What is Hydrosalpinx? This question arises for almost all women who have been given such a tricky diagnosis. If we leave complex medical terms aside, then we can say otherwise that this is dropsy of the fallopian tube (oviduct). Yes, yes, a bag of liquid has formed on the pipe, the dimensions of which vary widely.
Hydrosalpinx
Sometimes, after removing a pathological formation, a woman is shown just a huge “bubble” with a cloudy liquid, reaching the size of a small children’s ball. The female reproductive system is a fairly complex and precise structure, which in its normal state provides ideal conditions for conceiving a new life.
It is no coincidence that oviducts got their name. They are the real path along which the egg or zygote (newly born fetus) “goes” into the uterine cavity. What if this path suddenly became impassable? Then pregnancy becomes impossible, and doctors are forced to give the woman a terrible diagnosis - Infertility. When making this diagnosis, the ICD code - 10 - N70.1 is prescribed in the medical history.
Chronic hydrosalpinx
Chronic hydrosalpinx on the left or right is an already advanced stage of the disease. It is characterized by a “blurred” clinical picture, it proceeds almost unnoticed, causing irreparable harm to the woman’s reproductive system. The constant presence of inflammation and exudate disrupts the functioning of the fallopian tubes. They lose their contractility and elasticity.
But the biggest pathological changes concern the ciliated layer of the oviduct. Cilia, small projections on the lining of the reproductive organ, are designed to help a fertilized egg reach the uterus. They seem to roll over the zygote, because it is deprived of organs of movement. But when dropsy occurs, the eyelashes stick together, and therefore their natural function is disrupted.
Bilateral hydrosalpinx is becoming more common these days. This diagnosis indicates that the oviducts are affected on both sides (Hydrosalpinx on the right, on the left). Bilateral damage to the reproductive system sharply worsens treatment prognoses and increases the risk of infertility. According to statistics, right-sided and left-sided lesions of the fallopian tubes occur with the same frequency.
Prognosis and complications
Long-term hydrosalpinx can be complicated by:
- Violation of the integrity of the tube with spillage of contents into the pelvic cavity. As a rule, this is possible with excessive physical exertion.
- Suppuration - the formation of pyosalpinx, a chronic purulent abscess of the tube.
- Persistent dysfunction of the fallopian tubes.
If you consult a doctor in a timely manner, you can minimize the risk of complications.
With adequate treatment and restoration of tubal patency, spontaneous pregnancies are possible. If the degenerative processes in both fallopian tubes were irreversible, which led to the removal of organs, then pregnancy is only possible with the help of IVF.
What is valve hydrosalpinx
It happens that the commissure blocks the oviduct, but the connective tissue has a softer, more pliable consistency. As liquid accumulates in the pipe, the pressure inside the cavity increases many times, which leads to overstretching of the walls.
Ventilated Hydrosalpinx
The fluid begins to put pressure on the connective tissue with such force that the adhesion cannot withstand, and it becomes possible for the outflow of exudate, which breaks either into the uterine cavity or into the abdominal cavity.
Everything described above occurs with valve hydrosalpinx! The fallopian tube becomes partially patent, which in many cases helps a woman become pregnant. Hundreds of cases have been documented in which women became mothers even with enormous amounts of dropsy.
But a fluid breakthrough can also cause irreparable harm, especially when using IVF (in vitro fertilization). An embryo conceived outside a woman's body and then transferred to her uterus can simply be washed away by the flow of exudate. Thus, all the efforts of reproductive specialists (artificial insemination doctors) fail. That is why it is increasingly recommended to surgically remove dropsy of the fallopian tube before conception “in vitro”.
Classification of the disease: unilateral, bilateral hydrosalpinx and other varieties
Pathology, depending on the location, is:
- One-sided. An adhesive process is observed in one of the tubes (right/left), against the background of which a right-sided or left-sided hydrosalpinx is formed. In this case, the woman still has a chance to get pregnant normally. But the possibilities of natural conception are reduced by 2 times, since only one oviduct is functioning.
- Double-sided. With this type of pathology, both pipes are affected. The passage of the egg is not preserved in any of them. Blocked fallopian tubes make it impossible to conceive naturally.
Hydrosalpinx is classified according to its structure as follows:
- Simple. The effusion containing transudate consists of one cavity.
- Follicular. With this form, a cavity is observed, divided into several particles by adhesions.
- Ventilated (in some sources - valve). This pathology is characterized by periodic emptying of effusion. The contents are poured into the uterus, from which it moves into the vagina, providing characteristic discharge.
Causes of Hydroalpinx
The mechanism of occurrence of the disease has not been fully studied, but the causes of Hydrosalpinx include:
- congenital abnormal development of the organs of the reproductive system;
- disruption of the movement of lymph along the lymphatic tract;
- abdominal operations;
- previous ectopic pregnancy;
- pathological growth of the endometrium;
- perforated appendicitis;
- adhesive disease in the pelvic area;
- poor circulation and/or chronic foci of inflammation in the reproductive organs;
- previously suffered sexually transmitted diseases, especially Chlamydia and Gonorrhea;
- some intestinal pathologies.
The causes of bilateral Hydrosalpinx are identical to the above points.
Forecast
Even with successful restoration of patency and elimination of the adhesive process, in the case of long-term, sluggish inflammation, the full functional viability of the pipes is significantly reduced, since the microvilli of the mucous membrane lose their proper mobility and peristalsis slows down. Patients who have undergone salpingo-ovario- or fimbryolysis in this situation are at risk for tubal (ectopic) pregnancy.
When tube patency is restored and acute hydrosalpinx is removed, natural conception and pregnancy occur in approximately 75% of cases, and the probability of an ectopic pregnancy does not exceed 5%.
Symptoms of Hydrosalpinx
The symptoms of Hydrosalpinx are very varied. These include:
- watery vaginal discharge. They may have a cloudy or serous-purulent structure;
- nagging pain in the area of projection of the appendages. Their intensity is medium;
- When the disease worsens, women note a fairly sharp rise in temperature to 39 degrees. Celsius.
Much less common are prolonged rise in temperature, unexplained weakness, fatigue, poor general health, and depressive psychological conditions that are difficult to treat. These signs are identical for both Hydrosalpinx on the right and on the left.
All signs of Hydrosalpinx can appear with varying degrees of intensity, which increases the risk of incorrect or delayed diagnosis. Sometimes the woman herself delays the gynecological consultation, only aggravating her situation.
