Salpingitis and oophoritis: what is it?
Salpingitis and oophoritis are inflammatory diseases. They often occur in the same context, since in most cases they appear against the background of each other.
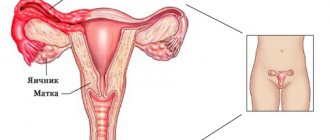
Salpingitis is an inflammation of the fallopian tubes. Oophoritis is inflammation of the ovary. Often the disease begins with one pathology, and after a while another appears. Therefore, in medicine there is a separate diagnosis “adnexitis”, which indicates inflammation of the oviducts and ovaries at the same time.
Salpingitis and oophoritis are usually detected in women of childbearing age and often result from unprotected sexual intercourse. Therefore, the main method of prevention is sexual education of girls at the stage of puberty.
Salpingitis has different forms of progression and is classified according to several indicators. The treatment method and prognosis of the disease depend on this. The main danger of the pathology is that over time, inflammation of the fallopian tubes leads to the development of adhesive disease with all the ensuing consequences. Patients after prolonged salpingitis often remain infertile, suffer from chronic pain in the pelvis and experience relapses of the inflammatory process.
https://youtu.be/stVMtwF8ceM
Pregnancy
Unfortunately, this disease practically eliminates the possibility of getting pregnant. However, if you have the above symptoms, this does not mean that you have oophoritis. Therefore, you should immediately consult a doctor.
During the development of this pathology, the fallopian tubes and ovaries irreversibly change, which makes the process of bearing a fetus very problematic. If, of course, you manage to get pregnant at all.
It is still possible to become pregnant in the chronic form or with right-sided oophoritis if you undergo a special course of treatment from a specialist before conception.
It is worth remembering that with this disease complications during pregnancy are possible:
- fetal infection;
- risk of miscarriage.
Therefore, before becoming pregnant, you should get advice from your doctor. Treatment of oophoritis should only be carried out by a highly qualified specialist.
Classification
Salpingitis and oophoritis are divided into left-sided, right-sided or bilateral . In other words, the inflammatory process develops in the appendages on the left, right or both sides. There are rare cases where left-sided oophoritis and right-sided salpingitis are detected, or vice versa.
According to the nature of the flow, they are distinguished:
- Acute salpingitis. The disease is characterized by an abrupt onset with a pronounced clinical picture. With the right treatment regimen, the prognosis is favorable. Acute salpingitis usually lasts no more than one week and ends with complete recovery without adverse consequences.
- Chronic salpingitis. Pathology becomes the result of an untreated acute form or develops due to an incorrectly chosen therapeutic regimen. Chronic salpingitis has a long course (more than 3 weeks) and practically does not manifest itself. The disease has relapses and often leads to complications.
Depending on the causative agent of the inflammatory process, acute salpingitis has the following forms:
- Non-specific. The cause of the pathology is microorganisms that are normally present in a woman’s body. They are part of the intimate microflora, but should not be in the fallopian tubes and ovaries. For some reason, they penetrate the appendages and provoke inflammation.
- Specific. The disease develops as a result of infections caused by pathogenic microorganisms. They can enter a woman’s body during sexual intercourse, as well as become the result of diseases of other organs and penetrate the appendages through the blood or lymph flow.
Types and signs of oophoritis
In clinical practice, acute, subacute and chronic oophoritis are distinguished; the process can be unilateral or bilateral.
Acute oophoritis begins suddenly, with sharp pain in the lower abdomen, which can radiate to the groin and lumbosacral region. Urination becomes difficult, sometimes painful, and purulent discharge from the vagina appears. Signs of oophoritis are accompanied by a general deterioration of the condition: high temperature, fever, headaches and muscle-joint pain.
Chronic oophoritis often has a hidden onset, that is, it can be primary chronic, or develop as a result of untreated acute oophoritis. The only sign of chronic oophoritis for a long time is unexpressed pain. The pain, as a rule, is not constant, is dull, aching in nature, and appears during overwork, hypothermia, stress, or during sexual intercourse. Most often, such signs of oophoritis in its chronic form appear on the eve of menstruation. Another sign of oophoritis in an advanced chronic form is menstrual irregularities due to impaired estrogen production by the affected ovary.
In some cases, chronic oophoritis is so subtle that it is detected only during examination for menstrual irregularities or infertility.
Causes of the disease
Salpingitis in 70% of cases is caused by an association of microorganisms. They can be either specific or nonspecific. Less commonly, inflammation of the appendages is caused by a single agent.
