Clinical symptoms diabetic retinopathy are present in approximately 10% of diabetic patients. However, some degree of it can be detected in more than 80% of patients receiving insulin. Fluorescein angiography, which reveals areas of altered permeability and vascular disorganization, often allows one to see severe circulatory disorders. Therefore, the retina serves as a very convenient place in which the presence of structural and functional microangiopathy can be assessed based on the state of microcirculation (figure below).
Pathogenesis and causes
The pathogenesis of diabetic retinopathy is quite complex. Among the main reasons are damage to the blood vessels of the retina: their excessive permeability, blockage of capillaries, the appearance of proliferative (scar) tissue and newly formed vessels. Such changes are caused by genetic features of the structure of the retina.
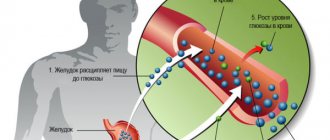
Metabolic changes that occur with elevated blood glucose levels play an important role in the development of the disease. In the presence of diabetes for up to 2 years, diabetic retinopathy is detected in 15% of patients; up to 5 years – 28%; up to 10–15 years – in 44–50%; from 20 to 30 years – in 90–100%.
Risk factors that influence the rate and frequency of disease progression include:
- level of hyperglycemia;
- duration of diabetes mellitus;
- chronic renal failure;
- arterial hypertension;
- having excess weight (obesity);
- metabolic syndrome;
- dyslipidemia.
Pregnancy, puberty, and bad habits also contribute to the development and progression of diabetic retinopathy.
Signs of retinopathy: how to understand that there is a problem?
Symptoms of retinopathy can be interpreted by a diabetic as normal fatigue of the eye muscles, which makes the disease even more dangerous. The initial warning signs of diabetic retinopathy are:
- Fogging. A kind of haze appears, clarity is disrupted, colors lose saturation and become faded.
- The appearance of “bunnies” before the eyes with diabetic retinopathy. Hovering dots, similar to those that appear in a healthy person when he closes his eyelids tightly.
- Bleeding into the retina. A blood rim appears around the pupil, somewhat reminiscent of a burst vessel.
- Deterioration of vision. It is observed already in the late, advanced stages of the disease.
You will not be able to confirm or refute the diagnosis on your own. Light fog and floaters may be symptoms of eye strain or increased dryness of the eye. Or, for example, improper use of lenses. A minor hemorrhage can easily be confused with a harmless burst vessel.
If you are one of the people suffering from diabetes, consult your doctor as soon as you suspect it. The presence of a problem can only be confirmed using computerized diagnostics.
Classification
There are several stages of the disease:
- initial;
- preproliferative;
- proliferative;
- terminal, or stage of final changes in the retina.
The initial stage of diabetic retinopathy is called non-proliferative. Occurs at any stage of the disease. It occurs in three phases.
- The first is vascular. It is characterized by phlebopathy and expansion of the avascular zone, the appearance of microaneurysms in areas of local capillary blockage.
- The second phase is exudative. It is distinguished by the occurrence of soft and dense exudates, muffs, edema in the macula (central zone of the retina), small single retinal hemorrhages.
- The third is hemorrhagic. It is accompanied by multiple hemorrhages, constriction of veins (they look like sausages), subretinal hemorrhages, the appearance of ischemic zones of the retina, and impaired permeability of the vascular wall.
If the non-proliferative form is not treated, it becomes pre-proliferative . At this stage, there are more changes in the retina. During the examination, the ophthalmologist detects traces of multiple hemorrhages, ischemic areas (areas in which blood circulation is impaired) and fluid accumulations. The pathological process affects the macula area. The patient complains of decreased visual acuity.
The proliferative stage of diabetic retinopathy is diagnosed in 5–10% of patients with diabetes. Provoking factors for its development include posterior vitreous detachment, high myopia, optic nerve atrophy and blockage of the carotid arteries. The retina suffers from oxygen starvation. Therefore, to maintain the required level of oxygen, new vessels are formed in it. This process leads to repeated retrovitreal and preretinal hemorrhages.