First stage of treatment
Hydrosalpinx cannot be completely cured conservatively. Often the condition recurs, since the pathomorphological prerequisites remain. Drug treatment of hydrosalpinx is ineffective, but it is carried out to alleviate the symptoms of the disease. Only rarely is it possible to restore the patency of the tubes with the help of medications.
Drug therapy for hydrosalpinx:
- When infected with bacterial microflora of the internal genital organs, antibiotics are prescribed.
- After systemic antibiotic therapy, antimycotic drugs are prescribed to prevent candidiasis.
- Nonsteroidal anti-inflammatory drugs help reduce swelling, reduce the secretion of exudate and improve microcirculation.
- Enzyme preparations are used to combat adhesions in the uterus and fallopian tubes.
- Immunocorrection and restorative therapy with vitamins.
Treatment of hydrosalpinx is carried out in two stages. First, anti-inflammatory therapy is prescribed, which helps stop the infection process in the tubes. For this, the patient is prescribed antibacterial drugs and vitamins. The effectiveness of physiotherapy procedures (electrophoresis, laser phoresis, magnetophoresis, ultraviolet irradiation, UHF, hirudotherapy) has been proven.
The second stage is surgery. There are many different ways to clear the blockage and create a bypass for the egg. Laparoscopic methods are the least traumatic, but quite effective.
Differential diagnosis
Today, various methods for differential diagnosis of the disease are available. These include:
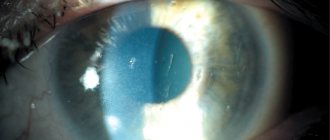
- Ultrasound (ultrasound examination). Hydrosalpinx on ultrasound looks like a liquid pathological inclusion, localized in the space between the ovary and the uterus itself. This echo sign is a decisive factor in making this diagnosis;
- gynecological examination;
- hysterosalpingography (hydrosalpingography (HSG);
- laparoscopy. It should be noted that laparoscopy can not only identify hydrosalpinx, but also cure it.
Diagnosis of hydrosalpinx
Hydrosalpinx is often discovered during a routine examination or when visiting a gynecologist regarding infertility. Only during an examination can the doctor detect a painful and round or oval-shaped formation in the area of the oviduct. It is possible to clarify the diagnosis and differentiate the dilated tube from other pathologies with instrumental examination.
Diagnosis of hydrosalpinx includes:
- gynecological examination;
- examination of vaginal discharge (smear);
- ultrasonography;
- hysterosalpingography;
- diagnostic laparoscopy.
Ultrasound scanning can be performed using both the percutaneous abdominal and vaginal methods. When examined, an enlarged fallopian tube with homogeneous contents is clearly visible between the uterus and ovary. With pyosalpinx, it has a heterogeneous character.
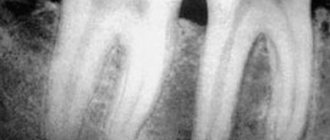
To check the patency of the tubes, hysterosalpingography is performed. Moreover, it should be remembered that the formation of hydrosalpinx can be a symptom of fallopian tube cancer. Therefore, when it is detected, you need to be careful and conduct additional cytology diagnostics.
Diagnosis of hydrosalpinx using laparoscopy is not only a diagnostic, but also a therapeutic method. Upon examination, enlarged oviducts with thinned walls are revealed. The fimbriae are usually swollen. During laparoscopy, it is possible to dissect the adhesions surrounding the oviduct and ovaries, due to which the physiological position of the tube is changed, and create a stoma (an opening for fluid outflow) to continue conservative treatment.
Conservative treatment
Treatment without surgery is the first step towards getting rid of the disease. To combat the inflammatory process, treatment with broad-spectrum antibiotics is used. Such drugs are prescribed not only in injections, but also in tablets and suppositories, which only simplifies treatment. Longidaza must be prescribed as a drug ideal for treating this disease.
To mobilize the body's own strength, general strengthening, vitamin, absorbable preparations and medications that remove excess fluid from tissues are additionally prescribed. The effect of drugs is enhanced by physiotherapeutic procedures and laser therapy.
Causes of pathology
The main source of the formation of disorders in the fallopian tube is the infectious-inflammatory process.
The infection can penetrate the oviduct in 2 ways:
- Rising. Infectious agents ascend through the woman’s reproductive system (through the vagina, uterus).
- Descending. Infection brings blood flow (from any organs: kidneys, intestines, etc.)
Inflammation can be caused by a variety of gynecological pathologies.
Hydrosalpinx can develop against the background of inflammation occurring in the reproductive system
Doctors give the following reasons for the formation of hydrosalpinx:
- endometritis;
- wearing an intrauterine contraceptive for a long period of time;
- inflammatory processes occurring in the appendages, ovaries or tubes (adnexitis, oophoritis, salpingitis);
- tuberculosis of the reproductive system;
- vaginal dysbiosis;
- promiscuity;
- long-term vaginitis;
- abortions;
- infections of the reproductive system (gonococci, trichomonas and others);
- curettage of the uterus;
- frequent hypothermia;
- myomatous nodes at the junction of the oviduct and uterus;
- adenomyosis;
- sexual infantilism (underdevelopment of the system - thin long pipes).
Not every adnexitis or salpingitis causes the formation of hydrosalpinx. Timely treatment of such pathologies allows you to get rid of the inflammatory process forever, without any consequences.
Predisposing factors
Pathological saccular formation in the oviduct is formed under the influence of the following factors:
- Endocrine disorders, such as diabetes, thyroid diseases, which reduce the protective forces of the female body.
- Frequent stress, psycho-emotional stress.
- Neglect of personal hygiene rules.
Treatment of Hydrosalpinx: auxiliary methods
Sanatorium-resort treatment is especially indicated for women with chronic bilateral hydrosalpinx. Mud baths have a powerful absorbing effect, which will certainly be beneficial for this disease. After all, if the fallopian tubes restore patency, then the likelihood of pregnancy will increase many times over.
Homeopathy is another auxiliary method of treating the disease. The benefits of taking homeopathic medicines are very controversial, have no evidence base and are not accepted by official medicine. But, after a detailed consultation with a specialist, you can try this method of defeating the disease.
On the forms of those women who have cured the disease, one can increasingly see positive reviews about treatment with leeches. Even wise Chinese healers for thousands of years saved women from diseases of the reproductive system through the use of a special type of leeches. Then this technique was undeservedly forgotten, but today it is experiencing a real “boom” in popularity.
This pathology has long been treated with propolis. To prepare the tincture, use only high-quality raw materials or buy a ready-made product at the pharmacy. For home preparation, take medical alcohol (60%) and mix it with crushed propolis (40%). Use the tincture to rub the skin of the abdomen on the affected side.