Salpingitis is caused by:
- streptococci;
- enterococci;
- chlamydia;
- gardnerella;
- E. coli and others.
It is impossible to say for sure why the pathogens of the inflammatory process penetrated the fallopian tubes and ovaries. Most often, salpingitis and oophoritis lead to:
- frequent change of sexual partners;
- refusal to use barrier contraceptives;
- failure to maintain intimate hygiene;
- practice of non-traditional methods of sexual intercourse;
- instrumental interventions in the functioning of the genital organs;
- installation of an intrauterine contraceptive device;
- childbirth;
- carrying out gynecological manipulations without observing the rules of asepsis.
The risk of salpingitis increases in patients with reduced immunity. Frequent colds, taking certain medications, bad habits, and unhealthy diet lead to suppression of the body's resistance.
Subtypes
In modern medicine, the following subtypes of the disease are distinguished:
- bilateral oophoritis;
- right-sided oophoritis;
- left-sided oophoritis.
Bilateral oophoritis
Bilateral oophoritis is inflammation in both ovaries. The signs of oophoritis with this subtype of the disease correspond to the points described above.
On palpation, pain in the lower abdomen and significant compaction in the ovarian area may be felt. To make an accurate diagnosis, several instrumental and laboratory studies should be performed. Symptoms of bilateral oophoritis are similar to appendicitis and salpingitis.
Left-sided oophoritis
Left-sided oophoritis is the formation of an inflammatory pathological process in the left fallopian tube and ovary. The symptoms are the same as described above. The only difference is that with left-sided oophoritis the pain is localized on the left, in the lower abdomen.
Right-sided oophoritis
Almost the same symptoms are diagnosed with right-sided oophoritis. The pain is localized on the right side, also in the lower abdomen. Diagnosis is exactly the same as for other forms of the disease.
Symptoms of salpingitis and oophoritis in women
Inflammation of the appendages in a woman begins with a pronounced clinical picture. Acute salpingitis develops over 5-7 days and, if left untreated, becomes chronic. In the initial stages, the disease seriously worsens the patient’s well-being and forces her to seek medical help.
If a woman ignores severe symptoms or tries to cope with them at home, then by the second week chronic salpingitis occurs. In this case, the severity of the symptoms decreases, the disturbing signs disappear and only mild discomfort remains.
Characteristic symptoms of salpingitis and oophoritis:
- shooting pain on the left or right in the lower abdomen (depending on the location of the disease);
- discomfort during sexual intercourse and gynecological examination;
- increased body temperature;
- discharge from the genital tract (abundant, foamy, with an unpleasant odor, colored).
Inflammation of the appendages can lead to menstrual irregularities and heavy bleeding. Over time, adhesive disease develops, which leads to obstruction of the fallopian tubes, anovulatory cycles and other problems, culminating in infertility.
Oophoritis
The name of this pathology comes from the Latin word oophoron, meaning “ovary”. Oophoritis
is an inflammatory process in this paired female organ. Inflammation can affect either one ovary or both. In the first case they speak of unilateral oophoritis, in the second there is a bilateral type.
As a rule, the pathological process also covers the fallopian tubes. In fact, it is in them that most often it begins to develop, after which the infection enters the ovaries. In this case, salpingoophoritis or adnexitis occurs.
Classification of oophoritis
By nature, oophoritis can be specific and nonspecific.
- A specific variety develops when the disease is provoked by pathogens of chlamydia, trichomoniasis, mycoplasmosis, and tuberculosis.
- The nonspecific form occurs when inflammation occurs under the influence of opportunistic microflora: staphylococci, streptococci, Escherichia coli, candida.
The infection enters the ovaries from the uterus, cervical canal, and fallopian tubes. In rare cases, microorganisms penetrate the ovaries through lymphatic and blood vessels.
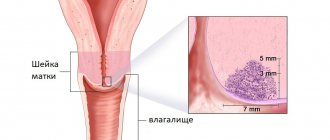
In case of infection from the uterine cavity, the inflammation gradually covers the fallopian tubes, moving from the mucous membrane to the muscular, and then the serous layer.
As a result, the wall of the fallopian tubes lengthens and thickens, pus begins to be released, and adhesions subsequently form. The inflammation spreads to the ovaries, the tissues of which begin to melt under the influence of pus penetrating into them.
The fallopian tube and ovaries are welded together. For this reason, it is impossible to separate the symptoms of salpingitis (inflammation of the fallopian tubes) and oophoritis.
