Vulvar cancer is considered a relatively rare type of cancer that develops in a woman’s genital organs. Most often, the lesion is localized on the labia majora. The most obvious and constant signs of disease progression are the presence of severe itching and bleeding.
Vulvar cancer, photos of which will be presented below, is diagnosed in 0.6% of all clinical cases of detection of malignant tumors of the reproductive system in females. It is better to identify the pathological process as early as possible, since this way the patient will be more likely to have a positive outcome from therapy.
What is vulvar cancer?
The first symptoms of vulvar cancer
Vulvar cancer is an oncological disease on the genitals: outside the labia or clitoris, vestibule of the vagina or posterior commissure, urethra - in soft, skin or mucous tissues. These may be lumpy growths, a flat ulcer with ridge-like edges, or nodes in the vulva.
It is easy to diagnose the disease visually and manually, since all genital organs are accessible for examination. However, vulvar oncology has not yet been fully studied, so vulvar and vaginal cancer in women is one of the most difficult to treat neoplasms.
The occurrence of the disease is influenced by the characteristics of the blood supply to its organs, innervation and lymphatic drainage. The topographic proximity of adjacent organs and the high physiological and psychosexual vital significance of the female external genitalia are also important. The disease is rare, occurring in 2-5% of women with cancer. But at the same time, cancer of the labia and other components is induced by hormonal changes, which occurs during the postmenopausal and menopausal periods in 50% of older women 60-80 years old.
Varieties
Many diseases of this type affect the female genital organs, located externally, but the labia majora are often affected. To the characteristic symptoms described, one can also add a gradual change in the color of the skin and the presence of a painful syndrome. If treatment of the pathology is not started in a timely manner, metastases may appear in other parts of the body.
To understand what a vulvar tumor is, you need to know what is included in its composition: the labia majora and minora, the pubic eminence and the clitoris, the entrance to the vagina, its bulb and opening, the large and small glands. Almost always, the pathological focus is located on the labia majora, and if the disease begins to develop on the external genital organs, they speak of the primary type.
Vulvar cancer location area. Source: assuta-clinics.com
Squamous cell carcinoma of the vulva is also called carcinoma. Its main area of localization is the outer skin. If we consider the medical characteristics, then this type of oncology is considered squamous cell carcinoma. In 90% of cases, patients are diagnosed with this type of vulvar cancer. A characteristic feature of the pathology is that it can develop without symptoms over several years.
A tumor in the vulva, called melanoma, accounts for only 5% of all clinical cases diagnosed with this malignant disease. Pathology can often be identified by the formation of a characteristic dark spot on the skin. The degree of spread of metastases to other parts of the body is very high. This type of pathology is often diagnosed in young women.
With the development of adenocarcinoma, glandular tissues are damaged. The likelihood of detecting this type of vulvar cancer is quite low. In the case of sarcoma, the tumor is localized in the connective tissues. The danger of progression of this type of pathology is that it is very aggressive and often ends in death.
Also, some patients are diagnosed with clitoral cancer. The frequency of diagnosis is 2.2-8% of all clinical cases. As cancer progresses in this area, the woman suffers from severe, severe pain. There is also such a variety as warty carcinoma, in which a slow growth of warts is observed on the genital organ.
As for the prognosis for recovery, in most cases it is favorable if the pathology is diagnosed at an early stage. However, the correctness of the treatment, as well as the presence or absence of metastases, will play a decisive role.
Precancerous diseases of vulvar cancer
The remaining statistical 50% of cancer cases occur in young women due to the herpes virus and papilloma. Kraurosis of the vulva affects the development of oncological tumors - these are precancerous diseases of the external genital organs. They give rise to dystrophic, atrophic and sclerotic changes in their skin, and subsequently – atrophy of the vulva. Leukoplakia often develops along with cancer.
According to the WHO classification (2003), precancerous diseases with changes in flat epithelial cells include:
Vulvar dysplasia (and carcinoma in situ):
- light (VIN*);
- moderate (VIN2);
- severe (VIN3) and carcinoma in situ.
Note: VIN refers to vulgar intraepithelial neoplasia of the vulva.
Causes
A vulvar tumor begins to progress when it is no longer possible to control the proliferation of cancer cells. If at a certain stage this process is not stopped, it will inevitably lead to the appearance of metastases in various parts of the body. The development of pathology occurs under the influence of two main reasons.
Pathological cells begin to move throughout the body through blood circulation and lymph flow. If possible, they kill healthy tissue as completely as possible, which in medicine is called an invasive process.
When pathological cells divide and grow under the influence of a process such as angiogenesis, such tissues will independently create vessels through which blood and nutrients will be supplied to them.
If the necessary treatment is absent, the pathological cells will begin to constantly increase their numbers, which will lead to the appearance of metastases throughout the body. Vulvar cancer, although diagnosed relatively rarely, still requires professional treatment.
There are also provoking factors, under the influence of which a tumor of the vulva and clitoral cancer can develop (photos will be presented).
Patient's age. Doctors often detect pathology in women who are 70 years of age or older. This condition is diagnosed in 50% of all clinical cases. One in five patients is diagnosed with a tumor before the age of 50.
Patients over 70 years of age are more susceptible to vulvar cancer. Source: likarni.com
Presence of HPV. Women who are carriers of the human papillomavirus are at risk for developing vulvar cancer.
Vulvar intraepithelial neoplasia. The presented term is a general term for precancerous conditions, under the influence of which the patient notes the presence of epithelial cells affected by the initial stage of carcinoma. Women with this diagnosis are also at risk for a high likelihood of developing pathology.
Lichen sclerosus. As this disease progresses, thickening of the skin is noted, and severe itching is also present. All this leads to increased susceptibility of the epidermis of the genital organs and vulva to cancer.
Melanoma. This type of disease also significantly increases the risk of developing vulvar cancer. It can occur under the influence of genetic predisposition, or in the presence of favorable factors in the woman herself.
Sexually transmitted diseases. If a patient has an increased level of antibodies to the genital herpes virus, the likelihood of developing vulvar cancer increases many times.
Bad habits. As studies conducted by scientists have shown, if a woman has an alcohol or nicotine addiction, the risk of developing cancer increases 6 times.
Bad habits increase the risk of developing cancer. Source: 1popecheni.ru
Organ transplantation. If a woman has undergone such an intervention at some point in her life, the likelihood of developing vulvar cancer also increases. This is due to the fact that during the recovery period she has to take a large number of immunosuppressants so that her own body does not tear off the foreign organ.
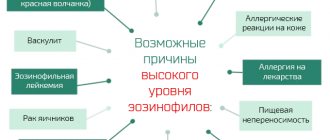
In addition to these risk factors, genital cancer can develop in women who have the human immunodeficiency virus. Also, the likelihood of developing pathology increases in the presence of lupus erythematosus, psoriasis, and also after radiation therapy for uterine cancer.
Classification of the disease
Squamous cell carcinoma of the vulva occurs in 70-90% of patients, since the epithelium contains squamous cells. It is divided into smaller and larger groups. A smaller group includes tumors that are induced by HPV. They are called aaloid-free and verrucous. The second large group includes an oncological process from a flat cell with an unknown etiology.
