Women often have to think about how to treat chronic vaginitis. According to statistics, at least a third of the fair sex faces this pathology. Without having pronounced symptoms, the disease may not cause alarm, and its manifestations are perceived as a minor problem, which is quite easy to get rid of. As a result, a disease that is not diagnosed and treated in a timely manner becomes chronic and can lead to serious complications.
Types and forms of the disease
Chronic forms of any disease are characterized by a long course with long remissions, when there are no obvious manifestations of the pathological process. Chronic vaginitis can exist in the female body for years, while infectious pathogens are inactive. However, under certain circumstances and under the influence of provoking factors, the formation of an acute or subacute process begins. At the same time, the general condition of the victims shows virtually no changes, which does not guarantee dangerous consequences in the form of infertility. The inability to conceive is explained by the spread of infection from the vaginal environment in an ascending manner.
Most often, trichomonas and candidal vaginitis are diagnosed, which are divided into infectious or non-infectious types. The formation of the former is provoked by pathogenic and conditionally pathogenic microorganisms. At the same time, opportunistic pathogens are a natural component of the vaginal microflora, provoking inflammatory processes only in the event of a change in the acidity of the environment. Pathogenic microflora can be specific or nonspecific. The list of specific pathogens includes:
- gonorrheal bacillus;
- ureaplasma and mycoplasma;
- Trichomonas;
- chlamydia.
However, it is nonspecific pathogens, which include staphylococci and streptococci, herpes and E. coli, and Candida fungi that cause the appearance of a chronic form of vaginitis. The bacterial form of pathology is considered separately, since, being a type of infectious disease, it does not demonstrate the presence of a pathogen, although when considering the composition of the flora, an increased number of opportunistic microorganisms is found.
Also, the forms of colpitis are determined in accordance with the duration of the pathology. In acute vaginitis, pathological processes are observed for up to two months. In the subacute form, the inflammation does not go away for more than two and no more than six months. They speak of chronic colpitis if the disease lasts for more than six months and develops in waves, when periods of remission alternate with exacerbations.
The nature of the inflammatory process also matters; chronic vaginitis can be serous, with the discharge having a clear color and liquid consistency. In the mucous form, the leucorrhoea is cloudy, thick and viscous, and the color of the secretion is whitish. Purulent colpitis is accompanied by an unpleasant-smelling, opaque, thick discharge of a yellowish or greenish color.
https://youtu.be/5METOIxto4w
https://youtu.be/6Hy4Zf_Goaw
Nonspecific vaginitis
In the group of vaginitis, it is customary to distinguish so-called nonspecific (or bacterial) vaginitis. They do not have a specific pathogen and are caused by opportunistic microorganisms: Escherichia coli, streptococci, staphylococci and other microbes present in the vagina.
With nonspecific vaginitis, the infection does not enter the vagina from the outside, but develops due to a small number of microorganisms present in the normal microflora. When, under the influence of provoking factors, the number of lactobacilli in the vagina begins to decrease, favorable conditions appear for the increased proliferation of unwanted microflora. When the number of pathogenic microorganisms becomes significant and begins to exceed the number of lactobacilli, local infectious inflammation develops. Thus, opportunistic microflora becomes pathogenic and causes symptoms of nonspecific vaginitis.
Nonspecific vaginitis can occur in the form of acute purulent vaginitis or have features of a chronic inflammatory disease. The severity of the symptoms of the disease depends on the source of infection.
Two forms of nonspecific vaginitis are more common: serous-purulent and diffuse.
Serous-purulent vaginitis does not have a clear clinical picture. It may be accompanied by minor inflammatory changes in the vaginal mucosa or acquire the features of a pronounced purulent process.
The main symptom of nonspecific vaginitis is pathological discharge. They can be liquid, watery, foamy. If there are a lot of desquamated epithelial cells on the surface of the vaginal mucosa, they enter the vaginal secretion, and the discharge becomes thick. Leucorrhoea often has an unpleasant odor and contains an admixture of blood, accompanied by itching and/or burning, especially when the delicate tissues of the vulva are involved in the inflammatory process.
With severe purulent inflammation in the vagina, the mucous membrane becomes swollen, thickens, and becomes covered with purulent films. When purulent films are removed from the vaginal wall, a wound bleeding surface is formed in their place. Attempts at sexual intercourse and gynecological examination cause the patient severe pain.
Chronic nonspecific vaginitis occurs without pronounced clinical manifestations. More often the patient is bothered by leucorrhoea, but the general condition does not change.
It is perhaps impossible to find an adult woman who has not experienced vaginal discharge. The vaginal microflora of healthy women does not always have constant characteristics; its composition changes before menstruation, against the background of colds, stress and many other circumstances. However, the ability of the vaginal epithelium, together with the immune system, to independently cope with unwanted changes helps the body cope with problems on its own. Only under conditions of poor immunity does acute infectious inflammation develop in the vagina.
That is why acute vaginitis in girls is almost always diagnosed among those under ten years of age. At this age, the immune system of children has not completed its formation, the vaginal mucosa is thin and vulnerable, and the vaginal environment is alkaline. As a result, low resistance to infections provokes vaginitis in children before the onset of puberty.