At the last (terminal) stage of the disease, massive hemorrhages occur in the vitreous body (hemophthalmos). Gradually more blood clots form. The retina stretches until it peels off. When the lens stops focusing light on the macula, complete loss of vision occurs.
Diabetic retinopathy
Diabetic retinopathy (DR) is a complication of diabetes mellitus that leads to irreversible damage to the vessels of the retina (plays a major role in vision).
DR can be asymptomatic for a long time, until significant damage to the retina occurs. The first symptoms may appear in one eye or in both eyes at once.
Pay special attention to:
- The appearance of ghosting of objects
- Blurred outlines of objects
- Difficulty reading any text
- Appearance of shadows around objects
- Appearance of a dark spot in the field of vision
- Color vision impairment
Risk factors
In order of importance, from most important to least important:
- Duration of diabetes mellitus: up to 5 years - incidence 9-17%
- from 5 to 10 years - 44-80%
- from 15 years - 87-99%.
Anyone who suffers from diabetes is a potential patient with diabetic retinopathy. For self-control, regularly perform the Amsler test.
Stages of diabetic retinopathy
There are three stages, depending on the degree of retinal damage:
- Stage I - Non-proliferative
- Stage II - Preproloiferative
- Stage III - Proliferative
1. Non-proliferative diabetic retinopathy
It is asymptomatic. When examining the fundus you can see:
- Angiopathy - changes in the caliber of blood vessels, dilation and tortuosity of veins
- Single solid exudates
- Microaneurysms
- Microbleeds
Treatment options
- Regular examination by an ophthalmologist - once or twice a year. Despite the fact that there is no decrease in vision, examination significantly reduces the development of complications such as macular edema, vitreous hemorrhages, and retinal hemorrhages
- Adequate control of blood glycemia (!)
- Compensation for associated risk factors for progression : arterial hypertension, cholesterol levels.
2. Preproliferative diabetic retinopathy
May be asymptomatic. There is a deterioration in the quality of vision: blurred contours, double vision, the appearance of a spot in the field of view, shadows around objects, difficulty reading, impaired color vision.
Diagnosis reveals:
- Soft and hard exudates
- Intraretinal microvascular anomalies (IRMA)
- Severe angiopathy - looping of venules, changes in the caliber of blood vessels
- Multiple hemorrhages
3. Proliferative diabetic retinopathy
The most severe form. Appears as:
a) Neovascularization - newly formed vessels, retina, optic disc.
Fundus photo of a patient with proliferative diabetic retinopathy
b) Macrohemorrhages (preretinal, subretinal, subhyaloid, hemophthalmos) - there is a sharp decrease in vision, loss of the visual field, a dark spot in front of the eye.
Fundus photo of a patient with subhyaloid hemorrhage.
c) Gliosis
d) Traction retinal detachment
Diabetic macular edema
Can develop in all conditions. Accompanied by a sharp decrease in vision, “curvature” of straight lines and distortion of objects. Detected using optical coherence tomography.
Optical coherence tomography of the retina of a patient with diabetic macular edema
Treatment of diabetic retinopathy
Treatment depends on the stage.
1. Prevention
The gold standard is panretinal laser photocoagulation of the retina. It is performed for uncomplicated retinopathy in the preproliferative stage. Significantly reduces the risk of complications and permanent vision loss.
2. Treatment of diabetic macular edema
The patient is given intravitreal injections of anti-VEGF drugs and/or corticosteroids:
- "Eilea"
- "Lucentis"
- "Ozurdex."
3. Surgical treatment
For complicated forms of proliferative retinopathy (neovascularization, hemophthalmia, retinal hemorrhages, tractional retinal detachment), surgical treatment is performed - subtotal vitrectomy, removal of proliferative tissue, endolaser coagulation.
Remember: the development and outcome of the disease depends on the stage. Since DR has no obvious symptoms and appears only after irreversible changes in the fundus, it is necessary to undergo routine examinations with an ophthalmologist.
And patients with diabetes should undergo it at least once a year!
