroureteronephrosis develops. All this leads to obstructive nephropathy, and then to the progression of chronic renal failure, which ultimately leads to the death of the patient.
Stages of BPH
The disease develops slowly, gradually. Urologists distinguish several stages.
Initially, the appearance of a sluggish stream during the act of urination and the need to make efforts during migration are noted. At night, the number of visits to the restroom increases. This is the so-called compensation stage.
At the time of subcompensation, there is a feeling that the bladder is not completely empty after urination. The stream of urine is even more sluggish, sometimes even intermittent. An increase in the size of the prostate affects even the rectum located anteriorly. It squeezes it, causing a feeling of incomplete bowel movement and a false urge to defecate.
Decompensation of the condition leads to a pronounced worsening of the obstruction. There is no longer a stream, urine is released in droplets. Voluntariness and control over urination are lost. Due to urinary retention, chronic renal failure develops. Severe weakness and fatigue increase.
The patient is losing weight. Appetite and need for fluid intake decrease. Confusion may occur. Decompensates cardiovascular and endocrine diseases. Without treatment, the outcome is unfavorable - uremic coma and death.
Symptoms
What are the symptoms of prostate adenoma? There are two sets of symptoms.
The first is signs of bladder outlet obstruction:
- “you have to wait”, long delay before urinating;
- there is an obstacle after the bubble, so the stream flows thin and sluggish;
- urination is prolonged, intermittent, there is actual difficulty in emptying.
The further the pathological process has progressed, the stronger the feeling of an unemptied bladder will be. Then symptoms of urinary retention will appear, as well as paradoxical ischuria.
The second group of symptoms is called irritative. Translated from Latin, irritation is irritation. Everyone knows how unpleasant it is to hold urine for a long time, but now imagine that such imperative and uncontrollable urges appear quite often when the bladder is stretched, and become constant companions. As a result, the urge to urinate at night appears, it becomes more frequent, painful, and the greater the residual volume of urine, the more pronounced the unpleasant symptom of a feeling of heaviness in the lower abdomen, and pain appears.
Stages of the disease
There are 3 degrees of hyperplasia - compensated, subcompensated and decompensated. Their features:
- The first stage varies from 1 year to three. Thanks to the study, the enlargement of the prostate gland is determined; it itself has clear boundaries. The median sulcus can be easily palpated during a rectal examination. It is painless; in a sitting position, the man is also not bothered by discomfort. The main symptom of this phase of development is rare episodes of urinary retention, urges mainly at night.
- The second stage lasts less than six months. It is characterized by spontaneous release of urine immediately after the bladder overflows. The growth of the seal leads to compression of the urethra. The stream of urine becomes intermittent and sluggish. Urine sometimes contains blood; more often there are no red blood cells, but the secreted masses have an unnatural cloudy tint. Thanks to the study, it is possible to determine the enlargement of the prostate, the absence of clearly defined boundaries, and compression of the urethra. During diagnosis, the presence of residual urine is detected.
- The third stage is characterized by severe symptoms. Excessive distension of the bladder is caused by a constant and significant amount of residual urine. Its stagnation leads to infection and secondary kidney damage (up to failure of this paired organ). The prostate gland is significantly enlarged, which is determined during rectal and hardware examination. If the tumor is malignant in origin, severe hematuria and weight loss are observed.
At the compensated stage of hyperplasia, patients rarely seek medical help. The reason is mild symptoms of the disorder.
Diagnostics
As you can see, prostate adenoma is a disease with clear and understandable complaints, but a full examination and laboratory and instrumental studies are still necessary.
- When initially contacting a urologist, the patient is asked to keep a diary of urination for some time, which must necessarily reflect the number of urinations per day, as well as the volume of urine released.
- Then he undergoes a routine urological examination, with a mandatory digital rectal examination of the prostate.
- Routine tests are taken: a general urine test, a biochemical blood test, which must contain creatinine and urea in order to assess kidney function. This is very important, especially in the later stages of the disease.
- For prostate adenoma, PSA, or prostate-specific antigen, is taken to rule out prostate cancer. Let us remember that normally the PSA value should not exceed 4 ng/ml.
- After this, the instrumental examination begins. An ultrasound of the bladder is performed to fully assess its size and the presence of stones. They find out how much residual urine is in the bladder. Be sure to evaluate whether there is dilation of the renal pelvis, calyxes of the kidneys and ureters, that is, they conduct a complete ultrasound diagnosis of the urinary system and kidneys.
- An ultrasound scan of the prostate using a rectal probe is mandatory. This allows you to determine not only the shape of the gland, but also the boundaries and size of the hyperplastic part itself, as well as the direction in which it grows.
In the figure below, the arrow shows how the prostate adenoma grows inside the bladder, and this is clearly visible. That is, it not only squeezes the urethra under the bladder, but can also grow wherever it pleases, disrupting the shape of the prostate. (A – anterior, frontal projection, “full face”, B – lateral, sagittal projection, “profile”).
It may be recalled that according to ultrasound data, the prostate gland is considered enlarged if its linear dimensions extend more than 4 cm. Its volume should not exceed 25 cm³. Using a transrectal sensor during color Doppler ultrasound, you can evaluate blood circulation parameters in the prostate gland.
- Patients also undergo uroflowmetry. This beautiful name hides the study of urinary flow rate and volume. A threshold of 15 ml per second is considered critical, and if less urine is released, this means that: either there is already bladder outlet obstruction, or the contractile function of the bladder is insufficient. How to distinguish which of the two options a patient has? That's right, measure the pressure inside the bladder!
- For this purpose, cystometry is performed. This is what allows you to make the final decision. If cystometry shows low pressure, then the contractile function of the detrusor is to blame, and if the pressure is normal, then urine flows poorly due to an enlarged adenoma and bladder outlet obstruction. It is not difficult to understand that if cystography showed low pressure in the bladder, then this is unfavorable, since it indicates that the detrusor has already exhausted its compensatory ability, its hypertrophy has changed to hypotrophy, and, most likely, the patient is in the second stage.