Diagnosis of nonspecific vaginitis is quite simple and does not require a large list of examinations. Studying the composition of the vaginal microflora using a smear “for flora” and bacterial culture of vaginal contents makes it possible to identify the culprits of inflammation and begin therapy.
Patients often confuse the concepts of nonspecific vaginitis and bacterial vaginosis. Despite the fact that both conditions are provoked by opportunistic microorganisms, they are completely different diseases and are treated differently. With bacterial vaginosis, there is no inflammation in the vagina; in fact, it is a dysbiotic condition of the vagina. Nonspecific vaginitis always means an inflammatory-infectious process.
What triggers the development of the disease
The chronic form of vaginitis is an inflammatory disease that develops against the background of an acute form that is not completely cured or not detected in a timely manner. Initially, the pathology develops due to insufficiently strong immunity or due to a change in the acidity of the vaginal environment. The causative agents of the disease include fungi, viruses, bacteria, including chlamydia and trichomonas. Inflammation of the vaginal mucosa of a non-infectious nature can be caused by the following provoking factors:
- High temperature of the water used for douching.
- Allergens and other substances contained in intimate care products and latex.
- Urine in the presence of genitourinary fistulas, due to which fluid from the bladder enters the vaginal lumen.
- Vaginal dryness against the background of atrophic non-infectious vaginitis, which forms due to a lack of sex hormones in older women.
Inflammatory processes can also begin under the influence of psycho-emotional disorders, but most often the chronic form is the next stage of acute or subacute pathology that has not been adequately cured. Accordingly, subacute vaginitis is a transitional form, the development of which is provoked by vaginal trauma, hormonal imbalances, and deteriorated immunity. Acute or subacute vaginitis can also develop due to uncleanliness.
Attention! Whatever causes the pathology, quite often victims, having noticed signs of the disease, begin to self-medicate, which can also cause a chronic form of colpitis.
The age category in the case of the development of a chronic disease does not matter - older ladies, middle-aged women, young girls and little girls suffer from vaginitis. At the same time, there may be several forms of colpitis formed in the body - it all depends on the reasons that provoke the inflammatory process. Risk factors include:
- Unprotected intercourse with an infected partner.
- Uncontrolled use of hormonal pharmaceuticals.
- Presence of respiratory and other pathologies.
- Endocrine disorders, including diabetes mellitus.
- Carrying a child.
- Constantly arising stressful situations.
- Frequent hypothermia.
- Insufficiently high immunity, and HIV infection can also affect the state of the system.
- Unbalanced diet, abuse of alcohol and spicy foods.
- Long-term use of underwear made of synthetic fabrics.
The chronic type of vaginitis is a sluggish inflammation that develops inside the epithelial tissues of the vagina and in most cases is bacterial in origin. The course of the disease lasts from 2-3 months to several years, and the disease itself can enter the acute stage no more than 3-4 times a year during the period when a woman’s immune system is most weakened due to physiological changes in the body or under the influence of other negative factors. factors present in the patient’s daily life. According to medical statistics, at least 15% of women suffer from a chronic form of vaginitis. Of this total, only 9% are aware of the existence of this gynecological problem and are taking active steps to get rid of the disease. Unfortunately, taking even potent medications does not always bring a positive therapeutic result, and the disease reappears after some time in the form of a relapse.
Reasons for recurrence of the disease
Quite often, after undergoing a course of treatment, vaginitis, which previously occurred in a latent form, again makes itself felt and worries the woman with the same symptoms, which not only reduces the quality of sexual life, but also does not allow her to fully perform her job duties, engage in raising children and running a household. Relapses of vulvovaginitis occur due to the presence of the following causative factors.
Decreased immune status
In order to maintain a stable microflora inside the vagina, it is necessary to ensure reliable protection of the body from the cells of the immune system. Only then, after completing the course of treatment, will the patient be able to maintain her feminine health and not face a recurrence of the disease. If the immune system becomes weak, then a small number of pathogenic microorganisms are activated and a repeated outbreak of infectious inflammation occurs. This behavior of the body indicates that at one time the acute form of this disease remained untreated.
Causes of subacute vaginitis
The form of the disease in question is transitional. It is easy to take a step from it to health, if appropriate therapy is carried out, or to the return of an acute condition. Experts cite the reasons why the latter is likely:
- Low immunity. The weakening of the protective forces makes it possible for pathogenic organisms to multiply, since not enough cells are produced that destroy them;
- Vaginal injury. Damage to its mucous membrane negatively affects the microflora and gives a head start to pathogenic bacteria. The organ reduces its restorative properties;
- Hormonal disorders. A deficiency of some substances and an excess of others negatively affects the composition of the local flora, provoking inflammation;
- Ignoring hygiene standards. This is a circumstance that interferes with normal redox processes. Uncleanliness creates conditions for the proliferation of pathogenic organisms.
If at least one of the listed circumstances is present, the acute course of the disease and with proper therapy may end in the subsidence of the disease, and not in its elimination.