Clinical picture
Diabetic retinopathy develops and progresses without characteristic symptoms. Decreased vision in the nonproliferative stage is not subjectively noticeable. A feeling of blurriness of visible objects can cause macular edema. There are also difficulties when reading at close range. Moreover, the sharpness of vision depends on the concentration of glucose in the blood.
In the proliferative stage of the disease, a veil and floaters appear before the eyes (the result of intraocular hemorrhages). After some time they disappear on their own. With massive bruising into the vitreous body, a sharp deterioration or complete loss of vision occurs.
Forms
In ophthalmology, there is the following classification of diabetic retinopathy:
- Non-proliferative. The vascular walls of the retina become thinner, provoking the occurrence of multiple pinpoint hemorrhages, microaneurysms and foci of lipid deposits are formed. With diabetic nonproliferative retinopathy, macular edema is also possible, which results in deterioration of central vision.
- Preproliferative. The pathogenesis of this form is as follows. Due to impaired blood circulation in the retina, tissue oxygen starvation begins, multiple hemorrhages, venous anomalies and lipid deposits occur. In diabetic preproliferative retinopathy, the affected areas of the retina fall out of sight.
- Proliferative. Due to insufficient blood supply, the body creates new pathological vessels with fragile, permeable walls, through which multiple hemorrhages occur. Abnormal vessels grow throughout the fundus of the eye, causing tissue scarring. If left untreated, new blood vessels form and scarring continues, leading to retinal detachment and loss of vision in both eyes. Proliferative diabetic retinopathy is a serious disease and most often occurs as a result of lack of proper treatment for hyperglycemia.
It is recommended to begin treatment of the pathology immediately when the first signs of vision deterioration occur. If this is not done, then eye diabetes turns into a proliferative form, provoking the occurrence of irreversible pathological changes.
Diagnostics
To screen for diabetic retinopathy, the patient is prescribed ophthalmoscopy under mydriasis, visometry, biomicroscopy of the anterior segment of the eye, perimetry, biomicroscopy of the eye with a Goldmann lens, Maklakov tonometry, diaphanoscopy of eye structures.
The ophthalmoscopic picture is of greatest importance for establishing the stage of the disease. In the non-proliferative phase, microaneurysms, hemorrhages, hard and soft exudates are detected. In the proliferative phase, the fundus picture is distinguished by intraretinal microvascular abnormalities (tortuosity and dilatation of veins, arterial shunts), endoviteral and preretinal hemorrhages, fibrous proliferation, neovascularization of the retina and optic disc. To document changes in the retina, a series of fundus photographs are taken using a fundus camera.
For opacities of the vitreous body and lens, an ultrasound of the eye is prescribed instead of ophthalmoscopy. To assess the impairment or preservation of the functions of the optic nerve and retina, electrophysiological studies are carried out: electrooculography, determination of CFSM, electroretinography. To detect neovascular glaucoma, gonioscopy is performed.
The most important method for examining retinal vessels is fluorescein angiography. It records blood flow in the choreoretinal vessels. If necessary, angiography is replaced by laser and optical coherence scanning tomography of the retina.
To identify risk factors for the progression of diabetic retinopathy, the levels of sugar in urine and blood, glycosylated hemoglobin, insulin, lipid profile and other indicators are examined. No less informative diagnostic methods include ultrasound of the renal vessels, 24-hour blood pressure monitoring, ECG and echocardiography.
Diagnosis of DR
Since people with diabetes are at risk of developing problems with the eye and cornea, they need to regularly visit an ophthalmologist.
If a patient comes to the clinic due to deteriorating vision, at the first appointment the doctor is obliged to study his medical history. Further examination of the patient and classification of the disease may include the following diagnostic methods:
- perimetry. Using this technique, the doctor obtains information about the viewing angle of the eye with the affected cornea;
- visometry. Helps determine visual acuity on a special table;
- ophthalmoscopy. Involves checking the HD with a special mirror;
- diaphanoscopy. Detects tumors in the eyeball and cornea;
- biomicroscopy. Identifies corneal lesions and GS lesions with a slit lamp.
In certain cases, ultrasound is used to examine the patient.
Important! Prevention of blindness and various complications depends on the timely detection of ocular lesions that will be signs of progression of DR.
