When menopause occurs, the female body experiences hormonal changes. There is a decrease in sex hormones, reproductive function fades, and during menopause the monthly renewal of the uterine mucosa does not occur. During this period, a woman needs to closely monitor the health of the reproductive system. Problems do not end with the onset of menopause. Endometrial hyperplasia often occurs during menopause. A woman must know what it is so as not to miss the initial development of the pathology. Symptoms detected in time and treatment prescribed by a specialist will help stop the development of the disease, but for this the woman herself must monitor her health and undergo regular preventive examinations.
What is menopause and when does it occur?
Menopause is the 12-month period after the last natural periodic discharge in women, occurring between the ages of 45 and 55 years. It is caused by depletion of the follicle supply. If menopause occurs before the age of 40, then this process is called ovarian wasting syndrome. Some women experience late menopause - after 55 years.
There are cases when the pause is caused artificially. In this case, a woman stops menstruating due to surgical removal of the ovaries, chemotherapy, or medication.
During menopause, the female body changes. The changes are caused by a lack of hormones and changes in the functioning of the ovaries. It is at this time that the risk of developing many gynecological pathologies, such as uterine cancer and endometrial hyperplasia, increases.
https://youtu.be/t2N031WSl3E
Causes of the disease
Normally, with a deficiency of the hormone estrogen in the female body, dystrophy of the epithelium of the inner layer of the uterus is observed, but ovarian dysfunction leads to various pathological changes in the ratio of hormones. In this case, an atypical reaction from the mucous membrane is observed in the form of endometrial proliferation. The reasons for the appearance of pathology and subsequent curettage are:
- uncontrolled use of hormonal drugs;
- chronic inflammatory processes in the uterine cavity;
- numerous surgical interventions (abortions, operations);
- history of infectious diseases of the genitourinary system;
- diabetes;
- hereditary factor.
Note! The risk group for endometrial hyperplasia includes overweight women suffering from hypertension and chronic liver diseases.
General information about the disease
By the term “hyperplasia,” doctors mean tissue proliferation. It occurs due to excess cell production. The endometrium is the inner lining of the uterus. It provides the fetus with optimal conditions for full development. Each menstrual cycle, the thickness of the endometrium changes. The thinnest layer occurs immediately after the end of menstruation. During ovulation, the endometrium thickens up to 8 mm under the influence of the hormone estrogen. If conception does not occur, the level of hormones decreases due to the production of progesterone, the internal mucous membranes of the organ are depleted, the egg leaves the body - menstruation begins.
During menopause, hormonal levels are disrupted. Under the influence of increased levels of estrogen, the endometrium increases in volume. Due to the reduced level of progesterone, this process does not stop. In most cases, endometrial growth is characterized by premenopause. Indeed, despite the presence of monthly discharge, age-related changes occur in a woman’s body, accompanied by changes in hormonal levels.
What types of hyperplasia are there?
The types of endometrial hyperplasia in menopause depend on which mucosal cells predominate in the abnormal formation.
Classification.
Experts identify the following types of disease:
- Glandular - the mucous membrane grows towards the tissues of the uterus due to an increase in the size of the glands located in it. In this case, their shape is disrupted.
- Cystic - due to the fact that the cells of the mucous membrane overlap the glands, they begin to swell and form cysts. The likelihood of this type of disease degenerating into oncology is very high.
- Focal (polypoid) - polyps (growths on a thin stalk) grow from gland cells, around which separate areas (foci) of endometrial growth appear.
- Atypical (adenomatous) - due to the rapid change in the shape and size of the cells of the mucous membrane, the endometrium very actively grows into the tissues of other organs. This form of the disease is very dangerous because it turns into cancer in a short period of time. During menopause and postmenopause it is quite rare, since hormonal changes lead to a slowdown in all processes occurring in the body.
- Basal is a very rare type of disease in which cells of the basal layer of the endometrium grow deep into the tissues of the uterus.
A woman may develop a combined type of disease. For example, glandular cystic hyperplasia. In this case, in addition to the growths of the mucous membrane, which consist of glandular tissue, cysts and nodules are formed.