In folk medicine, decoctions of anti-inflammatory herbs are used as medicinal microenemas. Juice treatment, which is combined with clay therapy, is actively used.
It should be remembered that traditional medicine cannot become the main treatment even if a mild degree of this pathology is detected. Folk remedies are just an addition to complex treatment!
Pregnancy with hydrosalpinx
There is still an opportunity to conceive a child! But with the condition that only one side of the fallopian tubes is affected. In this case, the chances will decrease by 50%. The process of bearing a child will be difficult and with the risk of spontaneous abortion. This course of events is determined by defects in the ciliated epithelium and impaired peristalsis of the fallopian tube. In some cases, fertilized eggs are retained in the oviduct for a period of 4 days, implanted and begin to develop there. The result is an ectopic pregnancy.
Reasons for unexpected termination of pregnancy:
- mechanical influence: fluids regularly flowing from the ventral hydrosalpinx can wash away the zygote without allowing it to implant;
- damage to the uterine mucosa due to discharge that causes endometritis;
- death of the embryo due to the toxic effects of the transudate;
- decreased hormonal regulation and sensitivity of the endometrium of the uterus.
With bilateral hydrosalpinx, the likelihood of natural pregnancy is completely excluded. In this case, the only effective option is IVF. But here, too, the chance of a successful outcome is reduced by two or even three times.
If pregnancy does occur, then such women automatically fall into the risk group. Termination of pregnancy can occur both early and late. Treatment of hydrosalpinx is postponed to the postpartum period.
Treatment of hydrosalpinx disease with surgery
Sometimes it happens that treatment of Hydrosalpinx can only be continued through surgery - removal of the dropsy. When removing Hydrosalpinx, a gentle technique is most often used - laparoscopy.
To carry it out, the latest optical technology is required, through which dropsy is removed without opening the abdominal cavity, which minimizes the risk of postoperative complications, reduces the likelihood of developing adhesions and bleeding, and does not cause serious cosmetic defects.
After the stage of removing the dropsy, the surgeon performs plastic surgery of the oviduct, restores its patency, excises adhesive scars and restores re. Laparoscopy of Hydrosalpinx has a number of contraindications, which the gynecologist treating you will definitely warn you about.
Some women suffer from a real phobia that prevents them from having surgery on time and finding the joy of motherhood. In such cases, a competent gynecologist will definitely advise you to visit thematic forums where you can casually communicate with people who have overcome identical problems.
On such sites you can look at photos and listen to videos about the stages of surgery, get acquainted with the symptoms and duration of the postoperative period, and find out the norm of laboratory tests. But if fear remains an insurmountable obstacle, then, without hesitation, you should go to a professional psychologist.
Treatment prognosis
If the patency of the tube is restored and the hydrosalpinx is removed, then the woman’s chance of conceiving and carrying a child increases to 60–75%.
When the tube is removed, the patient is recommended IVF (artificial conception). In this case, the effectiveness of the event is 30–35%.
Possible complications and consequences
Despite the fact that the disease in most cases does not cause severe discomfort in a woman, if left untreated it can lead to serious consequences:
- menstrual irregularities;
- vaginal dysbiosis;
- bending of the uterus;
- ectopic pregnancy;
- intestinal obstruction;
- pyosalpinx (purulent-inflammatory type) - in case of infection attached to the transudate;
- infertility;
- rupture of the fallopian tubes;
- inability to bear a child (constant miscarriages);
- purulent peritonitis (when purulent contents leak into the peritoneum as a result of rupture of the oviduct).
Surgery
The last stage of treatment for hydrosalpinx is surgical removal of the pathological neoplasm. It is important to understand that conservative therapy without surgery will not bring the desired effect and the disease will continue to progress. It is necessary to eliminate all adhesions that have formed in the pelvis.
The main method of combating hydrosalpinx is laparoscopy. This technique is not only the most effective, but also gentle, and you can choose an individual intervention technique, which depends on the patient’s desire to have or not have children in the future.
Hydrosalpinx can be removed by tubectomy. Source: medbe.ru
Here are some options for quickly solving the problem:
- Tubectomy - performed in situations where there is no other way to get rid of the pathology, and involves the removal of one or two fallopian tubes;
- Salpingoneostamia - with this intervention, the doctor performs actions that create a new opening in the middle section of the oviduct;
- Fimbryoplasty - performed to free the fimbriae from adhesions and to remove fluid from the fallopian tube;
- Salpingo-ovariolysis is the dissection of formed adhesions around the ovary and fallopian tube, after which its normal position is restored.
It is important to understand that hydrosalpinx is a serious complication of gynecological inflammatory diseases. If a girl wants to become a mother in the future, and also cares about the functioning of her body in general, and the reproductive system in particular. She needs to undergo proper treatment, which should be entrusted to an experienced doctor.
Physiology
Understanding a disease such as hydrosalpinx, what it is and what the causes are, it is necessary to understand the role of anatomy and physiology in this complex process. The fallopian tubes are a paired organ that looks like a tube (empty inside) with two lumens. Its length ranges from 10 to 12 centimeters, with the right side slightly longer than the left.
One lumen of the fallopian tube is open in close proximity to the ovary towards the abdominal cavity, and the second is directed towards the uterus. Thanks to this anatomical structure, reproductive and other internal organs communicate, so the likelihood of developing an ascending infection increases significantly.
Above, hydrosalpinx was presented, a photo of the pathological formation, and this picture describes in detail the anatomy of the fallopian tubes.
Anatomical features of the fallopian tubes. Source: treatment-online.com.ua
In turn, the walls of the fallopian tubes consist of three layers. On the inside, the organ is covered with ciliated epithelium. Since it is covered with peculiar villi that make progressive movements, the fertilized egg moves along the tube towards the uterus. There is also a mucous component, thanks to which conditions are created in which the zygote, egg and sperm can survive.
The muscle layer is responsible for performing contractile movements. The fibers of this tissue are also directed towards the uterus. On the outside there is the peritoneum, which provides some protection to the fallopian tubes from various kinds of negative influences.
When everything becomes clear with the anatomical structure, you can begin to consider how hydrosalpinx is treated without surgery, with surgery and traditional methods. But the first thing would be to correctly understand the mechanism of formation of the pathological process.
Therapy
If hydrosalpinx has been diagnosed, treatment without surgery, reviews of which vary, is carried out provided that conservative therapy can provide a sustainable therapeutic effect. If correct therapy is not carried out in a timely manner, the pathological process will be complicated, and then surgery will be the only way to solve the problem.
