Acute pain inside the jaw and swelling of the gums often mean that a person has developed periodontitis. This is a serious inflammatory problem in which the focus is located at the very top of the tooth. It is rarely diagnosed as an independent disease and is often a consequence of advanced caries and poor oral hygiene. It has many symptoms and manifestations and must be distinguished from periodontal disease and gingivitis. Only the dentist should carry out diagnostics and select the necessary treatment.
What is dental periodontitis?
When faced with such a diagnosis for the first time, the patient, first of all, wants to get an answer to the question - what is dental periodontitis?
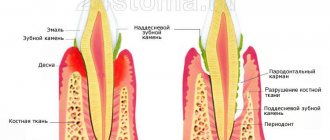
This disease is a chronic inflammatory process in the membranes surrounding the apex of the root of the dental unit and ensuring its reliable fixation in the jaw bone.
Over time, there is a gradual destruction of the periodontal structure and the formation of a purulent focus at the apex of the affected root. Inflammation, which characterizes the development of periodontitis, rarely occurs against the background of complete well-being. In most patients, bone loss in the periapical region occurs as a result of the presence of a chronic source of infection in the dental pulp.
Causes
The main reason for the development of periodontitis is the breakdown of nerve fibers and damage to the ligament that holds the tooth. This is what explains the painful mobility of the dentition, discomfort when touching and chewing. Body temperature may rise, and sometimes with periodontitis, regional lymph nodes increase in size.
In some cases, the pathology can be completely painless - with bone resorption in the root area and the formation of a granuloma, which visually looks like a sac on the apical part of the tooth. In more serious cases, cavities - cysts - may form, requiring long-term and complex treatment, which does not always help save the tooth.
With periodontitis, complications may develop from internal organs and body systems - glomerulonephritis, damage to heart valves, joints.
Very often, the main reason for the development of periodontitis is improper, poor-quality root canal treatment.
In this case, the photographs will show channel cavities and fragments of instruments.
Such teeth need to be extracted; it is not necessary to remove them - a good doctor will do everything possible to save the root. The main component of treatment is ultrasound, antiseptic treatment.
Based on their origin, periodontitis is divided into infectious and non-infectious. In the first case, the inflammatory process is caused by microorganisms and their metabolic products. Bacteria penetrate through the periodontal root canal, where they can reach lymphogenous and hematogenous nodes. Infectious periodontitis is the result of acute diffuse, chronic gangrenous pulpitis, necrotic degenerative changes in tissues.
Non-infectious periodontitis is the result of chronic or immediate injuries - bruises, improper pulp extraction, sharp biting of hard foods. Chronic injuries are quite common among smokers who use pipes, wind players, and those who like to bite threads with their teeth. Also, pressing with a pen on the tooth or placing the filling too high can also play a cruel joke. Aggressive chemicals like formalin cause chemical periodontitis when the root canals expand.
Provoking factors
The existing classification of periodontitis provides not only the clinical picture of the development of the pathology, but also the causes of its occurrence. Considering the type of factor that caused the formation of a focus of inflammation in the area of the apex of the root of the affected tooth, the following types of disease are distinguished:
- Infectious . In this case, the pathological process is caused by the penetration into the periodontium of toxins released during the life of pathogenic microorganisms and decay products of non-viable pulp. In this case, bacteria can penetrate beyond the root apex not only through the root canal, but also during generalization of the inflammatory process from nearby tissues, for example, if the patient has a history of sinusitis.
- Traumatic . In this case, periodontitis can occur as a result of a single damaging effect on the tooth (biting hard objects, blows, bruises) or due to chronic microtrauma (inflated filling, direct bite, etc.).
- Medicinal . Periodontitis develops as a complication of improper treatment of pulpitis - exceeding the time limit for applying arsenic paste to the inflamed pulp, removing filling material, pins, etc. beyond the root apex. An increased reaction of the patient’s body to the components of dental materials can also provoke the appearance of a chronic focus of inflammation in the periapical area.
In a child, periodontitis of a baby tooth develops for the same reasons as in adults.