Conservative therapy
In the initial stages of the disease, the main method of treatment is conservative. The patient is advised to take long-term medications that reduce capillary fragility - angioprotectors (Doxium, Parmidin, Dicynon, Predian). It is also necessary to maintain adequate blood glucose levels.
Sulodexide, ascorbic acid, vitamin P and E are prescribed for the treatment and prevention of vascular complications. Antioxidants (for example, Strix) provide a good effect. These preparations contain beta-carotene and blueberry extract. These beneficial substances improve vision, strengthen the vascular network, protecting against the effects of free radicals.
A special place in the treatment of diabetic retinopathy is occupied by the normalization of carbohydrate metabolism. This occurs by taking glucose-lowering medications. Conservative therapy also involves normalizing the patient’s diet.
People suffering from this disease are subject to medical examination. Based on the severity of diabetes, the period of incapacity for work is determined. The patient is contraindicated from work involving heavy visual load, vibration, tilting of the head and body, or lifting heavy objects. It is strictly forbidden to work in transport and in hot shops.
Treatment
Treatment of diabetic retinopathy is aimed at maximum correction of metabolic disorders in the body, normalization of blood pressure levels, and improvement of microcirculation.
For macular edema, intravitreal injections of corticosteroids have a good therapeutic effect.
Progressive diabetic retinopathy is the basis for performing laser coagulation of the retina, which can reduce the intensity of the neovascularization process and reduce the risk of developing retinal detachment.
Laser coagulation of the retina
For severe diabetic retinopathy complicated by retinal detachment or macular traction, vitrectomy is performed. During surgery, the vitreous body is removed, bleeding vessels are cauterized, and connective tissue cords are cut.
Surgery
If the diagnosis of diabetic retinopathy reveals serious disorders: hemorrhages in the retina, swelling of its central zone, the formation of new vessels, then laser therapy is indicated for the patient. In particularly difficult cases - abdominal surgery.
When new bleeding vessels and macular edema appear, laser coagulation of the retina is required. During this procedure, laser energy is delivered to damaged areas of the retina. It penetrates the cornea, vitreous body, anterior chamber humor and lens without incisions.
The laser is also used outside of central vision to cauterize areas of the retina that are starved of oxygen. With its help, the ischemic process in the retina is destroyed. As a result, new vessels stop appearing. This method also eliminates already formed pathological neoplasms. This leads to a reduction in swelling.
The main method of surgical treatment of diabetic retinopathy is laser therapy.
The main goal of laser coagulation is to prevent the progression of the disease. To achieve it, an average of 3-4 sessions are required. They last 30–40 minutes each and are held at intervals of several days. Pain may occur during the procedure. Therefore, local anesthesia is performed in the tissues surrounding the eye. A few months after completion of therapy, a specialist evaluates the condition of the retina. For this purpose, fluorescein angiography is prescribed.
If vitreous hemorrhage occurs with nonproliferative diabetic retinopathy, the patient requires vitrectomy. During the procedure, the doctor removes the accumulated blood and replaces the vitreous with silicone oil (or saline solution). At the same time, scars that cause retinal separation and ruptures are cut with a laser, and bleeding vessels are cauterized. This operation is recommended to be performed in the early stages of the disease. This significantly reduces the risk of complications.
If the patient has severe changes in the fundus of the eye, many newly formed vessels and fresh hemorrhages, cryocoagulation of the retina is performed. It is also necessary if vitrectomy or laser coagulation is impossible.
What are the complications?
Without proper treatment of diabetes mellitus and diabetic retinopathy, serious complications arise, leading to blindness.
- Traction retinal detachment. It occurs due to scars in the vitreous humor that are attached to the retina and stretch it when the eye moves. As a result, tears form and vision loss occurs.
- Rubeosis of the iris is the growth of blood vessels into the iris. Often these vessels rupture, causing hemorrhages in the anterior chamber of the eye.
By the way, we recommend reading the article Which sugar substitute is best for diabetes? Review of sweeteners
Rubeose
- Glaucoma – increased intraocular pressure. Glaucoma occurs due to the fact that sprouted newly formed vessels interfere with the normal outflow of intraocular fluid. This type of glaucoma is difficult to treat.
