What is intestinal hyperplasia
This pathology means excessive production of intestinal lymphoid tissue cells, which leads to its growth in the mucosal and submucosal layers of the organ. At the same time , the mass of the intestine increases, its functioning is disrupted .
The disease is diagnosed in people of both sexes of any age. The occurrence of intestinal hyperplasia is not associated with eating certain foods and does not depend on the area of residence.
There are many reasons for the development of pathology. They look like this:
- Various disorders of the secretory processes of the intestinal mucosa.
- Hormonal disorders of the body.
- Damage to organ tissues by autoimmune, carcinogenic cells.
- Violation of the nervous regulation of the gastrointestinal tract.
- Long-term chronic stressful situations.
- Colonization of the intestines by pathogenic bacteria.
- Disorders of the immune system.
- Disorder of gastrointestinal motility.
The clinical picture of the disease largely depends on which part of the intestine is affected. The general condition of the body may suffer, the patient becomes weak, and body temperature rises periodically. There are also often complaints of spastic abdominal pain.
Patients may be bothered by long-term diarrhea (stool often contains bloody and mucous impurities), flatulence. In the case of a protracted course of the pathology, a decrease in the patient’s body weight is often diagnosed.
Find out how rectal pain is treated.
Hyperplasia of the gastric mucosa
Have you been struggling with GASTRITIS and ULCERS for many years without success?
“You will be amazed at how easy it is to cure gastritis and ulcers just by taking it every day.
Hyperplasia is the abnormal growth of tissue caused by accelerated cell division. A similar process can develop in almost any organ, the stomach is no exception. Let's consider gastric hyperplasia - what it is, how it is characterized and whether this pathology can be treated. In the gastric layer, it forms quite often and is considered a very dangerous process, since accelerated cell division and proliferation in many cases leads to neoplasms. In some cases, the disease is not limited to cell growth alone; structural changes occur - however, already at advanced stages.
Which guts does it hit?
This pathological process can be diagnosed along the entire length of the gastrointestinal tract. But the most common location of hyperplasia is the small intestine .
This is explained by the fact that this department is constantly in contact with pathogenic microflora, viral and autoimmune agents.
It is important to note that the final section of the small intestine is rich in lymphoid tissue, which functions as the body’s immune defense, so it is most susceptible to hyperplasia. This is often observed with viral infections and helminthic infestations.
This applies to the crypts of the large intestine. These formations also perform the function of immunoprotection and contain hormonal cells. For this reason, they often increase in size. Therefore, focal hyperplasia of the crypts of the colon mucosa is quite often diagnosed in gastroenterology.
It is important that various helminths also often affect this part of the digestive tract. This pathology of the mucous membrane is a reaction of the intestine to invasion.
Rectal mucosa, structure, features of functioning
The rectal mucosa is covered by columnar epithelium, which is equipped with a large number of bacilli cells. It also contains quite a lot of liberkühn glands, which are almost entirely formed by mucous cells. This can explain the fact that in the case of the development of pathologies of various types, abundant mucous discharge is observed from the rectum.
Just above the anus there is a series of vertical formations. These elevations are called the columns of Morgagni. They look like longitudinal rollers. They are formed by a fold of the mucous membrane and rise 2-4 cm above the mucous membrane itself. Indentations are formed between the columns, at the end of which there are blind pockets. They can often retain particles of feces and foreign bodies, which subsequently provoke the development of inflammatory processes.
The composition of rectal mucus has enzyme components that contribute to the partial processing of nutrients. Everything that is not processed is formed into feces and excreted from the body.
What is focal hyperplasia
Focal hyperplasia means the formation of areas of lymphoid growths that have boundaries. This condition is diagnosed more often, in some cases it is considered as a variant of the norm.
Sometimes patients do not notice any changes in the functioning of the gastrointestinal tract throughout their lives. But if the growth process progresses, then clinical signs of the presence of a pathological process in the body will gradually appear .
Lymphoid cells initially form into follicles, which aggregate into larger conglomerates. The latter, in turn, are capable of forming cell colonies.