Cancer affects the vulva and its organs in different ways. The labia majora - 52%, minor - 7.1%, the clitoris is affected in 12-20%, the posterior commissure - in 6.4%, the periurethral zone - in 1.7%, the Bartholin gland - in 0. 2%.
Anatomy of the vulva
ICD code is C51, anatomical areas are designated as follows:
- labia majora – C51.0 and labia minora – C51.1;
- clitoris – C51.2;
- cancer of other localization – C51.8;
- unspecified areas of the vulva with oncological process – C51.9.
In accordance with the histological classification (WHO, 2003), they are also divided into: squamous cell keratinizing carcinoma of the vulva, non-keratinizing and basaloid, verrucous or verrucous and papillary, condylomatous and other forms.
Glandular malignant neoplasms include:
- extramamillary or Paget's cancer of the vulva;
- Bartholin gland: squamous cell, adenoid cystic, glandular squamous or transitional cell, adenocarcinoma;
- adenocarcinoma in situ;
- mammary-like anogenital glands (adenocarcinoma);
- squamous (or flat component);
- adenoid cystic;
- transitional cell;
- small cell;
- basal cell;
- from ectopic tissue cells of the mammary gland;
- from sweat gland cells.
Vulvar tumors in women are often located in soft tissue. These include according to WHO 2003:
- rhabdomyosarcoma;
- aggressive course of angiomyxoma;
- leiomyosarcoma;
- dermatofibrosarcoma protuberans;
- oncofibrous histiocytoma;
- epithelioid sarcoma;
- onkoshvanny;
- malignant hemangioendothelioma;
- Kaposi's sarcoma;
- hemangiopericytoma;
- liposarcoma;
- alveolar soft tissue sarcoma.
The new WHO histological classification (Lyon, 2003) of soft tissue tumors includes sarcomas such as:
- botryoid;
- leiomyosarcoma;
- epithelioid;
- alveolar soft tissue;
- liposarcoma;
- Dermatofibrosarcoma protuberans.
Other malignant processes include tumors in the form of:
- melanoma;
- hemoblastosis;
- lumps in the yolk sac, formations from Merkel cells;
- metastatic secondary fistulas.
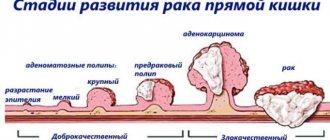
Stages of the malignant process
Clinical stages of vulvar cancer without surgical intervention data determine the degree of malignancy of the primary process.
- Stage 1 is a tumor that does not extend beyond the vulva, located on the skin tissue of the perineum: behind the vagina and up to the anus. Cone diameter - ≤2 cm;
- Stage 2 is determined by a lump with the same location, its diameter is >2 cm;
- Stage 3 indicates a node of any size. The spread occurs through the following channels: urethra and anus, covers the lower 2/3 of the vagina, metastasizes to the lymph nodes;
- Stage 4 is characterized by neoplasms of different diameters that spread through the urethra, vagina, bladder, rectum, and adhere to the pelvic bone tissue. There is metastasis to distant organs.
Data from surgical interventions (histological confirmation) are used for primary cancer in the FIGO and TNM classification (2009).
Classified as vulvar cancer (C 51)
Decoding the data of the primary tumor T:
- TX – cannot be assessed;
- T0 – cannot be determined;
- Tis – determine pre-invasive cancer (cancer in situ), grade III intraepithelial neoplasia (VINIII);
- T1 – the lump does not extend beyond the vulva and/or perineum and vulva;
- T1a – lump ≤2 cm in diameter, there is stromal invasion up to 1 mm1;
- T1b – lump larger than 2 cm or has stromal invasion > 1 mm1;
- T2 – the formation has a different diameter and is distributed to the perineal organs: vagina, urethra and anus;
- T32 – has a different size and covers: the urethra and 2/3 of the vagina, the walls of the bladder, the rectum, and is fixed to the bone tissue of the pubis.
Notes:
- 1 - deep invasion is determined by the distance from the epithelial-stromal junction of the dermal outgrowth on the surface to the deepest invasive point;
- 2 - FIGO does not use the T3 indicator, but only T4.
Interpretation of indicators of regional lymph nodes N - on the thigh and groin:
- NX – RLU – no assessment is possible;
- metastases:
- N0 – cannot be determined in the RLU;
- N1a – found in 1–2 lymph nodes (<5 mm);
- N1b – there are ≥ 5 mm in a single LN;
- N2a – in many lymph nodes <5 mm;
- N2b – in many lymph nodes > 5 mm;
- N2c – identified in the lymph nodes, there is capsule germination;
- N3 – there is a metastasis fixed or with ulcerations in the RLU.
Indicators of distant metastases M:
- M0 – no metastases in distant lymph nodes;
- M1 – metastases in distant lymph nodes and pelvis were identified.
Interpretation of indicators of the degree of histological differentiation G. The degree was established:
- GХ – cannot be installed;
- G1 – high;
- G2 – average;
- G3 – low or undifferentiated cancer;
- G4 – poorly differentiated vulvar cancer with a predominance of flat cells and keratinization. It is rare and has a poor prognosis.
In squamous cell carcinoma of the vulva, metastases are found in regional lymph nodes: in the groin (on both sides), on the thigh. Less commonly, in the pelvic area from a clitoral tumor. Hematogenous dissemination of cancer almost never occurs. Lymphogenous pathways of metastasis of vulvar cancer are characteristic. Due to the close connection of lymph vessels, bilateral and cross metastases occur.
Metastases from formations in the endometrium, urethra and bladder more often penetrate into the vulva and develop secondary cancer. Occasionally, tumors of the vagina, ovaries, mammary glands, kidneys, bronchi, cutaneous melanoma, lymphoma and choriocarcinoma metastasize to the vulva.
Regional lymph nodes are affected when the size of the nodes is:
- T1 – with a frequency of 8.9%;
- T2 – with a frequency of 25.3-35%;
- T3 – with a frequency of 31.1 – 55%.
What factors may affect the risk of developing vulvar cancer?
- early sexual intercourse with different sexual partners, numerous abortions;
- smoking;
- STI;
- low social status;
- occupational hazards: laundries, dry cleaners, production of nickel, chromium, formaldehyde, etc.;
- immunodeficiency;
- obesity and diabetes;
- family predisposition;
- the presence of other malignant tumors of the genitals;
- chronic vulvitis;
- leukoplakia;
- condylomas and warty growths on the vulva;
- high fertility.
Causes
The causes of vulvar cancer in women most often include precancerous diseases, the presence of HPV DNA, and the presence of genital warts due to papillomavirus infection. It can cause papillomas or epithelial dysplasia in places such as the vulva, vestibule, anus, cervix, tongue, lips, palms and soles, and penis in men.
Attention! Women are at risk of developing cancer if they have HIV or VIN (vulgar intraepithelial neoplasia). The risk of the disease also includes frequent changes of sex partners, alcohol and smoking.
Symptoms
The first sign of the development of oncology is the presence of lesions on the genital organ. Against this background, there is severe itching, irritation, and sometimes bleeding occurs. Unfortunately, women do not always go to see a gynecologist if they have these conditions. Due to this, diseases are detected already at an advanced stage, when therapy involves a more serious effect on the body.