Since adhesions form during hydrosalpinx, the main and most dangerous complication of the disease is infertility. The fight against pathology takes place in two stages. Conservative treatment is initially prescribed, therefore, when hydrosalpinx is diagnosed, antibiotic treatment is mandatory, and the course must be complete.
At the same time, specialists select individually for each patient, taking into account the characteristics of the body and the clinical picture, immunomodulators, for example, Immunal, Imudon, Timalin, Taktivin, Likopid. Autohemotherapy can be performed, in which one’s own venous blood is administered intramuscularly.
It is necessary to take vitamin complexes, but their parenteral administration is also allowed. Various physical therapies have a good effect; although they are not able to cure the pathology on their own, they can speed up the process of recovery of the body. Therefore, doctors often prescribe UHF, gynecological massage, electrical stimulation of the fallopian tubes, magnetic cutting, and ultraviolet irradiation to their patients. It is possible that the problem can be solved by resorting to hirudotherapy, but before this a medical consultation is necessary.
What indicates pathology
Symptoms of hydrosalpinx do not have signs characteristic only of this pathology. They can also be observed in other diseases of the pelvic organs: salpingitis, endometritis, parametritis.
Chronic hydrosalpinx of small size may not manifest itself and become an accidental finding on ultrasound. If there is a significant accumulation of fluid, the following signs of hydrosalpinx may appear:
- nagging pain in the lower abdomen;
- dyspareunia;
- periodic increase in temperature.
With draining hydrosalpinx, liquid, light discharge may appear from the vagina. Menstruation with pathology may not change or become painful and more intense.
Exacerbation of inflammation manifests itself in the form of more pronounced pain in the lower abdomen on the affected side. With hydrosalpinx of two fallopian tubes, there may be non-localized pain in the pelvis. In this case, the temperature rises to 38-39°C, weakness and signs of general malaise appear. Sometimes there may be similarities with renal colic, acute appendicitis.
A complication may be the addition of a secondary infection and transition to pyosalpinx. Suppuration leads to a deterioration of the condition, the appearance of symptoms of intoxication in the form of headache and muscle pain, chills.
Hydrosalpinx is dangerous due to rupture of the fallopian tube. In this case, acute pain in the abdomen appears, signs of a state of shock: rapid heartbeat, a sharp decrease in pressure, cold sticky sweat, pallor.
Hydrosalpinx and pregnancy
Most women with this pathology face problems conceiving. In this regard, the question of whether it is possible to become pregnant with hydrosalpinx is common among such patients. Doctors do not exclude the possibility of conception, but pay attention to reducing its likelihood. Removing adhesions in the fallopian tubes does not always help solve the problem, so doctors recommend in vitro fertilization (IVF). If the fallopian tubes are removed, this is the only option for conception.
What causes the disease
The penetration of infectious pathogens occurs through the bloodstream, which comes from the kidneys, bladder, and intestines. The inflammatory process can also be provoked by gynecological pathologies.
The main reasons why hydrosalpinx may develop are:
- uterine cleaning and abortion;
- intrauterine contraceptives;
- hypothermia;
- inflammation of the uterus;
- adenomyosis;
- features of the anatomy of the pipes (long, thin, tortuous);
- frequent change of partners;
- myomatous node, which is located at the entrance of the oviduct to the uterus.
Among the predisposing factors that significantly increase the risk of pathology formation are:
- frequent stressful situations;
- emotional stress;
- diabetes;
- thyroid diseases;
- failure to comply with personal hygiene rules.
It should also be noted that not in all cases, salpingitis or andexitis can result in the development of hydrosalpinx.
With a healthy immune system, as well as timely treatment, inflammatory processes in the fallopian tubes are eliminated and do not cause any unpleasant consequences.
Treatment (antibiotics and suppositories)
If Adnexitis is diagnosed, treatment with antibiotics and suppositories is inpatient with bed rest. First of all, treatment is aimed at reducing pain in a woman, and then therapy is carried out to eliminate the cause of the disease.
The treatment regimen and tactics consists of several stages, which is carried out in accordance with all the doctor’s recommendations. How to treat adnexitis, and which drugs are best to inject and which ones to take in tablet form can only be prescribed by a qualified specialist.
List of drugs used in treatment:
Source: https://krasotagood.ru/adneksit-salpingooforit-kod-mkb-10.html
Prevention
Preventive measures are quite simple and commonplace, but this does not reduce their effectiveness. A woman should adhere to the following principles.
- Immediately treat diseases of the pelvic organs.
- Avoid sexual contact with random people.
- Use condoms as a barrier method of contraception.
- Observe personal hygiene rules.
- Give up bad habits such as alcohol and smoking.
- Visit your gynecologist regularly and conduct preventive examinations.
Despite the rather meager symptoms, a woman should not be deceived by the harmlessness of this pathology. It is necessary to contact a specialist at the first signs of the disease, as serious consequences are possible. However, with timely treatment measures, all negative development options can be completely nullified.
The first signs of hydrosalpinx
Painful sensations are not the first sign of the disease. On the contrary, they join when the pathology progresses, accompanied by inflammation or activation of the bacterial flora. Pain can occur during acute hydrosalpinx, but this is preceded by earlier symptoms:
- deterioration in general health;
- temperature rise to subfebrile levels;
- pulling sensations, which many patients attribute to inflammation of the appendages in the past.
How to avoid chronic adnexitis?
As a prevention of primary chronic adnexitis (occurring without a preliminary acute stage), it is recommended:
If you are sexually active, it is necessary to examine both partners.
Reviews
I was treated with all sorts of methods - antibiotics, physiotherapy, etc. A month later, an ultrasound showed that the pathology had disappeared. However, after 2 months, during a follow-up examination, hydrosalpinx was again discovered. I had to change the doctor, who determined that the pipe was not working and surgery was required. Laparoscopy was performed. I was lucky, probably, the pipe remained in place, they only performed plastic surgery.
Anna, 46 years old
Just a year ago, a similar diagnosis was made, because something similar was found in the fallopian tube. Treatment was antibiotics, Vishnevsky ointment and Viferon. I have never had such a pathology again. I’m not even sure now that the diagnosis was made correctly. Currently pregnant, naturally.
Veronica, 32 years old
Don't get too carried away with self-medication. This can lead to not the most comforting consequences. Only a properly formed set of therapeutic measures can give positive results. The main thing to remember is that if you have the first signs of a disease such as hydrosalpinx, you should not delay visiting a doctor.