Etiology
Lymphofollicular hyperplasia of the stomach is an increased proliferation of tissues and cells in the gastric mucosa. This condition occurs as a result of the negative impact of external and internal factors, which, as they influence, modify the structure of the membrane, significantly increasing the number of new cells. The reasons for these changes may be various factors, namely:
Very important! Savina G.: “I can recommend only one remedy for the quick treatment of ulcers and gastritis” read more.
- internal secretion disorders;
- hormonal imbalances;
- influence of carcinogens;
- disruptions in the digestive tract;
- the influence of specific tissue breakdown products;
- bacteria Helicobacter pylori;
- constant stress;
- autoimmune diseases;
- hereditary predisposition;
- herpes infection;
- chronic gastritis;
- inflammatory processes in the body.
Hyperplasia of the gastric mucosa is characterized by the formation of an abnormal number of cells and tissues; over time, the follicular tissue of the submucosal layer increases, which leads to the formation of the disease. This process can be triggered by obesity, various liver dysfunctions or hyperglycemia. In medicine, a hereditary factor is considered as a risk of a disease. Active cell proliferation leads to the formation of compactions, diagnosed as gastric polyposis. These accumulations increase over time and can trigger the formation of tumors.
Manifestations of the disease are similar to other pathological conditions and are easy to confuse. Only a specialist can make a diagnosis and prescribe treatment.
THIS IS REALLY IMPORTANT! Right now you can find out a cheap way to get rid of stomach pain. FIND OUT >>
What can it lead to?
Clinically, focal intestinal hyperplasia occurs when lymphoid cells aggregate into larger structures. In such situations, hyperemia of the intestinal mucosa occurs.
Its structure gradually becomes thinner, the wall becomes covered with erosion. The progression of erosion can lead to destruction of the mucous membrane and gastrointestinal bleeding. This condition is a dangerous complication because it can be fatal.
In addition, a long course of the disease can lead to exhaustion of the body and loss of body weight . The emotional state of patients suffers seriously; they often become depressed and irritable.
Prevention measures
To prevent gastric hyperplasia, the following recommendations must be followed:
- Eat properly. Eliminate fried, spicy, smoked foods from your diet. Eat often and in small portions. Try not to overeat, and your last meal should be at least 2 hours before bedtime.
- To live an active lifestyle. Walk more in the fresh air. But it is recommended to avoid heavy physical activity.
- Stop smoking and drinking alcohol.
- Avoid stressful situations, use sedatives if necessary.
It is also important to have regular checkups with your doctor. Routine medical examinations will help avoid not only the development of hyperplasia, but also other dangerous diseases.
Is it curable or not?
The answer to this question is decided individually for each patient. If the pathology is associated with temporary disturbances in the functioning of the body, then after they pass, hyperplasia will disappear. This applies to hormonal disorders, autoimmune diseases, pathologies of the immune system, and helminthic infestations.
It is important for the attending physician to identify the main cause of hyperplasia of the intestinal mucosa. It must be remembered that in some situations this condition is a variant of the norm. It is important for patients to be constantly under the supervision of their attending physician.
Surgical treatment is indicated in cases where foci of hyperplasia rapidly increase in size, which leads to disruption of the functioning of the organ, also with a high risk of bleeding, and a severe clinical picture of the disease.
Surgery is mandatory in cases where there is a suspicion of an oncological process.
It is important to note that hyperplastic lesions may appear in certain areas of the intestine and then disappear during the life of almost every person.
In most cases they pose no danger. However, if the symptoms listed above appear, you should definitely consult a doctor.
Symptoms and signs
The clinical course of the disease is characterized by secrecy. In the early stages of pathology formation, the patient may not present any complaints. In such cases, hyperplasia becomes an accidental diagnostic finding during FGDS. Further progression of the disease leads to a number of symptoms that are not specific. Among them:
- Anemia. A decrease in hemoglobin levels most often occurs due to tissue changes in the fundus and body of the stomach. The cause is a disruption in the production of internal factor Castle (a specific enzyme). The second sign is a tendency to bleeding in the area of pathological growth.