Symptoms of chronic vaginitis
The signs of the latent variety of vulvovaginitis are distinguished by the fact that they appear in the form of an extremely blurred clinical picture and only periodically when the woman’s body is in a weakened state. The symptoms of the disease look like this:
- from time to time a slight tingling, itching and burning sensation is felt inside the vagina, which lasts from a few seconds to 5-10 minutes, and then the pathological symptoms disappear;
- 2-3 times a week a small amount of mucus comes out of the vagina, emitting an unpleasant yeasty or putrid odor (it all depends on what microbes predominate inside the female genital organs);
- at times, a red rash forms on the surface of the labia minora and majora, which does not hurt, but is very itchy;
- the walls of the vagina and the mucous membrane around the genital opening acquire a rich red color, swell and have an atypical appearance;
- during the period of manifestation of the disease, in 35% of cases the body temperature rises, reaching 37 degrees Celsius and very rarely exceeding this threshold.
Most often, these symptoms occur in the autumn-spring season, when a woman is in the most weakened state due to a lack of vitamins, minerals, and the daily presence of damp and cold weather, which can lead to hypothermia. In children, the signs are well described here.
Necessary tests and diagnostics
The list of diagnostic procedures and types of tests that are required for chronic vaginitis are standard and consist of the following manipulations:
- taking a smear from the surface of the vaginal walls to study the bacterial microflora and determine the dominant strain;
- blood from a vein in order to establish the woman’s hormonal levels, conduct a biochemical analysis, and also exclude the possible presence of infectious pathogens that are sexually transmitted;
- clinical blood test, which is taken from a finger and in the laboratory the percentage of red blood cells, platelets, leukocytes, phagocytes, lymphocytes is determined;
- Ultrasound diagnostics of the condition of the organs of the female reproductive system located in the pelvic area.
After receiving the results of these tests and diagnostic procedures, the attending physician receives comprehensive information about the state of the woman’s health and how severe the inflammatory process in the vaginal area is, which has become chronic.
Symptoms and signs of vaginitis
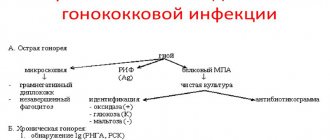
The most informative today are microscopy of a vaginal smear, bacterial culture of vaginal discharge, and blood analysis using the PCR method. Regardless of the pathogen, any vaginitis must be treated, even if its manifestations are minor. The transition to a chronic course and the ascending spread of infection cause inflammation in the ovaries, uterus, fallopian tubes and can be complicated by infertility.
How and with what to treat chronic vaginitis?
The therapeutic course of chronic vulvovaginitis is selected individually based on what type of bacterial or viral microflora was diagnosed based on the results of a study of a selected smear. To completely cure the disease, the doctor creates a complex of therapeutic measures, which includes drugs of the following categories:
- antibiotics (penicillin, synthetic or macrolides, which are administered intramuscularly or taken by the patient in the form of tablets);
- ointments and gels for application directly to the surface of the inflamed vaginal mucosa;
- douching with antiseptic solutions of Miramistin, Chlorhexidine and Furacilin;
- warming the lower abdomen with electrophoresis or dry heat.
The type of specific drug, its dosage, duration and order of administration are determined exclusively by a gynecologist based on the clinical picture of the disease. Self-treatment of a chronic form of inflammation of the vulva is unacceptable, as it will only lead to a deterioration in the woman’s well-being.
Treatment regimen
Experts use the following approach in the treatment of vaginitis:
- use of antifungal and antimicrobial drugs;
- immunomodulatory drugs;
- analgesic and anti-inflammatory drugs;
- vitamins and probiotics;
- treatment of the underlying disease, for example, during menopause, hormonal therapy is carried out.
Suppositories for vaginitis
Depending on the specific pathogen and the stage of the treatment process, suppositories are selected. First, let's talk about the combined type. They can be used either as monotherapy or added to the main treatment.
Let's highlight the popular combination candles:
- Terzhinan. Used in the treatment of specific and candidal vaginitis. One vaginal tablet is administered before bedtime for one to three weeks. Nystatin and ternidazole included in Terzhinan eliminate fungal infections, neomycin is a broad-spectrum antibiotic, and dexamethasone is a hormonal substance that eliminates burning, itching and pain;
- Ginalgin. The product restores the natural balance of microflora. It is used in the treatment of trichomonas and nonspecific vaginitis. Typically the course of treatment lasts from seven to ten days. Ginalgin contains powerful antimicrobial components, and citric acid creates ideal conditions for the development of lactobacilli;
- Polygynax. Neomycin and polymyxin B included in the composition have a pronounced antimicrobial effect, and nystatin has an effect on fungal infection.
Suppositories with lactobacilli are also used, which normalize the acidity of the vagina, restore the microflora and dissolve the biological film from the walls of the vagina. They are usually used after the end of the main treatment. A prominent representative of this group of medicines is Gynoflor, which contains lactic acid bacteria, lactose, which promotes the proliferation of lactobacilli, as well as the female sex hormone, which accelerates the process of regeneration of the mucous membrane.