- You should not think that this is where the diagnosis ends. It is imperative to evaluate renal function, conduct an MRI, perform excretory urography, confirm or refute the diagnosis of hydroureteronephrosis, as well as vesicoureteral reflux.
- Finally, at the very end of the diagnosis, urethrocystoscopy is performed. With the help of an endoscopic technique, it is finally determined how deformed the urethra is, what changes there are in it, whether there are expansions, diverticula, stones, and just in the process of urethrocystoscopy it is already possible to perform some therapeutic manipulations. But this will be discussed in detail later.
Nonspecific risk factors for the development of BPH in men are also identified
Among them are the following:
- nicotine abuse (smoking) due to its effect on alpha-adrenergic receptors;
- genetic predisposition, which is not realized in everyone;
- increased blood pressure;
- diabetes mellitus and other metabolic disorders;
- features of eating behavior, tendency to obesity, metabolic syndrome;
- age over 40-50 years;
- diseases accompanied by decreased liver function;
- hyperestrogenism, hyperandrogenism and other hormonal changes.
In the presence of an existing benign prostate adenoma, urologists identify the so-called progression factors shown in the table.
| BPH progression factor | Meaning |
| the total value of points assessing symptoms on the international scale 1 PSS | more than 7 |
| concentration of PSA or prostate-specific antigen in the blood by ELISA | more than 1.4 ng per milliliter |
| prostate volume according to the results of Tr-ultrasound | more than 30 cubic meters cm |
| the maximum value of the rate of bladder emptying according to the results of a uroflowmetric study | More than 12 milliliters per second |
If one or more of the listed signs are detected, the risk of disease progression increases almost 4 times, which subsequently dictates the need for surgical treatment.
Treatment
Could it be that a patient with an adenoma is observed but not treated? Can there be prostate adenoma without surgery, and even without pills? Yes maybe.
If a patient’s complaints have almost no effect on the quality of life, if according to ultrasound data the volume of the prostate gland does not exceed 30 cubic centimeters, then they simply go to the urologist for a follow-up examination. If the disease progresses, then treatment of prostate adenoma with drugs is prescribed.
Medication
Usually, if prostate adenoma is diagnosed at the first stage, then the effectiveness of drug therapy is 70-80%. As a result of treatment, urinary retention is prevented, urine passage is improved, and treatment is aimed at eliminating bladder outlet obstruction. Since there is no one, ideal drug, treatment of prostate adenoma comes down to prescribing the following drugs:
- adrenergic blockers: Prazosin, Tamsulosin;
- 5-α reductase inhibitors: this is a drug such as Finasteride. It is also used to treat alopecia, or androgenic baldness in men, as it regulates testosterone metabolism;
- prevention of urinary infection: antibiotics are prescribed.
Surgical
Moving on to operations for prostate adenoma, we should definitely talk about minimally invasive interventions.
Stenting
So, one of the simplest solutions is to simply place a stent or endoprosthesis endoscopically in the very section of the urethra inside the prostate that is narrowed. Thus, the patency of the urinary tract is restored, and everything seems to be fine. The urethra is no longer compressed, but such stents are installed only if there is an absolute contraindication to surgery. This may be severe renal failure, the presence of diabetes mellitus, and other concomitant pathologies.
Why does urologists not like this method, which seems to be the best? There seems to be no obstacle, and the treatment of prostate adenoma is completed, since there is no more bladder outlet obstruction. The fact is that the risk of complications is very high. Constant contact of the prostate under high pressure with the stent makes it possible to develop infections; quite often the patient feels severe pain, and one of the side effects is clogging of the stent with uric salts, the so-called encrustation.
The figure shows an x-ray where the endoprosthesis is located in the prostatic urethra. Of course, soft tissues are not visible, but the endoprosthesis is clearly visible, since it must be radiopaque. Pay attention to the upper edge of the endoprosthesis. It is twisted into a spiral, which is fixed in the bladder.
Thermal destruction
Further, there are methods called thermal. If the tissue of the hyperplastic area is exposed to either high or low temperature, then capillary blood circulation is gradually disrupted, adrenergic receptors die, epithelial proliferation ends, and finally tissue death and sclerosis occurs. So, the result is a stable area that will no longer put pressure on the urethra, and, most importantly, will not grow.
Such methods are used by introducing sources of extreme temperatures into the urethra, or into the rectum at the level of the prostate gland. This can be thermal radiation, radio frequency, ultrasound, or laser exposure to the prostate adenoma. Among the titles:
- transurethral hyperthermia;
- transurethral thermal destruction;
- transurethral radiofrequency thermal influence, and so on.
Temperatures are used that gradually increase from 40 to 120 degrees. Advantages should be given to ultrasonic destruction of the adenoma, when the waves are focused using a special computer navigation program. As a result, only the necessary points are destroyed, which are heated to 120 degrees, and the surrounding tissues are not affected.
Operations
But sometimes all these methods are not applicable, and real surgery is needed. It is used when there is no effect from medications, and bladder outlet obstruction increases, with all the unpleasant symptoms described above.
Also, indications for surgery are the gradual accumulation of a large amount of urine in the bladder, or acute urinary retention, which becomes frequent. It is necessary to operate if a focus of infection is formed, if stones are constantly forming, or if upper symptoms arise: threatening hydronephrosis and progression of renal failure.
As usual, in any branch of surgery, there is a radical method, which cures and completely solves the problem, and a palliative one. It does not solve the problem, but it significantly changes the quality of life. Palliative interventions are used when there are obstacles to radical treatment. These are concomitant diseases, very old age of the patient, and so on. In this case, the gland is preserved and an epicystostomy is applied. In this case, urine is removed from the bladder directly through the anterior abdominal wall to the outside.