- Blindness.
Prevention
The main way to prevent diabetic retinopathy is to maintain normal blood sugar levels. Optimal correction of lipid metabolism, compensation of carbohydrate metabolism, and blood pressure control are also important. Taking antihypertensive and hypoglycemic drugs will help with this.
Regular physical activity has a positive effect on the overall well-being of diabetics. Another way to a fulfilling life is proper nutrition. Limit the amount of carbohydrates in your diet. Focus on foods rich in natural fats and proteins.
For timely diagnosis, regularly consult an ophthalmologist. Do this when relevant complaints appear and at least once a year. Young people with diabetes are recommended to undergo examination at least once every 6 months.
What it is?
Diabetic retinopathy is an ophthalmological disease. This is a disease of the retina, namely its blood vessels. In people with diabetes, it is often triggered by abnormally high blood glucose levels.
Reference! Our retina is a layer of light-sensitive tissue located at the back of the apple. Entering it, the rays of light are collected, after which this information is transmitted to the brain, where it interprets the image.
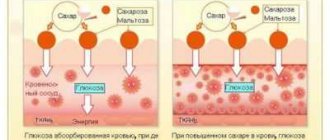
Increased glycemia changes the structure of the walls of blood vessels. The consequence of this effect is that they become more permeable. Ultimately, the disorders lead to significant loss of visual acuity, which cannot be restored.
Possible complications
Incorrect or untimely treatment of background retinopathy can lead to serious complications, among which doctors identify retinal vein thrombosis and the development of partial or complete hemphothalmos of the eye . In rare cases, the patient experiences complete blindness, much more often - decreased visual acuity. Depending on the type of pathology, complications may vary. For example, diabetic retinopathy may cause retinal detachment, hemophthalmos, cataracts, or blurred vision.
The disease is fraught with serious complications
Background retinopathy poses a serious danger to women during pregnancy, since the underlying disease can become aggravated during pregnancy, which often leads to artificial termination of pregnancy. To avoid such complications, it is necessary to promptly treat all eye diseases, including retinopathy.
Classification of complications
Stages of hypertensive retinopathy
There are 4 stages of development of this hypertension:
- The first stage is called angiopathy, which is damage to the blood vessels. In this case, disorders are diagnosed only in small capillaries of the inner shell. All these changes are functional and minor. They are reversible if treatment is started in a timely manner.
- The second stage of hypertensive retinopathy is angiosclerosis, in which organic degeneration of the vascular walls occurs. Their elasticity and capacity decreases, as there is more connective tissue than functional tissue. In addition, cholesterol deposits are observed in the retinal vessels.
- Actually, hypertensive retinopathy, which is accompanied by pronounced changes in blood vessels. Pathological foci form in the inner shell. They surround capillaries and arterioles that have been damaged. The center of the retina becomes cloudy. Under an ophthalmoscope, hemorrhages, as well as star-shaped degenerative-dystrophic processes, are clearly visible.
- Neuroretinopathy, or stage 4 hypertensive retinopathy. It is the most severe and dangerous, due to the fact that the pathology spreads to the optic nerve. This leads to the death of its fibers. There is swelling and clouding of the disc. At this stage, vision rapidly declines. Various visual functions deteriorate. This stage of hypertensive retinopathy can result in complete blindness.
It is not a fact that hypertensive retinopathy will go through all these stages. If hypertension is treated and ophthalmological signs of retinal damage are detected in time, it is possible to stop the pathology at the initial stage. But in the early stages, the patient may not notice any symptoms. To detect them, you need to periodically visit an ophthalmologist. If you have arterial hypertension, it is recommended to do this once every 6-8 months.
Who is at high risk?