Prevention of periodontitis
Maintain good oral hygiene, do not ignore brushing your tongue, change your toothbrush on time and use floss. Visit the dentist once a year; oral hygiene and professional teeth cleaning will help maintain your teeth and a snow-white smile.
The main thing is not to let the disease progress and when the first alarming symptoms appear, consult a dentist. Under no circumstances should you heat a sore tooth. Heat will only accelerate the spread of inflammation, and the pain will intensify. The only chance to cure periodontitis and save a tooth is qualified dental care!
Quantity
Clinical forms of the disease
Depending on the nature of the pathology, periodontitis is divided into acute and chronic. Additionally, dentists, taking into account the development phase of the infectious process, distinguish subtypes of each of these types of pathology.
Acute periodontitis is divided into:
- Serous - local areas of dilated capillaries form around the apex of the affected tooth root, in which there is an accumulation of protective blood cells. The inflammatory reaction causes the formation of limited periodontal edema and the appearance of pain.
- Purulent - small foci filled with purulent contents appear in the periapical region, which increase in size over time and merge into one foci of suppuration. The patient complains of intense pain and mobility of the damaged tooth.
Chronic periodontitis can be:
- Fibrous – as a result of a prolonged inflammatory reaction, scarring of periodontal tissue is observed. This form of the disease has the most favorable prognosis, since it rarely leads to an exacerbation of the pathological process.
- Granulating - in the focus of inflammation there is random destruction of bone structures and active proliferation of connective tissue.
- Granulomatous - a capsule forms in the area of the apex of the affected tooth root, as a result of which the source of inflammation is delimited from the surrounding tissues. Inside the capsule, the bone tissue is destroyed.
The most pronounced clinical picture is characterized by chronic granulating periodontitis .
What is the difference between pulpitis and periodontitis?
Similar symptoms of pulpitis and periodontitis arise from the inflammatory nature of these diseases. In both cases, dental tissue is affected. The differences lie in the localization of the process and visible manifestations of pulpitis:
- Regardless of the stage, the source of inflammation is concentrated in the pulp - the soft tissue inside the crown. No changes are observed in the surrounding areas; the crown is firmly held in the alveolus.
- The specific difference between pulpitis and periodontitis is the acute reaction of the diseased tooth to a temperature stimulus and the absence of discomfort when tapping.
- There is no pronounced difference between the color of the crown and the general tone of the dentition.
- Opening the pulp in the chronic form of the disease is extremely painful, the area bleeds slightly.
Since periodontitis is often a complication of pulpitis, an accurate diagnosis is made after a differentiated examination.
Symptoms
When a patient develops periodontitis, the symptoms and treatment of the pathological process are determined by its clinical form. The main sign of the formation of acute periodontitis is the occurrence of acute pain in the affected tooth (increased reaction to the slightest touch to the crown of the tooth) and the appearance of a feeling of “pushing out” of this unit from the jaw.
The accumulation of exudate in the periapical area and the appearance of purulent contents cause an increase in the intensity of pain and its irradiation to surrounding areas (ear, temporal and infraorbital areas). If pus comes out - through the root canal or holes in the periodontium - the patient feels sharp relief and attenuation of pathological symptoms.
Otherwise, there is a deterioration in the general condition of the patient - an increase in body temperature to critical levels, the formation of edema of the soft tissues of the face. In the absence of qualified assistance, extremely dangerous complications may develop - osteomyelitis, phlegmon, sepsis.
With the development of chronic periodontitis, the clinical manifestations of the pathology are as follows:
- change in the color of the crown of the affected tooth - over time, the enamel becomes darker and darker;
- periodic occurrence of dull aching pain due to mechanical pressure on the dental unit. In addition, during a medical examination, pain of varying intensity occurs when lightly tapping the dental crown;
- formation on the gum in the projection of the roots of a fistula (vesicle with purulent contents);
- mobility of the affected unit.
Quite often, with the development of chronic periodontitis, the patient complains of bad breath.