The second option is TUR of prostate adenoma, or transurethral resection. Part of the prostate gland is removed, and there are many types of this operation, for example, laser vaporization, electroincision, and so on.
In some cases, with transurethral resection, it is possible to completely remove not only the prostate adenoma, but also to gradually remove the entire gland in parts through the urethra, but only if its volume does not exceed 80 cubic centimeters. If there is even more iron, then surgeons have to work for a long time, and the risk of significant blood loss increases.
The surgical intervention consists of inserting a resectoscope through the urethra, and the prostate, in simple terms, is “cut into pieces” and removed through the resectoscope tube.
The illustration shows a schematic TUR - electrical resection. Initially, we went for resection, but circumstances made it possible to expand the scope of the intervention, and as a result, it became possible to completely remove the prostate gland. In this case, it will no longer be a resection (removal of part of an organ), but a transurethral prostatectomy (removal of the entire organ).
With prostate adenoma, there are emergency indications for surgery, and, first of all, acute urinary retention and massive urethral bleeding, which is called profuse macrohematuria.
Methods for treating prostatic hyperplasia
There are two main approaches to treatment: conservative therapy (medicines, minimally invasive techniques, folk remedies) and surgical intervention.
Drug treatment
If the pathological process was identified at the initial stage of development, medications are prescribed that slow down the growth of the tumor. They also relieve symptoms that accompany the proliferation of prostate tissue.
For prostatic hyperplasia, the following medications are effective:
- Alpha adrenergic blockers. These drugs help relax the muscle tissue of the prostate, reduce the pressure that areas of overgrown tissue exert on the urethra, and facilitate the passage of urine. Alpha blockers are effective for sluggish, intermittent and painful urine flow. This group of medications includes Cardura, Urocard, Artesin, Omnic, Terazosin.
- 5-alpha reductase inhibitors. Drugs of this pharmacological group block the action of enzymes that stimulate the growth of tumor cells. These medications remain the only means that can non-surgically reduce the extent of hyperplasia and get rid of adenoma. This group includes Prosteride, Propecia, Finasteride.
- Herbal medicines are products that have a natural composition and help at the initial stage of the development of the disease. To a greater extent, they are preventive; they should be taken when the first signs of urination problems appear. Popular drugs in this group are Prostamol Uno and Tykveol.
Drugs for symptomatic therapy can also be used. This:
- Antibiotics (Gentamicin). They are required in case of bacterial infection.
- Antiseptic suppositories (Norfloxacin, Rifampicin). The products ensure the neutralization of pathogenic microorganisms.
- Medicines to eliminate erectile dysfunction that can occur with prostate adenoma (Tadalafil).
Minimally invasive methods for reducing prostate size
You can reduce the size of the prostate gland using the following procedures:
- Embolization of prostate arteries. The essence of the method is to block the arteries that supply blood to the enlarged prostate. As a result, the iron decreases in size.
- Laser therapy. In this case, a beam of laser beams is directed at the prostate, as a result of which the liquid in the adenoma tissue evaporates and the blood vessels are sealed.
- Cryotherapy. Prostate cells are exposed to extremely low temperatures using liquid nitrogen. As a result, adenoma tissue is destroyed.
- Ultrasound treatment. High-intensity ultrasound heats and destroys adenoma tissue.
Traditional methods of treatment
To reduce the severity of symptoms of prostatic hyperplasia, use the following folk recipes:
- Pumpkin seeds with honey. Take 500 g of peeled seeds and mix with a glass of natural honey. The resulting mass is rolled into balls and placed in the refrigerator for 2-3 hours. Eat 2-3 balls before meals.
- A decoction of chestnut shells. You need to take the peel, grind it and take 3 tablespoons of the resulting mass, pour 600 ml of boiling water over them, and leave overnight. In the morning, the infusion is filtered and placed in a water bath. Keep it there until the volume of the decoction evaporates to 200 ml. Take the resulting mixture, cooled, 1 tablespoon 2-3 times a day, before meals.
- Burdock infusion. You need to take 12 g of crushed burdock root and pour two glasses of boiling water. Let it brew for 2 hours, strain. Take 4 times a day, half a glass.
- Cream with fir oil. You need to add 6 drops of oil to any hypoallergenic cream and mix. Lubricate the perineal area with this mixture before going to bed.
- Herbal composition. Take 15 g each of burdock root, white mistletoe, corn silk, pepper knotweed, and cinquefoil. Mix all ingredients, take 1 tablespoon of crushed mixture. Pour this amount into 200 ml of boiling water and cool. Take 3 glasses daily during the day.
- At the first signs of adenoma development, it is recommended to take a bath with juniper. Add 15 ml of juniper essential oil to a bath of warm water. The duration of the procedure is 15-20 minutes.
Surgical methods
Surgical intervention is required if the prostate becomes too large, as well as in the later stages of development of the pathological process.
You can remove an adenoma in the following ways:
- Open adenomectomy. The intervention is performed by opening the bladder under general anesthesia. After reaching the anterior wall of the bladder, it is dissected, then digital isolation is performed and the tumor tissue is removed. The removed fragments must be sent for histological examination. The advantage of such an operation is its radicality, complete removal of the tumor formation.
- Transurethral resection. This operation is performed most often, but is not suitable for cases of large tumors and if there is a risk of the adenoma degenerating into a malignant formation. The intervention is carried out as follows: using a special instrument, they reach the bladder through the urethra, determine the location of the tumor and remove it with a loop that is on the instrument. The adenoma is excised in parts.
- Transurethral incision. This method involves making an incision in the area of the prostatic urethra. This manipulation allows you to expand the lumen of the urethra. Transurethral incision is effective for small adenomas.
Surgeries can cause complications, the most common of which are bleeding, thrombosis of the veins of the pulmonary artery and lower extremities, and infectious and inflammatory processes.