With the development of oncology, itching appears in the intimate area. Source: netzudu.ru
Symptoms of vulvar cancer include the following:
- The presence of a painful syndrome during intimate intimacy;
- Bleeding from the genitals;
- Presence of itching and burning;
- With melanoma, dark spots appear on the skin;
- There is pain during urination;
- The level of sensitivity of the vulva increases;
- New growths similar to warts may appear;
- The skin becomes thickened, and sometimes there are ulcers.
It is worth understanding that the above symptoms may be in full or partial, since depending on the type of oncology and its location, the signs of the disease will differ. Therefore, if a woman notices atypical changes in the gynecological part, it is imperative to consult a doctor.
Symptoms and manifestations of vulvar tumors
Early general signs of vulvar cancer are similar to those of vulgar intraepithelial neoplasia (VIN). As the problem area progresses, an inflammatory process appears:
- the mucous membrane becomes irritated and itchy, becoming rough;
- a red or white warty bump or abrasion appears;
- a long-term, non-healing painful ulcer forms;
- pain in the vulva becomes long-lasting and recurrent;
- urination causes pain in the urethra;
- discharge of blood with pus appears;
- the inguinal lymph nodes are enlarged.
Symptoms and manifestations of rare vulvar cancer
Melanoma is suspected if the following symptoms are present:
- rapid growth and increase in nevus density;
- pigment changes;
- ulcerations with slight bleeding and crusting;
- redness around the growth and new nodes with cracks;
- increasing the volume of lymph nodes.
Vulvar melanoma metastasizes to distant organs: bones, adrenal glands, liver, lungs and brain. Melanoma cells reach the papillary dermis (1 mm) through the basement membrane, and metastases occur in 5% of cases. If the tumor grows into the papillary layer with an invasion of 1.1-2 mm and spreads through the subcutaneous fatty tissue, then survival rates drop, and relapses occur in 78% of cases.
Paget's disease. The anogenital area is endowed with apocrine glands, so Paget's disease occurs in 2% of women during menopause. The tumor has an invasive component and often develops as a result of the screening of cancer cells from a primary tumor located nearby into the mucosa.
Symptoms:
- red, weeping eczematous lesion in the form of dermatosis;
- hyperkeratosis in the form of small lesions on the labia majora, skin of the abdomen and thighs;
- the presence of multicentric foci in the skin.
At the same time, Paget's disease can occur in the mammary glands and vulva. If pagetoid changes in the epidermis are found in the perianal zone, then cancer may develop in the rectum.
Sarcomas of the vulva
Botryoid sarcoma or embryonal rhabdomyosarcoma can be detected in girls under 10 years of age, and at any age - leiomyosarcoma in smooth muscles. Clinically, the symptoms of vulvar cancer in women are unpredictable. Subcutaneous painful nodules of high differentiation with the presence of necrosis are more often found. There is infiltration into surrounding tissues with a mitotic index > 10 mitoses in 10 fields of view. Metastases spread to the retroperitoneal space and peritoneal lymph nodes.
Symptoms of epithelioid sarcoma or malignant rhabdoid cancer are similar to soft tissue sarcoma of the extremities and large Bartholin gland cyst of the vaginal vestibule. Symptoms appear:
- discomfort during sexual intercourse, movement and wearing tight-fitting underwear, skirts and trousers;
- complications with the appearance of painful purulent abscesses;
- high temperature, intoxication: nausea, weakness, vomiting;
- a sharp deterioration in health.
When the tumor size is up to 10 cm, sharp painful pulsation and distension in the perineal area are possible. If the tumor opens on its own, then pus flows out and the sexual flora becomes infected. This can be seen in the signs of vulvitis, vaginitis and pathological vaginal discharge. Epithelioid sarcoma repeatedly recurs and metastasizes.
Dermatofibrosarcoma protuberans occurs at different ages; its symptoms are similar to low-grade cutaneous sarcoma. Fibrous cancer is most often located on the labia majora. It is located in the capsule, there is no invasion of the mucous membrane. After treatment it often recurs. Metastases spread to the lungs.
Metastatic tumors in the perineum occur in 8% of women. The cells are delivered by lymph from the primary cancer site: the cervix or endometrium of the uterus, ovary, breast, kidney, stomach or tongue. As a continuation of the tumor from the bladder, urethra or vagina, vulvar cancer is formed, the symptoms of which sharply reduce the quality of life of patients.
They suffer from the following clinical symptoms:
- inflammation and bleeding, especially after sexual intercourse;
- pain radiating to the lumbar region, sacrum, perineum;
- swelling of the extremities after metastasis to the lymph nodes, germination into neighboring organs;
- hyperthermia, general weakness and fatigue;
- disorders of the functional functioning of the gastrointestinal tract and urination.
Vulvar cancer symptoms and signs with photos
In the early stages of vulvar cancer, the patient may have no obvious complaints. Sometimes its harbingers are leukoplakia, kraurosis, and lichen sclerosus. Often the onset of the disease is asymptomatic.
The most initial signs of vulvar cancer are a feeling of itching, discomfort or burning in the genital tract. Pain syndrome usually appears later. It is difficult to detect the first external changes without examination, but sometimes you can notice that a lump (enlarged lymph node) has appeared in the groin area, which does not hurt.
The primary visible manifestations are spots on the mucous membrane, the detection of which is not difficult: it is enough to carefully examine the vulva, but this is often done too late. The spots have a whitish-grayish tint; similar symptoms occur with leukoplakia.
Characteristic symptoms of exophytic growth are inflammation, ulceration, purulent, bloody discharge, which indicate that the disintegration of the cancerous tumor has begun. Endophytic germination is characterized by swelling, compaction, and infiltration.
Late manifestations include weakness, fatigue, and low fever. In the terminal stage, symptoms progress rapidly, which is expressed by severe exhaustion, weight loss, weak pulse, shortness of breath with light exertion. As a result, death occurs.
Diagnosis of the disease
Diagnosis of cancer of the female genital organs is carried out:
- gynecological examination;
- palpating the RLU;
- vulvoscopy, vaginoscopy and colposcopy;
- cytological examination;
- incisional wedge biopsy to the lowest point of tumor formation and part of the tissue with healthy cells;
- histological examination of tumor biopsy;
- Ultrasound of lymph nodes in the groin, hips and ilium;
- Ultrasound of the peritoneal and pelvic organs;
- chest x-ray examination;
- ECG.
A total biopsy is used due to the rapid generalization of the tumor. Anamnesis and impression smears from the surface of the tumor are assessed. Vulvar cancer is confirmed by diagnosis using immunohistochemical studies (proteins: actin, desmin and myoglobin are determined) and electron microscopy to identify microfilaments.
Important! To correctly determine the prognosis and prescribe treatment, the expression of proteins p53, Ki-67, S-100, RE, RP and other tumor markers is studied at the molecular biological level.
In accordance with the indications, the following is carried out:
- fine-needle puncture biopsy of the lymph nodes of the groin and thigh and monitor the procedure with ultrasound (if metastasis to the lymph nodes is suspected);
- cystoscopy when the oncological process moves into the wall of the bladder (according to ultrasound indications);
- biopsy of the rectal mucosa and/or bladder;
- rectomanoscopy (if there are complaints and spread of cancer in the vulva);
- coagulogram before surgery;
- PET – positron emission tomography in late stages;
- CT, MRI to clarify the spread of the oncological process.