Symptoms of periodontitis
The development of periodontitis often occurs without symptoms, as a result of which patients end up in the doctor’s office when the disease is at an advanced stage and requires a complex removal procedure. If you notice that:
- Teeth periodically hurt when closing the jaws.
- Visually, the teeth began to appear larger.
- At night, the gums begin to ache, and the body temperature begins to rise.
It is recommended to visit a specialist's office because these are all signs of periodontitis formation. It can be recognized independently by a change in the color of the gums: as a result of the inflammatory process, they become darker and sometimes bluish.
The above symptoms are characteristic of the initial stage. Advanced periodontitis can be identified by the following symptoms:
- The appearance of tooth mobility.
- Swelling in the gum area, and sometimes in the cheeks.
- Acute pain when eating.
The presence of these signs suggests that a significant amount of pus has accumulated around the tooth root, putting pressure on the soft gum tissue. The lack of medical intervention at the initial stage will lead to the release of these masses and the subsequent spread of microbes. But not every type of periodontitis has such serious consequences, which is why it is worth paying increased attention to the classification of the disease.
Types of periodontitis
Dentists classify periodontitis according to several parameters - the degree of development of the disease and the location of infection. According to the location of the inflammatory process, periodontitis is divided into:
- Apical, affecting the area near the edge of the tooth root.
- Regional, developing in the soft tissues of the gums.
The appearance of the apical form of the disease is a consequence of improper or untimely treatment of pulpitis, then the marginal form develops due to injury to the soft gum tissue.
Dentists distinguish between acute and chronic types of periodontitis. The acute form is the initial stage, and appears in the appearance of pain during pressure, as well as swelling of the gums. Acute periodontitis has two stages of formation:
- Serous, during which pain appears sporadically, but the tooth stands firmly in its rightful place.
- Purulent, when unpleasant sensations become frequent, and the tooth begins to loosen, releasing purulent discharge.
If left untreated in the acute stage, it will become chronic, which has three different variations:
- The fibrous form of chronic periodontitis is initial and almost invisible - the pain is unsystematic or completely absent, and the presence of an inflammatory process can only be determined using an x-ray.
- Granulating is the most common form in dental practice. Its course is associated with constant pain, severe swelling and discharge of pus from the gums.
- Granulomatous - more serious than all the others. As the disease evolves to this stage, granulomas are formed in the soft tissues - gum voids that are filled with pus, which is an ideal environment for microbial life. They are actually a time bomb and can only be removed surgically.
The abundance of varieties requires a variety of treatments and a set of measures aimed at eliminating the disease.
Diagnosis of periodontitis
Diagnosis of periodontitis involves the following measures:
- careful collection of anamnesis and identification of patient complaints;
- examination of the crown of the affected tooth - clarification of the degree of its destruction and changes in enamel staining;
- conducting electroodontometry - to determine the threshold of excitability of pulp tissue. The lower it is, the greater the risk of an inflammatory reaction or necrotizing process;
- radiography – using the resulting photo of the affected tooth, the dentist identifies characteristic changes in the pattern of bone tissue in the periapical area, even in the case of asymptomatic development of the disease. By studying the image, the doctor can not only assess the severity of the inflammatory reaction, but also suggest possible causes of its occurrence. Taking into account the X-ray data, the dentist develops appropriate treatment tactics for periodontitis.
In some clinical cases, the doctor may additionally prescribe the patient a clinical blood test.
Treatment options
Let's consider the main methods of treating periodontitis, taking into account the form and stage of the disease.
Conservative
The tactics of action in this case depend on the severity of the clinical symptoms and the causes of the development of the pathology.
At the initial stages, pastes are used that absorb granulomas and cysts, which trigger regeneration processes in bone tissue.
In the later stages, a temporary tooth filling is used, but you will have to visit the dentist much more often to refill and replace medications; moreover, doctors do not give any guarantees of successful treatment (for example, a patient wants to save a tooth with advanced periodontitis, and the dentist suggests he try conservative treatment ). When the canals are cured, a permanent filling is performed.