Diet
If you have prostate hyperplasia, you should follow a special diet. It is necessary to remember these rules:
- mandatory complete exclusion of everything fried and fatty;
- refusal of alcoholic beverages;
- exclusion of all spices and seasonings (only lemon juice and dried herbs are allowed as a dressing);
- limiting the consumption of legumes and chocolate;
- refusal of fatty rich broths;
- exclusion of marinades, canned food, fish caviar;
- refusal of flour products, baked goods of any kind;
- exclusion of strong tea and coffee.
The following products are useful for adenoma:
- apples;
- oranges;
- strawberry;
- pumpkin;
- cucumbers;
- tomatoes;
- cauliflower;
- seaweed;
- seafood;
- chicken breast;
- vegetable oils: olive, sunflower, corn;
- vegetable soups;
- pumpkin seeds;
- nuts;
- bran;
- turkey meat.
You need to eat meals in small portions, 5-6 times a day.
An integrated approach to the treatment of prostate adenoma will help cope with the pathology and return the patient to a full life.
Complications and consequences
Currently, with a competent approach, effective treatment of prostate adenoma almost always leads to either stable remission or recovery, and the prognosis, in most cases, is favorable. After removal of a prostate adenoma, the patient is observed by a urologist, if we are talking about resection, so that there is no relapse and to eliminate the risk of hyperplasia elsewhere in the organ.
If the prostate gland is completely removed, then after recovery and elimination of the infectious process, the patient is seen by a urologist only if there was hydronephrotic transformation, reflux or signs of chronic renal failure, that is, complications of adenoma. If left untreated, the consequences of prostate adenoma can be catastrophic and lead to death. Firstly, this is acute urinary retention, which in some cases leads to pyelonephritis, sometimes urosepsis, and sometimes to rupture of the bladder with the development of urinary peritonitis.
That is why it is advisable for all men aged 45 years and older to visit a urologist at least once a year and simply undergo an examination.
Clinical picture
The severity of symptoms of prostate hyperplasia depends on the stage of development of the disease. In some cases, symptoms may be absent or may be so mild that the man does not attach any importance to them. Under such conditions, the disease develops uncontrollably.
The main signs of prostate adenoma include the following:
- weakness of the urine stream, which may be interrupted;
- frequent urge to empty the bladder, which are imperative;
- urinary incontinence (usually at night);
- feeling of incomplete emptying of the bladder;
- the need to strain the abdominal muscles in order to urinate (at more advanced stages of the pathological process).
In the presence of complications, symptoms become more pronounced. The man notes the following violations:
- traces of blood in the urine;
- burning when urinating;
- heat and pain in the bladder area;
- inability to empty the bladder;
- increased fatigue;
- weight loss.
In case of complications, the clinical picture of prostatic hyperplasia is supplemented by the symptoms of diseases such as pyelonephritis, cystitis, urolithiasis, acute or chronic renal failure.
Sources
- Vinarov A.Z. Drug treatment of patients with hyperplastic prostate gland. Abstract of the dissertation for the degree of Doctor of Medical Sciences, Moscow, 1999.
- Gorilovsky L.M. Epidemiology, risk factors for the development and biological course of benign prostatic hyperplasia. Benign prostatic hyperplasia. - Moscow, 1999.
- Portnoy AC Surgical treatment of adenoma and prostate cancer//L. 1989
Treatment of adenoma
The fight against prostatic hyperplasia is carried out on two fronts: drug therapy and surgical intervention.
It is worth noting that uroselective drugs themselves do not have a significant effect on the size of the adenoma.
Medicines “slow down” tumor growth.
When taken correctly, there is an effective elimination of the negative symptoms accompanying the growth:
- prostate muscles relax
- the process of urination does not experience serious difficulties
- there is less desire to visit the toilet at night
- the stream becomes saturated
- no need to strain
- the feeling of incomplete emptying of the bladder disappears
The conservative approach is based on the use of two groups of drugs: alpha blockers, 5-alpha reductase inhibitors.
The first includes a large list of drugs that allow you to relax the muscles of the bladder and prostate gland, thereby making urination “comfortable” for the patient. After a few days of use, the first results are visible, but side effects are possible: hypotension, tachycardia, dizziness.
These drugs include:
- alfuzosin
- terazosin
- doxazosin
- tamsulosin
- silodosin
The second group, called inhibitors, directs its therapeutic potential to hormones that promote enlargement of the prostate. These include: proscar, advodart.
The drugs act with some time lag. Noticeable results should be expected a few weeks after starting use. In some cases, there is a possibility of short-term side effects in the sexual sphere.
Let's take a closer look at two drugs: cardura and proscar.
Doxazonin, secondarily called cardura, helps improve the patient's urodynamics. Allows you to minimize the manifestations of characteristic signs of pathology. The set of positive qualities is extensive:
- eliminates tension from the muscles of the urethra and bladder neck
- in the presence of hypertension, stabilizes blood pressure
- in case of existing disorders, has a positive effect on potency
- has a high anti-sclerotic effect
Proscar, or otherwise finasteride. The effectiveness of the treatment is noted even with the impressive size of the adenoma.
Helps reduce prostate size by up to 20%.
The course interval is long, tangible results should be expected six months after the start of treatment.
Remember, the choice and prescription of a specific remedy should be made by a urologist; do not self-medicate.
Surgical methods of treatment
Here is a list of indications when surgery is inevitable:
- acute urinary retention
- blood in urine
- urolithiasis disease
- renal failure
The decision about surgery is made taking into account the individual characteristics of the body, concomitant diseases, and of course the age of the patient.
When in a forty-year-old patient, the proliferation of prostate tissue creates fundamental obstacles to a full life, it would be more advisable to consent to surgery. Otherwise, the body will spend the remaining years in “torment” and on pills.
At the same time, with an advanced age of the patient, there is usually a large bouquet of other diseases that can negatively affect the results of the operation. If signs of prostate hyperplasia first appeared at such an advanced age, then drug therapy seems preferable. In such situations, the issue is always resolved individually.