Antibiotics
Antibiotics for vaginitis are not always prescribed and only based on the results of a laboratory examination. Sometimes the disease can be eliminated by eliminating the provoking factor, for example, reduced immunity and hormonal imbalance.
The doctor selects antibacterial agents. First, let's look at systemic antibiotics:
- Amoxiclav. The drug contains not only the antibacterial substance amoxicillin, but also clavulanic acid, which performs a protective function. The fact is that pathogens produce enzymes that can destroy the antibacterial substance, and this acid prevents such a negative effect.
- Doxycycline. It is a broad-spectrum antibiotic with a bacteriostatic effect.
- Klacid. This is a drug of the latest generation, belonging to the group of macrolides. Effective against chlamydia, mycoplasma, ureaplasma.
If we talk about local antibiotics, they are most often produced in the form of combination drugs Polizhinaks and Terzhinan. They act directly at the site of the pathological process and are less likely to cause side effects.
Treatment of children has a number of its own characteristics. The drugs are used in dosages based on age. First of all, the fight against the main treatment is carried out: diabetes mellitus, pinworms, etc. Measures are taken to strengthen the immune system. To completely eliminate the disease, etiological therapy is carried out.
Folk remedies
Traditional recipes, if used correctly, can help speed up the healing process. You should not replace drug treatment with traditional treatment; this is only an auxiliary therapy that combats unpleasant clinical symptoms. Use these recipes alone after undergoing an examination and making an accurate diagnosis.
Let's consider three options for holding sitz baths:
- chamomile, calendula and sage. Dry raw materials are crushed and thoroughly mixed. It is enough to take two tablespoons of medicinal plants and pour one glass of boiling water over them. Next, keep the product in a water bath for half an hour. After the product has cooled, it is filtered, the required amount of water is added and used in the form of sitz baths;
- infusion. You will need celandine grass. To prepare the infusion, take two tablespoons of chopped herbs and pour them with a liter of boiling water. For three hours, the product is infused in a thermos, it is filtered and used for baths;
- horsetail In the same way, take two tablespoons of chopped herbs, infuse and filter.
It is strictly unacceptable to use these infusions for douching for vaginitis. Sitz baths only! This can lead to injuries to the vaginal mucosa, as well as dysbiosis.
If the cause of vaginitis is insufficient levels of female hormones, medicinal plants that contain phytoestrogens are used. Let's look at two effective recipes:
- Licorice root contains plant estrogens and strengthens the immune system. One tablespoon of crushed root is poured into a glass of boiling water and left for twenty minutes in a water bath. After straining, the infusion is ready for use. You should take one tablespoon of the product thirty minutes before meals;
- Red clover. Also contains phytoestrogens, ascorbic acid, essential oils. The infusion is prepared in the same way, only you should take a third of a glass half an hour before meals.
Complications
The absence of a medicinal effect on the disease or incorrectly selected drugs leads to the fact that over time, negative consequences and complications arise, manifested in the following conditions of the female reproductive system:
- atrophy of the vaginal mucosa and frequent bleeding with a small amount of capillary blood discharge;
- female infertility and the inability to conceive a child despite the use of hormonal medications;
- involvement in the inflammatory process of the ovaries and organs of the genitourinary system (urethra, bladder, kidneys);
- menstrual irregularities;
- a significant risk of developing malignant tumors of the uterus, as well as in the tissues of its cervix;
- lack of a normal personal life and the constant presence of pain during sexual intercourse.
These complications can be easily avoided if you visit a gynecologist in a timely manner and treat inflammatory processes occurring inside the vagina. Otherwise, chronic vaginitis will become a constant companion and the cause of a painful condition of the female genital organs.
According to statistics, a third of women throughout their lives face the problem of vaginitis (colpitis), which often turns into a chronic stage. Despite all the achievements of modern medicine, the number of cases not only does not decrease over the years, but, on the contrary, is constantly growing.
Prevention of vaginitis
Carrying out diagnostic and therapeutic procedures - abortions. curettage of the uterine cavity, probing of the uterine cavity. hysterosalpingoscopy. placement and removal of an IUD (intrauterine device), hydrotubation, and management of labor without aseptic standards increase the risk of developing vaginitis several times. Mechanical trauma to tissues during manipulation reduces their redox capabilities; infection can also be introduced from the outside on gloves or instruments. In addition, the incorrect use of hygienic and therapeutic tampons contributes to the spread of infection. Trauma and foreign bodies in the vagina also contribute to the development of vaginitis.
A long course of vaginitis causes emotional and sexual disharmony in a woman, as well as serious violations of her reproductive health. Women who have bacterial or trichomonal vaginitis are at greater risk of contracting sexually transmitted diseases and HIV infection.
A consultation with a gynecologist is necessary if you: have unusual vaginal symptoms; had unprotected sex or sexual relations with multiple partners; you are considering the possibility of pregnancy in the near future; after the course of treatment, the symptoms of vaginitis persist. Drug therapy for vaginitis is prescribed taking into account the pathogen and factors predisposing to the onset of the disease. For the treatment of bacterial vaginitis, antibiotics are often prescribed, taking into account the sensitivity of the pathogen, both orally and in the form of vaginal products.