Root apex resection
It is resorted to in exceptional cases, since the doctor does everything possible to preserve the root. Resection allows you to remove the cyst without affecting the tooth itself. The main disadvantage of the operation is that it violates the integrity of the root, which becomes mobile and can become loose. Partial removal of the apex on multi-rooted teeth gives good results, but you will still have to chew with them with caution in the future.
Resection involves creating an incision, trephination, excision of the root tip and suturing. If the granuloma or cyst is large enough, bone grafting will have to be done for further implantation.
If conservative therapy is not possible, resection of the apex of the tooth root is performed.
In especially severe cases, hemisection of the tooth may be used. This is an operation to remove the damaged part of the tooth and then install a crown.
Features of treatment of acute form with the presence of ulcers, abscess
In acute periodontitis, the canals must first be cleared of exudate. Drainage of the periodontal gap is carried out through the root canal, gum pocket or hole left after extraction. If these drainage techniques cannot be used, the dentist makes an incision along the transitional fold.
An incision along the transitional fold is a traumatic but effective technique. It also helps with complications from abscesses.
Antibiotics are prescribed in cases where the symptoms of intoxication are severe. The main group of drugs is sulfonamides.
For severe pain, analgesics can be used; for autointoxication and sensitization, a 10% calcium chloride solution, clemastine or another antihistamine is prescribed.
All manipulations must be carried out under anesthesia; tooth trepanation and filling removal are carried out with high-speed turbine burs. For pain relief, conduction and infiltration anesthesia with a solution of lidocaine, ultracaine at a concentration of 2% is suitable. Acute phenomena are well relieved by decoctions of chamomile, eucalyptus, and soda rinses.
Root canal treatment
When the inflammation subsides, instrumental and medicinal treatment of the canals is carried out. In the absence of exudation, percussion and palpation will be painless.
The canal should be filled at the apical level.
If exudate continues to be released, the cavity is drained. Multi-rooted teeth often have difficult and/or crooked canals, making them difficult to drain. In this case, instead of drainage, you can use silver plating, the resorcinol-formalin method, electrophoresis or anode galvanization. Then the tooth is closed as tightly as possible for 3-4 days, the canals are filled with paste with resorcinol and formaldehyde.
In some cases, tooth pain after root canal cleaning can persist for up to a week. This is an absolutely normal process after invasive intervention. If the discomfort continues for a longer time, this is a clear reason for a repeat visit to the dentist.
Features of treatment of the medicinal form
Therapy for the medicinal form of the pathology begins with eliminating the provoking factor. The goal of treatment of drug-induced periodontitis is to reduce the degree of periodontal intoxication and reduce the volume of exudate released. This is achieved through fractional removal of purulent and other contents of the root canals through mechanical treatment, the use of antidotes, and drugs that reduce the separation of exudate. In case of arsenic periodontitis, which occurs more often than others, the amount of exudate can be reduced through the use of iodine-containing preparations, a solution of nitrofural with hydrocortisol 0.15%.
Elimination of exacerbation of chronic periodontitis
For exacerbations of chronic periodontitis, physical and impregnation treatment methods are used. After suffering from periodontitis, any injury or hypothermia can lead to relapses, and they are already fraught with tooth extraction and the need for prosthetics.
Treatment of periodontitis
Treatment of periodontitis, regardless of its clinical form, is aimed at eliminating the inflammatory reaction in the area of the apex of the affected tooth. To do this, the dentist opens the tooth cavity and completely removes the softened tissue. After this, the doctor expands the root canals and thoroughly cleanses them of infected contents and decaying pulp tissue.
Depending on the degree of development of the pathological process, endodontic treatment of the tooth can be carried out over several visits to the patient. To disinfect root canals, antiseptic agents such as 3% hydrogen peroxide solution and enzyme solutions are used. To facilitate expansion and mechanical cleansing of the root canal, the dentist uses preparations made on the basis of EDTA.