Now let's briefly look at the main types of operations.
- Transurethral microwave therapy - the method is effective for slight enlargement of the prostate. The operation lasts an hour, local anesthesia is used. A thin probe with a branch (antenna) is inserted into the urethra. Through it, high-frequency electromagnetic waves reach the prostate. The doctor adjusts the energy level, creating the necessary balance. Achieves the desired effectiveness and minimizes trauma to the prostate. Complications are possible, much depends on the experience of the surgeon and the characteristics of the patient’s body.
- Needle ablation - thin needles are inserted, which are then heated using radiofrequency waves. Necrosis of the overgrown prostate tissue occurs. However, the cells are destroyed gradually and are subsequently eliminated from the body naturally. The procedure is performed on an outpatient basis, with up to 6 punctures at a time.
- Plasma vaporization is a patient-friendly operation, since the time interval of exposure to the plasma instrument is insignificant. Water is “evaporated” from prostate tumor tissues by laser. Cells die, the size of the prostate decreases. At the same time, laser exposure causes coagulation (“sealing, sticking together”) of the surrounding blood vessels. The likelihood of bleeding during such surgery is minimized, and wounds heal faster. Temporary complications are possible: burning in the urethra, bloody urine, muscle spasms in the bladder.
- Transurethral resection - excess prostate tissue is “removed” by thermal treatment. The operation is appropriate for small volumes of the prostate and residual urine. A number of complications are likely, so the average hospital stay is two weeks.
- Open surgery (prostatectomy) is performed for large volumes (from 80 cubic cm) of the prostate gland. An incision is made in the pubic area, and excess glandular tissue is removed with a scalpel. The wound is then sutured and a catheter is inserted into the urethra.
- Embolization of prostate adenoma - blocking (“blockage”) of the arterial vessels supplying blood to the enlarged prostate. Left without nutrition, prostate tissue necrosis occurs and a decrease in size is observed. This operation is performed by an endovascular surgeon.
Rehabilitation and complications in the postoperative period
Complications after surgery may include
- problems with urination;
- urinary incontinence;
- bleeding and blood clots;
- infection;
- sexual dysfunction
- recurring problems such as urinary retention and UTIs
Problems with urination. Men may initially experience painful urination or difficulty urinating. These problems will gradually decrease, and after a couple of months, urination will become easier and less frequent.
Urinary incontinence. When the bladder returns to normal, men may experience some temporary problems with urinary control. The longer you had problems urinating before surgery, the longer it will take for your bladder to regain full function after surgery.
Bleeding and blood clots. Some bleeding is normal and should go away within a few days.
Scar tissue. One year after the initial surgery, scar tissue sometimes forms and requires surgical treatment. Scar tissue can form in the urethra and cause it to narrow. A urologist can correct this problem during an office visit by stretching the urethra. Rarely, the opening of the bladder becomes scarred and compressed, causing a blockage.
Sexual dysfunction. Some men may experience temporary problems with sexual function after surgery for benign prostatic hyperplasia. The duration of recovery of sexual function depends on the type of surgery for benign prostatic hyperplasia and the duration of symptoms before surgery.
Surgery rarely causes loss of erectile function. However, surgery for benign prostatic hyperplasia most often cannot restore the function that was lost before the procedure.
Prostate surgery can make men infertile by causing retrograde ejaculation—the reverse flow of sperm into the bladder.
Types of adenoma by growth form
Depending on the direction of tumor growth, hyperplasia has several forms:
- subvesical (tumor grows near the rectum). With this form, the patient often experiences discomfort not during urination, but during the act of defecation;
- intravesical (the formation grows in the direction of the bladder). Ingrowth of the prostate into the bottom of the bladder leads to deformation of the neck of the upper urethra;
- prevesical - expansion of the lateral parts of the prostate adjacent to the bladder.
Based on the form of tumor tissue growth, prostate adenoma is classified into 2 types.
Diffuse prostatic hyperplasia is characterized by a uniform increase in the organ during the development of the disease without pronounced foci. Adenomatous prostatic hyperplasia is characterized by the formation of nodules inside the prostate. There can be from one to several depending on the stage and course of the disease.
BPH is classified in different ways. You need to understand what each type means. Most often you can find a tumor divided into types according to its position in the prostate.
| Type of tumor | Location |
| Subvesical | Proliferation of tissue towards the rectum. |
| Intravesical | The tumor tends towards the bladder and compresses it. This causes irritation of the nerve endings and frequent visits to the toilet. |
| Retrotrigonal | Tissues grow under the triangle of the bladder, complicating the outflow of urine from it and pinching the mouths of the ureters. This type is often called nodal. |
Often, an adenoma develops several foci at once. The first two types of hyperplasia are often bilateral, that is, the tumor is symmetrical.
Another classification divides benign prostatic hyperplasia into types depending on the cells that formed the tumor.
| What tissue is the tumor formed from? | What is this? |
| Fibrous | The seals are separated from the connective tissue of the organ. Connective and stromal cells participate in the formation of adenoma. |
| Muscular (diffuse) | Muscle tissue cells grow, forming nodes. This type is extremely rare. |
| Glandular | There is a significant increase in the organ due to the division of its cells. Glandular hyperplasia develops slowly, often without obvious symptoms. It is usually discovered during a random routine examination or during the diagnosis of other diseases. |
It is possible to understand what type of disease is tormenting the patient by cytological examination of tumor tissue.
How to prevent disease
Prostate adenoma is a benign tumor of the stroma or glandular tissue. Chronic urinary retention leads to intoxication and the development of chronic renal failure. To avoid the development of pathology, it is recommended to carry out preventive measures.
These include:
- Complete cessation of smoking and alcohol.
- Balanced diet.
- Healthy lifestyle Regular exercise.
- If you have prostate adenoma, you can have sex. Regular sex life stimulates the gland.