Causes and prevention of hydrosalpinx
Hydrosalpinx is a complication after inflammation of the appendages. It, in turn, can be caused by the following reasons:
- Hypothermia. Promotes activation of pathogenic flora, weakening of protective functions and the inflammatory process.
- Abortions or miscarriages in the past. Mechanical damage to the appendages, as well as infection during surgery, plays a role.
- Endometritis is inflammation of the uterus.
- Incorrectly installed uterine device.
- Endometriosis – reduces the patency of the fallopian tubes.
- History of gynecological surgery – scars or adhesions may remain on the uterus and ovaries, which disrupts the protective properties of the organs and makes them more susceptible to the influence of negative factors.
- Protection with non-barrier methods of contraception – increased likelihood of infection and chronic inflammatory processes;
- Urinary system infections - inflammation and pathogens are easily transmitted to the genitals.
- Uterine fibroids - mechanically compress the appendages, which provokes the formation of adhesions, inflammation and hydrosalpinx;
- Dysbacteriosis of the vagina and even the intestines - leads to a decrease in protective forces, activation of pathogenic flora, which spreads through the genital tract.
On the right side, hydrosalpinx can occur as a complication of appendicitis. Systemic endocrine diseases, as well as the psycho-emotional state, play an important role in the formation of hydrosalpinx. Constant stress and frequent hypothermia cause many diseases in the field of gynecology.
Traditional methods
If the doctor has accurately diagnosed hydrosalpinx, treatment with folk remedies, reviews of which are often positive, can also help the body cope with the progression of the pathological process. It is very important that the treatment be comprehensive, because herbal infusions alone, as well as physical procedures, will not lead to recovery.
So, traditional healers advise using the following plants:
- Drink infusions of the following herbs: St. John's wort, sage, chamomile, currant leaf;
- You can prepare an infusion of adonis;
- It is very good to take juniper baths, for which a decoction of the branches is first prepared and then poured into the bath;
- It is recommended to take oat infusion, a mixture of honey, butter and aloe leaves;
- Microenemas with herbal decoctions (chamomile, oak bark, calendula) may be useful;
- It is necessary to include natural pumpkin, potato and nettle oils in your diet, separately or in combination with each other.
Before starting treatment, you must make sure that the woman is not allergic to medicinal plants. In case of individual intolerance to herbs, a different method of therapy should be chosen.
Causes of hydrosalpinx
The transformation of the fallopian tubes into the sactosalpinx type (saktos - sac) is facilitated by the adhesive process that develops as a result of previous diseases of the pelvic organs. At the same time, connective tissue grows in the lumen of the tube, and septa form, forming pseudocysts. The lumen of the pipe narrows to the point of complete obstruction in a certain area. Due to impaired blood and lymph circulation in the walls of the tube, transudate begins to accumulate in the formed cavity, consisting of secretions produced by the mucous membrane, blood plasma and extracellular fluid. When the cavity is filled with transudate, the walls of the tube are significantly stretched, deformed and thinned. The fluid may periodically pour out or be partially absorbed by the walls, but the presence of adhesions and an inflammatory reaction determines the re-formation of hydrosalpinx and the recurrent nature of the disease.
In most cases, hydrosalpinx is preceded by a local infectious-inflammatory process (salpingitis, adnexitis, endometritis), caused by both nonspecific microbial flora (including mixed infection) and STI pathogens (chlamydia, gonorrhea, mycoplasmosis, trichomoniasis, etc.). The group at increased risk for the formation of hydrosalpinx includes patients with endometriosis who have undergone reconstructive surgery on the fallopian tubes and other surgical interventions on the pelvic organs.
Treatment methods: effective and not so effective
Getting rid of the pathology is necessary to eliminate the source of chronic infection, which can lead to serious complications. For women of reproductive age, elimination of pathology is necessary for a successful pregnancy or to prepare for IVF. Treatment methods can be conservative or surgical.
Conservative therapy
Treatment of hydrosalpinx without surgery is possible only in cases of small size of the disease, as well as in cases of draining formation. This method can be used in women who are not planning a pregnancy and who refuse more radical and reliable methods. Conservative therapy is also aimed at preventing the addition of infection and the transition of pathology to pyosalpinx. The following methods of influence are used:
- drug treatment;
- physiotherapy;
- balneotherapy.
Drug treatment is carried out using broad-spectrum antibiotics in the presence of an infectious process. If, based on the results of an examination for sexually transmitted infections, a specific pathogen is isolated, then antibiotics are selected taking into account its sensitivity.
For treatment, proteolytic drugs are used that help resolve adhesions:
- "Distreptase";
- "Longidaza".
The effectiveness of “Distreptase” has not been proven by clinical randomized studies; it is used only based on the experience of past generations. The therapeutic potential of Longidase has been confirmed by relevant studies. It is available in the form of tablets, suppositories and powder for the preparation of a solution for injection.
These drugs are used not only for the treatment of chronic salpingitis, oophoritis, hydrosalpinx, but also at the stage of rehabilitation in the postoperative period after operations on the pelvic and abdominal organs.
Physiotherapy is prescribed by a doctor taking into account the pathologies a woman has: warming and increasing blood flow procedures may not be suitable for everyone. With fibroids, which can also cause hydrosalpinx, many physiotherapeutic methods are contraindicated, as they can provoke the growth of the node.
People's approach
Traditional medicine offers treatment using medicinal herbs for oral administration or preparing decoctions from them. A tampon is moistened in the resulting aqueous extracts and left in the vagina for some time. Reviews about the treatment of hydrosalpinx with boron uterus indicate the effectiveness of the technique.
But folk remedies do not have the necessary anti-inflammatory activity and are unable to suppress infection or dissolve adhesions. Therefore, they are used only as an auxiliary method in combination with doctor’s prescriptions.
Surgical intervention
The main way to get rid of it is surgical treatment. Preference is given to laparoscopic methods of intervention. The following types of operations can be performed:
- salpingo-ovariolysis - dissolution of adhesions around the appendages and ovaries, as well as restoration of patency inside the tubes;
- fimbryolysis is a similar intervention, but it is limited to dissolving adhesions on the fimbriae;
- salpingostomy - creation of a new hole in the ampullary section of the tube or creation of patency of an anatomical hole.
After surgical treatment, suppositories are additionally prescribed to prevent adhesions, physiotherapy and mud therapy.