For a therapeutic effect on the affected periodontium, a drug with an anti-inflammatory effect is left in the root canals for 1.5 weeks. The tooth cavity is closed with a temporary filling. If during this period the patient notices a decrease in the intensity of the symptoms of the disease, the dentist re-rinses the root canals and fills them with hardening pastes or gutta-percha pins.
After the canals are sealed, the doctor must carry out x-ray control to prevent the filling material from leaving the apex of the tooth root. To prevent complications, it is recommended to repeat x-ray examinations every 3 months for the next year after treatment.
The complexity and duration of the treatment process in the case of inflammation in the periapical region depend on the stage of development of the pathology, the size of the pathological focus, the anatomical features of the structure of the affected tooth and the age of the patient.
In most clinical cases, the development of periodontitis occurs over a long period of time. It is much easier to prevent the penetration of pathogenic agents into the periapical area than to subsequently stop the inflammatory process. Prevention of periodontitis involves timely treatment of caries and regular dental examinations.
Why does periodontitis form on the gums?
Many people ignore doctors' advice to visit the dental office every 6 months. Such preventive examinations help to detect caries or other enamel damage in a timely manner. Any chips create conditions for infection to enter and develop deep into the periodontal tissue. In the vast majority of cases, periodontitis is a consequence of inflammatory diseases such as periodontal disease, gingivitis, pulpitis, and a cyst on the root of the tooth.
Conventionally, several causes of the disease can be identified:
- Infectious : dangerous microbes enter the gums with the bloodstream from the internal organs, with ARVI, influenza or bacterial sore throat from the nasopharynx. Periodontitis with pus can become a complication of scarlet fever, diphtheria, sinusitis or measles.
- Contact : occurs when there are crowns in the patient’s mouth that are heavily damaged by caries. Food particles and pathogenic pathogens from saliva remain in such a cavity. They decompose, and decay products accumulate in the dental canals. These are the prerequisites for the development of fibrous and granulosa forms.
- Medicinal : the infection is often caused by the dentist when performing manipulations on the gums. Sometimes careless or inept cleaning of the canal ends with dental material getting into it. Arsenic or acids destroy teeth and periodontal tissues, causing them to fester. With caution, the doctor should use such agents as phenol, formalin, and special pastes with an antiseptic.
Studies of identified cases of periodontitis have shown that it is more often diagnosed in people with chronic diabetes mellitus, intestinal pathologies and stomach ulcers, and problems with the thyroid gland. The formation of a purulent focus is affected by decreased immunity, frequent colds and prolonged stressful situations.
The only way to diagnose the disease is still radiography. The image shows darkening at the root of the tooth and provides information about the condition of the jaw bone tissue. It is important to know whether there is a cyst or fibrous formation, and whether the tooth can be saved from removal.
Types of periodontitis
Periodontitis can be marginal, acute, apical, traumatic, chronic. The chronic form is fibrous, granulomatous, granulating. Sometimes dentists diagnose retrograde periodontitis, which appears due to tooth infection.
The types of disease also include traumatic acute periodontitis, which occurs when there is heavy load on the dentition or when there is a lack of teeth. This type of disease often progresses to periodontitis, affecting the gums and bones. This is a very severe form of the disease that can cause sepsis and tissue necrosis. In this case, it is very important to provide timely effective treatment and prevent extensive tissue destruction.
Forms of the disease
As mentioned above, acute periodontitis is presented in serous and purulent forms, the latter can be classified as follows:
- Periodontal stage. It is characterized by the sensation of an overgrown tooth, which is associated with the formation of a microabscess as a result of the action of pus.
- Enodoosal stage. It occurs with the penetration of pus into the bone tissue, where the process of infiltration subsequently occurs.
- Subperiosteal stage. Swelling of the face and gums as a result of the accumulation of pus under the periosteum, the formation of gumboil and severe pain.
- Submucosal stage. Due to the destruction of the periosteum, pus flows into the soft tissues, the pain subsides a little because of this, but the swelling of the face increases.
Forms of periodontitis
Periodontitis can occur in three forms: acute, chronic, or exacerbation. Each of them has features in the clinical picture, prevalence and evaluation criteria, according to which doctors are able to make the correct diagnosis and choose treatment methods for periodontitis.