Endometrial norms
During menopause, the endometrium becomes thinner. Its thickness varies within 5 mm. Doctors consider this indicator to be normal. Sometimes the growth of the endometrium during menopause reaches 7-8 millimeters. This indicator indicates the possible onset of a pathological process, but is not yet classified as hyperplasia. For some patients, tissue thickness of 7-8 millimeters is the norm. But doctors recommend periodically undergoing ultrasound (every 3-6 months) in order to exercise dynamic control over tissue proliferation.
If the endometrial thickness reaches more than 8 mm, gynecologists recommend that the patient undergo a curettage procedure. It is necessary to confirm the development of the pathological process, study the tissue structure and prescribe treatment.
Preparing for scraping
Since endometrial curettage is a surgical procedure, it requires careful preparation (except in cases of emergency cleaning).
Firstly, you need to remember that the procedure is done on certain days of the menstrual cycle. Secondly, you need to be examined by a cardiologist, neurologist, therapist and pass a full list of necessary tests.
The list of mandatory tests before endometrial curettage includes:
- general blood test (finger prick) and urine test,
- determination of blood clotting characteristics (sampling from a vein),
- blood chemistry,
- testing for antibodies to hepatitis, HIV, syphilis (RW analysis),
- microscopy of a vaginal smear to determine the degree of purity,
- secretion seeding tank,
- determining the level of female hormones,
- electrocardiogram (ECG).
We also need two ultrasound examinations in two different cycles, which show that the thickness of the endometrium is more than 1.5 cm. The manipulation is done before the start of the expected menstruation, when the thickness of the functional layer is maximum for removal.
14 days before the intervention, the patient is advised to stop taking medications or dietary supplements, except those prescribed by the attending physician. Before curettage, thorough cleansing of the body is necessary so that rehabilitation is faster and more effective.
Important! Anticoagulants must be discontinued to avoid severe bleeding during manipulation. A week before surgery, sexual relations are limited or completely excluded, especially if contact bleeding is present. Douching is also canceled. You should avoid eating food 12 hours before the procedure, and drinking 6 hours before the procedure. In the evening, on the eve of the procedure, a cleansing enema is performed.
The only case when curettage is carried out without tests and preliminary preparation is if the patient is transported by ambulance with severe bleeding.
Classification of the disease
There are several types of endometrial hyperplasia. They differ in the direction of tissue growth:
- Glandular hyperplasia of the endometrium is diagnosed if the layer of the inner lining of the uterus increases due to modification of the glands located in it. The increase in volume occurs in the direction of the muscles of the organ.
- Cystic form. Cystic formations begin to form in the cavity of the membrane. This type of pathology is dangerous, since cells produced by excess hormones can degenerate into malignant ones.
- Basal hyperplasia. During menopause, this form of the disease is rarely diagnosed. During its development, an increase in the thickness of the basal layer of the uterus is observed.
- Focal form. The thickness of the membrane increases unevenly, forming growths (polyps) on the walls of the uterus.
- Atypical hyperplasia. During menopause, this type of pathology is rare. It is the most dangerous of all types of manifestations of the disease, as it quickly turns into uterine cancer. If an atypical form of endometrial hyperplasia is confirmed, doctors remove the organ.
Most often, glandular and cystic forms of the disease are diagnosed during menopause. The main reasons for the development of these types of pathology is hormonal imbalance.
Does the disease go away on its own during menopause?
Many women mistakenly believe that the disease can go away on its own without proper treatment. This position leads to aggravation of the condition. The process of proliferation of endometrial tissue will not be stopped and may subsequently degenerate into a malignant neoplasm.
The disease does not always go away completely even after drug treatment; surgical intervention is required, and without the necessary therapy, the pathology will cause an exacerbation of other problems and a general deterioration in the body’s condition. Frequent bleeding will cause severe anemia.
Causes of hyperplasia during menopause
There are several factors that cause endometrial hyperplasia to develop during menopause. In most cases, they begin to form even before the onset of menopause (premenopause).
- Hormonal disbalance. This is the most common cause of the development of pathology. In women over 45 years of age, there is a decrease in progesterone production and increased estrogen levels. This imbalance provokes modification of the lining of the uterus.
- Metabolic disease. With age, most women develop the problem of excess weight. Fatty layers of tissue provoke the production of estrogen, thereby exacerbating the hormonal imbalance that manifests itself during menopause.
- Failure of the endocrine system. For this reason, endometrial hyperplasia is often observed in postmenopausal women.
