Curettage is prescribed for girls of various age categories. After manipulation, menstrual flow will not look the same as before. Heavy periods after curettage can be both pathological and physiological. The cleaning procedure itself can cause a number of complications. You need to follow some recommendations in order to normalize your periods in a short time. The recovery period after the procedure takes several weeks. Any unpleasant symptoms require urgent medical attention. Otherwise, you may miss the development of serious complications.
Scraping is a serious procedure
Medicinal properties of the drug for local therapy
Local treatment of the inflammatory process in the uterus is selected by the doctor individually in each specific case: not always and not all women need to use drugs for insertion into the vagina. Vaginal suppositories for endometritis should provide the following therapeutic effects:
- impact on the maximum number of microorganisms;
- removing germs from the vagina;
- elimination of inflammatory symptoms (itching, burning, excessive leucorrhoea);
- preventing the spread of infection;
- prevention of endometritis during invasive diagnostic interventions.
Terzhinan contains several drugs (Ternidazole, Neomycin, Nystatin), which provides a wide spectrum of action on different types of microbes. The rapid elimination of vaginal inflammation occurs due to Prednisolone, which has an optimal anti-inflammatory effect.
Therapeutic or prophylactic use of suppositories will help prevent the penetration of microbes into the upper parts of the female genital organs, which will be the best prevention of complications (endomyometritis, salpingitis, oophoritis, adnexitis).
Discharge after treatment with Terzhinan
The drug does not penetrate the bloodstream, having a direct effect on the infected areas.
Once in a woman’s body, the tablets begin to melt under the influence of altered temperature conditions and subsequently vaginal discharge removes their remains.
Yellowish, odorless discharge is not considered a pathology and does not cause pain. They can have different consistencies, be liquid or slightly sticky, abundant or scanty. At the beginning of therapy, a slight itching sensation is usually caused, which disappears over time. Observed for several hours after administration of the drug.
The acquisition of secretion from the genital tract of a pathological nature is observed when:
- severe burning, itching, or putrid odor;
- cutting or nagging pain;
- white clots, greenish, brown, reddish, curdled or foamy discharge.
The above symptoms often indicate pathological changes in the body and require consultation with a doctor.
Bloody discharge
A change in the color of vaginal secretion after inserting a tablet from yellow to pink, red or brown occurs due to certain reasons.
Menstrual cycle
Menstruation is not a reason to stop taking the drug. Dissolution of tablets occurs over a longer period of time compared to candles. In addition, they are not washed out even with heavy bleeding and do not lose their medicinal properties.
Using the drug immediately before or during menstruation increases bleeding. This effect is associated with the dissolution of the tablet in the blood, which leads to an increase in the volume of its secretions.
The process does not threaten health and is normal.
Incorrect deposit
When inserting a dry Terzhinan tablet into the vagina, it is possible that the mucous membrane may be injured, which leads to bleeding.
In addition, the woman should take a comfortable position to administer the medication:
- lie on your back with your legs extended or bent at the knees and hips;
- squat down and spread your knees wide;
- stand and at the same time rest one foot on a raised surface.
All actions must be careful to avoid injury to the mucous membrane with your hands.
With erosion and inflammatory processes in the cervix, a dry tablet can have an irritating effect on the affected areas, which leads to slight pink discharge. The same effect is observed with installed intrauterine contraceptives.
Allergic reaction
The appearance of pink mucus may indicate an allergic reaction of the body to the main and additional ingredients of the drug.
Infections
Inappropriate dosage of the drug, negligent attitude to the requirements of the instructions for its use is fraught with the progression of inflammatory and infectious processes, which is manifested by a change in the color of vaginal discharge.
Hormonal imbalances
Despite the fact that Terzhinan contains the hormonal agent prednisolone, its dosages are very small and the effect occurs only at the local level. Therefore, Terzhinan can hardly be classified as a hormonal drug.
However, the use of the medicine may lead to premature menstruation.
Read more Ovulation test from Clover
Presence of neoplasms
If drug therapy is accompanied by a burning sensation, pain and bleeding, you must stop treatment and consult a doctor. Perhaps the reason lies in the presence of neoplasms (polyps and cysts), which bleed under the influence of the active components of Terzhinan.