Acute periodontitis
Acute periodontitis is not a rare diagnosis in dentistry. Acute inflammation - occurs for the first time and due to severe pain, patients rush for help. Based on the symptoms, doctors can determine the type of acute inflammation, and after examination, understand whether it really has arisen for the first time, or whether it is an exacerbation of chronic periodontitis.
Patients should understand that there are different types of even acute inflammation, and they are treated differently. Therefore, it is necessary to give complete answers to questions, and if there has been pain in the tooth before, be sure to inform the doctor about it.
Chronic periodontitis
Chronic periodontitis can be asymptomatic, and the patient’s complaints are related only to aesthetics: the tooth has become gray, seems lifeless, and there is a deep carious cavity on its surface. Some forms of chronic inflammation have symptoms, but more often patients ignore them: discomfort when biting on the causative tooth, a fistula in the present or past.
The danger of chronic periodontitis lies not only in the possible exacerbation, but also in the fact that a potential source of infection for the entire body is formed and maintained. Such conditions are especially dangerous in pediatric practice.
Exacerbation of periodontitis
With an exacerbation of periodontitis, symptoms characteristic of the acute form appear: pain, poor general health, swelling of the face, but there are also differences with the symptoms of acute periodontitis. Treatment of the disease in the acute stage is significantly different from that in the acute form, so patients should tell the doctor whether there were symptoms and pain before today, and accurately describe its nature. Instrumental and visual research methods will help make the correct diagnosis.
Treatment methods
Periodontitis must be treated! Moreover, both in acute and chronic forms, the disease requires close attention. If you do not deal with this problem, then you cannot avoid serious complications - periostitis of the jaw (flux), osteomyelitis (purulent-necrotic process) of bone tissue, abscess, acute sinusitis and even the development of sepsis in response to a local infectious process.
We must not forget that in the immediate vicinity of the oral cavity there are the eyes and the human brain, where infection and pus can spread through the bloodstream. Therefore, you should immediately contact your dentist if symptoms of periodontitis appear.
There are traditional methods for treating this pathology, but given the nature of the lesion, they can only act as an effective adjuvant to the main therapy.
First, the doctor will necessarily open the tooth to provide good access to the inflamed periapical tissues that are located behind the root of the tooth. Under anesthesia, he will mechanically clean the canals , change their length if necessary, treat them with an antiseptic, introduce the necessary antibacterial drugs (for example, lincomycin), which will stop inflammation, stop further tissue destruction and promote their speedy recovery. It is not a fact that a one-time administration of the medicine will help. Periodontitis usually requires several treatment sessions. All this time the tooth remains open or under a temporary filling.
After the pain subsides and the inflammation subsides, the doctor will place a permanent filling and take a control x-ray. Tissue regeneration processes will be completed in approximately 6-10 months. Then we can assume that periodontitis has been defeated.
In difficult cases, for example, with the development of a cyst or fistula formation, a more radical method of treatment is required - surgery. Conservative treatment of a cyst - drainage of the cystic cavity, elimination of pathogenic microflora, destruction of the internal lining of the cyst - is a long process that does not always end in success.
Physiotherapeutic procedures and warm soda 15-minute baths up to 7-10 times a day are effective.
Modern dentistry is one of the most progressive areas of medicine, therefore in 85% of cases there is a complete cure of periodontitis while maintaining the anatomical integrity and functions of the tooth.
Prevention
To avoid any form of periodontitis, you must follow simple recommendations from dentists, which apply to most clinical cases:
- You need to brush your teeth at least twice a day - the brush should not be too hard, so as not to injure the gums or introduce infection into the soft tissues.
- After each meal, use mouthwash - if you don’t have a special liquid on hand, just rinse your mouth thoroughly with warm boiled or filtered water.
- Visit the dentist at least 2 times a year - a scheduled appointment allows you to identify most diseases in the early stages, begin treatment in a timely manner and avoid serious consequences.