The main cause of vaginitis is the entry and reproduction of pathogenic microflora into the vagina due to weakening of the body, poor hygiene, and prolonged mechanical trauma to the mucous membrane. In childhood, vaginitis can develop when infection is introduced hematogenously into the bloodstream during scarlet fever. flu The most common factors predisposing to the development of vaginitis are:
Features of its manifestation are associated with changes in discharge, swelling of the vagina and vulva. Delayed menstruation, long periods, lack of cycle. Bloody discharge of mucus outside the days of menstruation.
Penetration into the internal genital organs occurs through dirty hands and stale clothes. Mechanical damage to the mucous membranes of the vagina often provokes vaginitis. There are frequent cases of the disease in girls of childhood and adolescence. The most likely cause of such cases is viral infection through the bloodstream.
What is the disease
Vaginitis is an inflammation of the vaginal mucosa caused by various factors. This is such a common pathology that almost every woman encounters it throughout her life.
Signs of vaginitis (colpitis) are not always clearly expressed. Often the disease is asymptomatic, which is why the woman does not seek medical help.
Chronic vaginitis is characterized by long periods of remission, during which there are no obvious manifestations of the disease. This condition can last for years, infectious agents are in an inactive state. But as soon as a provoking factor appears, an acute or subacute process develops.
Diagnostic methods
Diagnosis of the chronic form of vaginitis is complicated by long periods of remission, when a gynecological examination is not as effective as in the acute course of the disease.
The gynecologist makes a diagnosis based on:
- information received from the patient;
- external manifestations of chronic inflammation;
Laboratory examination of vaginal microflora is necessary to confirm the diagnosis
- smear of vaginal flora (helps identify the presence and type of pathogen);
- laboratory tests of urine and blood (indicate the degree of inflammation and the general condition of the body).
Causes of chronic vaginitis
In order to understand how inflammation of the vaginal mucosa develops, you need to imagine how and under what conditions representatives of the microflora “get along” with each other.
The vaginal mucosa contains a fairly large number of microorganisms. Their growth and reproduction depend on the acidic state (pH). The acidity of vaginal secretions is regulated by lactobacilli or vaginal bacilli. When their content is sufficient, lactic acid is produced, which maintains a certain pH level. Normally, it is no more than 4.5, and this acidity level suppresses the growth of pathogenic microflora.
The vital activity of lactobacilli is directly influenced by the hormonal status of a woman, that is, the functional ability of the ovaries.
If the hormonal balance is disturbed, for example, during menopause, then the content of lactobacilli decreases. Therefore, older women often suffer from atrophic vaginitis.
In addition to sex hormones, the content of lactobacilli is influenced by the state of immunity, the quality of nutrition and intimate hygiene, stress and various diseases, in particular diseases of the endocrine system.
The quantitative and qualitative composition of the vaginal microflora is influenced by various factors
The quality of sperm plays a major role in the colonization of the mucous membrane with pathogenic bacteria, since with each sexual intercourse without using a condom, a huge number of microorganisms enter the vagina.
With an insufficient amount of lactobacilli, opportunistic flora (streptococci, staphylococci, candida and gardnerella) begin to multiply intensively, and inflammation of the mucous membrane occurs with characteristic symptoms.
As for specific bacteria that provoke STDs (trichomonases, gonococci and chlamydia), their contact with the vaginal mucosa causes inflammation, regardless of the acidity state. They are not present in the normal vaginal microflora.
Risk factors for the development of vaginitis are:
- unprotected sexual intercourse with an unexamined partner;
- uncontrolled use of hormonal drugs;
- unbalanced diet, including alcohol intake, addiction to spicy foods;
- respiratory and other infections;
- endocrine diseases (diabetes mellitus and others);
- pregnancy;
- frequent stress;
- reduced immunity (including HIV infection);
- hypothermia;
- long-term wearing of synthetic underwear.
These factors contribute to both the transition of a chronic process to an acute one and the development of a primary chronic one, with unexpressed clinical signs.
It is worth noting that the quality of nutrition plays a serious role in the transition of infection to a chronic form. The fact is that modern food products, such as canned food, meat and dairy products, contain a certain amount of antibacterial agents. If you regularly consume such food, there is a risk of disrupting the natural microflora of the vagina and suppressing the protective properties of the mucous membrane. Against this background, infectious agents are able to multiply quickly and cause inflammation.
On the other hand, preservatives and antibiotics that are consumed in food inhibit the growth of some pathogenic bacteria. The clinical picture of inflammation is “blurred”; there may not be clear and reliable signs of disease. But the infection does not go away; the bacteria exist for a long time and are activated when the opportunity arises.
Main types of vaginitis
Based on the type of pathogen, vaginitis is divided into bacterial, viral or herpetic, candidiasis, etc. With insufficient production of hormones, atrophy of the mucous membrane occurs and atrophic vaginitis develops. According to the symptoms of the disease, specific vaginitis can be distinguished, which develop under the influence of mycoplasma, trichomonas, chlamydia, etc., as well as nonspecific, which develop under the influence of streptococci and staphylococci.