- Pain syndrome. It often occurs during hunger or at night (due to the active production of hydrochloric acid). Symptoms range from mild intermittent discomfort to a systematic feeling of pain.
- Dyspepsia. Hyperplasia of the gastric mucosa leads to indigestion. Manifests itself in the form of nausea and occasional diarrhea.
About the disease
Lymphofollicular hyperplasia can affect the organs of the endocrine system and intestines, but the most common is hyperplasia of the stomach and intestines. This is probably due to a large number of risk factors for all parts of the gastrointestinal tract:
- long-term inflammatory processes in the stomach, for example, chronic gastritis; - consumption of carcinogens, that is, products containing dangerous additives with the letter code E; — damage to the mucous membrane by Helicobacter pylori bacteria; - prolonged stress.
When the endocrine system is damaged, the trigger is often an existing endocrine or systemic disease. Thus, there is lymphofollicular hyperplasia of the thymus, which develops against the background of an existing lesion of the pituitary gland.
Causes
Various factors can trigger the development of the disease, including:
- hormonal disbalance;
- chronic gastritis;
- peptic ulcer;
- hereditary tendency to focal hyperplasia;
- an abnormal deviation in the regulation of the functioning of an organ by the nervous system;
- advanced form of chronic inflammation of the mucous membranes of the organ;
- incompletely cured infectious diseases in the stomach;
- Helicobacter;
- defects in the intrasecretory functioning of the stomach;
- negative impact of a carcinogen or other chemical compounds on mucous membranes.
Diagnostics
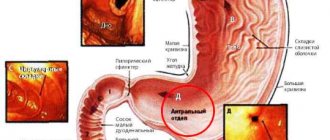
Since the disease is characterized by the proliferation of the mucous layer, its localization in the stomach and intestines can be detected using endoscopic methods (FGDS, colonoscopy, sigmoidoscopy), as well as during X-ray examination with contrast. During X-ray diagnostics, using contrast distribution, you can determine the degree of proliferation of newly formed tissues. And with endoscopic methods, it is possible to obtain altered tissue for histological examination.
Damage to the endocrine system is characterized by changes in the blood picture with high lymphocytosis. A significant increase in lymphocytes should always alert the doctor.
With a confirmed diagnosis of Lymphofollicular hyperplasia, it is necessary to undergo regular examinations, because abnormally overgrown tissues have a tendency to become malignant. And if this happens, then early detection of the process contributes to a good prognosis.
Nutrition for hyperplasia of the gastrointestinal tract
In order for the treatment to give a positive result, the patient first needs to reconsider his diet. For stomach pathology, it is recommended to use:
- Fresh vegetables and fruits.
- Lean poultry meats.
- Low-fat fermented milk products.
- Various cereals.
The doctor must tell his patient about the dietary habits during the treatment and rehabilitation period. Also, such a diet will be recommended to them for prophylactic purposes to prevent relapse of the disease.
What is lymphofollicular hyperplasia?
Generalized signs of lymphofollicular hyperplasia are considered to be an increase in temperature, a feeling of weakness, a quantitative increase in lymphocytes
Lymphoid hyperplasia of the gastrointestinal tract is divided into local (local) and diffuse (scattered). With local lymphoid hyperplasia of the colon, visible polyps are formed. Diffuse lymphoid hyperplasia is a scattered benign neoplasm; it is thought to be a general response of mucosal lymphoid cells to an unknown stimulus.
Nodular lymphoid hyperplasia of the duodenal bulb is characterized by multiple individual mucous nodules. The most common cause of malignant lymphofollicular hyperplasia of the intestine or stomach is extranodal B-cell lymphoma from marginal zone cells (maltoma, or MALT lymphoma).
Some studies show that maltoma is slightly more common in women than in men. No significant racial differences in disease prevalence were identified; Some studies suggest that lymphofollicular hyperplasia of the ileum is slightly more common in white people than in black people.