- Have your teeth professionally cleaned and tartar removed annually – even minor plaque creates conditions for the proliferation of pathogenic bacteria.
General advice for everyone includes giving up bad habits. Smoking and alcohol contribute to the deterioration of dental health, as well as their attractiveness and natural whiteness.
Treatment
The treatment of acute periodontitis is based on a conservative approach. This treatment gives a positive result in almost eighty-five percent of cases. The main principle is to stop inflammation, prevent further spread of infection and restore tooth function.
Conservative treatment of apical periodontitis
Treatment should be comprehensive and include:
- drainage of the cavity with removal of dead tissue;
- prescription of antibacterial drugs, both local and systemic;
- physiotherapy;
- immunomodulatory and restorative agents to increase the overall resistance of the body and speedy tissue regeneration.
All manipulations are carried out after thorough anesthesia with a solution of Lidocaine or Ultracaine.
Opening the cavity and removing exudate and necrotic tissue is a mandatory step, since with limited access it is impossible to fully influence the lesion with antibacterial agents.
Chlorhexidine, Miramistin, Furacillin, Ectericide, etc. are used to wash the canals.
After the inflammatory reaction subsides, the canals are filled. A short course of broad-spectrum antibiotics (Ampicillin, Augmentin, Suprax) and non-steroidal anti-inflammatory drugs (Nimesulide, Ibuprofen) are prescribed internally. A good effect is achieved by combining the therapy with physiotherapy: laser, UHF, magnetotherapy.
If conservative therapy is ineffective or there is significant damage to the tooth, it is removed.
Treatment at home
When pain occurs, use an anesthetic, for example, Analgin, Ketorol, etc. You should rinse the mouth with a soda solution in order to remove food debris from the carious cavity.
Photo 1. Analgin in the form of tablets, 20 pieces per package, 500 g, .
Next, you need to apply a cotton swab soaked in medical alcohol to the area where the pain syndrome is most manifested.
Important! Treatment at home is possible only at the initial stage of the disease, using antibiotics and antiseptics.
What is periodontitis?
In medicine, this disease is defined as follows: periodontitis is an inflammation of the periodontium, that is, the connective tissue between the cortical plate of the tooth socket (alveoli) and the cementum of the tooth root. The thickness of the periodontium is different for everyone, on average it is 0.19-0.26 mm.
Simply put, with the development of periodontitis, the area of tissue that surrounds the root of the tooth and is responsible for its stability becomes inflamed. The periodontium is closely connected with the surrounding tissues: along its entire length - with the jaw bone, through the apical foramen - with the pulp, at the edges of the tooth socket - with the periosteum and gum.
The disease is characterized mainly by damage to the ligaments that hold the tooth in the alveolus, degradation of bone tissue of varying severity, resorption (destruction) of the walls of the tooth socket and even root cement.
According to statistics, this is a common disease, diagnosed in 45-50% of cases of dental problems. Periodontitis never occurs out of nowhere. As a rule, it is a consequence of untreated caries. The disease is quite serious, it is not so easy to cope with, it has a negative effect on the entire human body and can cause such serious complications as an abscess, acute sinusitis, osteomyelitis, periostitis or sepsis.
Causes of acute periodontitis
There are a number of conditions that are etiological factors in the development of the disease, these include:
- mechanical damage to the tooth and surrounding tissues;
- inflammation of the dental pulp – acute apical periodontitis of pulpal origin;
- carious lesions of teeth;
- exposure to toxic and toxic substances;
- ingress of infectious agents - often coccal and fungal microflora;
- spread of the inflammatory process from neighboring organs when the maxillary sinuses and gums are affected.
The leading role in the pathogenesis of acute periodontitis is played by the entry of viruses, bacteria, protozoa, and fungi into the tooth cavity and nearby tissues; they spread through the periodontal pocket and the apex of the tooth. During development, pathogens can release endotoxins that negatively affect all anatomical and physiological structures. The inflammatory process begins, the body’s immune defense cannot cope with the damage. In advanced stages, destructive changes appear.