- Frequent invasions of the uterine cavity (gynecological operations). Due to frequent mechanical stress, the membrane receptors stop responding to progesterone levels. The more abortions and curettages a woman had to endure, the higher the likelihood of developing GGE in the climatic period.
- Predisposition to pathology at the genetic level. Doctors confirm that this disease is more often diagnosed in patients whose relatives have encountered the same problem.
Also, proliferation of mucous membranes is observed against the background of fibroids and mastopathy. In some cases, pathology can be caused by a malfunction of the immune system.
Endometrial hyperplasia
Menopause mainly affects menstrual function. In premenopause, irregular menstruation occurs:
- lengthening or shortening the cycle;
- acyclic bleeding;
- profuse bleeding.
In menopause and postmenopause, menstruation is normally absent. The appearance of bloody discharge, even in small quantities, indicates pathology. In such cases, diagnosis and treatment are needed.
It is known that estrogens have a significant effect on the condition of the endometrium, or the inner layer of the uterus. With estrogen deficiency, excessive growth of the inner layer of the uterus of a pathological nature, which is called hyperplasia, can be observed. This pathology can lead to the formation of polyps. In the case of malignancy of individual hyperplastic areas of the endometrium, a malignant tumor may develop.
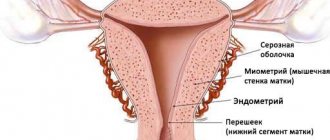
The endometrium is the inner layer of the uterus, which has two components:
- functional;
- basal.
The endometrium ensures the implantation and growth of the fertilized egg inside the uterus. In the first phase of the cycle, the functional layer of the endometrium grows, preparing for the implantation of a fertilized egg. Its thickness after menstruation is 1 mm. The growth of the inner layer of the uterus to 5-8 mm is ensured by the dominant sex hormones of the first phase of the cycle. In the absence of conception and pregnancy, the functional layer is rejected at the end of the cycle due to the dominant hormones of the second phase. The basal layer, being stable, thanks to its cellular reserves ensures the restoration of the inner layer of the uterus.
During menopause, the functional layer undergoes atrophy due to hormonal changes. By postmenopause, the upper functional layer practically disappears.
Hormonal fluctuations begin long before menopause and postmenopause. Often, endometrial hyperplasia develops in premenopause, which leads to its diagnosis at a later period. In addition, with a deficiency of estrogen, as with their excess, hyperplastic processes can also be observed.
Signs
Symptoms of endometrial hyperplasia in postmenopause manifest themselves individually. The main sign of a hyperplastic pathological process is bleeding. But they are not observed in all patients. Sometimes thickening of the membrane occurs without discharge. Other manifestations of the disease include:
- Very painful menstruation. In this case, the pain is spastic in nature.
- Irregular menstrual cycle. Sometimes spotting appears twice in a month.
- Heavy and prolonged periods (10-14 days).
Sometimes symptoms of uterine endometrial hyperplasia are accompanied by general malaise, insomnia, migraine, decreased performance, and irritability. The woman feels very thirsty.
Symptoms of the disease
The main sign of endometrial hyperplasia is the presence of interruptions in the menstrual cycle. A girl may complain of unusual discharge before or after menstruation, or of discharge in large volumes during menstruation. Also during this period you may be concerned about:
- pain in the abdomen,
- weakness,
- temperature increase,
- stomach upsets,
- general malaise,
- headaches, etc.
Sometimes endometrial hyperplasia occurs without symptoms, but a woman cannot become pregnant for a long time. Therefore, if, in the absence of complaints and regular sexual activity, pregnancy does not occur for a year, you should seriously think about it and be thoroughly examined by highly qualified specialists.
How to diagnose
In most cases, suspicion of endometrial hyperplasia is diagnosed by a gynecologist, to whom a woman approaches with complaints of painful or irregular menstruation. There are several methods for diagnosing the disease:
- Ultrasound. If during this diagnostic study it is discovered that the thickness of the endometrial layer is 7-8 mm, the gynecologist will prescribe an additional examination.
- Hysteroscopy. During the procedure, the doctor makes a visual examination of the uterine cavity using endoscopic equipment. The examination is carried out under general anesthesia. In most cases, a tissue biopsy is performed simultaneously with the examination of the membrane.
- Curettage (diagnostic curettage of the endometrium). The procedure is prescribed in cases where the thickness of the growing tissue exceeds 8 mm. Curettage is performed to further examine the endometrium and exclude the appearance of cancer cells.