Symptoms
Symptoms of LFH vary greatly and depend on the underlying cause. In some cases, they can also be similar to the symptoms of stomach cancer. However, some patients are more likely to suffer from heartburn, nausea, vomiting, diarrhea and flatulence.
Initially, patients feel weak, suffer from loss of appetite, and sometimes nausea. Sometimes there is a diffuse feeling of pressure in the abdomen. Only at the last stage, in addition to night sweats, abdominal pain and fever occur. Sometimes body weight decreases.
With LFG of the intestine, intestinal bleeding is possible.
Causes
Concomitant problems - obesity, liver dysfunction - can trigger the pathogenic mechanism of lymphofollicular hyperplasia
During infections or inflammations in the body, the work of the immune system is enhanced: the division of immune cells - lymphocytes - accelerates in the lymph nodes. The main function of lymph nodes is to filter lymph. To ensure immune functions, the lymph nodes become significantly enlarged - this is a normal and healthy sign of increased immune activity.
The lymph node may also become enlarged due to the growth of malignant cells. As a rule, lymph nodes affected by cancer do not cause pain when touched and are difficult to move because they merge with the surrounding tissue.
There are numerous lymph nodes in the wall of the stomach. If they are malignantly enlarged, they are called gastric lymphoma. Most gastric lymphomas are malignant maltomas that are limited to the gastric mucosa. MALT stands for mucosa-associated lymphatic tissue.
There are primary and secondary gastric lymphomas. Primary make up about 80% of all lymphomas of the digestive tract. They develop directly from lymphoid cells of the gastric mucosa. There are no other diseases that would contribute to the development of the disease. Secondary gastric lymphomas develop as a result of metastasis of tumors located in other organs.
The ileum constitutes approximately 60% of the entire length of the small intestine and is thus up to 3 m in adults. The ileum contains a large number of lymphoid follicles called Peyer's patches. Lymphofollicular hyperplasia of the ileum occurs due to primary or secondary immunodeficiency, as well as chronic inflammatory bowel disease - Crohn's disease.
Diet and lifestyle changes
The patient's nutrition is of great importance in the treatment of hyperplasia.
It is completely prohibited to use:
- canned food;
- spicy seasonings;
- overheated dishes;
- foods with a predominance of fats;
- any spices;
- roast;
- alcohol;
- lemonade.
It is recommended to constantly include lean meat or fish, cereals, vegetables, and fruits in your daily diet. All dishes must be served chopped. Food should be steamed, boiled, stewed. It is advisable to adhere to the principle of fractional nutrition. Don't overload your stomach.
Lifestyle adjustments are also necessary. It is necessary to take vitamins, and use medications required for treatment only as directed and under the strict supervision of the attending physician.
Diagnostics
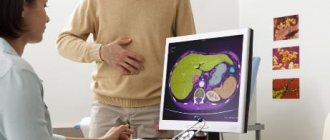
Examinations allow us to determine the level of spread of neoplasms, and endoscopy allows us to obtain the necessary sample of tissue for a biopsy in order to obtain information about the presence or absence of histology
First, a physical examination of the patient is performed and a history is taken. Imaging techniques (computed tomography, magnetic resonance imaging, and positron emission tomography) do not accurately visualize LPH but may be helpful in confirming the diagnosis.
Gastroendoscopy can reveal local changes in the gastric mucosa.
Colonoscopy and sigmoidoscopy are used to identify lymphofollicular intestinal hyperplasia.
Signs of bone marrow damage can be identified by histological examination. Histologically, lymphofollicular hyperplasia of the gastric mucosa is characterized by a large number of immunocompetent cells in the lamellar layer of the mucous layer.
Cytogenetic studies can reveal chromosomal abnormalities in malignant cells. The most common anomalies are trisomy 3, t(11;18) and, less commonly, t(1;4).