Pregnancy
Pregnant women should be especially careful to monitor the body's response to Terzhinan therapy.
Thus, brown discharge may indicate a frozen or ectopic pregnancy.
Bloody discharge in large quantities and with an unpleasant odor prevents the flow of amniotic fluid.
Premature birth, placental abruption, or spontaneous abortion in the early stages cannot be ruled out.
If bleeding is accompanied by severe pain in the lower abdomen and lower back, calling an ambulance is required.
Indications for use
After detecting endometritis, the doctor will prescribe complex therapy, which will include a drug for topical use. Terzhinan should be used for medicinal purposes in the following cases:
- when trichomonas are detected in vaginal smears;
- against the background of colpitis and vulvovaginitis;
- with bacterial vaginosis accompanying endometritis;
- against the background of detected thrush (vaginal candidiasis);
- with acute inflammation of the uterus caused by various types of infection;
- against the background of typical inflammatory symptoms in the cervical canal (erosion, cervicitis).
The need for prophylactic use of antimicrobial suppositories arises in the following situations:
- before any therapeutic and diagnostic intervention in the uterine cavity (probing, aspiration, hysteroscopy, abortion, insertion or removal of a device);
- during examination and treatment of erosion on the cervix (colposcopy, biopsy, cauterization);
- against the background of chronic asymptomatic endometritis, as one of the components of preconception preparation;
- against the background of gestation in the presence of any focus of chronic infection in the reproductive organs;
- before natural childbirth to prevent birth injuries and infection of the baby.
Significant advantages of Terzhinan for therapeutic and prophylactic use are the possibility of use during pregnancy (starting from 14 weeks) and high antimicrobial activity against many different microorganisms. By strictly following the doctor’s recommendations, you can get the most beneficial effect when using the drug.
Foamy and curdled discharge
Normal vaginal discharge should be thin or mucous, odorless, and white in color. If, after taking Terzhinan, curdled or foamy leucorrhoea with an unpleasant putrid or rotten odor appears, this indicates the ineffectiveness of treatment or infection with the following infections:
- candidiasis,
- bacterial vaginosis,
- trichomoniasis.
In this case, you need to consult a doctor again. Also, curdled leucorrhoea may indicate the destruction of beneficial vaginal bacteria by the active preparations of vaginal tablets. To normalize the microflora, additional intake of probiotics is necessary.
Complex therapy regimens
Depending on the purpose of use, the doctor may prescribe the following course therapy options:
- preventive (daily administration of a suppository at night 6 days before the diagnostic and treatment procedure);
- therapeutic (for acute inflammation or against the background of endometritis, you should use 10 suppositories, injecting the drug into the vagina once a day before bedtime).
Usually, after 2-3 suppositories, a woman’s unpleasant symptoms disappear, but this is not a reason to stop treatment: it is necessary to continue the therapy recommended by a specialist. Unauthorized and premature cessation of treatment may cause relapse of vaginal and uterine inflammation.
Normal discharge after cleaning procedure
Discharge after such surgery is a natural process. A small amount of bloody mucus should not cause concern to patients. The marks on the pad have many similarities with menstrual marks.
The discharge after curettage of the uterine cavity should be red. Rarely, heavy bleeding may appear - this is also a variant of the norm. The main thing is that a new pad should last for at least 3 hours. Normally, excessive mucus should clear up within 14 days. Sometimes this period extends to 3–4 weeks. An increase in the duration of moderate bleeding is not a pathology, but specialist supervision is necessary.
Contraindications and side effects
The disadvantage of Terzhinan is the multicomponent nature of the drug: if a woman has a tendency to allergic reactions to any antimicrobial component, individual intolerance may occur.
Prednisolone, which is part of the suppositories, is a hormonal drug, so it is undesirable to use the drug uncontrolled and for long courses (more than 20 days).
Sometimes, from the first days of treatment, a woman experiences a strong burning sensation immediately after inserting the suppository, but this initial reaction passes quickly, so there is no need to stop therapy.