If the thickening exceeds 10 mm, gynecologists recommend undergoing a separate curettage procedure, followed by irradiation of the organ cavity with radioactive phosphorus. The reagent is injected into the patient’s vein, migrates throughout the body and accumulates in pathogenic areas of the membrane. The doctor takes biological material from these areas for histological examination.
Diagnostics
The diagnosis is established after examining a patient who is in menopause and postmenopause. The gynecologist carefully examines the patient’s complaints, which may suggest the presence of endometrial hyperplasia of the uterus.
The examination includes several basic diagnostic methods.
- Ultrasound. This is one of the most informative and simple research methods, which allows you to measure the thickness of the endometrium of the uterus and determine the proliferation of tissue.
- Hysteroscopy. The manipulation is performed using a hysteroscope and is a diagnostic and treatment method. Thanks to the built-in video camera, the doctor can examine the uterine cavity in detail. When using the tool, it is possible to remove polyps and collect material for subsequent biopsy. This analysis is necessary to determine the histological type of hyperplasia and exclude a malignant process. In general, hysteroscopy is indicated if the thickness of the endometrium of the uterus at menopause is 6 mm.
- Diagnostic curettage. This procedure is also performed for diagnostic and therapeutic purposes. Curettage is often used to stop uterine bleeding. Curettage of the uterus is indicated for endometrial thickness of 8 mm in menopause.
If the thickness of the endometrium of the uterus in menopause is 10 mm, it is necessary to carry out RDV and study the cavity using radioactive phosphorus.
Drug treatment
It is recommended to treat endometrial hyperplasia with medications if the tissue thickness does not exceed 6-7 mm. Therapy is based on taking hormonal medications that provoke an increase in progesterone levels. The patient must undergo a routine ultrasound throughout the entire treatment period (6-8 months of constant medication use), during which the doctor constantly monitors changes in tissue growth indicators.
Drug treatment does not give 100% results. The likelihood of relapse of the disease on hormonal drugs is high.
Treatment
The appropriate treatment option for HPE is determined by:
- type of illness;
- woman's age;
- existing symptomatic manifestations;
- the presence of concomitant pathologies.
Taking into account all these parameters, the patient is prescribed the necessary drug therapy or surgical intervention.
Medication
A conservative method of treating hyperplastic growth of the endometrium, i.e. treatment of endometrial hyperplasia without curettage, involves the use of hormonal drugs. The most commonly used are progestins, gestagens and other products containing progesterone (Depo-Provera, Megestrol acetate, Levonorgestrel). In most cases, six-month treatment with these medications allows for complete relief from the pathology.
Surgical
If drug therapy does not produce the expected results, surgical treatment of the pathology is performed. Depending on the results of preliminary tests, one of the surgical intervention methods is used:
- Curettage of the uterine cavity. Recommended if the thickness of the modified tissue exceeds 10 mm. The procedure lasts 30-40 minutes under local anesthesia.
- Cauterization. This method of surgical intervention is used for focal hyperplasia. During the procedure, the doctor acts on the foci of modified tissue with cold, laser or electrical impulses.
- If there is an increased risk of developing malignant tumors, doctors recommend removing the uterus. During the hysterectomy procedure, the organ is completely removed. And if a woman’s ovaries are damaged during menopause, they are also removed during surgery.
Which type of surgical intervention to use is determined by the attending physician individually. Hormone therapy is sometimes used in preparation for surgery. It promotes rapid recovery of the body after intervention.
Clinical and histological diagnosis
An increase in the volume of the uterine lining during menopause requires special diagnostics. The basic study that allows one to suspect pathology is ultrasound. This method is not suitable for accurate diagnosis and can only determine that the thickness of the shell is greater than normal. Also, during an ultrasound, the localization of tumors can be determined. If the results of this study show that the mucosa is thicker than 5 mm, the patient is assigned a histological diagnosis according to the following criteria:
- Thickness up to 7 mm. Observation by specialists for 3-6 months is recommended.
- Thickness 8 mm. Diagnostic curettage is recommended.
- Increase in endometrial thickness to 10 mm or more. Separate curettage of the cavity and cervix with histological analysis of the materials is prescribed.
Additional examinations may include the following procedures:
- Biopsy.
- Targeted biopsy.