In some cases, inflammation can also affect the surrounding peritoneum, and periadnexitis develops.
The accumulated exudate can be clear or purulent. In the first case, it forms a hydrosalpinx, in the second, a pyosalpinx. Due to the accumulation of purulent discharge in the ovaries, pyovar is formed - purulent extensive melting of ovarian tissue. Further spread of the infection leads to its spread beyond the ovary. Pelvioperitonitis develops.
Forms and symptoms of the disease
Pathology can occur in three forms:
- acute;
- subacute;
- chronic.
The clinical picture of each of them has its own specifics.
In the acute form, the following symptoms are observed:
- general malaise;
- feverish condition;
- increased body temperature;
- constant severe pain of high intensity;
- depending on the prevalence of inflammation, they can be localized on one side or be bilateral, radiating to the lumbar region, sacrum;
- frequent painful urination (accompanied by pain);
- acute pain during sexual intercourse;
- presence of intermenstrual bleeding;
- There may be abundant purulent and serous discharge from the genitals;
- Disturbances in the functioning of the gastrointestinal tract are also possible.
A gynecological examination reveals an increase in the size of the ovaries and their soreness. The acute form of the disease requires hospitalization and subsequent hospital treatment.
Subacute variety
Oophoritis is relatively uncommon. It develops when the inflammatory process is provoked by tuberculosis or mycotic infection. Symptoms are similar to those of the acute form, but are less pronounced.
Correct treatment started in a timely manner leads to complete recovery. Otherwise, the disease may become chronic.
, which is characterized by a long course, periods of exacerbations and remissions.
In the acute phase, the clinical picture is as follows:
- dull aching pain in the lower abdomen, in the vagina, in the groin area, intensifying against the background of hypothermia, before menstruation, during colds;
- disruption of the regularity of the menstrual cycle due to disruption of normal ovarian activity;
- constant scanty discharge (leucorrhoea);
- pain during sexual intercourse;
- decreased libido;
- inability to get pregnant.
A gynecological examination reveals:
- increased sensitivity of the ovaries;
- pain on palpation;
- swelling.
The changes also affect the psycho-emotional sphere. Patients experience:
- increased irritability;
- sleep disorders;
- decreased physical and mental performance;
- increased fatigue.
In some cases, chronic oophoritis occurs without exacerbations. A similar scenario is possible, for example, with gonorrheal inflammation of the ovaries, which is characterized by an asymptomatic course, which over time leads to the development of obstruction of the fallopian tubes, the formation of adhesions around the ovaries and secondary functional infertility.
Depending on the prevalence of the inflammatory process, oophoritis is divided into unilateral (left- or right-sided) and bilateral.
A unilateral variety is said to occur when one ovary is affected. Most often it develops due to the presence of infectious diseases of the genital organs, gynecological operations or other procedures, stress, hypothermia, and against the background of weak immunity.
Basically, the symptoms of the disease are as follows:
- increased fatigue;
- increased body temperature;
- the high temperature cannot be brought down with the help of antipyretics;
- pale skin;
- pain in the lower abdomen (localized on the affected side);
- bleeding between periods;
- vaginal discharge;
- irritability;
- decreased sex drive.
When the right ovary is affected, the symptoms often resemble appendicitis. For this reason, a careful differential diagnosis is required.
Often inflammation from one ovary spreads to the second. , bilateral oophoritis develops
. The clinical picture is as follows:
- intense pain in the lower abdomen, groin area, often radiating to the lower back;
- intermenstrual uterine bleeding;
- painful urination;
- constant nervous tension;
- sleep disturbance;
- vaginal discharge.
Depending on the form of the course, bilateral oophoritis is divided into:
- acute bilateral;
- chronic bilateral.
In an acute bilateral process, the following are observed:
- temperature fluctuations;
- vaginal discharge;
- acute pain in the groin area, lower abdomen, lower back;
- uterine bleeding;
- pain when urinating;
- disturbances of the monthly cycle.
In chronic bilateral oophoritis, the symptoms are similar to those described above, but are less severe. Moreover, this form of pathology poses the greatest danger, since it can cause ovarian dysfunction and subsequent infertility.
Treatment of oophoritis
The course of treatment is prescribed depending on the causes of inflammation and the specific form of the pathology.
Acute oophoritis is treated in a hospital setting. Patients are prescribed:
- compliance with bed rest;
- applying ice to the lower abdomen;
- taking antibiotics;
- painkillers;
- sulfonamides and other antibacterial drugs;
- desensitizing medications that have a suppressive effect on inflammatory mediators;
- sleeping pills;
- vitamin complexes;
- UV irradiation.