The drug Terzhinan, which is part of the combination therapy for endometritis, is an important factor in local therapy. With the help of suppositories, you can remove germs from the vagina and eliminate the symptoms of local inflammation.
The drug is the most important factor in prevention - you must follow the advice of a specialist using vaginal suppositories before any gynecological operations and procedures. The safety and effectiveness of the drug help prevent intrauterine infection of the fetus and treat vaginal infections in pregnant women.
The basis of the course of treatment for endometritis is antibacterial agents, which are used in various dosage forms. Preparations for local use in the form of rectal and vaginal suppositories show high effectiveness. Suppositories are available with different compositions and pharmacological effects. They can have anti-inflammatory, antimicrobial and absorbable effects during adhesions.
Read in this article
Bloody discharge after the drug
In medical practice, there have been cases when women encountered bloody discharge from the genital tract, which they associated with the use of the drug Terzhinan. Considering the chemical composition and mechanism of action of this drug, Terzhinan does not contribute to the occurrence of this adverse reaction. The following factors can cause the formation of this complication:
- Premature onset of menstruation, provoked by hormonal changes in a woman’s body;
- The development of reproductive system diseases such as cervical erosion, endometriosis, polyps and endometritis.
Note! If a pregnant woman, while using Terzhinan, discovers bloody vaginal discharge, she is advised to immediately seek medical advice. Discharge of blood from the genital tract in a pregnant woman may indicate the development of such serious pathologies as premature placental abruption and spontaneous termination of pregnancy (miscarriage). It is important to note that vaginal bleeding has nothing to do with the use of vaginal suppositories.
If a woman experiences bleeding from the genital tract while using Terzhinan vaginal suppositories, she will need a comprehensive medical examination. The standard diagnostic plan contains the following items:
- General clinical blood test;
- Coagulogram;
- Ultrasound examination of the pelvic organs;
- Examination of vaginal smears for cytology;
- Study of blood samples for the level of sex hormones.
This is interesting: How is surgery to remove hydrocele (hydroxycele) in men performed, what are the indications and consequences?
In some cases, to clarify the diagnosis, a woman undergoes diagnostic curettage followed by histological examination of samples taken from the mucous membrane of the uterine cavity.
Note! If necessary, a woman may be prescribed hormonal medications, as well as drugs that normalize the level of estrogen in the body.
What effective suppositories are prescribed for treatment of endometritis?
Therapy of any inflammatory disease of the female reproductive system is a complex system, the main role in which is given to antibacterial and anti-inflammatory drugs. They are usually prescribed in the form of tablets or injections, but suppositories are an equally effective dosage form.
The advantage of suppositories is their direct impact on infectious agents, which contributes to their rapid destruction.
In addition, the active ingredients bypass the gastrointestinal tract and do not have a negative effect on the liver and kidneys.
In the treatment of endometritis, suppositories can be used in two ways:
- by inserting a suppository deep into the vagina (Flagyl, Hexicon and others);
- rectally, that is, by introducing it into the rectum through the anus (Diclofenac, Longidaza and others).
The choice of specific suppositories for the treatment of endometritis depends on many factors:
- the nature of the disease;
- acute or chronic stage;
- severity of symptoms;
- individual reaction to a specific drug.
Types of suppositories
Based on their pharmacological action, the following types of suppositories are distinguished:
- products with an antibacterial effect aimed at pathogenic microflora in the vagina;
- antimicrobial, suppressing the growth and reproduction of pathogenic bacteria;
- preventing the formation of adhesions and having a resolving effect.
Suppositories may contain active substances with narrowly targeted action, but they can also be combined.
And here is more information about the principles of treatment of endometritis.
Anti-inflammatory
Suppositories of this type are used to relieve unpleasant symptoms of a pathological process that can affect other organs of the reproductive system in addition to the uterus.
Drugs aimed at eliminating inflammation are divided into two large groups:
- Steroid anti-inflammatory drugs , which contain natural or synthetic hormones. Such drugs are very effective in relieving the symptoms of inflammation, relieving itching and pain. In order not to upset the hormonal balance, such suppositories can only be used under the strict supervision of a doctor.