- Diagnostic curettage followed by analysis.
- Echosalpingography.
Important! In old age, the symptoms of gynecological and oncological diseases may be similar, and therefore examination of the affected tissues for cancer elements is mandatory!
Drug and surgical treatment
Excessive new formation of uterine mucus is a disease that requires mandatory and prompt treatment. Therapy should be chosen by the attending physician, based on the results of the studies. Pathology can be treated with both medication and surgical methods.
Drug hormone therapy
Drug therapy is justified in the early stages of the disease, when histological analysis of tissues does not reveal degenerated cells. To normalize the patient's condition, hormone therapy based on progesterone is performed. Taking the drugs can last up to 6 months with constant monitoring of the layer thickness. Treatment medications and their dosage should be prescribed only by the attending physician. Based on the results of regular ultrasounds, the dosage of the drug should be adjusted downwards. Also, drug therapy can be prescribed before and after surgery.
Important! After hormonal therapy, relapses of the disease are possible, so women are recommended to have control ultrasounds every 3-6 months!
Operative therapy
The operation is performed if the pathology has resumed after drug treatment, if polyps or degenerated cells are detected. Today, several types of surgical interventions can be used depending on the location and stage of the disease:
- Scraping. This procedure is used to remove overgrown tissue. The operation lasts no more than 30 minutes and is performed under local anesthesia. The purpose of the procedure is to get rid of excess mucus and prevent and stop bleeding.
- Cauterization. This operation is used for focal forms of the disease. Cold, electric current or laser are used to cauterize pathological areas. The choice of cauterization method remains with the specialist.
- Removal of an organ. Complete removal of the organ is carried out if degenerated cells are detected and there is a high risk of developing cancer. Surgery is also indicated for deep tissue damage. The operation may also remove the ovaries and tubes.
It is worth noting that endometrial hyperplasia in postmenopause is the most dangerous in terms of the occurrence of oncology. In this case, most often the woman’s reproductive organs are removed to avoid cancer.
Additional therapy with folk remedies
Most patients are in no hurry to use traditional treatment for pathology, preferring to use traditional medicine recipes. Gynecologists advise not to regard herbs as the main therapy, but to use them in combination with medications. The most common traditional medicine recipes that have proven effective in treating HPE are:
- Fresh juice from burdock root and golden mustache. These liquids are mixed in equal proportions and taken twice a day, 1 tablespoon. A significant drawback of this recipe is the possibility of carrying out therapy only in the warm season.
- Alcohol tincture of nettle (prepared independently). 200 gr. 500 ml of medicinal raw materials (fresh leaves and sprouts) is poured. alcohol (strong moonshine). Keep for three weeks in a warm, dark place, periodically shaking the container with liquid. The finished infusion is filtered and taken 1 teaspoon twice a day.
Treatment with folk remedies should be accompanied by regular examination by a doctor. This will make it possible to monitor the dynamics of the disease.
Disease prevention
With the onset of menopause, every woman should visit a gynecologist 1-2 times a year. Routine examinations will help doctors timely notice deviations and carry out corrective therapy. Also, women in old age should monitor their body weight; remember that excess weight causes an increased risk of illness. According to statistics, 40% of patients who seek help from gynecologists due to unknown bleeding are overweight.
In addition, preventive measures include avoiding uncontrolled use of drugs and herbal remedies containing phytoestrogens. Any pills, folk remedies, as well as herbs should be prescribed by a doctor based on blood tests for hormone levels. Self-medication only aggravates the situation and leads to deterioration of health.
Another preventative measure in old age is proper nutrition. You should exclude foods that are rich in estrogen from your diet, primarily beer and milk. Foods that are beneficial for women include tomatoes, pineapples, sea fish, lean meats, olive oil and red vegetables.
Every lady entering the difficult age of fading youth should understand that her future health depends only on her responsibility towards herself. Many ladies, having said goodbye to their periods, forget about visits to the gynecologist, which often results in the occurrence of dangerous conditions that require immediate professional help. Remember, a preventive examination is a necessity that saves you from serious operations.
Is relapse possible during menopause?
The possibility of recurrence of endometrial hyperplasia during menopause increases. Depending on the type of treatment chosen by the doctor, after which the tissue proliferation continued, further actions are determined:
- If the disease recurs after drug therapy, and the thickness of the layer increases by more than 8 mm, it is recommended to undergo a curettage procedure.