Regular examinations by a urologist, especially after 30 years, will help to identify disorders in time and begin treatment in a timely manner.
Treatment methods
Currently, there are quite a few methods for treating prostate hyperplasia. The choice of a specific method is made by the doctor.
All methods are divided into several broad categories:
- drug therapy;
- surgical intervention;
- non-surgical techniques.
If the first manifestations of BPH appear, the patient is indicated for drug therapy. Herbal medicine and homeopathy can also be used. The goal of this treatment for prostate hyperplasia is to restore blood circulation in the pelvis. Thanks to therapy, it is possible to stop the development of formation and cope with urinary tract infections.
A patient with prostate hyperplasia needs to maintain an active lifestyle. Doctors also advise limiting fluid intake at night. Avoid drinking alcohol and spicy foods. Smoking is also prohibited.
To restore the correct balance of hormones in prostate hyperplasia, androgens are used. Along with this, it is necessary to treat complications of BPH - these include cystitis, pyelonephritis, and prostatitis.
In case of severe urinary retention, which may be a consequence of hypothermia or alcohol consumption, the person should be urgently hospitalized. In a hospital setting, he undergoes bladder catheterization.
Drug therapy for prostate hyperplasia is divided into two main categories:
- Medicines of the first type are used to reduce smooth muscle tone. Due to this, the compression of the canal decreases, and the flow of urine also improves. This category of drugs includes alpha-blockers, which can have a short-term or longer-term effect. These include drugs such as tamsulosin, doxazosin.
- Medicines of the second type are responsible for blocking the transformation of the male hormone into its active form. Thanks to this, its effect on tissues, including the volume of the prostate, is reduced. This also helps to reduce the compression of the canal. This group includes 5-alpha reductase blockers.
Herbal treatment for BPH is also very popular. To cope with prostate hyperplasia, products based on plant extracts are used - nettle, prickly pear, palm, African plum. In addition, traditional medicine is actively used. These include a composition based on mistletoe, aspen, toadflax, and hazel. No less effective for prostate hyperplasia are onions, burdock, and honey.
It is important to keep in mind that using herbal remedies to combat BPH does not bring very quick results. Thanks to the use of such extracts, one can only slow down the development of the abnormal process.
In difficult situations of prostate hyperplasia, it is impossible to do without surgical intervention. It involves performing an adenomectomy - this operation involves excision of a formation in the prostate.
There are several types of interventions:
- Open, which is also called transvesical adenomectomy. In this situation, access is through the bubble. Such operations are used in complex cases, since they are highly traumatic. Along with this, such an intervention allows you to completely cope with the problem and defeat prostate hyperplasia.
- Minimally invasive procedures that involve a minimal amount of intervention. In this case, the surgeon does not make an incision, but gets into the desired area using modern video endoscopic devices.
Depending on the equipment used and the tasks, transurethral resection, electrovaporization and prostate incision may be used. Laser vaporization of the gland is also sometimes indicated.
Non-surgical treatment options include the following:
- balloon dilatation – involves expanding the desired area of the prostate by inflating a special balloon;
- needle ablation;
- cryodestruction;
- microwave coagulation;
- placement of stents in the area of narrowing.
Prostate adenoma stage 3
Symptoms. This is an already advanced stage in the formation of pathology. Severe symptoms are observed, including:
- incomplete emptying of the bladder;
- pollakiuria;
- intense pain;
- frequent night awakenings.
Tumor sizes vary from 55 to 80 mm. These are large formations that disrupt the normal functioning of the entire excretory system.
Treatment. Therapy in this case is combined. Gentle surgical intervention using transurethral access is indicated (surgical instruments are inserted through the urethra to access the prostate gland). At the end of the operation, the tissues are necessarily sent to the laboratory for histological and morphological examination. If the patient first came to the doctor at this stage of prostate enlargement and the specialist has suspicions about the nature of the current process, open abdominal surgery is indicated (for example, if there is reason to suspect a malignant process). Before prescribing treatment, a thorough diagnosis is required.
Read more: Surgeries for prostate adenoma: types, advantages and disadvantages
In the postoperative period, the use of specialized medications is indicated. Transurethral resection is good because it does not leave postoperative scars and involves a short rehabilitation period. 1-2 weeks after the intervention, you need to start doing therapeutic exercises. For the entire period of therapy, a gentle regimen of physical activity and a fortified diet with a minimum content of animal fats are recommended.
Prevention of prostate hyperplasia
Diffuse prostate hyperplasia is not so much a serious as an unpleasant disease. But it is better to prevent its occurrence than to undergo treatment for a long time.
Preventive measures include:
- nutrition correction (reduction of “harmful” foods and dishes in the diet);
- regular physical activity;
- systematic walks in the fresh air;
- rejection of bad habits.
Patients at risk and all men over 50 years of age should visit a urologist at least once a year. This will help to promptly identify the danger and begin therapeutic measures.
Prostate adenoma stage 2
Symptoms. It is still considered the initial stage of the disease. Symptoms manifest sufficiently and become noticeable to the patient. It is difficult not to detect pathology.
Treatment. At this stage, conservative complex treatment using drugs from the following groups is indicated:
- Alpha adrenergic blockers. Promotes relaxation of the smooth muscles of the urinary tract and normal evacuation of urine. The following names can be mentioned: Omnic, Kardura, Kornam, etc.
- 5 alpha reductase inhibitors (see here). They stabilize the size of the tumor, preventing the process from developing further. First of all, these are Finasteride and its analogues.
- Herbal preparations. For the most part, they have an antispasmodic effect. Specific names are selected by the doctor.
At this stage, the size of the tumor does not exceed 30-40 mm. Taking diuretics is strictly contraindicated.
Despite the fact that the treatment tactics of the second stage involve conservative methods, in some cases the early stages are already difficult. For such clinical situations, urologists have developed informal criteria by which the need for surgery is determined:
One of the manifestations of prostate adenoma in the second stage may be calculi (stones) in the bladder
- Acute urinary retention.