- Non-steroidal anti-inflammatory drugs . In modern gynecological practice, such drugs are used very widely because they have significantly fewer side effects.
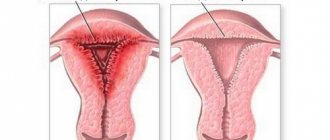
Embryo removal methods
The doctor makes a diagnosis of “frozen pregnancy” based on the following studies:
- Gynecological examination. With the help of palpation, the doctor can determine the discrepancy between the size of the uterus and the gestation period. This method is effective in late stages (from 15 weeks).
- Analyzes. Determining the level of human chorionic gonadotropin in the blood is an informative method for diagnosing frozen pregnancy. Before pregnancy, this figure does not exceed 5 mIU/l; in the first weeks after conception, it sharply increases hundreds of times. When pregnancy is terminated, the hCG level drops and tends to zero.
- Ultrasound examination of the pelvic organs. Ultrasound evaluates the following signs of freezing: heartbeat (absent), embryo development (stops), absence of an embryo in the fertilized egg.
If the results of the research confirm the death of the child, the woman will be provided with psychological support and medical assistance. Methods of fetal extraction depend on the stage of pregnancy. In the early stages, medication is advisable. If more than 7 weeks have passed since conception, the uterine cavity is curetted and cleaned.
Medication is the most gentle way to expel the fertilized egg from the uterine cavity. Under the influence of hormonal drugs, the uterus contracts and its contents come out, along with slight bleeding. The tablets are taken in the gynecological department, where the patient is under observation for 8-12 hours.
If the fetus is only partially aborted with bleeding, dead tissue remains in the uterus. To remove them, cleaning is indicated - a procedure for removing the remains of the embryo or fertilized egg. The manipulations are done under anesthesia, after which ice is applied and medications are given to relieve pain, contract the uterus, and prevent inflammation (for example, Terzhinan).
Rules for the introduction of rectal and vaginal suppositories
The effectiveness of suppositories directly depends on the correctness of their use.
Rectal suppositories to prevent the penetration of infectious agents should be administered after a cleansing enema. You need to use a candle taken from the refrigerator, this will make it easier to introduce it, since it melts easily even at room temperature. Hands should be washed thoroughly with soap before performing the procedure.
The woman herself can determine the body position in which it is easiest for her to administer suppositories; this can be done lying down, pulling her bent knees towards her stomach, standing, leaning slightly forward, or squatting.
The main thing is that when inserting the suppository, the gluteal muscles are completely relaxed, otherwise the procedure may cause pain. The suppository should pass into the rectum without any effort; for this, the anus can be lightly lubricated with a rich nourishing cream or Vaseline.
The suppository is inserted with the pointed end; after administering the drug, the gluteal muscles should be squeezed so that the drug does not spill out after dissolution. It is better to carry out the procedure before bedtime, so that you can lie down immediately after it and not get up for a long time. If suppositories need to be administered several times a day, after each procedure you need to lie down quietly for at least half an hour.
Since many suppositories contain oils, it is recommended to use a sanitary pad after using them, since some of them may leak out and stain your underwear.
Vaginal suppositories are inserted slightly differently. Firstly, it needs to be bent a little so that it stays better in the vagina.
What kind of discharge occurs after cleaning?
In 1–2 months, a woman’s body should recover after curettage. This applies to both hormonal levels and general condition. The duration of final recovery depends on the following factors:
- patient's age;
- the reasons that provoked the death of the fetus;
- chronic diseases;
- the period of gestation of the fetus at which the death occurred;
- number of births and pregnancies in the past.
Burgundy, red or brown marks on the pad after scraping are a natural process. Immediately after the operation they will be very abundant and this should not be a cause for concern. Every day the amount of discharge will gradually decrease.
On the 5th day after curettage of a frozen pregnancy, you should expect brown discharge. The reason for this phenomenon is the oxidation of hemoglobin cells. In the future, the vaginal secretion will also be brown.