In the laboratory, urine (general analysis) and blood are examined:
- to determine the group and Rh factor;
- to determine the HBS-Ag antigen;
- for syphilis, determination of antibodies to hepatitis C virus, HIV antibodies and for HPV DNA testing;
- to determine general indicators;
- for total protein, urea, bilirubin, glucose by biological methods.
Additionally, the function of external respiration, kidneys with radioisotopes, excretory urography (according to indications), and radioisotope lymphography are examined.
Diagnostics
Initially, a woman needs to go for examination to a doctor. During a gynecological examination, if there is a suspicion that vulvar cancer is developing, the specialist will know exactly what this disease looks like, so a preliminary diagnosis will be made, after which it will require clarification. If tumor formations or lesions are detected, the physician will perform a biopsy.
It is very important that the examination is comprehensive, including examination of the area around the clitoris and urethra, as well as the perineum. Palpation of the Bartholin glands is mandatory. If these procedures cause severe pain to a woman, then the doctor may use local anesthesia.
Depending on the biopsy results obtained, the following diagnostic measures will be carried out:
- Cystoscopic examination of the bladder, which allows us to identify the presence or absence of metastases in it;
- Rectoscopy is prescribed to exclude the possibility of damage to the rectum by cancer;
- A visual examination allows you to assess the condition of the skin of the entire body and confirm the presence or absence of pathological areas.
In addition, magnetic resonance or computed tomography can be used in diagnosis. X-ray examination is suitable for examining the lungs, since metastases can be present there too. If, after all the steps, the doctor has confirmed the presence of vulvar cancer, then it will be necessary to determine its stage.
What happens to organs during the development of the disease. Source: doctoros.ru
In medical practice there is its own classification for this. If we consider a four-level distribution, then thanks to it doctors can distinguish five stages:
- Zero – cancer cells are found only on the superficial skin;
- The first is that the localization of the pathological process has reached the vulva and perineal area, but the size itself is no more than two centimeters;
- Second - the description is identical to the first stage, but the size of the tumor exceeds two centimeters;
- Third, cancer cells spread to neighboring internal organs, often into the vagina or anus, and penetration into the lymph nodes is possible;
- Fourth, the lymph nodes are affected on both sides; the intestines, bladder, and urethra are involved in the pathological process.
It is very important that a woman undergo regular examinations by a gynecologist. This will allow the healthcare professional to diagnose cancer at an early stage. If vulvar cancer is detected, it is imperative to immediately begin the therapy prescribed by your doctor.
Vulvar cancer treatment
Treatment of vulvar cancer is carried out using the following methods:
- surgical;
- combined (surgical and radiation);
- complex and individual, combining radiation, medicinal and surgical techniques at the 4th stage and in case of recurrence;
- irradiation as an independent method or simultaneously with chemotherapy in case of absolute contraindications to surgical treatment.
Surgery on the vulva for cancer is performed by radical vulvectomy and femoroinguinal lymph node dissection. If the tumor is small, lymph node dissection is performed through separate incisions. If the tumor has spread over a large area, to hide the defects, tissue is removed from the vulva, pubis, perineum, thigh and groin on both sides using a one-piece plastic surgery method.
Treatment methods by stage
Squamous cell carcinoma of unknown etiology is most often described.
- Stage 0 (TisN0M0):
- the node is widely locally excised, departing from the edge 05-1.0 cm, and the operation is combined with laser treatment;
- skin vulvectomy is performed with tissue flap transplantation (or without);
- perform application chemotherapy with 5% Fluorouracil ointment.
- Stage IA (T1aN0M0):
- for microinvasive cancer, a tumor with d ≤ 2 cm and stromal invasion ≤ 1 mm is widely excised. If there is no severe diffuse dystrophy, inguinofemoral lymphadenectomy is not performed. The incision line is drawn at a distance of 1-2 cm from the edge of the formation circumference;
- carry out an urgent histological examination to determine the final extent of the operation;
- in case of multifocal lesions or the development of an oncological process in the vulva, cutaneous vulvectomy is performed simultaneously with dystrophic changes. Inguinal lymphadenectomy is not performed;
- Radiation exposure as an independent method is used if there are contraindications to surgery.
- Stage IB (T1bN0M0), carried out:
- radical hemi-vulvectomy and biopsy of sentinel lymph nodes are carried out when the diameter of the oncological node is <4 cm, inguinofemoral lymphadenectomy for metastases, the incision line from the edge of the node is 1-2 cm around the entire circumference;
- biopsy of sentinel lymph nodes on the affected side (lateral lesion) at a distance from the midline ≥ 1 cm, on one side inguinofemoral lymphadenectomy for metastases;
- bilateral biopsy of sentinel lymph nodes to determine the lesion: central (up to 1 cm from the midline), clitoris or posterior commissure; in case of metastases - bilateral inguinofemoral lymphadenectomy;
- radical vulvectomy and bilateral inguinofemoral lymphadenectomy with isolated removal of lymph nodes in the groin;
- radiation therapy for vulvar cancer: irradiation of inguinal lymph nodes (at N0) in women with medical contraindications or refusal of surgery;
- radiation methods using a radical program in case of a widespread tumor process or the impossibility of performing a radical vulvectomy.
- Stage II (T2N0M0)
They perform combined operations, combining chemistry and surgery for oncological processes in the lower part of the urethra and/or vagina, or anal ring.
The following methods are used:
- preoperative chemotherapy or chemoradiotherapy. At the same time, the operability of the node is increased and its size is reduced;
- radical local excision or vulvectomy and simultaneously bilateral inguinofemoral lymphadenectomy with a clinical incision line along the circumference up to 1-2 cm from the edge of the tumor masses;
- combined surgical intervention and simultaneously distal ureterectomy and/or distal vaginectomy for a tumor in the lower third of the vagina and/or urethra;
- treatment is prescribed as in the late stage of cancer, if the tumor has spread to the anal area;
- for the vulva area - postoperative irradiation and chemotherapy in the presence of: tumor > 4 cm, incision line < 8 mm, lymphovascular spread, tumor stromal invasion > 5 mm;
- for the area of regional and external iliac lymph nodes - postoperative chemotherapy and radiation if there is:
- macroscopic metastases in the RLU;
- more than 2 microscopic metastases in the RLU;
- radical radiation therapy if it is impossible to perform surgery due to too large areas of the oncological process or concomitant diseases.
- Stage III (T1,T2;N1a,N1b;M0), (T1, T2;N2a, N2b;M0)
Choose the following methods:
- neoadjuvant chemotherapy or radiation and excision of the remainder of the tumor masses;
- in case of oncological process in the lower part of the vagina and/or urethra - a combined operation: radical vulvectomy, inguinofemoral lymphadenectomy and simultaneously distal ureterectomy and/or distal vaginectomy, then postoperative chemotherapy;
- treatment as for the last stage of cancer, if the tumor has spread to the anal area.
- IVA stage (T1,T2;N3;M0), (T3NanyM0)
Choose treatment:
- radial;
- complex: superradical surgery + chemotherapy with Cisplatin at a dose of 40 mg/m² once every 7 days, using a neoadjuvant and/or adjuvant regimen;
- neoadjuvant chemotherapy and subsequent surgery or radiation.