Vaginitis is a fairly common disease in women. Depending on the type of vaginitis and the nature of its course, local or general medicinal treatment may be prescribed.
Depending on the type of vaginitis, treatment methods will vary. Therefore, it is extremely important to diagnose the type of disease in a timely manner.
Symptoms
The chronic version of this disease is characterized by a long period of remission and relapses. Normal vaginal discharge is a colorless liquid, transparent or whitish, odorless and does not cause irritation to the mucous membrane of the external genitalia. With exacerbation of chronic vaginitis, symptoms of an acute (or subacute) inflammatory process occur.
Signs of inflammation of the vaginal mucosa:
- Increase in the number of discharges.
- Unpleasant smell.
- Inflamed and swollen mucous membrane.
- Unusual consistency and color of discharge (foamy, curd-like, thick green).
- Itching, burning, discomfort in the vaginal area.
- Painful urination and sexual intercourse.
In addition to general symptoms, there are individual differences depending on the specific pathogen. In the chronic version, during the period of remission, patients may not be bothered by anything. Or the discomfort is so minor that it does not prompt you to seek medical help. In this case, the symptoms may go away on their own, until the next provoking factor, but the infection will remain.
Distinctive signs of vaginitis of various origins - table
| Infectious factor | Signs |
| Gonorrhea |
|
| Trichomonas |
|
| Gardnerella | Discharge with a characteristic “fishy” odor. |
| Candida |
|
Trichomonas vaginitis
Among vaginitis of specific origin, trichomonas vaginitis is most often diagnosed. It is the leader among sexually transmitted infections and is associated with many serious complications.
The culprit of the inflammatory process is Trichomonas vaginalis, a single-celled protozoan microorganism with extremely pathogenic properties. Trichomonas enters the body mainly (98%) from a sick person, namely during unprotected sexual intercourse, therefore Trichomonas vaginitis is diagnosed in sexually active women and is very rarely detected in girls.
Trichomonas vaginitis has several forms. After infection enters the vaginal mucosa, so-called “fresh” trichomoniasis develops with an acute, subacute or sluggish (torpid) course. After the acute period, inflammation can occur in a chronic, asymptomatic form. There is also trichomonas carriage, when the presence of trichomonas does not cause illness in the carrier, but can provoke it in a sexual partner.
Acute trichomonas vaginitis has all the signs of severe infectious inflammation and is characterized by an extremely rapid course. As a rule, the disease begins soon (5 – 15 days) after sexual intercourse. Against the background of deterioration in health, profuse, thick greenish leucorrhoea with an unpleasant odor appears; it has a characteristic foamy appearance, which makes it possible to suspect the Trichomonas nature of the inflammation during the initial examination. Abundant purulent leucorrhoea causes irritation of the vulva, causing severe itching and a burning sensation.
Trichomonas have pronounced penetrating ability. In conditions of poor immune defense, they quickly spread through the mucous membranes, penetrating the urethra and cervical canal, causing the phenomena of Trichomonas urethritis and cervicitis. By ascending route, the infection can reach the uterine mucosa, ascend into the fallopian tubes and even into the ovaries, causing not only inflammation, but also infertility.
Inflammation in trichomonas vaginitis is rarely limited to the vaginal mucosa. A gynecological examination also reveals inflammation of the mucous membranes of the cervix and vulva, and there is a lot of foamy yellow-green leucorrhoea in the vagina.
The presence of Trichomonas can be detected with a simple flora smear. To determine the presence of concomitant infection, a bacteriological examination is carried out. Acute uncomplicated trichomonas vaginitis, with timely diagnosis, responds well to simple therapy and is completely eliminated.
Diagnostics
To make a diagnosis, anamnesis is collected (a set of information about the course of the disease). If these symptoms do not appear for the first time, there is reason to suspect a chronic process.
In addition to the characteristic discomfort and discharge, women with chronic vaginitis often experience:
- Dystrophy of the mucous membrane (especially during menopause and later).
- Ulcers on the mucous membrane.
- Cervical erosion is an area of absence of the characteristic epithelium, which visually looks like an ulcer.
- Nabothian cysts on the cervix.
All these changes in the mucosa are detected when examining the vagina and cervix using a gynecological speculum. A more detailed picture is provided by colposcopy - examination using a microscope.
It is important to know that a long-term chronic inflammatory process on the vaginal mucosa causes atypical deformation of cervical epithelial cells. And this is fraught with the development of oncological pathology.
For differential diagnosis of the causative agent of inflammation or a group of pathogenic organisms, specific laboratory tests are carried out:
- Flora smear from the vagina and cervical canal.
- Smear on flora from the urethra.
- Culture of microflora with determination of sensitivity to antibiotics.
- ELISA (enzyme-linked immunosorbent assay) - determination of antibodies to chlamydia, mycoplasma, gardnerella, trichomonas, ureaplasma and candida.