The disease develops in diabetics with an overwhelmingly high probability. Statistical analyzes have proven that in people over 30 years of age with a duration of diabetes of 10-15 years, retinal retinopathy manifests itself in an astounding 89% of cases. In 30%, the disease is diagnosed at a late stage. Diabetic retinopathy causes absolute vision loss in approximately 2% of people with diabetes and causes severe visual impairment in 10% of patients. Some factors only increase the likelihood of progression and development of the disease. These include:
- duration of diabetes: the longer, the higher the risks;
- poor glycemic control;
- predisposition to diabetic retinopathy;
- bearing a child.
The duration of diabetes is a major risk factor. On the other hand, a statistical analysis of people under 18 years of age with type I diabetes showed that even a short duration of the disease does not exclude the occurrence of ophthalmological problems. When diabetes lasted up to 5 years, retinopathy was recorded in 6% of children. When the sample included children with a duration of diabetes of 5-10 years, the percentage increased to almost 20%. Almost half of them had an advanced stage of eye disease.
The mechanism of pathology development
With retinopathy, blood circulation to the tissues of the eyeball is disrupted. They do not receive enough oxygen and nutrients, so the pathological process, unfortunately, over time inevitably negatively affects a person’s vision. As a rule, this disease affects both eyes, but sometimes it may be less pronounced in one of them.
Elevated glucose levels lead to the fact that this carbohydrate does not enter the cells in the required quantity. Because of this, blood circulation in the retina slows down, and the body, in an attempt to improve it, begins to form new blood vessels. They grow from existing capillaries, but this process does not lead to anything good. The new vessels are defective, they are brittle and weak, so hemorrhages can often be found in the patient’s eyes. Swelling and blood in the retina or vitreous lead to significant impairment of vision.
The risk of going blind for a diabetic is 25 times higher than for a healthy person. And it is diabetic retinopathy that often leads to such consequences. To maintain the ability to see normally, it is important not only to detect the disease in time, but also to begin proper treatment, because without supportive therapy, in almost 80% of patients, retinopathy progresses and leads to complete or partial loss of vision.
Forms of primary retinopathy
Central serous
The etiology of primary retinopathy is not well understood, so it is called idiopathic (for an unknown reason). The central serous form of retinopathy is called central serous retinitis or idiopathic macular detachment. The disease develops in men 20-40 years old who do not have somatic abnormalities. Patients complain of migraine-like headaches associated with emotional stress. During the examination, the doctor reveals a unilateral retinal lesion.
Symptoms of central serous retinopathy:
- micropsia (visible objects decrease in size);
- scotomas;
- decreased visual acuity;
- narrowing of visual fields.
Ophthalmoscopy makes it possible to identify a limited round or oval dark protrusion on the retina. This is a serous detachment of the epithelium in the macular area. With this form of retinopathy there is no foveal reflex, there are yellowish or grayish precipitates.
Therapy for central serous retinopathy is based on laser coagulation of the retina. It is necessary to use drugs to strengthen the vascular wall, improve microcirculation and reduce swelling. Patients are prescribed oxygen barotherapy (oxygen treatment). With timely treatment, it is possible to stop the detachment and restore vision.
Acute posterior multifocal pigment epitheliopathy
This form of retinopathy is characterized by multiple flat subretinal lesions of a grayish-white color. With their reverse development, depigmentation occurs. During the examination, the doctor sees perivascular edema of peripheral vessels, dilated veins, and swelling of the optic nerve head.
A large number of patients have cloudy vitreous fluid, the disease is complicated by iridocyclitis and episcleritis. Impaired central vision, scotomas (central, paracentral) occur.
Treatment of acute posterior multifocal retinopathy is carried out conservatively:
- vitamins;
- vasodilators (pentoxifylline, vinpocetine);
- angioprotectors;
- retrobulbar injections (corticosteroids);
- hyperbaric oxygenation.
External exudative
This form is more often diagnosed in young men. It is called Coats disease or external exudative retinitis. Characterized by unilateral lesions, the presence of exudate, hemorrhages and cholesterol crystals under the retinal vessels. Angiography often reveals microaneurysms and arteriovenous shunts. As a rule, deformations affect the periphery of the fundus, less often the macular zone.
External exudative retinopathy is characterized by a slow but progressive course. Treatment will consist of laser coagulation of the retina and hyperbaric oxygen therapy. The result is ambiguous, since the disease can be complicated by retinal detachment, glaucoma, and iridocyclitis.