The presence of discharge of this shade is a sign of an inflammatory process. Women with green and yellow discharge after curettage of a frozen pregnancy should undergo a number of additional examinations.
Pathological discharge occurs for many reasons:
- Spread of infection in the vagina.
- During the curettage process, the fertilized egg was partially removed.
- During the operation, the reproductive organ was injured.
- A woman develops endometritis.
According to statistics, the highest risk of complications is observed in the first 3 days after surgery. If after this time the woman feels well, and the curettage was carried out by a highly qualified doctor, then complications are unlikely to arise.
Infectious pathologies and inflammations, which cause complications, are usually detected at the time of diagnosing a frozen pregnancy. This is why experts agree that 80% of complications in the first 24 hours after surgery arise due to the unprofessionalism of doctors.
Useful video
To learn how to properly insert suppositories rectally, watch this video:
Different endometritis also requires different treatment. Methods of therapy, regimens for the treatment of chronic and acute, postpartum and autoimmune, purulent will be slightly different. Although the drugs may be the same.
Acute endometritis develops due to infections. It can be purulent, catarrhal. The reasons may lie in abortion, examination procedures, and sometimes postpartum. Symptoms: fever, chills, pain. The treatment is long-term, antibacterial.
One of the effective remedies is suppositories for vaginitis. They are selected depending on the shape and type. What are needed for treatment of bacterial, atrophic, acute, mixed? Which ones will be the best and most effective during pregnancy?
In combination with medications, physiotherapy for endometritis helps to get rid of the problem as quickly as possible. Treatment may include both a set of procedures (especially important in the chronic form) and certain influences.
Almost no disease affecting the female reproductive organs can be treated without the use of suppositories, which are used either vaginally or rectally.
This is especially important in the treatment of inflammatory gynecological processes. Anti-inflammatory suppositories are widely used in gynecology, but in addition to their advantages, they also have a number of disadvantages, as do all other medications.
Use during pregnancy
- Terzhinan is prescribed when planning and during pregnancy for the treatment and prevention of vaginitis of various origins, candidiasis and other urogenital infections.
- The components of this drug have a low degree of absorption, so they do not harm the health of the fetus.
- This drug is recommended for use from the second trimester. Treatment in the first trimester and during lactation is carried out only when the benefit to the mother exceeds the risk to the child.
- The method of use during pregnancy and dosage correspond to the standard treatment regimen.
Suppositories as a dosage form
Suppositories (suppositories) are considered one of the dosage forms of medications and consist of a base (which gives the shape of a candle) and a medicinal substance. A characteristic feature of suppositories is their ability to remain solid at room temperature and melt to a liquid state at body temperature. According to the method of administration, suppositories are divided into 3 groups:
- rectal - inserted through the anus into the rectum and can be shaped like a cigar, cone or pointed cylinder;
- vaginal - inserted into the vagina and come in the form of balls, egg-shaped or cone-shaped;
- sticks - are inserted into the cervix, ureter, external auditory canal, and so on.
The advantage of suppositories is that the drug enters the blood quickly (after 30 minutes about 50%, after 1 hour - 100%), bypassing the digestive tract, without being destroyed in the liver. In addition, suppositories that are administered vaginally, in addition to their generalized effect, have a local effect on the site of damage. When using suppositories, there are practically no allergic reactions, and the administration of suppositories itself is quite simple and painless.
Possible consequences and complications
After the embryo is removed, the threat to the woman’s life disappears. However, often the patient consults a doctor with the following complications:
- bleeding;
- adhesions in the pelvis;
- pain in the lower abdomen;
- inflammatory process due to damage to the walls of the uterus or incomplete extraction of the embryo;
- perforation of the uterine wall.
Within two weeks from the moment of curettage, it is important for a woman to monitor her health and take anti-inflammatory drugs (for example, Terzhinan). It is advisable to undergo a follow-up examination and make sure that the body is gradually recovering. It includes an ultrasound, blood test for hormones, and other examinations as indicated.