If there is exudate in the pelvis, fallopian tubes, as well as the formation of purulent tumors, a puncture is prescribed. It is carried out through the posterior vaginal fornix. After suctioning out the contents, antibiotics and alpha-chymotrypsin are injected into the site of inflammation. The procedure is carried out approximately 3-4 times.
In order to increase the body's reactivity, the following is prescribed:
- aloe injections;
- autohemotherapy (every other day);
- FIBS;
- taking multivitamin medications.
If necessary, detoxification therapy can also be used.
Inpatient treatment is also indicated for subacute types of the disease. It is carried out until the inflammatory process and infiltrates are completely eliminated.
In the chronic course of oophoritis, emphasis is placed on the use of physiotherapeutic procedures. When prescribing them, they are guided by the characteristics of the clinical manifestations of the disease.
1. If exacerbation of chronic inflammation predominates, SCV or DCV therapy is used, as well as magnetotherapy with an alternating low-frequency magnetic field. If the exudation is insignificant, UHF or HF therapy is prescribed.
2. If the pain syndrome predominates, it is advisable to use:
- low frequency pulse currents;
- electrophoresis of salicylic acid and amidopyrine;
- UV irradiation.
3. If adhesive changes predominate, apply:
- exposure to ultrasound in pulsed (intermittent) radiation mode;
- inductothermoelectrophoresis;
- inductotherapy;
- medicinal electrophoresis.
To consolidate the results, patients are recommended to undergo sanatorium-resort treatment.
Diagnosis of inflammation of the appendages in women
Salpingitis is quite easy to diagnose. The gynecologist may suspect inflammation of the appendages during the initial appointment, when he hears about the symptoms from the patient. An ultrasound is prescribed to confirm the diagnosis. Normally, the fallopian tubes are so large that they cannot be seen on an ultrasound. If the oviducts are visualized during the scan, then we are talking about inflammation. Sometimes a concomitant disease is hydrosalpinx, in which fluid accumulates in the pipe.
Inflammation of the ovaries is also determined during ultrasound. Oophoritis is characterized by an increase in the diameter of the female reproductive glands. To determine the cause of the disease, a woman is prescribed a laboratory blood test and vaginal smears.
, it is important to perform an antibiotic sensitivity test to determine the causes of inflammation . Only in this case can effective treatment be prescribed.
Treatment
The course of treatment directly depends on the reasons that provoked the progression of the disease in the ovaries and fallopian tubes.
Treatment of oophoritis is carried out only in a hospital setting.
The course of treatment is prescribed after determining the exact cause of the disease and carrying out diagnostics. Painkillers and antibiotics must be prescribed. At the initial stage, if there are no contraindications, ice can be applied to the lower abdomen to reduce pain.
If an acute stage of the disease is diagnosed, then, in addition to medications, a course of physiotherapeutic procedures is prescribed. If the adhesive process has not yet begun, absorbable drugs and the following procedures are prescribed:
- gynecological massage;
- mud therapy.
Gynecological massage
If taking antibiotics and other medications does not produce results, then surgical intervention is possible - complete removal of the ovaries (such treatment is radical).
Self-medication in this case is unacceptable, since the disease can not only go into a chronic stage, but also cause the development of a serious complication - infertility. Folk remedies can only be used in tandem with synthetic medications and only with the permission of the attending physician.
Chronic and acute salpingitis: treatment
Acute salpingitis is treated with antibiotics and antiprotozoal agents. It is important to identify the disease in a woman at the initial stages so that it does not become chronic. Acute salpingitis, with the correct treatment method, can be easily corrected and ends with recovery after 7-14 days of therapy. Chronic salpingitis requires more serious treatment, which is not always effective.
To treat inflammation of the appendages in women, a pathogen sensitivity test is performed. Drugs that are effective in a particular case are prescribed. An individual list of medications is selected for each patient. Broad-spectrum antibiotics for oral and injection use are usually used, as well as topical suppositories with antiseptic and antibacterial effects. In addition, when using antibiotics, antifungal agents are prescribed.
For the treatment of chronic salpingitis, in addition to antibiotics, auxiliary drugs are selected. The use of proteolytic drugs, painkillers, anti-inflammatory and antispasmodics is recommended.