- Formation of stones in the bladder.
- Decrease in urine flow intensity below 10 ml/s.
- Hematuria.
- Significant volume of residual urine (over 80-100 ml).
In the absence of contraindications, the use of minimally invasive instrumental treatment methods (which by their nature are not considered surgical) is allowed: vaporization, cryodestruction, electrocoagulation, etc.
Classification of the disease
There are four stages of development of BPH, which are divided depending on the location of the tumor, the degree of its enlargement, the level of urinary disturbances, and the effect of tumor growth on other organs.
The main stages of benign prostatic hyperplasia:
- Compensatory. It is characterized by a passive course; the man does not feel any serious changes in his well-being. Sometimes problems with urination may occur (usually at night), since the prostate gland is already slightly enlarged in size. The period of development of the disease is from 12 to 36 months.
- Subcompensatory. The connective tissue continues to grow, which is manifested by a frequent urge to urinate, while emptying does not occur completely. Unpleasant sensations occur in the lower abdomen, the risk of inflammation increases, incontinence is sometimes noted, and the urine becomes cloudy.
- Decompensation. This stage is considered advanced - maximum compaction of the bladder cavity occurs. A man loses the ability to empty himself completely, urine flows out spontaneously in small droplets. The urine becomes very cloudy and may contain blood. The patient often loses weight, experiences chronic fatigue and loss of strength, the patient's skin becomes pale, and the man often suffers from constipation. A persistent odor of urine is felt from the patient’s mouth and entire body. At this stage, urgent hospitalization is necessary - there is a danger of developing oncology and even death.
The fourth stage of BPH development is sometimes not distinguished as a separate type, since it is a continuation of the third stage, but in a more serious form. The patient is practically unable to empty himself, the passage of urine is difficult, intoxication begins, infectious foci arise, the patient’s condition is assessed as extremely serious.
In each degree, the manifestation of signs of the disease occurs with varying intensity. It is important to diagnose them in a timely manner in the early stages in order to counteract the development of complications dangerous to the body.
Prevention
There is no surefire way to stop BPH, but losing weight and eating a healthy diet that includes fruits and vegetables can help.
Staying active also helps control your weight and hormone levels.
Data from the Prostate Cancer Prevention Study suggest that a diet low in fat and red meat and high in protein and vegetables may reduce the risk of symptomatic BPH.
Additionally, regular alcohol consumption was associated with a reduced risk of symptomatic BPH. But! This should be interpreted with caution given the adverse effects of excessive alcohol consumption.
For more information on the methods and cost of treatment for benign prostate hyperplasia in Belgium, write to us using the feedback form or request a call back.
Complications
They appear when adenoma is advanced, when a sick person ignores the first signs and does not seek help.
Urinary retention in acute form - it is impossible to empty the bladder when it is full. Severe pain appears above the pubis, radiating to the penis and lower back, and a feeling of fullness. The pathology develops at stages 2-3 of the disease and requires immediate hospitalization. In an emergency, it is necessary to carry out catheterization or puncture of the bladder, otherwise acute renal failure and hydronephrosis will develop.
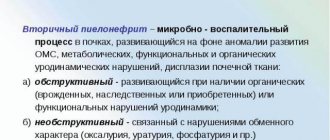
Inflammatory complications. Most often, cystitis develops - inflammation of the bladder mucosa, manifested by pain during urination, fever, and dysuric symptoms. Occurs as a result of the penetration of bacteria into a weakened bladder.
Secondary pyelonephritis is inflammation of the calyces and pelvis. Obstruction of the urinary tract, stagnation and development of vesicoureteral and pelvicaliceal reflux play a role in the pathogenesis of the disease.
Hematuria – with adenoma, blood appears in the urine. Bleeding can be obvious (macrohematuria) or hidden (microhematuria). In the latter case, the complication is detected by the results of a urine test. The cause of hematuria is the expansion of the venous wall of the bladder neck. Bleeding often develops after diagnostic and therapeutic procedures.
Urolithiasis - deposition of stones occurs as a result of stagnation. The physicochemical properties of urine change, which causes crystallization of its salts. With urolithiasis, blockage of the urinary tract with a stone may occur, which leads to acute urinary retention.
Causes of pathology
The risk group for prostate diseases includes all older men suffering from bad habits. Increase the chance of developing hyperplasia:
- smoking;
- alcoholism;
- sexual dysfunction – impotence or excessive activity;
- previous venereal diseases;
- poor quality nutrition (unbalanced diet, choice of products with chemical additives);
- lack of physical activity.
Negative factors also include heredity. There is a high likelihood of developing adenoma in those men whose fathers and grandfathers suffered from BPH. Similarly, it happens that if phimosis is observed in a parent, then it can be found in his son or grandson.
Even the absence of risk factors does not prevent prostate hyperplasia. Doctors believe that this disease can occur against the background of:
- hormonal changes (including in adolescents);
- dysfunction of the thyroid gland;
- age-related increase in the amount of female sex hormones (observed after 40-50 years);
- high testosterone levels.
Under the influence of these factors, the prostate increases in size, squeezing the posterior portion of the urethra and the muscles surrounding it. Tissue proliferation can lead to more severe consequences, depending on the stage of tumor development.
Surgery and postoperative period
In especially severe cases, drug treatment alone is not enough, and, as a rule, it is necessary to resort to surgical intervention. This may be excision of hyperplastic tissue (adenomectomy) or total resection of the prostate gland (prostatectomy).
There are two types of surgical intervention:
- Open operations (transvesical adenomectomy). With this intervention, access to the gland tissue is gained through the wall of the bladder. This type is the most traumatic and is used only in advanced cases. Open surgery provides complete cure for BPH;
- Minimally invasive operations (in which there is practically no surgical intervention). They are performed using modern video endoscopic technology, without an incision. Access to the prostate through the urethra.