- IVB stage (T any, N any, M1), (distant metastases)
Choose:
- chemoradiation methods according to a program compiled individually;
- individual palliative chemotherapy.
Relapses of the oncological process
Vulvar cancer can recur in the postoperative period, so treatment is carried out:
- surgical intervention in the presence of local relapses ± irradiation;
- radical vulvectomy and evisceration of organs in the pelvic area;
- chemoradiotherapy with or without surgery;
- if the iliac lymph nodes are affected and it is possible to operate them, radical lymphadenectomy and subsequent irradiation;
- palliative chemotherapy.
Important! Patients need to be observed and advised after treatment:
- 2 years – after every 3 months;
- 5 years – every six months after diagnosis;
- after 5 years - every year.
Radiation therapy
After surgery, the patient is irradiated for 21-28 days. External irradiation is performed on the primary tumor and areas of regional metastases (groin-thigh).
Carry out: conventional irradiation of primary tumor formation: ROD* 2-3 Gy, SOD** - 36-40 Gy (CT 2-2, 5D) and areas of regional metastases: ROD 2-3 Gy, SOD - 40 Gy (CT, 2- 2.5D) or conformal irradiation on the primary tumor: ROD 3 Gy, SOD 40 Gy (CT or MRI, 3D, electron accelerator with an MLC - multileaf collimator) and areas of regional metastases: ROD 2-3 Gy, SOD 40 Gy (CT , 2-2.5D, electron accelerator with the presence of MLC).
Therapy is carried out according to indications:
- intracavitary radiation using HDR brachytherapy devices (192Ir,60Co): SOD 28-30 Gy (3D with planning HR-CTV, IR-CTV);
- radical combined radiation;
- remote beam:
- conventional for the primary cancer node ROD 2-3 Gy, SOD 50-60 Gy (CT, 2-2.5D) and for areas of regional metastases - ROD 2-3 Gy, SOD 60 Gy;
- conformal irradiation to the primary oncological epicenter: ROD 2-3 Gy, SOD 50-60 Gy (CT or MRI, 3D, electron accelerator with the presence of MLC) and areas of regional metastases: ROD 2-3 Gy, SOD 60 Gy (CT or MRI, 3D, electron accelerator with MLC);
- intracavitary radiation, and use brachytherapy devices HDR (192Ir, 60Co): SOD 28-30 Gy (3D with planning HR-CTV, IR-CTV).
ROD is a single focal dose; **SOD is the total focal dose;
Chemotherapy
Chemistry is carried out according to one scheme:
- from 6 courses or until the oncological process begins to progress: neoadjuvant, 1st and subsequent lines;
- of 2-3 courses, using the neoadjuvant regimen.
For a minimal amount of chemotherapy, the following is administered:
- 50 mg/m² Cisplatin once, repeat 6 times every 21 days;
- 50 mg/m² Cisplatin on the first day + 500 mg/m² for 1-3 days. Repeat 6 times with an interval of 21 days.
Treatment is carried out with the optimal volume:
- Paclitaxel - 175 mg/m² + Cisplatin - 75 mg/m² on the first day, interval - 21 days;
- Paclitaxel -175 mg/m2 + Carboplatin AUC 5-6 on the first day, interval – 21 days;
- Cisplatin -50 mg/m2 on the first day + Gemcitabine 1000 mg/m2 on days 1.8, interval – 21 days;
- Xeloda-2500 mg/m2/day for days 1-14, interval – 21 days.
Systemic chemotherapy according to other regimens includes the following combinations of drugs:
- 500 mg/m² 5-fluorouracil – on day 1;
- 1.4 mg/m² Vincristine intravenously – on the 1st day;
- 15 mg of Bleomycin inside a vein or muscle – 5 days or 10 mg/m² inside a muscle – 2 times a week, for a total of 2-3 weeks. The interval between courses is 21 days.
Treatment of advanced or recurrent vulvar cancer is carried out according to the following polychemotherapy regimens:
- Cisplatin – 70-90 mg/m² – intravenous infusion (rate up to 1 mg/min) with pre- and post-hydration – on the 1st day. Vinorelbine – 25 mg/m² orally (injected over 6-10 minutes) – on the 1st and 8th days;
- Cisplatin – 75 mg/m² – intravenous infusion (rate up to 1 mg/min with pre- and post-hydration) – on the 1st day. Fluorouracil – 4 g/m², intravenous continuous infusion for 96 hours.
- Mitomycin C – 10 mg/m² – intravenously (injected over 20-30 minutes) – on the 1st day. Fluorouracil – 1 g/m², intravenous infusion for 24 hours. Start 30 minutes after IV Mitomycin C on days 1, 2 and 3.
Consequences of complex cancer treatment
After a vulvectomy: partial, local or complete, the lymph nodes may become enlarged.
When they are removed, lymphadenoma occurs:
- legs swell;
- fluid is retained in 55% of patients;
- sutures become inflamed and come apart in 30% of patients.
During surgery, the nerve may be damaged, which is manifested by a feeling of numbness, tingling, and the presence of cold and hot areas of the skin. In addition, a seroma appears near the suture - liquid under the skin, which prevents the suture from healing quickly. Thrombosis causes discomfort and pain in the groin area.
The consequences of radiation therapy for vulvar cancer can make life difficult for patients for many months or even years. The skin above the epicenter is damaged by the rays and causes hyperemia and inflammation in the form of dry and then wet-vascular epidermitis and other local inflammatory reactions.
To prevent this kind of complications, you will need Vinilin (balm), aloe liniment, Tezan, sea buckthorn oil and other special products for the skin and mucous membranes to lubricate the irradiated areas.
Local damage includes thinning of the skin, atrophy of the mucous membrane, dryness, death of the bulbs and loss of pubic hair. Pigmentation increases, capillaries dilate, and sclerotic tissue appears under the skin.
The consequences of chemotherapy manifest themselves as:
- decreased appetite and immunodeficiency;
- the appearance of anemia, nausea and vomiting;
- excessive fatigue and deterioration of general condition;
- decrease in hemoglobin with a deficiency of leukocytes, platelets and lymphocytes in the blood;
- baldness;
- complications in the gastrointestinal tract;
- persistent diarrhea;
- burning in the urethra;
- narrowing of the vagina;
- for pain in inflamed vaginal scars.
Metastasis
The stages of metastasis are determined by the lymph circulation of a given organ and its individual parts.
• The outflow of lymph from the external genital organs occurs through a group of superficial inguinal lymph nodes located directly under the Pupart ligament, numbering 12-16 and lying in front of the lata fascia of the thigh (stage I).
• Then the lymph enters the deep inguinal lymph nodes, located subfascially along the femoral vein in an amount of 3-5. One of the nodes of this group, the Cloquet lymph node, or Rosenmüllerian gland, lies in the femoral canal medial to the femoral vein (stage II).
• Further, the lymph flow is directed to the hypogastric, obturator and iliac lymph nodes lying along the hypogastric, obturator and iliac veins (stage III).