Diagnostic features
In this case, the diagnosis is carried out by an ophthalmologist, although examinations can also be carried out by other doctors. As a rule, the patient is prescribed the following diagnostic procedures:
- tonometry (measurement of intraocular or blood pressure using a special device - a tonometer);
- angiography (x-ray examination of the patient’s blood vessels using contrast);
- laser scanning;
- ultrasound examination (ultrasound);
- perimetry or visual field testing;
- ophthalmoscopy (examination of the patient's fundus using a fundus lens or ophthalmoscope).
Direct ophthalmoscopy
On a note! In addition to the above diagnostic methods, another procedure may be prescribed - electroretinography. This is a special diagnostic method in which the doctor, using special equipment (electroretinograph), measures the electrical potential of the patient’s retina.
Causes
Doctors consider the following to be the most common pathologies that can cause background retinopathy:
- leukemia, anemia;
- pathological abnormalities in the development of blood vessels (as a rule, this applies to infants);
- development of diabetes mellitus;
- atherosclerosis;
- damage to the patient's eyeball or traumatic brain injury;
- regular increase in blood pressure or development of hypertension.
Postthrombotic state
Background retinopathy can also occur as a result of blockage of the central retinal vein by a thrombus (blood clot). To identify the disease in a timely manner, you need to know its clinical picture. This will identify retinopathy at an early stage of development.
Diagnosis of the disease
Retinopathy of prematurity
There is a pathology that develops not in adults (as in the above cases), but in premature infants, which has received the appropriate name. The disease is caused by underdevelopment of the retina in prematurely born children.
In order for the organ to complete its formation, such infants need to ensure visual rest and local tissue respiration (glycolysis) without the participation of oxygen. At the same time, in order to stimulate metabolism and the final stage of development of other organs, premature babies need additional oxygenation, which inhibits the processes of glycolysis in the retina.
Most often, retinopathy of prematurity is observed in children born earlier than 31 weeks and weighing less than 1.5 kg. Pathology can also develop in infants who have undergone blood transfusion or oxygen therapy against the background of premature birth.
In this regard, all children at risk are examined by an ophthalmologist a month after birth and every 2 weeks until all eye structures are fully formed. This is necessary to prevent late complications of eye pathology - amblyopia, strabismus, primary glaucoma, retinal detachment, etc.
In most cases, the symptoms of retinopathy of prematurity disappear spontaneously, so often only expectant management is required. Sometimes specialists resort to laser coagulation, cryoretinopexy, and in rare cases, surgery to remove the vitreous body or scleroplasty.
Types of disease
Doctors divide retinopathy into two types: nonproliferative and proliferative. The first is more common: it accounts for about 80% of cases. It is also considered softer - damage to the structure does not extend beyond the layers of the retina.
Read more about the different types of retinopathy below:
| Name | Characteristic | Effect on vision |
| Non-proliferative (or simple) | When it occurs, damage to microvessels occurs: some of them become clogged, and other anomalies appear. The disease is often accompanied by posterior capsular cataracts | Some patients live with this type of retinopathy for a long time without progression of the eye disease. But with jumping glucose, the number of capillary blocks only increases, which is the cause of impairment of the weak visual apparatus |
| Proliferative retinopathy | It is characterized by a significant lack of oxygen, which provokes the formation of new blood vessels on the surface of the retina. They subsequently bleed | Vision is seriously impaired. Due to prolonged lack of oxygen, abnormal formations can form not only on the surface of the retina, but also in the iris of the eye. This is a common cause of secondary glaucoma. |
Note! Over time, nonproliferative retinopathy can transform into proliferative retinopathy at later stages. Thus, it flows from early to developed.
For the first 4-5 years, simple (non-proliferative) retinopathy occurs without any noticeable symptoms. The patient may experience mild discomfort due to occasional sudden fogging.
What does an ophthalmologist diagnose?