Periodontitis in children
In childhood, they develop as a result of untreated caries, damage to teeth from falls and blows, and the penetration of infection from another inflammatory source in the body. In addition, this pathology may be a consequence of systemic or autoimmune damage to connective tissue.
It must be said that the symptoms of periodontitis among children have certain differences from similar damage to permanent teeth. Thus, in the presence of immature tooth roots, an exclusively granulating form of the disease develops. In acute cases, the general condition of the child may be disrupted. The chronic form of the lesion, as a rule, develops primarily without an acute stage.
Another feature should be mentioned that a pronounced inflammatory process in the periodontium can be caused by even a minor carious defect or occur even when the tooth cavity is closed. If treatment is not carried out on time, various complications arise. For example, the rudiments of permanent teeth are damaged, which leads to edentulism (complete or partial absence of teeth). Premature eruption of permanent teeth and the development of periostitis or osteomyelitis are also possible.
Causes of the disease
Acute periodontitis occurs with the active development of pathogenic microorganisms: streptococci, staphylococci, actinomycetes and yeast-like fungi.
Microbes and their toxins cause necrosis and inflammation of the pulp and subsequently affect the periodontal tissues. Most often, patients aged 20-45 years experience acute periodontitis. There are several reasons for the development of inflammation in the periodontal tissues:
- infectious infection,
- mechanical injuries,
- destructive effects of chemicals.
Up to 98% of cases of acute periodontitis occur in an advanced form of caries, which leads to pulpitis. From the pulp, inflammation spreads to the periodontal tissues through the apical openings of the root canals.
Diagnostics ↑
Diagnosis is not difficult.
The presence in the past of throbbing pain, intensifying at night (history of pulpitis) or a significant defect in the crown of the tooth, painless on probing, speaks in favor of acute periodontitis.
Severe pain that intensifies when you touch the tooth allows you to verify the correctness of this diagnosis.
Differential diagnosis should be carried out with:
- Acute pulpitis.
With pulpitis, the pain pulsates, has a paroxysmal character and does not change with percussion; with periodontitis, strong, tearing and continuous, aggravated by touching the tooth; - Exacerbation of chronic periodontitis.
The best way is an x-ray; in acute periodontitis there are no changes in the periodontal area; - Osteomyelitis.
The lesion is extensive, covering the roots of several teeth. Therefore, severe pain occurs when percussion occurs on several adjacent teeth.
Read about the correct use of Hexoral spray for children. How to get rid of caries on teeth? Recommendations here.
What are the causes of acute traumatic periodontitis? Find out in this article.
Development mechanism
At the periodontal stage of the disease, its focus is not associated with other areas of the periodontium, but as the inflammatory process increases, they merge and damage most of the periodontium. In its confined space, an increase in pressure is observed and, as a result of an inevitable breakthrough, exudate penetrates into the bone spaces of the jaw. This breakthrough leads to a relief of pressure and a decrease in pain, accordingly, the patient experiences relief, however, the inflammation does not stop and if treatment is ignored at this stage, then this process spreads to the periosteum.
At the subperiosteal stage of acute periodontitis, the periosteum, due to its dense structure, withstands the pressure of the exudate for some time. At this moment, patients observe the appearance of a fairly significant swelling in the area of the apex of the tooth root, bringing with it painful sensations. When, over time, a breakthrough of the periosteum occurs, the exudate rushes to the oral mucosa, where it does not meet any serious resistance. As a result, a fistula forms and pus flows out, as a result of which the painful sensations significantly weaken until they disappear. Naturally, the inflammatory process does not stop, we are talking exclusively about external manifestations, and its course can lead to various complications, including osteomyelitis.
Features of non-surgical treatment of periodontitis at the Healthy People clinic
provides surgical treatment of chronic periodontitis and its chronic stage at an affordable cost. The clinic’s dentists select a treatment option that will suit the patient’s capabilities and condition.
They try to cure almost all forms of periodontitis without surgery. This allows you to avoid wasting time and money and achieve maximum effect.
The cost of treatment can be found out by calling the Healthy People clinic or looking at the website in the prices section.