Lymph circulation of the clitoris occurs in a unique way with the help of two lymphatic “legs”. Lymph flows through the “lower leg” to the superficial inguinal lymph nodes. Through the “upper leg,” the lymph, bypassing the superficial inguinal lymph nodes, passes through the inguinal canal, accompanying the round ligament, and reaches the iliac lymph nodes.
In the upper third of the vulva there is a wide network of lymphatic anastomoses and the crossing of lymphatic tracts coming from the middle and lower third of the external genitalia.
The most important pathogenetically are metastases to regional lymph nodes.
Metastasis, as a rule, occurs by embolic route, and only when the lymph nodes are “blocked” by cancer cells does carcinomatous lymphangitis occur between the primary lesion and the secondary lymph nodes.
A feature of metastasis of cancer of the external genital organs in women is the staged, sequential damage to various groups of lymph nodes. Metastases to the pelvic lymph nodes appear late. The main role in metastasis is played by the duration of the process and the degree of its spread.
Photos of cancer of the external genitalia in women 18+
[collapse]
Traditional treatment for vulvar cancer
When diagnosed with vulvar cancer, treatment with folk remedies smooths out side complications after complex therapy. You can also treat cancer in its early stages at home.
For squamous cell carcinoma, greater celandine is used to provide antitumor, antiviral and anti-inflammatory effects. It has a weaker effect on the stratified epithelium of the vulva and rectum in the anal zone than on the single-layer epithelium behind the anus. But after the menstrual cycle, the epithelium of the vulva also becomes thinner, so celandine preparations will be highly effective for at least a week in this area. In this case, infuse the dried herb (1 tbsp) in a glass of boiling water for an hour. Then the genitals are irrigated or wet lotions are applied for 60 minutes - 3-4 times a day. Course duration is 1-2 months.
It is worth noting! It is contraindicated to use celandine for leukoplakia, increased inflammation and swelling.
As for hemlock oil infused with green seeds, use as an anti-cancer agent on areas of the skin where blood circulation is poor must be done with caution due to its toxicity. Oil from propolis and poplar buds relieves inflammation, allergies and itching, and heals damage. Oil from yellowing sophora and horse chestnut anesthetizes, increases microcirculation, kills microbes, relieves swelling, heals wounds and ulcers.
Ointment recipes:
- Mix beeswax (4 tbsp), lanolin (1 tbsp) and dry celandine grass powder (1 tbsp). The mixture is heated to dissolve the wax. After mixing thoroughly, allow the ointment to cool and lubricate the mucous membrane or apply it to the vulva on a piece of cloth for 15 minutes;
- mix Vaseline (4 tbsp) and celandine juice (1 tbsp), apply to the mucous membrane, or apply ointment to it on a piece of cloth for 15 minutes. Repeat the procedure 2-3 times a day, course – 2 weeks;
- Veselka mushroom powder (10 g) is mixed with heated propolis oil (10-15% - 100 g). The ointment is applied on gauze or a piece of tissue for swelling, itching and pain in the problem area.
Douching with veronica infusion is useful for vulvar cancer: add veronica (2 tbsp) to boiling water (0.5 l) and let it brew. Douching is performed at night for 15 days, then resumed after a week's break. In the morning, use a solution for washing: add 1 tbsp to 1 liter of boiling water. a spoonful of baking soda and a little shavings of tar soap to relieve itching. After the procedure, use sea buckthorn or fir oil to lubricate the vulvar mucosa.
To prepare the oil:
- fill the container 70% with raw materials;
- pour in unrefined sunflower oil;
- let it brew for 2-3 months in a warm corner;
- heat the jar with the contents in a bathhouse for half an hour to 40-45°C;
- strain until the oil cools.
Oil applications alternate with tampons in the vaginal area and the use of aqueous herbal decoctions for external use. Irrigations are carried out with infusions of collections of white sweet clover, gorse, Kuril tea (pentifolium), sage, white mistletoe branches, and barberry leaves. All herbs are taken in equal parts by weight, mistletoe and Kuril tea - twice as much. For infusion in a thermos you will need 1 tbsp. l. collection, 1 tsp. honey and 1 tbsp. boiling water
Dry plant powders can be used externally: mix the roots of yellow Sophora, hairy ash (roots), and Amur maakia bast (10:5:1). The powder is drawn into a dry syringe and sprayed onto the vulva. For ointment, the powder is mixed with petroleum jelly and applied to the tissue for pain and itching. After 2-3 hours, the remaining ointment is removed with a napkin moistened with olive oil.
If there are wounds and ulcers, then the vulva is cleansed with honey mixed with fish oil (3:1). Honey heals wounds, activates blood flow and lymphatic drainage, kills microbes, fish oil also heals ulcers and restores cell membranes due to anti-cancer vitamin A, softens the mucous membranes and skin.
Treatment
If vulvar cancer has been identified, treatment is prescribed by a leading specialist. In most cases, surgery is preferred, but chemotherapy, radiotherapy and biotherapy are also used. However, surgery is always a priority, since it allows you to remove part of the affected organ, but at the same time preserve the sexual functions of the body.
If the disease is detected at an early stage, limited surgery is performed. If vulvar cancer hurts a lot, your doctor can also tell you what to do. If such a symptom is present, it is worth considering that the disease has already reached its final stages. In this case, the operation will also be performed, but the intervention is already considered more large-scale (local).
There are several types of interventions through which vulvar cancer is treated. Operations can be performed using a laser beam, which will play the role of a regular scalpel, and its beam can remove damaged areas of the organ. When performing excision, the specialist aims to remove as completely as possible all cancer cells, as well as some of the healthy tissue around the pathological lesions.
Treatment can be carried out through vulectomy, which can be skinning, cutaneous, or superficial. The surgeon will gradually remove the top layer of skin that shows signs of cancer. Subsequently, if it is necessary to close the wound surface, grafts from other parts of the patient’s body are used.
Vulvectomy for oncology. Source: picstopin.com
When carrying out radiation or radiotherapy, there is a decrease in the depth of the oncological lesion, as well as a decrease in the tumor, which is very important to achieve immediately before the operation. This will make it easier to remove the tumor during subsequent interventions.
In addition, radiotherapy is used to treat lymph nodes; it is also used to reduce symptoms and improve the general condition and quality of life of a woman. Depending on the stage of the oncological process, the method of using radiotherapy will be determined.
In most cases, the implementation of chemotherapy is justified in combination with radiotherapy, since the former will act as palliative care. But they often resort to the use of creams, ointments and lotions that cover the skin in the affected area.
As for biological therapy, it is characterized as immunological treatment. Such an effect on the body involves taking synthetic or natural substances that provide additional support to the body and gives it the strength to fight cancer itself. Also, for this oncology, it is very effective to use a drug such as Imiquidone.
Patients should be aware that the rate of recurrence in cancer pathology is quite high. Thus, doctors claim that the disease returns in every fourth case after treatment. To avoid the development of complications, it is necessary to regularly visit a gynecologist who will conduct a preventive examination.
Life expectancy for vulvar cancer
Five-year survival rate for vulvar cancer is 23-60% of the total number of sick women, with local spread of the cancer process - 30%.
With early surgery, radiation and combined treatment of vulvar cancer, the prognosis for stages II–III is 58.7%.
If Cyclophosphamide or Methotrexate was administered before surgery at intervals of 7-10 days and then radical surgery was performed, the 5-year survival rate reached 72.1%.