The specialist conducts a full examination of the visual system using computerized equipment. When diagnosing, the following are examined:
| Diagnostic object | Diagnostic method |
| IOP (intraocular pressure) | Determined by eye tonometer |
| Internal structure of the retina | Ultrasound examination using A- and B-scan |
| Condition of nerve cells and optic nerve | Analyzed using electrophysiological method |
| Ocular fundus | The ophthalmoscopy method is used |
| line of sight | Donbers test. Carried out for a comprehensive assessment of the condition of the retina at its periphery |
It is recommended that all patients with diabetes mellitus undergo a complete vision examination at least once every six months, regardless of type. Regular visits to the ophthalmology office will help to detect the development of the disease in the early stages and begin effective treatment along with preventive measures.
Hypertensive retinopathy: treatment
- Treatment of this pathology is determined by its stage, the age of the patient, the presence of concomitant diseases, contraindications and other factors. Conservative and surgical methods are used. In the first stages, the disease can be stopped with the help of medications:
- vasodilators;
- retinoprotectors;
- angioprotectors;
- hypolipidemic;
- vitamin complexes;
- anticoagulants.
The main therapy is aimed at lowering blood pressure. In addition, it is important to prevent its sudden increase. If the pathology leads to serious damage to the retinal vessels, surgery will be required. Laser coagulation may be prescribed. This procedure is also used for retinal detachment. The surgeon uses a laser beam to target pathological lesions, preventing their further spread. When the retina is detached, it is soldered to the choroid. Laser coagulation is a safe procedure, but it is not performed for cataracts, corneal opacity, a large number of hemorrhages and a high risk of retinal detachment.
Cryodestruction can also be performed. During this treatment, the doctor directs cold radiation to the affected areas of the eyeball, which makes it possible to restore the structure of the blood vessels and return the exfoliated inner membrane to its place. Due to the opening of wide opportunities associated with the development of laser technologies, cryodestruction is carried out much less frequently.
If all these methods are ineffective, vitrectomy is performed - removal of the vitreous body. During this operation, blood clots, bands and other pathological formations can be removed from the eye.
Traumatic retinopathy
Traumatic retinopathy is caused by sudden compression of the chest, as a result of which, due to spasm of the arterioles, a state of retinal hypoxia is observed and the release of edematous transudate into it.
Immediately after the injury, signs of hemorrhages and organic damage to the retina appear. Atrophy of the optic nerve is often a complication. In general, the consequences of traumatic retinopathy (the so-called “Berlin retinal opacities”) are reduced to subchoroidal hemorrhages, swelling of the lower layers of the retina and leakage of fluid into the space between the choroid and the retina.
Treatment consists of emergency vitamin therapy, elimination of hypoxia, and hyperbaric oxygenation.
Diagnosis of retinopathy
Examination for primary retinopathy is carried out using an ophthalmoscope. The procedure makes it possible to identify changes that the disease provokes: detachment, swelling, the presence of precipitates and hemorrhages, dilated veins, optic disc defects, turbid fluid under the vessels.
Diagnosis of secondary retinopathy requires consultation with a neurosurgeon, neurologist and endocrinologist.
Examination methods:
- For hypertensive retinopathy. Consultation with a cardiologist. Ophthalmoscopy, fluorescein angiography of the retina.
- With atherosclerotic. Direct or indirect ophthalmoscopy, angiography.
- For diabetic. Ophthalmoscopy, ultrasound of the eyeball, determination of visual fields, electroretinography, laser scanning.
- Retinopathy of prematurity. Regular visits to the ophthalmologist (a month after birth, then every two weeks).
Retinopathy in ophthalmology
Ophthalmology gives the following definition of retinopathy - a set of pathological deformations of the retina of different origins. Moreover, this disease is not accompanied by inflammatory processes and damage to the retina caused by other eye diseases. Ocular retinopathy consists of two groups: the primary group of diseases and the secondary group of diseases.
The primary group of retinopathy diseases has three subtypes of disease origin: central serous, acute posterior multifocal, external exudative.
The secondary group of diseases or also called “background retinopathy and retinal vascular changes” of retinopathy diseases has four subtypes of disease origin: diabetic, hypertensive, traumatic, postthrombotic retinopathy and blood diseases.