Planning a new pregnancy is discussed with a doctor, and both future parents must undergo a medical examination. It is recommended to wait at least six months before conceiving so that the female body can recover. If conception occurs earlier, doctors take all necessary measures to maintain the pregnancy. Under medical supervision, a woman has every chance of bearing and giving birth to a healthy child.
Candles for women with colpitis
When the vaginal mucosa becomes inflamed, we talk about colpitis (vaginitis). Depending on the infectious agent that caused the inflammatory process, vaginitis can be specific (for example, trichomonas, fungal, gonorrheal, etc.) and nonspecific (staphylococcal, streptococcal, polymicrobial). Distinctive signs of colpitis are unpleasant sensations in the area of the external genitalia (itching, burning are unbearable), an increase in vaginal leucorrhoea, as a rule, they have an unpleasant odor, a possible increase in temperature, pain in the lower abdomen, and urination disorders.
The main importance in the treatment of colpitis is the prescription of local therapy aimed at destroying pathogenic microorganisms and suppressing their activity. In the first 3–4 days, douching is prescribed (no more than 2 times a day, see how to do douching correctly) with antiseptic solutions (chlorhexidine, rivanol, sodium bicarbonate, potassium permanganate) and/or decoctions of medicinal herbs (calendula, chamomile, lemon balm , sage). Anti-inflammatory suppositories are prescribed simultaneously with douching.
Treatment of colpitis with vaginal suppositories depends on the pathogen, that is, suppositories are selected that are most active against a particular pathological microflora. Therefore, any drug is prescribed only by a gynecologist based on the results of the clinical picture, laboratory tests and the patient’s medical history; self-medication is unacceptable and dangerous.
Discharge during treatment with Terzhinan
The most common side effect during treatment with Terzhinan is yellow discharge from the vagina. This situation is explained by its physiological nature. The remains of the vaginal medicinal suppository are removed. After the administration of Terzhinan, yellow or even lemon-colored discharge may continue for several hours. During this time, pads should be used to prevent the discomfort associated with this physiological condition.
It’s another matter when they note the appearance of bloody discharge from the vagina after Terzhinan. Women often encounter cases of spotting bleeding, which appear precisely after starting to take the drug. According to the chemical composition of this medication, it should not cause side effects such as bleeding.
If yellow discharge after taking Terzhinan changes its color to pink, red, brown, this may indicate the following:
- Beginning of the menstrual cycle.
Heavy bleeding during the use of Terzhinan is associated with the menstrual cycle. If the drug is taken just before or during menstruation, bleeding increases. This is due to the fact that the dissolved tablet mixes with menstrual blood, increasing its volume. In this case, there is no need to worry.
- Incorrect administration of the tablet.
According to the instructions, it must first be wetted in warm water and then inserted into the vagina. If the drug is administered in dry form, the vaginal mucosa can be injured. This is manifested by streaks of blood in the vaginal secretion or pinkish discharge.
- Inflammation of the cervix or erosion.
If, after taking Terzhinan, bleeding becomes more intense, accompanied by severe pain in the abdomen or lumbar region, which the woman had not previously experienced, you should consult a doctor. Terzhinan cannot provoke such conditions, but the introduction of a dry tablet sometimes causes minor bleeding as a result of irritation of erosive areas.
Pinkish mucus may appear due to an allergic reaction to the components of the drug.
- Infection.
If the instructions for use of the drug are not followed or the dosage is incorrect, the inflammatory and infectious process progresses. This may be manifested by vaginal secretion that has a pinkish tint.
If spotting appears during pregnancy, it may be a pathology. It usually bleeds when premature labor begins and placental abruption occurs. Placental abruption is indicated by abundant pieces of mucus with blood streaks.
Excessive bleeding may be leaking amniotic fluid. They usually have a pungent odor.
Brownish discharge indicates fetal fading or the presence of an ectopic pregnancy. In this case, the dried blood is removed from the body along with the components of the drug.
In this case, while taking the drug, menstruation occurs prematurely.
- Installed intrauterine device.
The presence of pinkish mucus is observed in women with an intrauterine device.
If there is a polyp or cyst, Terzhinan stimulates the release of blood from them.