But removal of hydrosalpinx does not guarantee restoration of the functions of the appendages. Prolonged stretching of the muscle layer and toxic effects on the epithelium of exudate disrupt contractility and peristaltic movements. But in some cases, spontaneous pregnancy may occur in the near future after recanalization.
For women planning a pregnancy using IVF, treatment for hydrosalpinx involves removing the abnormal fallopian tube. This way you can get rid of the risk of toxic effects on the embryo and endometrium, and also increase the chances of success already in the first protocol.
Diagnostics
Initially, if a woman suspects that she has developed a gynecological pathology, she needs to go to see a doctor and undergo a standard examination procedure in a chair. When the doctor performs a palpation procedure, the pathological formation is palpated, and it looks like a tight, elongated formation on one or both sides. With such an examination, pain may or may not be present in the area of the appendages.
To confirm the diagnosis, additional examinations are prescribed:
- Transvaginal ultrasound scanning. Thanks to it, you can determine the location of the tumor, its size and shape.
- Hysterosalpinography. An X-ray examination using a contrast agent, as a result of which a series of pictures is taken, thereby visualizing a pathological formation in the uterine cavity.
- Laparoscopy. This method is used to diagnose and, if necessary, treat hydrosalpinx. With this procedure, it is possible to determine where the formation is located and to determine the thickening of the fallopian tubes.
In addition to the procedures presented, the woman will also need to undergo standard tests and be checked for the presence or absence of HIV infections and other viruses.
Causes
When understanding a disease such as hydrosalpinx on the left, what it is, and how it can be dangerous, it is necessary to understand the reasons that lead to the development of this disease in women of reproductive age. So, the main reason is the closure of the middle section of the fallopian tube, which is a consequence of infection and the onset of inflammation.
In the photo below you can see what hydrosalpinx is on the left.
As for the methods of penetration of pathogenic microorganisms, they can penetrate the fallopian tubes both ascendingly, that is, from the organs that are located below them (cervix, uterus, vagina), and descending (transmitted throughout the body during the blood circulation) from the appendix , intestines, kidneys, tonsils, bladder.
Also, the inflammatory process can develop against the background of progression of any gynecological pathologies. If a woman has been diagnosed with hydrosalpinx, the causes of this condition may be as follows:
- The woman underwent a therapeutic or diagnostic curettage procedure;
- The woman has ever had an artificial termination of pregnancy (abortion);
- Opportunistic microflora has become more active, which happens when the body's metabolic system decreases due to hypothermia;
- The girl uses intrauterine contraception;
- A woman does not have a permanent sexual partner, she enters into promiscuous intimate relationships with different men, often changing them;
- Sexual infections were diagnosed, for example, gonococcus, chlamydia, trichomonas, ureaplasma;
- Inflammation of the endometrial uterine layer develops;
- There are diseases of the uterus, appendages, ovaries;
- During laparoscopy, the woman's oviduct was injured;
- The fallopian tubes have an abnormal structure; they are long, too thin and tortuous;
- In the place where the fallopian tube enters the uterus, a fibroid has formed (the node closes the lumen);
- Adenomyosis progresses;
- There is external endometriosis, in which adhesions and aseptic inflammation are formed;
- The woman has a progressive inflammatory process affecting the cervical canal and cervix;
- Under the influence of various factors, there was a disruption in the composition of the vaginal microflora, and dysbacteriosis was noted.
Why right-sided and left-sided hydrosalpinx occurs, what kind of pathological formation it is, is clear, but we should not forget that the disease develops not only for the main reasons, but also under the influence of provoking agents.
The risk group for the accumulation of fluid in the fallopian tubes includes those women who have malfunctions of the thyroid gland, dysfunction of the endocrine system, and diagnosed with diabetes mellitus. Also, stress, severe emotional stress, and insufficient intimate hygiene are always a predisposing factor. Next, let's look at the symptoms of hydrosalpinx.
Hydrosalpinx
The disease can manifest itself acutely or be indolent with remissions and relapses.
It affects one pipe or both at the same time. The cavity filled with transudate can be one or divided by partitions into several chambers. The diameter of the pipe increases from several millimeters to several centimeters, and the walls become thinner. Due to poor circulation, swelling of the fimbriae occurs.
The main complication of hydrosalpinx is infertility, which is caused not only by obstruction of the oviduct, but also by a constantly maintained inflammatory process that prevents embryo implantation, causes damage incompatible with life and miscarriages in early pregnancy.
Treatment of hydrosalpinx is carried out conservatively or more effectively surgically. If it is impossible to completely restore the functionality of the oviduct, or there is a relapse, tubectomy is recommended in many cases to prevent complications.
Classification of hydrosalpinx
| Right-handed | the pathological process affects only the right fallopian tube. |
| Left-handed | the pathological process affects only the left fallopian tube. |
| Bilateral | Both tubes are affected. Most often, with this form of pathology, complete infertility develops (the inability to get pregnant on your own). |
| Simple | a process limited to one cavity of the fallopian tube. |
| Follicular | a process in which cavities are formed, formed by the growth of adhesions that divide the lumen of the fallopian tube into several chambers. |
| Ventilated | The fluid accumulated inside the tube, due to its pressure and elasticity of the internal adhesions, breaks into the uterine cavity, and then out through the vagina. |
Causes of hydrosalpinx
Hydrosalpinx is often caused by adhesions formed as a result of inflammatory processes. They prevent the normal outflow of secretions produced by the mucosa. Liquid can also accumulate due to sweating into the cavity of the tube from the extracellular space and small vessels.
- Adhesions can be located in the abdominal cavity or inside the oviduct. The adhesive process in the abdominal cavity occurs after surgical interventions for various diseases of the internal organs, for example, after appendicitis, peritonitis of various etiologies. The cause of the adhesive process can be inflammation of the appendages, endometriosis and other female diseases.
- Adhesions in the fallopian tube are formed during inflammatory processes of an infectious and non-infectious nature. Their formation occurs gradually, so at some stage, when the adhesions do not completely block the lumen of the pipe, the liquid accumulating in it can be periodically emptied. This is the so-called ventilated form, it is characterized by periodic abundant mucous discharge.
- The causes of hydrosalpinx are inflammatory processes in the genital or nearby organs that cause adhesions. These can be infectious diseases, STDs, caused by specific and nonspecific microflora.
- The inflammatory process is usually localized in the uterus (endometritis), ovaries, appendages (adnexitis) or in the abdominal cavity (appendicitis). The disease is often provoked by abortion, diagnostic curettage, and surgical interventions on the pelvic and abdominal organs.