Vaginitis in pregnant women
Yeast colpitis during pregnancy is the most common of all types. Serious hormonal changes lead to changes in microflora and the development of the disease. The course of the disease is quite severe: candidal colpitis during pregnancy is expressed by severe swelling of the mucous membrane, perineal pain, intense discharge with pus and odor.
It is necessary to treat vaginitis during pregnancy in women without delay; the consequences for the child and the expectant mother are very serious:
- intrauterine fetal infection;
- miscarriage or termination of pregnancy for medical reasons;
- placental inflammation, fetoplacental insufficiency;
- perineal ruptures during childbirth;
- sepsis.
How to treat colpitis?
Therapy for chronic vaginitis is long-term, and it is not always possible to get rid of the disease completely. It is important to understand that a chronic process occurs in the body due to many factors that inhibit local and general immunity. Therefore, therapy must be comprehensive.
The following principles are followed in treatment:
- eliminating factors that contribute to the maintenance of chronic inflammation;
- elimination of the pathogen, taking into account sensitivity to antibacterial drugs.
Addressing factors that support inflammation includes:
- Complete nutrition. Preference should be given to “live” foods, that is, mainly raw vegetables and fruits. It is better to exclude meat and fish completely, but if it doesn’t work out right away, limit it to 1-2 times a week. Do not use factory-made dairy products, but home-made ones. Alcohol, spicy and salty foods, and smoked foods should be completely excluded from the diet.
- Elimination of excess weight, especially for patients with endocrine diseases.
- Exclusion of those personal hygiene products that may cause irritation and allergic reactions from the external genitalia.
- Identification and sanitation of other foci of infection - caries, chronic tonsillitis, sinusitis and pyelonephritis, helminthiases.
Treatment of the infection itself is carried out by local and general methods.
The following types of drugs are prescribed (the form and dosage are determined by the attending physician):
- Antibiotics - for specific vaginitis, trichomonas, chlamydia and others (Trichopol, Cefazolin and others). They are prescribed not only to the woman, but also to her partner.
- Estrogen hormones - for atrophic vaginitis in menopausal women (Femoston, Klimonorm).
- Antihistamines (Suprastin, Erius).
- Vitamins of groups B and C.
- Immunomodulators (Galavit, Interferon).
- Antifungal agents (Fluconazole, Diflucan).
Local treatment is also aimed at eliminating the pathogen and increasing local immunity.
- Irrigation of the vagina with antiseptic solutions - Miramistin, Nitrofural.
- Local antibiotics and antiseptics in the form of suppositories or vaginal tablets, for example, Terzhinan, Hexicon. Estrogen suppositories are prescribed to women over 40 years of age, taking into account their hormonal status. For the treatment of candidal vaginitis, Econazole or Clotrimazole is used.
- Eubiotics and probiotics (Vagilac, Lactacid) to restore the number of lactobacilli and maintain normal pH levels.
Drugs used for chronic vaginitis - photo gallery
Folk remedies
There are many medicinal herbs in nature to treat vaginal inflammation. All of them are of great value, but only in combination with traditional therapy that a doctor can prescribe.
Attempts at self-cure using herbal infusions and decoctions increase the risk of an ascending infection - the development of inflammation of the internal genital organs.
To speed up the process of restoration of the vaginal mucosa, use:
- Pharmaceutical chamomile. Use sitz baths and douching with chamomile. To prepare the decoction:
- 2 tbsp. l. dry flowers need to be filled with a liter of hot water;
- keep in a water bath for 15 minutes;
- After cooling to body temperature, you can use the resulting decoction for douching or use it for a sitz bath. Chamomile relieves tissue swelling well and accelerates the healing of damaged areas of the mucous membrane.
- A mixture of St. John's wort and centaury. Used internally for severe itching and burning. To prepare the decoction:
- take a tablespoon of each herb;
- pour a glass of hot water;
- keep in a water bath for 10 minutes;
- After cooling, the resulting decoction should be taken one tablespoon at a time before meals.
- Rose hip. Effective for severe swelling of the vagina. Rosehip infusion is used for douching. To prepare it:
- 100 g of dry fruits pour 500 ml of boiling water;
- keep in a thermos for two hours;
- You need to douche with this infusion after pre-cooling it twice a day.
Folk remedies against colpitis - photo gallery
Treatment of colpitis
It is not possible to cure vaginitis on your own. Treatment of the disease is best left to professionals. The doctor will conduct diagnostic tests, based on which he will prescribe therapy. Treatment should be comprehensive, and the effect should be aimed at the main causative agent of inflammation: antibacterial, antiviral, hormonal drugs, antibiotics, and immunomodulators are prescribed. The issue of combining several types of medications is decided during the examination process.
Innovative medicines allow you to get rid of colpitis and have a beneficial effect on the intimate area. Without disturbing the activity of good microorganisms in the mucous membrane, they fight pathogenic flora. The drugs are not absorbed into the blood. There are no contraindications for expectant mothers.
Common antifungal medications:
- Iodoxide, Neotrizol, Nystatin - vaginal suppositories. The course of therapy is 2 weeks.