Nutrition
Particular attention in the process of treatment and recovery is played by a properly selected balanced diet for vulvar cancer. First of all, patients are recommended to drink as much green tea as possible, approximately 4-5 cups per day. If this drink is natural, then thanks to the special components it will be possible to reduce the level of inflammation, which is definitely present during tumor progression.
When cancer develops, you need to eat a healthy and balanced diet. Source: zagge.ru
It is also necessary to include a large amount of garlic in your daily diet, as it helps improve blood circulation and also increases phagocytosis. In addition to this, you should also consume the following products:
- Onions and cabbage;
- Fruits and vegetables that are high in carotene (carrots, tomatoes, pumpkin, peaches, apricots, persimmons);
- Berries (raspberries, blueberries, blackberries, cranberries);
- Legumes;
- Flaxseed and olive oil;
- Sea kale;
- Rosemary, mint and basil.
If you take a large amount of vegetables and fruits, the substances they contain will help suppress the growth of tumor formation and neutralize carcinogens. In addition, the process of formation of healthy cells will improve. It is strictly forbidden to drink alcoholic beverages or sweets if you have cancer. You will have to give up drinking coffee and black tea.
Disease prevention
Patients who have already undergone radiation for vulvar cancer should have their blood tested every 3 months in the first or second year and every six months in subsequent years.
If anemia and leukopenia appear, then control tests are done more often. After irradiation, the body is strengthened with vitamins, quality nutrition, and also:
- re-transfusion of blood and its individual components: leukocyte and erythrocyte mass;
- drugs are used that stimulate leukopoiesis (reproduction of leukocytes) and eprythropoiesis (reproduction of red blood cells).
A healthy lifestyle and nutrition, movement and personal hygiene are the prevention of cancer.
Be healthy!
Prevention
The results of treatment for cancer of the external genitalia depend on the stage of the disease. However, despite the possibility of early diagnosis of cancer and timely treatment of precancerous conditions, this disease is not diagnosed in a timely manner. One of the reasons is the late presentation of patients. Therefore, widespread health education among the unorganized population would contribute to earlier appeal and earlier detection of this disease.
With an advanced form of cancer, it is necessary to implement a complex of treatment measures that would eliminate the possibility of relapse. Prevention of local cancer recurrences consists of performing wide extirpation of the entire organ using an electrosurgical method along with the surrounding skin.
To prevent regional metastases, it is recommended to remove the inguinal lymph nodes even in the absence of pronounced signs of their involvement by a cancerous tumor.
Prevention of cancer of the external genital organs in women in the broad sense of the word should consist of timely surgical treatment of all diseases in this area that have a long course. These include: leukoplakia, kraurosis, Bowen's disease, Paget's disease, Queyre's erythroplakia. Any disease of unknown nature that is not amenable to conservative treatment is subject to surgical treatment with histological examination.
The information presented in this article is intended for informational purposes only and cannot replace professional advice and qualified medical care. If you have the slightest suspicion that you have this disease, be sure to consult your doctor!
Diagnostic measures
During a gynecological examination, the tumor looks like a gray spot on the labia majora or minora. You can identify areas of ulceration and bleeding areas, swelling, and increased sensitivity of the vulva. Regional lymph nodes are enlarged and sensitive to palpation. To detect metaplasia, a smear is taken to check for the presence of atypical tissue.
Instrumental techniques
Diagnosis is carried out using a special microscope, under which you can examine the affected organ.
- Colposcopy is performed using a special device - a colposcope. Using it, you can examine the affected areas, their boundaries and the degree of infiltration under magnification. It also includes vulvoscopy, which is an examination of the vulva under a microscope.
- Ultrasound of the pelvic organs and lymph nodes is necessary to detect metastases, carcinoma germination, and determine the condition of the internal genital and urinary organs.
- Biopsy is the removal of a part from a pathogenic focus. The material is taken with a special thin needle and then sent for histological and cytological examination. This is necessary to determine the degree of malignancy of the neoplasm, aggressiveness of growth and detection of human papillomavirus.
- CT and MRI are diagnostic procedures with contrast that are used to identify distant sites of metastasis, the number and extent of affected lymph nodes. They study the patient’s body layer by layer, which makes it possible to study all the changes.
Preventive measures
To avoid the occurrence of a malignant tumor in the vulva area, it is important to undergo a timely preventive gynecological examination and, if necessary, treat genital diseases that can provoke the development of cancer. When the first symptoms of a dangerous pathology appear, you should consult a doctor as soon as possible, undergo a comprehensive diagnosis and begin therapy prescribed by a specialist.
Elderly women suffering from neurodystrophic disorders in the genital area and who are at risk should pay special attention to their health and refrain from self-medication.
Main symptoms of penile cancer
Penile cancer (photos below) initially appears on the skin in the form of a small spot that has a pink or red tint.
This spot is most often located on the head of the penis, but sometimes it appears in other places, for example, anywhere along the entire length of the penis shaft.
It does not hurt, there is no bleeding from it, and in general there are no specific inconveniences . But as the disease progresses, this spot enlarges, spreads across the penis, thickens and takes on the appearance of a tubercle.
From this moment on, a painful sensation appears and skin itching is possible, and there may be bleeding. If the foreskin is affected, there may also be a purulent discharge that has a strong odor. Outside the penis, enlarged lymph nodes are detected. All of the above are the main symptoms of penile cancer .
Also, as penile cancer (photos below) develops, the following symptoms appear:
- The appearance of pain during urination;
- Sleep disturbance, lack of sleep;
- General malaise and weakness throughout the body;
- Loss of body weight.
Cancer of the glans penis: causes
As for the etiology of penile cancer, it consists of many possible factors. It has long been confirmed by many medical staff that the development of this pathology is associated with a man’s bad habits , such as smoking and drinking alcohol, as well as with poor intimate hygiene.
It is noted that men who smoke are generally at greater risk of developing malignant neoplasms in the entire urinary system. This is mainly due to the fact that the products formed as a result of burning the contents of tobacco products have a carcinogenic effect.
As for not carefully observing intimate hygiene , this factor contributes to the accumulation of smegma and dead epidermal cells under the foreskin, which provokes irritation of the scalp and the formation of an inflammatory process. Having a permanent nature, all this increases the likelihood that cancer of the glans penis (photos are presented above).
Also, the cause of the development of cancer of the head of the penis may be the presence of phimosis , in which the foreskin compresses the head.
Other diseases, such as Bowen's disease, leukoplakia, Kaposi's sarcoma and Queyra's erythroplasia, can also be development factors. The reasons include a variety of sexually transmitted infections and promiscuity in general.
Etiology
The etiology of this disease is not well understood. It is impossible to say exactly what exactly is the provoking factor of this disease. According to clinicians, the oncological process develops as a result of hormonal changes in the reproductive system, which occurs during menopause and menopause. This process, in turn, leads to a decrease in the sensitivity of receptors to estrogen substances.
Predisposing factors for the development of cancer are the following:
- dystrophic processes in the genital area;
- vulvar dysplasia;
- papillomavirus infection;
- diabetes;
- HIV;
- obesity;
- early menopause.