There is another type of surgical intervention that cannot be compared with those described above. Prostate artery embolization is an operation that is performed by endovascular surgeons (the above described are performed by urologists) and consists of blocking the prostate arteries with small particles of a special medical polymer (through the femoral artery). Hospitalization is not required, the operation is performed under local anesthesia and is not traumatic.
After any type of surgery there is a small risk of complications such as urinary incontinence, impotence or urethral stricture.
Unfortunately, at some stages of the disease surgery is simply necessary. BPH is a serious disease, and even after surgery you need to follow some rules in order to finally get rid of the disease and not provoke a recurrence. The three main points that you must follow after surgery are a proper diet, a healthy lifestyle and regular visits to the doctor.
Diet during the postoperative period is extremely important for the patient , as it can significantly contribute to a faster recovery. The diet after surgery completely excludes fatty foods, spices, salty and spicy foods and, of course, alcohol. It is recommended to eat low-fat foods rich in fiber.
As for work, if your profession does not involve frequent physical activity, then you can return to the workplace a couple of weeks after the operation. When working sedentarily, it is recommended to do a warm-up every half hour. A sedentary lifestyle can contribute to stagnation of blood in the organs, which only worsens the disease. For the first few days after surgery, don't even think about lifting anything heavy!
Stop smoking at least in the postoperative period (two weeks after surgery), if you cannot quit the bad habit completely. Nicotine damages the walls of blood vessels, and this affects the blood circulation of the prostate, which can result in an inflammatory process.
Many people think that after removal of BPH they should forget about sexual activity forever. This opinion is wrong, and a man’s sexual function is completely restored after some time. However, you should resume sexual relations no earlier than 4 weeks after the operation.
Another piece of advice that is worth paying attention to: you can drive a car no earlier than a month after BPH removal.
In general, the postoperative period lasts about a month, after which the patient can return to normal life. However, experts strongly recommend leading a healthy lifestyle to prevent the recurrence of the disease.
Almost immediately after the operation, the urine stream becomes stronger, and emptying the bladder becomes easier. After removing the catheter, pain may occur when urinating for some time, the reason for this is the passage of urine through the surgical wound.
Experts do not exclude the occurrence of urinary incontinence or urgent urge to urinate in the postoperative period; these phenomena are completely normal. The more your symptoms bothered you during your illness, the longer your recovery period will be. Over time, all problems will disappear and you will return to a normal rhythm of life.
There may be blood clots in the urine for some time after the intervention. This phenomenon is associated with wound healing. It is recommended to drink as much fluid as possible to properly flush your bladder. But if there is severe bleeding, you should immediately contact a specialist.
After the patient returns to consciousness, the doctor must report the result of the operation. If the patient experiences pain or discomfort in the pelvic area, be sure to notify your healthcare provider.
Gel for penis enlargement for only 147 rubles!
"Titan Gel" - guaranteed penis enlargement. With Titan Gel you will always be in full combat readiness mode!
Read more…
Diagnostic methods
If suspicious symptoms occur, a man should consult a urologist. The doctor will interview the patient, after which he will certainly examine him through a rectal examination to assess the shape and size of the prostate, determine its consistency, and identify the pain of the organ upon palpation.
What research methods can a doctor prescribe:
- urine analysis (biochemical, general);
- culture of prostate secretion;
- identification of prostate antigen-marker of prostate cancer;
- Ultrasound of the prostate gland;
- plain radiography;
- CT and MRI of the pelvic organs;
- cystoscopy;
- biopsy.
A full diagnosis is re-administered after the end of therapy to assess its effectiveness.
After assessing the results of all studies, the doctor will prescribe treatment: first, medication, then, if such therapy does not bring results, surgical intervention is prescribed.
Stages and symptoms
Symptoms of prostate adenoma in men are divided into 2 groups: irritative and obstructive. As the pathology develops, increasing signs and complications are observed.
Modern medicine distinguishes 4 stages of development of the condition. The main signs of adenoma correspond to characteristic changes in the functioning of the urethra.
Compensated form
Prostate adenoma of the 1st degree is characterized by compression of the urethra, as a result of which urine is difficult to excrete.
Symptoms of the initial stage:
- frequent urge to urinate during the day;
- decrease in the volume of urine excreted;
- imperative urges become more frequent;
- periodically there is a delay in the outflow of urine;
- the need to tense the auxiliary muscles.
The kidneys and ureters do not undergo changes, so the general condition of the patient remains stable.
Subcompensation
Benign prostatic hyperplasia of the 2nd degree negatively affects the functioning of the bladder. Due to the constant increase in the volume of unremoved urine, the ureters dilate, signs of chronic renal failure and other changes appear in the upper parts of the urinary system.
Stage 2 symptoms are:
- portioned release of the bladder;
- the thickness of the bubble walls increases;
- some urine is retained;
- involuntary urination becomes more frequent;
- urine is cloudy and may contain bloody impurities.
Decompensation
At this stage, the clinical picture of chronic chronic renal failure increases. Complications from progressive kidney pathology may occur.
Symptoms of grade 3 adenoma:
- constant urge to urinate;
- the ureters dilate as much as possible;
- severe pain in the lower abdomen;
- excretion of urine in small portions.
Associated symptoms in men with pathology:
- weakness;
- nausea;
- loss of appetite;
- constipation;
- thirst.
There is a high probability of developing stage 3 cancer. Due to the large size of the tumor and complete dysfunction of the bladder, waste accumulates in the body, which leads to intoxication.
Terminal
The final stage, at which atony occurs and urination stops completely. The volume of accumulated urine can reach up to 2 liters.
Symptoms of grade 4 prostate adenoma are accompanied by symptoms of chronic renal failure that are incompatible with life. The nitrogen content in the patient's blood sharply increases, the water-electrolyte balance is disturbed and the patient dies from uremia.