A disruption in the outflow of fluid can occur when neoplasms form in the oviduct, which, increasing in size, block its lumen. Therefore, during the examination it is necessary to carry out differential diagnosis with oncopathology.
Signs and symptoms of hydrosalpinx
Usually the disease is asymptomatic. A small amount of transudate can cause nagging pain in the pelvic area on one side, heaviness. Since the fluid gradually stretches the walls of the oviduct, complaints of severe pain are rare. It may appear during sex or when performing certain physical exercises.
Sharp pain on one side, accompanied by increased heart rate and cold sweat, indicates a pipe rupture and emptying of the contents into the abdominal cavity. Unlike pyosalpinx, when diagnosed with hydrosalpinx, peritonitis does not always develop, but the likelihood of bleeding from the damaged tube is high.
More often there is a valve form, in which fluid is emptied into the lumen of the uterus. In this case, the woman experiences profuse leucorrhoea (mucous discharge).
Emptying does not indicate restoration of patency and cure, since the process is usually recurrent in nature. This is due to the fact that adhesions remain, and their rupture promotes the re-formation of fibrin threads.
In addition, when the pipe cavity is stretched, its normal peristalsis is disrupted, which also contributes to the formation of adhesions.
So, symptoms of hydrosalpinx can be:
- nagging pain in the lower abdomen, which may intensify during sexual intercourse;
- mucous discharge;
- difficulty conceiving.
Often, a woman does not feel any discomfort, and the pathology is detected when visiting a doctor about infertility. Hydrosalpinx is one of the causes of tubal infertility.
Moreover, infertility with this pathology can be associated not only with tubal patency.
- Periodic abundant emptying of the transudate can physically “wash away” the blastocyst, which is especially important if a woman, due to infertility, has decided to seek the help of assisted reproductive technologies and undergo IVF.
- There is also evidence that the exudate contains a large amount of bioactive substances that adversely affect the embryo, contributing to early miscarriage. Therefore, if a woman is indicated for IVF, in order to reduce the risk of unsuccessful procedures, it is recommended to undergo laparoscopic tubectomy in advance.
- Symptoms of hydrosalpinx usually appear against the background of chronic salpingitis, and with exacerbations it can lead to suppuration of the effusion, the formation of pus, pyosalpinx, and subsequently to peritonitis.
- If with hydrosalpinx the increase in body temperature is short-term and does not exceed 37.4-37.7 degrees Celsius, then pyosalpinx is characterized by fever, increased heart rate, and weakness. The consequences of pyosalpinx are very dangerous, so if such symptoms are detected, a visit to the doctor cannot be postponed.
Diagnosis of hydrosalpinx
Hydrosalpinx is often discovered during a routine examination or when visiting a gynecologist regarding infertility. Only during an examination can the doctor detect a painful and round or oval-shaped formation in the area of the oviduct. It is possible to clarify the diagnosis and differentiate the dilated tube from other pathologies with instrumental examination.
Diagnosis of hydrosalpinx includes:
- gynecological examination;
- examination of vaginal discharge (smear);
- ultrasonography;
- hysterosalpingography;
- diagnostic laparoscopy.
Ultrasound scanning can be performed using both the percutaneous abdominal and vaginal methods. When examined, an enlarged fallopian tube with homogeneous contents is clearly visible between the uterus and ovary. With pyosalpinx, it has a heterogeneous character.
To check the patency of the tubes, hysterosalpingography is performed. Moreover, it should be remembered that the formation of hydrosalpinx can be a symptom of fallopian tube cancer. Therefore, when it is detected, you need to be careful and conduct additional cytology diagnostics.
Diagnosis of hydrosalpinx using laparoscopy is not only a diagnostic, but also a therapeutic method. Upon examination, enlarged oviducts with thinned walls are revealed. The fimbriae are usually swollen.
During laparoscopy, it is possible to dissect the adhesions surrounding the oviduct and ovaries, due to which the physiological position of the tube is changed, and create a stoma (an opening for fluid outflow) to continue conservative treatment.
Treatment of hydrosalpinx
If a woman is diagnosed with hydrosalpinx, its treatment requires surgical intervention, which is performed by laparoscopy or laparotomy. It is necessary to cut the adhesions that prevent the outflow of fluid. When the outflow is restored, it is necessary to continue treatment with conservative methods.
The laparoscopic method for this type of intervention is more preferable because it has the following advantages:
- Minimally invasive and low-traumatic operation. Three small incisions are made through which endoscopic equipment is inserted and the altered oviduct is removed.
- Rapid recovery after surgery; already on the second day the patient is allowed to walk, and after a week to lead a normal lifestyle, with the exception of strong physical exertion and heavy lifting.
- Lack of contact with air during the laparoscopic method prevents the formation of new adhesions.
To prevent the formation of adhesions, patients are raised early; bed rest is indicated only in the first hours after surgery, until the patient recovers from anesthesia. Then they are allowed to sit, stand up, and walk under the supervision of medical staff or caregivers.
After surgery, conservative treatment is prescribed, which includes:
- antibiotic therapy;
- anti-inflammatory substances;
- painkillers;
- absorbable drugs.
Physiotherapy shows good effectiveness; the following are prescribed:
- electrophoresis;
- laser phoresis;
- magnetic therapy;
- electrical stimulation of the fallopian tubes;
- balneotherapy;
- mud therapy.
It is quite difficult to restore the patency of the tube, since even after getting rid of adhesions, it is not always possible to achieve complete restoration of the ciliated epithelium, thanks to which the fertilized egg moves from the ovaries into the uterine cavity. This can lead to an ectopic pregnancy, so if a woman does not plan to have children, then when treating hydrosalpinx, it is better to remove the altered tube.
The possibility of getting pregnant with one tube with a unilateral process remains, but if both tubes are affected, there is a high risk of developing an ectopic pregnancy, which is dangerous for the woman.
Experts recommend resorting to assisted reproductive technologies in case of infertility due to hydrosalpinx.
But in this case it is necessary to undergo a tubectomy, since altered tubes are a source of infection, support inflammation of the endometrium, and reduce the chances of becoming pregnant during IVF.
Prevention of hydrosalpinx
Prevention of hydrosalpinx is the prevention of the development and timely treatment of inflammatory processes in the reproductive organs and abdominal cavity. To do this, it is necessary to increase the body's resistance and reduce the risk of infection.
To prevent hydrosalpinx, it is recommended:
- avoid casual relationships, use barrier methods of protection (condoms);
- plan your pregnancy so you don’t have to do a curettage;
- eat right, food should be rich in vitamins and minerals to improve overall immunity;
- lead a healthy, active lifestyle;
- exercise.