In the acute period, the patient is prescribed symptomatic medications that alleviate general well-being. They are selected according to symptoms. After treatment, especially for chronic salpingitis, physiotherapy is recommended to prevent adhesive disease, for example, in the gynecological department of the LC on Timur Frunze.
Inflammation of the ovaries in women - symptoms and treatment
The specialist prescribes a course of therapy for the patient, focusing on the symptoms of the disease and data obtained during laboratory tests. The disease in the acute stage is subject to treatment in a hospital setting with a prescription for bed rest. In the first few days, painkillers, antibiotics, and also restoratives are used. After relief of the acute condition, the course is supplemented with various physiotherapeutic procedures.
Treatment of chronic ovarian inflammation comes down to properly selected antibacterial therapy. The specialist must determine how sensitive the pathogen is to certain medications. This will allow the doctor to prescribe the dosage of the drug and the duration of the course of taking it. Suppositories can be used to treat inflammation of the ovaries
(as an aid to relieve symptoms of the disease).
The best way to prevent the disease is to strengthen the body’s overall immunity. Women suffering from immune system disorders are advised to spend more time in the fresh air, lead an active lifestyle if possible, and take vitamins. A balanced diet should contain a significant amount of vegetables, fruits and dairy products.
Prevention of inflammation of the appendages
Prevention of salpingitis and oophoritis should be carried out throughout life. Even before puberty, it is important to organize sex education for the girl, teach her personal hygiene and other natural rules of protection against genital tract infections.
To reduce the risk of salpingitis, it is recommended:
- do not start sexual activity early;
- use barrier contraceptives with new partners;
- have unprotected sexual contact only with a trusted man;
- take a responsible approach to any gynecological manipulations and carry them out only in certified medical institutions, which include the GMS clinic;
- lead a healthy lifestyle;
- Visit a gynecologist regularly and get tested even if there are no complaints.
Symptoms of the disease
For oophoritis, all symptoms of inflammation are typical, but the severity of the manifestations depends on the variant of the disease, the type of microbes and immune defense.
The worst thing for a woman is acute gonorrheal salpingoophoritis, in which the symptoms are more pronounced and the risk of dangerous complications is highest.
Chlamydia creates conditions for chronic inflammation, forming in the future an adhesive process in the area of the uterine appendages and tubal infertility.
With oophoritis, the following symptoms are distinguished:
Pain
Pain in the abdomen, depending on the type of inflammation, can manifest itself:
- sharp, strong and constant;
- pulling sensations in the lower abdomen;
- pressing and dull pain;
- periodic wave-like unpleasant sensations;
- minor pain associated with physical activity or sexual intercourse.
Vaginal discharge
The inflammatory process in the female genital organs is almost always accompanied by vaginal leucorrhoea, which can be as follows:
- profuse purulent with an unpleasant odor;
- thick milk;
- copious mucous-milk with itching;
- curdled;
- milk mixed with blood;
- bloody or bloody.
Temperature
In case of exacerbation or acute oophoritis, a temperature reaction will necessarily occur. The following options are possible:
- high body temperature reaching 39-40°C;
- spasmodic reaction with an evening sharp rise in temperature and night chills;
- slight increase to 37-38°C;
- normal body temperature;
- reduction to 36°C.
Menstrual irregularities
Changes in the menstrual cycle are associated with disruption of the ovulation process and hormonal imbalance caused by inflammation of the ovaries. There are the following problems with menstruation:
- delayed menstruation;
- untimely arrival of critical days;
- heavy periods;
- prolonged bleeding after normal menstruation;
- random bleeding.
Childbearing problems
Hormonal disorders in the ovaries and lack of ovulation against the background of oophoritis are the cause of infertility. With proper treatment of acute inflammation, endocrine function is normalized and the ability to conceive is restored.
With chronic variants of the disease, especially with frequent relapses, the risk of irreversible infertility increases sharply.
With combined damage to the ovary and fallopian tubes, impaired fertility is caused by tubal obstruction.
Causes of oophoritis
The main reason for the development of oophoritis is the presence of infection in the body, which enters the ovaries through the fallopian tubes, blood or lymph. Let's determine the main causes of ovarian inflammation and the characteristics of infection:
- Infections can enter the body not only sexually (through unprotected sexual intercourse), but also through household contact (through water or towels in common areas, saunas, swimming pools). The most common pathogens are chlamydia, urepasm, mycoplasma, gonococcus, streptococcus, trichomonas, and E. coli.