- If the situation repeats after curettage, the uterus is completely removed.
The percentage of recurrent cases of pathology with initially well-chosen treatment is low. To prevent the possibility of relapse, the patient must undergo regular follow-up examinations.
Possibility of relapse
The probability of relapse of pathology during menopause after drug treatment is quite high. In such a situation, the doctor may prescribe surgical intervention to prevent it from recurring in the future. The pathology recurs after conservative treatment if there are atypical cells. The specialist prescribes a repeated comprehensive examination, after which he changes the treatment tactics.
If there are recurrent factors, the specialist prescribes surgery. This is the only option to protect a woman from the process of degeneration of healthy cells into malignant ones.
Reviews from women about manipulation
Despite the apparent traumatic nature of the method, curettage is one of the most effective methods of treatment. Reviews from patients speak about this:
Maria, 52 years old
Against the background of menopause, discharge with blood suddenly appeared, I had to go to the gynecologist. He sent me for an ultrasound and told me that I needed to go to bed for cleaning. It was scary, but everything went easily, then I was prescribed a course of hormones, and my condition stabilized.
Irina, 43 years old
My menopause was early and difficult, and then I started bleeding. I thought that the cycle had resumed, but after 2 weeks I began to faint and my husband called an ambulance. I had an ultrasound and was urgently sent for curettage followed by histology. Everything turned out to be fine, but now I’ve been taking pills for six months, so far so good.
Valentina, 51 years old
I went for cleaning more than once - there were reasons. And in menopause, I was diagnosed with hyperplasia and sent for curettage. The procedure is effective, although not very pleasant. But there was no discharge, and the histology was done - now I’m calm.
Preparing the patient
If cervical dilatation is not necessary, if a small-caliber endometrial sampling device is used, no formal preoperative preparation is required.
- It is advisable to come to the curettage procedure with an empty stomach, as manipulation of the cervix and curettage can cause nausea and vomiting.
- Patients should refrain from eating for 6-8 hours and drinking liquids 2 hours before the procedure if there is general anesthesia.
- It is advisable to take an analgesic with a small amount of water an hour before curettage, if there is no general anesthesia.
- According to modern recommendations, blood and urine tests are done at the request of the anesthesiologist.
- Prophylactic antibiotics are not required.
Traditional medicine
Folk remedies for hyperplasia are also used. Herbal medicine occupies first place in folk medicine. Burdock, nettle, hogweed, and plantain cope very well with this disease.
Women who have experienced the effects of “grandmother’s remedies” note that after folk healing they feel better, bleeding becomes less heavy, the menstrual cycle is restored, and pain during menstruation decreases.
In most cases, alcohol tinctures are used, which are very easy to prepare at home. The boron uterus is dried and placed in a glass jar, into which forty-proof alcohol, vodka or cognac 0.5 liters are poured. The tincture should be infused for two weeks, stored in a place where there is no light and shaken every day.
Take one teaspoon 2-3 times a day with a glass of water. The course of treatment lasts three months. According to reviews, patients note a good effect from douching with a decoction of this plant.
Burdock must be prepared in advance. It is collected in late autumn or early spring. To prepare the medicine, you need to squeeze the juice from fresh roots. Take two teaspoons in the morning and evening before meals. The course lasts six months.
Nettle is very famous for its hemostatic properties. To treat hyperplasia, you need to brew a decoction: pour two tablespoons of the plant with boiling water (1 cup) and cook for 15 minutes, adding water to the initial volume. Take ¼ cup of decoction 3-4 times a day.
In addition, you can use herbs that are antagonists of female hormones. These include fireweed, rapeseed and jarutka.
Women who have tried traditional medicine speak positively about their effect on the body. But, despite the positive reviews, you should not abandon traditional methods of treatment; therapy should be carried out comprehensively under the supervision of the attending physician.
The most positive reviews can be found about herbal decoctions and douching, for which boron uterus is used. Patients claim that the product is completely safe, highly effective, and does not cause side effects.
Features of curettage for hyperplasia
Women are always concerned about how this procedure occurs, what the consequences and risks are. Curettage is a surgical procedure that is performed in the operating room. In this case, the patient is in a comfortable position on the gynecological chair.