Such preventive measures will help increase overall immunity and avoid contracting various infections. If infection does occur, you cannot treat yourself. You need to see a doctor to undergo a full diagnosis and course of treatment. Inadequate therapy for STDs leads to chronicity of the process.
Source: https://AltraVita-IVF.ru/informatsiya-dlya-patsientov/spravochnik-zabolevanij/gidrosalpinks-sz.html
Symptoms and consequences of the disease
Hydrosalpinx occurs with elevated temperature and is accompanied by nagging pain. If these symptoms appear, you should consult a doctor. The disease can lead to primary or secondary infertility, so it should not be left without due attention.
Every year, more and more women hear the disappointing diagnosis of hydrosalpinsk. But in fact, a person far from medicine cannot always understand what this term means, what the consequences of this disease are and how treatment should be carried out to eliminate this problem. Since the disease can lead to the inability to get pregnant, it is very important to understand all the nuances and aspects so that no difficulties or problems arise later.
Symptoms and treatment of chronic and acute salpingoophoritis
Salpingoophoritis (adnexitis) is an inflammatory disease of the uterine appendages, including the ovary, fallopian tube and adjacent tissue. The name of the disease is derived from two Greek words: salpinx (tube) and ooforon (ovary). This is a fairly common pathology that affects girls and women at any age. Most often, salpingoophoritis occurs in young women who are sexually active.
According to the clinical course, acute salpingoophoritis is distinguished, occurring with severe symptoms; subacute with a blurred clinical course and chronic, lasting more than 2 months, accompanied by alternating exacerbations and remissions.
Leading specialists in the treatment of hydrosalpinx in the Southern Federal District
Ermolaeva Elvira Kadirovna is a well-known and recognized specialist in the North Caucasus in the treatment of hydrosalpinx without surgery. She is a gynecologist, ultrasound doctor, physiotherapist-resortologist. Elvira Kadirovna is approached by women who want to improve the aesthetics of the genital organs, reduce the size of the vagina and refresh intimate relationships from all regions of Russia and foreign countries.
Ermolaev Oleg Yurievich Candidate of Medical Sciences, gynecologist-endocrinologist, operating gynecologist with 25 years of successful experience in treating hydrosalpinx without surgery. Able to see relationships that elude others.
Shchepkin Petr Sergeevich Gynecologist, specialist in the treatment of hydrosalpinx, treatment of sactosalpinx, treatment of pyosalpinx. Experienced ultrasound doctor.
About the doctors of the Clinic in detail...
| INTERNATIONAL RECOGNITION of the reputation and achievements of the Women's Health Resort Clinic in the development and implementation of effective and safe treatment methods and the quality of medical services provided is the AWARDING of the Women's Health Resort Clinic in Pyatigorsk with the SIQS International QUALITY CERTIFICATE in the field of medicine and healthcare. International Socratic Committee, Oxford, UK and Swiss Institute for Quality Standards, Zurich, SWITZERLAND. |
The resort clinic for women's health operates on a paid basis and in the voluntary health insurance system.
We work WITHOUT WEEKENDS and holidays:
Monday - Friday from 8.00 to 20.00, Saturday, Sunday, holidays from 8.00 to 17.00.
Treatment of hydrosalpinx by appointment by multi-line phone number 8 (800) 500-52-74 (toll-free within Russia), or +7 (call from anywhere in the world).
| ONLINE information about the treatment of hydrosalpinx WITHOUT SURGERY can be found at: BOOK ONLINE for hydrosalpinx treatment WITHOUT SURGERY here. REGISTER online for hydrosalpinx treatment here. Buy a course for the treatment of hydrosalpinx by calling +7 or here. |
Make an appointment with a gynecologist
We are at your FULL DISPOSAL if you have any doubts or wishes.
Reviews from women about treatment using different methods
I'll tell you my story about hydros. 4 years of infertility, laparosis, obstruction and fluid in both tubes (plastic surgery was done), it was no longer possible to get pregnant, there were tears, endless doctors and their treatments, in a word, in the fifth year of not being pregnant, my husband and I went to an eco clinic for a consultation. In general, nothing prevented us from starting the protocol, of course, after preliminary standard examinations. Ultrasound on different days of the cycle did not detect hydros. They started a long protocol, they injected me with defereline, and I went home to wait for my period. There is a delay, the test is positive, the doctor is horrified. The doctor warned me not to tempt fate and to take precautions, but I thought that getting pregnant naturally was not my case. Further pain, absence of the heel in the uterus, surgery, they removed the tube from the heel and checked the other one, at that time it was normal. Then there was a hormonal imbalance due to stress. Then 3 months of hormones and everything got better. I’m going on a short protocol, so far everything is fine, that’s how it was on the ultrasound. Although the doctor suggested postponing it because it was incredibly hot, the clinic closed for 2 weeks of vacation. I went on a short protocol, the last one that month before the clinic closed. As a result, she became pregnant and gave birth to a healthy girl, now she is almost 3 years old. I’m planning a second one, and the ultrasound showed hydros at the only tube, although I did an ultrasound every six months to a year, but the ultrasound specialist said the volume of fluid is small and can be treated conservatively, does anyone believe in this? They prescribed a mountain of pills and got pregnant after a control ultrasound and after stopping the OC.
vika1111
https://www.babyplan.ru/forums/topic/43740-gidrosalpinks/page__st__680#ixzz4b0Z4UHue
Good day! I’ll tell you my story... I’ve been together with my husband for 7 years, we started planning right away, we ran to the doctors, in 2010 they discovered hydrosalpinx, she cried, gave up, at first she was treated as an inpatient, then she had tubal plastic surgery, minimal chance of a natural pregnancy. I went to a sanatorium and was treated with mud, leeches, and irrigation. I brought BM and KSH from Altai, made mud compresses at home, some microenemas from antlers... in short, I decided not to give up. We were already getting ready for IVF, but at the last moment we changed our minds and rushed to the sea. Before my vacation, I decided to use a Chinese tampon. We arrived, the tests were empty. A month later I came home from work, took out the tampon, did a test... and it was Positive! !,! At 7 weeks, during an ultrasound, we saw fluid in the tube again, but it was no longer dangerous for my baby. And now we are 3 months old. Dear girls, believe, hope, fight, and do as your soul and Heart command! I wish you all to become mothers
Ryzhik //
https://www.babyplan.ru/forums/topic/43740-gidrosalpinks/page__st__680#ixzz4b0ZaXSIN