- Surgical interventions in the pelvic organs increase the chance of pathogenic organisms entering the ovaries through the uterus and fallopian tubes and causing their inflammation. In general, salpingitis and oophoritis are inextricably linked; very rarely there is inflammation of the tubes separately or the ovaries separately. As a rule, these diseases occur together, which is why in medicine they received the common name - salpingoophoritis (adnexitis).
- Intrauterine devices also increase the risk of oophoritis. When installing or removing the spiral, interference occurs in the mucous membranes of the uterus. Incorrect actions by a doctor can provoke the development of the disease.
- Hypothermia “hits” primarily the body’s immune barriers, as a result of which the bacteria living in it begin to actively multiply and cause inflammatory processes.
- Disruptions in the functioning of the endocrine system cause hormonal imbalances, which also causes disruption in the functioning of the immune system. Artificial termination of pregnancy (abortion) increases the risk of hormonal imbalance.
- Stress can cause exacerbation of chronic oophoritis. This happens because after strong emotional shocks, the immune defense weakens, pathogenic microflora receives a favorable environment for reproduction, and as a result, an inflammatory process in the ovaries.
In addition to the above reasons, there are additional risk factors that provoke inflammatory processes in the ovaries.
First of all, these include promiscuity with multiple sexual partners, neglect of barrier methods of contraception (condoms). All this increases the risk of infection.
Inflammatory processes in nearby organs can increase the risk of developing oophoritis. Thus, diseases of the urinary tract (cystitis, urethritis) are frequent companions of oophoritis.
Smoking, although not a direct cause of the disease, can have a negative impact on the overall health of the immune system. Nicotine, the harmful tars contained in cigarettes, literally “kill” the immune system.
How to treat oophoritis
When treating oophoritis, an integrated approach is important to prevent the disease from becoming chronic. Therefore, both drug therapy and traditional methods of treatment are used.
Drug therapy
Antibiotics are prescribed to treat inflammation of the ovaries. Preference is given to modern broad-spectrum drugs. Usually two groups of drugs are prescribed: macrolides and tetracyclines, or macrolides and penicillins.
In addition to antibacterial therapy, local drugs are used - intravaginal and rectal suppositories or tablets, which have antimicrobial and anti-inflammatory effects. For severe pain, analgesics can be used, but only in the first days of treatment.
Immunostimulants are often prescribed. It is especially important to use them in the chronic course of the inflammatory process in the ovaries.
At the end of treatment, if there are residual effects in the form of mild pain, you can give aloe injections. This drug has a resolving and anti-inflammatory effect.
When treating chronic forms of ovarian oophoritis, a course of drugs to resolve adhesions is required (for example, Longidaza suppositories).
In addition to medications, physiotherapy (electrophoresis, laser, UHF) has proven itself well. If possible, patients are recommended to undergo spa treatment in sanatoriums that specialize in the treatment and prevention of inflammatory diseases of the pelvic organs.
For greater effectiveness, sexual activity is not recommended during treatment. If a sexually transmitted infectious disease is diagnosed, treatment is necessary for both partners. In case of acute oophoritis, bed rest must be observed for at least 2 days.
Treatment with folk remedies
In addition to medications and physiotherapeutic procedures, oophoritis can be treated at home. Most often, plant-based infusions, teas and decoctions are prepared.
For example, to prepare an anti-inflammatory infusion for oral administration, you need to mix chamomile and linden. These herbs can be purchased at the pharmacy and are sold in convenient filter bags. Brew one sachet, let it brew for half an hour and take 100 ml twice a day. Nettle, mint, string, and hogweed have the same properties.
Douching has also worked well. To prepare a solution for douching you will need 20 grams. crushed oak bark and nettle leaves. Pour 200 ml of boiling water over the ingredients, let it brew, cool, strain and douche before going to bed. This product has an antiseptic effect.
These methods can be used as preventive measures, as well as in addition to drug treatment, but not independently. Before using them, you should definitely consult your doctor.
Diagnosis of the disease
A good prevention of complications is the timely detection of oophoritis, therefore the diagnosis of the disease should include the following studies:
- examination by a gynecologist;
- taking smears for sexually transmitted infections;
- bacterial cultures from the endocervix and vagina;
- general clinical tests to identify the severity of inflammation;
- assessment of hormonal problems based on hormone fluctuations in the blood;
- ultrasound scanning.
In most cases, this is enough to assess the situation in the woman’s reproductive system. According to indications, the doctor may refer you for a tomography (if a tubo-ovarian tumor or cystic formations in the ovary are suspected). In difficult cases, diagnostic laparoscopic surgery will be required.