In addition, etiological factors for the development of vulvar cancer include sexually transmitted diseases, frequent changes of sexual partners and abuse of alcoholic beverages and smoking. It should also be understood that none of the above etiological factors is a 100% predisposition to the development of vulvar cancer. However, with a favorable clinical picture, it can provoke the development of the disease.
Prognosis for benign tumors of the vulva
Benign neoplasms of the vulva can pose a danger only if they become malignant. However, this happens quite infrequently. Thus, they do not entail a great risk to life and health.
Recurrence of neoplasms is possible, especially when it comes to papillomas. To prevent this, antiviral treatment should be carried out after removal.
In addition, there is a risk of injury during the operation.
Kinds
The causes and symptoms of cancer of the male reproductive organ largely depend on the form of the disease. In medicine, penile tumors are classified into the following forms:
- nodular - a round neoplasm with a smooth surface appears under the skin of the penis and does not cause pain;
- ulcerative - small ulcers form on the head of the penis or foreskin, when palpated, pain occurs, and in case of injury they can bleed;
- papillary - looks like a cauliflower branch;
- edematous - a small node forms on the penis, accompanied by swelling of the genital organ and phimosis of the foreskin.
When cancer of the glans penis or other parts occurs, therapy depends directly on the form of the disease. The most common is HRC carcinoma, therefore, during diagnosis, symptoms with suspicion of this disease are first studied.
Side effects of treatment
As for radiation therapy and brachytherapy, a side effect of such treatment can be the formation of local complications, strictures of the urethra and necrosis of the entire penis. A side effect of laser therapy is postoperative bleeding. But they occur only in 7% of all cases of such treatment.
After surgery, there may be a narrowing of the urethra, insufficient length or rigidity of the penis, which prevents sexual intercourse, as well as a decrease or complete loss of sensitivity of the organ.
Possible complications
In the absence of timely and adequate treatment, a cancerous tumor in the vulva area leads to damage to internal organs and death. The type and stage of the disease plays a major role in the development of complications. Most often, the death of patients is caused by a pathological process localized in the clitoral area, accompanied by the appearance of large areas of infiltration and tissue swelling.
Complications can also arise after surgery on the genitals.
The most common consequences of the operation are:
- infection of the wound surface, suppuration of the lesion;
- thrombosis;
urinary and fecal incontinence;
- stenosis of the vaginal vestibule;
- cystic formations in the area of the inguinal lymph nodes;
- swelling of the lower extremities.
Even after complete cure of vulvar cancer, the possibility of a recurrence of the disease cannot be ruled out. Reviews from patients indicate that re-development of a malignant tumor is observed in 15-40% of cases. At the same time, doctors give a favorable prognosis only if the cancer process occurs in isolation, without affecting the lymph nodes.
Types of labia cancer
All types of labia cancer are classified according to their structure, growth patterns, and place of initial formation. Thus, cancer is primary and secondary, when the focus develops from hematogenously or lymphogenously brought atypical cells. The TNM classification helps to get an idea of the prevalence, give a detailed description of the stages, and determine the prognosis. It is used when making a diagnosis in a medical history and issuing a doctor’s report.
According to the cytological picture, the following types of cancerous tumors are found:
- • squamous cell, its varieties - keratinizing and non-keratinizing;
- • glandular;
- • basal cell (rare).
Cancer is classified according to the type of growth:
- • exophytic (nodular, papillary) - a lump-like node on a stalk;
- • endophytic (ulcerative) - a retracted ulcer with dense edges is detected;
- • infiltrative – expressed by thickening of the labia.
Stages
In medicine, there are four main stages of the oncological process, each of which has its own specific characteristics. Initially, stage zero is diagnosed; in this condition they speak of pre-invasion or pre-invasive carcinoma. At the first stage, the tumor is no more than 2 cm in diameter, there are no metastases, the second stage is characterized by an increase in the tumor to 2 cm or more, there are no metastases.
Subsequently, the third stage develops. Here, grade 3A can be diagnosed, in which the tumor grows into neighboring organs, for example, the vagina and urethra are affected, but there is also no metastasis. Stage 3B has the same symptoms as stage 3A, but metastases appear.
If left untreated, the disease progresses and is diagnosed as stage 4A. In this condition, there is complete damage to the urethra and rectum. Stage 4B can also be identified, in which all grade 4A transformations are noted, and the presence of metastases in regional lymph nodes and distant organs is noted.
What are the stages of vulvar cancer?
The stages of cancer are classified in various ways.
The four-level classification system for vulvar cancer includes the following five stages.
- Stage zero or carcinoma in situ: Cancer is present only on the surface of the skin.
- Stage one: The cancer is limited to the vulva or perineal area, and its size does not exceed two centimeters.
- Stage two: The cancer is limited to the vulva or perineal area and is at least two centimeters in size.
- Stage three: The cancer has spread to nearby organs, such as the anus or vagina. In addition, it can get into the lymph nodes.
- Stage four: The cancer has reached the lymph nodes on both sides of the groin. It can also reach the intestines, bladder and urethra.
Important! To effectively treat cancer and prevent the spread of the disease, diagnosis should be made as quickly as possible.
Prevention of labia cancer
Regular gynecological examinations help prevent the development of labia cancer, which not everyone can avoid. It is also advisable to follow the recommendations of oncologists to reduce the risk of getting sick. Increased immune status protects well from cancer, for which it is recommended to lead a healthy lifestyle, which includes:
- • moderate physical activity, hardening;
- • absence of bad habits (alcohol consumption, smoking, drug addiction should be excluded);
- • diet and proper diet with foods rich in vitamins, microelements, and plant fiber;
- • proper sleep and rest (it is better to avoid stressful situations and overwork, which, according to psychosomatics, provoke cancer);
- • genital hygiene;
- • maintaining normal weight;
- • absence of promiscuity.
Classification
It is not enough to just know what labia cancer looks like, but also to understand by what principles it is classified. In modern medicine there is no uniform distribution scheme, but sorting by stage, degree of prevalence and growth pattern is widely used.
Based on the type of growth of a malignant neoplasm, the following are distinguished:
- Exophytic - the pathological focus is localized above the skin and is presented in the form of a dense node;
- Endophytic – atypical malignant cells grow deep into the organ, against which an ulcer appears;
- Infiltrative - this type of growth is also called edematous or diffuse, and an infiltrate is formed on the entire surface of the labia.
Pathological formations may also vary in degree of prevalence. If the tumor remains in place, then they say that there is no infiltrative growth, there is microinvasive cancer (the depth of tissue damage is not more than 5 mm), invasive cancer, which can be squamous cell, basal cell and poorly differentiated.
The principle of the formation of metastases in the body. Source: lecheniemiomy.ru
As for the occurrence of metastases, secondary foci can be formed due to the spread of pathological cells throughout the body through the blood or lymph (hematogenously and lymphogenously, respectively), and more often the inguinal, glomerular and lumbar nodes are involved in the process.
Complications and consequences
Penile cancer is a complex disease that can lead to the development of some complications. The most common possible consequences are:
- Difficulties during or complete impossibility of intimacy;
- Loss of body weight;
- Development of anemia;
- Impairment in the bladder emptying system, which in turn can lead to the formation of pyelonephritis;
- Metastasis, in other words, the spread of tumor cells throughout the male body;
- Blockage of the urethra.