Diagnostic measures
To make an accurate diagnosis, you need to see a doctor. The doctor relies not only on the symptoms, but also on the results of the examination. It is very important to differentiate hyperplasia from chronic gastritis and ulcerative lesions.
First of all, the patient is sent for gastroscopy. An endoscope containing a camera and a light bulb is inserted into the stomach through the mouth. The doctor examines the walls. If there are changes in the walls, he begins to examine them more carefully.
After this, tissue is collected for examination. Using histology, it is possible to determine the type of disease and cause.
Ultrasound, computed tomography or magnetic tomography are used as additional diagnostic methods.
Treatment
You should not try to cure the disease on your own; if you detect the first signals of an impending disease, you should consult a gastroenterologist for advice
Benign lymphofollicular hyperplasia does not require treatment.
If a malignant growth of gastric lymphoid tissue is diagnosed at an early stage, antibiotic therapy can help eliminate Helicobacter pylori.
Most lymphofollicular hyperplasia of the gastric antrum respond to modern treatment methods - radiotherapy and chemotherapy.
In later stages, surgery may help by removing only the affected part or the entire stomach. Complete removal of the stomach is called a gastrectomy.
Tumors that are limited to the inner layer of the stomach wall (mucosa) can be removed during gastroscopy. In this case, only part of the tumor and immediately adjacent tissue are removed. For deep-seated tumors, part or all of the stomach, including surrounding lymph nodes, the spleen, and part of the pancreas, must be removed. To restore the passage of food, the rest of the stomach, or the end of the esophagus, is connected to the small intestine.
Additional chemotherapy (given both before and after surgery) may improve the chances of survival for patients with locally advanced tumors that have an increased risk of recurrence.
If the tumor has spread to the abdomen (peritoneal carcinomatosis), the patient's life can be prolonged by surgical removal of the affected peritoneal membrane in combination with so-called hyperthermic intraperitoneal chemotherapy.
If the tumor cannot be completely removed, surgery is not performed. In this case, drug treatment (chemotherapy, possibly in combination with other medications) can relieve symptoms, prolong and improve quality of life.
If the stomach is severely compressed by a tumor, inserting a plastic or metal tube (called a stent) may help you eat normally.
Many patients suffer from digestive problems after surgery.
Symptoms of both types of hyperplasia
In the initial stages, the disease does not make itself felt. A person remains in good health, so he does not worry about his health again. Complaints begin to appear only after hyperplasia of the digestive organ begins to progress at an accelerated pace. This happens if a person continues to lead the same lifestyle that led to such an illness.
In later stages, the disease can be recognized by the following signs:
- Severe pain in the upper abdomen, where the stomach is located. Unpleasant sensations are caused by involuntary muscle contractions. The pain can be either temporary or permanent.
- Stomach dysfunction.
- Anemia cannot be ruled out.
When stomach pain occurs, many people try to suppress it with painkillers. But in this case you can’t do that. You should immediately contact a specialist so that he can find the cause of the discomfort and offer suitable treatment. This is especially important in the case of hyperplasia, since pain indicates its rapid development.
Stages of lymphofollicular tissue proliferation
Depending on the size and stage of follicle reproduction, hyperplasia can be classified into stages:
- At the zero and weakest stage, follicles are present in minimal numbers. They are difficult to distinguish due to their small size and scattered location on the walls of the stomach.
- The first stage involves the presence of isolated cases of scattered growths of small microorganisms on the mucous membrane.
- At the second stage, more noticeable and dense neoplasms can be detected. However, they are separated from each other and do not form mergers.
- During the third stage, the presence of large groups of overgrown follicles with hyperemic mucous membrane is noticed.
- The last fourth stage implies the presence of erosion of the walls of the organ. Hyperemia of the mucous membrane with fibrinous plaque and a pronounced vascular pattern.
This picture shows that it is almost impossible to identify the disease in the early stages. Only at stages 3 and 4 noticeable clinical phenomena appear, such as severe pain in the stomach and bleeding. It is possible to detect the disease in the first stages only if you undergo regular examinations by a gastroenterologist.