- Ketoconazole - cream. We are treated for 5 days.
- Defflucan - tablets. Prescribed for one-time use.
- Metronidazole – suppositories or tablets. Course – 10 days.
- Ampicillin – use for 10 days. Available in tablet form.
- For viral vaginitis, add Valtrex, Zovirax, Acyclovir.
It is possible to cure colpitis with the simultaneous use of local medications. Antiseptic solutions and disinfectants are prescribed. The inside of the vagina is washed with solutions of boric acid, potassium permanganate, and baking soda. Therapy lasts up to 2 weeks.
Treatment of vaginitis should be aimed at eliminating concomitant diseases. Otherwise, the therapy will not be effective.
What accompanies colpitis?
Complex therapy involves getting rid of diseases that accompany vaginitis. Based on the test results and examination, the doctor refers the patient to specialized specialists. If you have problems with excess weight or elevated sugar levels, then the endocrine system is checked.
Drugs are prescribed that maintain the balance of the thyroid gland and strengthen the immune system: vitamins, minerals, probiotics, sorbents, immunostimulants and drugs that promote the absorption of glucose in the blood.
If colpitis occurs due to menopause, first of all, the condition of menopause is treated. Hormonal medications, vitamins and nutritional supplements are prescribed. It is recommended to exercise in a cool room.
For neuroses, antipsychotics, sedatives, and sleeping pills are used. For allergies - hypoallergenic drugs. The nephrologist and urologist will prescribe antibiotics and medications for kidney failure. Additional treatment is only possible under medical supervision!
Possible complications of vaginitis
Untimely treatment threatens with adverse consequences for the female body. The acute course of the disease turns into a chronic, sluggish form. This type of colpitis is difficult to treat. Women experience relapses. The quality of life is noticeably reduced.
Consequences of vaginitis:
- urethritis and cystitis - a disorder of the genitourinary system;
- inflammation of the inner layer of the cervix: erosion, cervicitis, endometritis;
- infertility, difficulties conceiving and bearing a baby;
- ectopic pregnancy;
- various infections not associated with vaginitis;
- the risk of synechia in girls is the fusion of the labia with each other.
If symptoms appear, contact a specialist immediately!
ethnoscience
In practice, folk remedies are used to relieve inflammation. It is recommended that you consult your doctor first. Herbs are prescribed mainly to pregnant women. There will be no expected therapeutic effect, but the itching and inflammation will go away.
Antiseptic collection:
- Add 15-20 g of dry chamomile and calendula to boiling water.
- Cook for 15 minutes and cool.
- We filter and use as a personal hygiene product.
Anti-inflammatory collection:
- Made from fresh herbs. Grind and wash 25 g of coltsfoot and blackberry leaves.
- Brew the raw material with boiling water and leave covered for 1 hour.
- Cool and use for douching and washing.
Alternative products soften the vagina, creating a state of comfort.
Forecast and consequences: is it possible to get rid of the problem completely?
A chronic process is much more difficult to cure than an acute one. An infection that exists for several years manages to adapt to existing conditions. Local and general immunity do not work. Immune cells responsible for recognizing and destroying foreign agents stop responding to them. Therefore, the prognosis for a complete cure depends on the state of immunity.
With correct diagnosis, adequate treatment and conscientious adherence to the doctor’s recommendations regarding lifestyle and nutrition, chronic colpitis can be kept under control, avoiding relapses and possible complications.
Those women who are planning a pregnancy should especially carefully monitor the condition of the vaginal flora. It is this condition that is most likely to provoke an exacerbation of the disease.
This is fraught with consequences:
- Threat of miscarriage and premature birth.
- Risk of intrauterine infection of the fetus and developmental defects.
- Infection of the fetus during childbirth.
- Postpartum inflammatory diseases of the uterus and sepsis.
Outside of pregnancy, chronic vaginitis is dangerous due to the spread of infection higher into the pelvic cavity. Then there is a risk of inflammation of the uterus and appendages, pelvic peritoneum with the development of adhesions, subsequent infertility and ectopic pregnancies.
Prevention
Almost all women of reproductive age are at risk of inflammation of the vaginal mucosa. The quality of nutrition, living in large cities with poor ecology and frequent stress - all these factors have a depressing effect on the immune system. Under such conditions, even your own bacteria, staphylococci and streptococci, can cause the inflammatory process.
Therefore, to reduce the risk of chronic vaginitis, it is recommended:
- Review your diet, excluding, if possible, meat, fish and dairy products produced with the addition of antibacterial and preservative components.
- Timely diagnose and properly treat infectious diseases of other organs.
- Avoid unprotected sex with untested partners.
- Avoid stress, learn to cope with it through relaxation exercises and sports.
- Avoid alcohol and other intoxications.
- Wear underwear made from natural materials.
- If you experience any discomfort or suspect a vaginal infection, do not try to treat it yourself, but seek qualified help.
The occurrence of chronic vaginitis is, as a rule, a decrease in a woman’s immune status for certain reasons. That is why the treatment of this disease is complex, complex, requires an individual approach and is unacceptable without the supervision of a doctor.