In most cases, the woman is given anesthesia. This is due to the fact that cleaning is a painful and unpleasant procedure. Anesthesia is not used only after childbirth or miscarriage, since the cervix is already quite dilated.
The gynecologist personally chooses which method to perform the operation - blind curettage or using a hysteroscope (this is a backlit video camera that also has a channel for supplying sterile air).
Blind scraping
After the anesthesia takes effect and the patient no longer feels the internal organs, the gynecologist begins the procedure. But, no cuts are made.
First, you need to widen the cervix to gain more space for surgical manipulation. To do this, a dilator is inserted into the vagina, the walls are spread apart and access to the cervix is gained.
Then, using special probes with different diameters, the cervix is gradually opened. When the desired result is achieved, the uterus is checked for curvature and length.
Next, using a curette (surgical spoon), they begin to scrape out the functional layer along the walls of the organ, paying special attention to the corners.
After cleaning, the vessels that bleed are cauterized, and the removed mucosa is sent for histological examination.
Endometrial scraping takes about 30 minutes. Then the patient is taken to the ward, where she is monitored by an anesthesiologist until she awakens and feels normal.
Curettage with hysteroscope
As with blind curettage, during the procedure the patient is on a gynecological chair in a medicated sleep. The gynecologist installs a dilator, inserts a hysteroscope, and with the help of air gradually expands the uterine cavity for work.
The curette is inserted into another channel of the device, and before removal, the condition, thickness, relief and color of the layer being removed is assessed.
After removal, it is placed in a container (one or several) and also sent for histological examination. A special instrument is inserted into the hysteroscope, which is used to cauterize the vessels to stop bleeding. The operation is considered completed.
Separate curettage
There is also such a thing as separate curettage. In other words, this is diagnostic curettage. Gynecologists use it in cases where it is necessary to find out the exact cause of pathological changes or complaints (irregular, prolonged periods, bleeding during menopause, suspected infertility).
The procedure is carried out similarly to the above schemes with full preoperative preparation.
Important! Diagnostic curettage is performed only in a hospital! Like any surgical intervention, the procedure has a number of contraindications:
- relapse of infectious, bacterial or viral diseases (chlamydia, gonorrhea);
- acute foci of inflammatory nature in the pelvic organs;
- exacerbation of chronic heart, kidney or liver diseases.
Complications and outcomes of proliferation of the uterine mucosa
The fundamental complication of the growth of the inner lining of the uterus is bleeding, the occurrence of which in menopause indicates precisely the designated pathological change.
Bleeding is not associated with critical days, and is characterized by copious bleeding and severe pain. Hyperplasia is most dangerous during menopause; at this age, women have prerequisites for the development of malignant tumor formations, which can also affect the mammary glands.
The situation worsens when diagnosing hyperplasia of the mucous membrane with the presence of atypical cells, that is, cells that have undergone modifications and no longer look like normal cells of this tissue. Based on these changes, one can immediately judge that the process will turn into cancer.
Other complications and outcomes of the disease may also occur. The patient may experience relapses of the pathological condition, the problem of infertility may arise, another manifestation of endometrial hyperplasia is anemia, which becomes chronic. These consequences can be avoided if you start treatment and consult a doctor for any deviations during menopause, rather than hope that everything will return to normal.
Hysteroscopy
If, as a result of curettage, material is obtained that histologists call “non-diagnostic”:
- not enough material;
- the picture is not clear during the study,
then there may be a need for hysteroscopy with targeted biopsy. The good thing about this method is that the doctor sees a “suspicious area of the endometrium” and takes a sample from it.
Hysteroscopy is of particular value in women with suspected malignant process, especially if the results of transvaginal ultrasound are non-diagnostic or the thickness of the endometrium according to ultrasound exceeds 5 mm.
Blind methods of endometrial sampling - biopsy and curettage often cannot 100% identify pathology in the endometrium.
- Blind sampling, either by endometrial biopsy or curettage, is a satisfactory method, the first diagnostic procedure for detecting uterine cancer that affects the entire surface of the endometrium.
- But they are inadequate for localized processes such as endometrial polyps, which can be malignant.
This information assumes that:
- in the presence of symptoms or signs of focal uterine lesions on ultrasound or after blind sampling;
- if postmenopausal bleeding symptoms persist,
It is imperative to visualize the endometrial cavity. For this purpose, contrast ultrasound or hysteroscopy is used.