Nonspecific vaginitis
For nonspecific colpitis, suppositories are usually prescribed, the main components of which include a broad-spectrum antibacterial drug and/or an antiseptic. Good anti-inflammatory suppositories include:
- Polygynax , consists of neomycin, nystatin, polymyxin B, is prescribed 2 times a day for a period of 5 – 14 days, (price 6 pcs. 280 rubles, 12 pcs. 450 rubles)
- Terzhinan is a combination of ternidazole, neomycin, nystatin, prednisolone, prescribed once a day in the evening for 10 days (price 240-400 rubles)
- Meratin-combi , consists of ornidazole, neomycin, nystatin and prednisolone, 1 suppository is administered before bedtime for 10 days
- Mikozhinax , a combination of metronidazole, chloramphenicol, dexamethasone and nystatin, duration of treatment 7 - 14 days, 1 - 2 suppositories per day are administered
- Hexicon , the main substance is chlorhexidine bigluconate, course of therapy is 7–10 days, it is necessary to administer 1 suppository daily (price 250 rubles)
- Betadine - the active substance iodine, is prescribed twice a day for 6 - 12 days (280-350 rubles)
Gardnerellosis
If gardnerella is detected in the smear, suppositories are prescribed, the main active ingredient in which is metronidazole. This list includes:
- Ginalgin (Ukraine), contain tinidazole, sinestrol, vitamin C, lactic acid, daily before bed for 7 - 10 days
- Terzhinan, Meratin-combi (Ukraine), Mikozhinax (Ukraine) twice a day for 12 days
- Metronidazole, Flagyl, Trichopol (vaginal tablets) twice a day for 10 days
- Klion-D - consists of metronidazole and miconazole, it is recommended to use it once a day for 10 days (about 200 rubles)
Genital herpes
The main emphasis in the treatment of genital herpes is on antiviral drugs. Suppositories are used locally, the components of which are antiviral agents:
- A-interferon 1 – 2 times a day for 1 week
- Viferon twice a day for 5 – 7 days
- Poludan three times a day for 7 – 10 days, treat the vulva and insert tampons with ointment into the vagina
- In addition to suppositories, ointments are used for tampons and treatment of the vulva: acyclovir, bonafton, epigen, alpizarin, megosin
Frozen pregnancy: causes and symptoms
Frozen pregnancy is a pathology in which the embryo dies in the uterus without signs of miscarriage. It can happen at any stage of gestation, but most often it is diagnosed before 10-12 weeks. The child’s heart stops beating, his growth and development stops. It remains in the uterus until curettage.
Reasons why a fetus dies in the womb:
- chromosomal abnormalities;
- infections suffered by a woman after conception (rubella, herpes, chlamydia);
- hormonal disorders in the maternal body;
- stress, excessive physical activity experienced by a woman;
- bad habits, drug abuse.
Causes of unknown origin are separately identified. The woman is healthy, leads a healthy lifestyle, takes care of herself and the child. However, the fetus freezes for no apparent reason.
At risk of premature embryo death:
- expectant mothers over 30 years old;
- women with fibroids, non-standard uterine shape;
- women who have had multiple abortions, genital infections;
- ladies with endocrine pathologies;
- patients who have previously been diagnosed with ectopic pregnancy.
For whatever reasons, freezing occurs, it is important to remove the fetus as soon as possible to avoid sepsis and other dangerous complications. The following symptoms will help a woman suspect something is wrong and promptly consult a doctor:
- Scanty menstrual flow. If the fetus dies within three weeks of conception, menstruation is likely to occur. It may come a little later, be scarce and longer. It is possible that a frozen pregnancy will be accompanied by a miscarriage with bleeding.
- Unpleasant sensations in the lower abdomen. Tingling and cramping do not mean that the pregnancy has stopped. These are warning signs of miscarriage. Pain similar to menstrual pain (pulling in nature) can be a symptom of embryonic freezing.
- One of the most striking symptoms of pregnancy is swelling and tenderness of the mammary glands. When the fetus freezes, these phenomena stop abruptly. The same goes for toxicosis. If it tormented a woman at first, and then quickly passed, it’s worth understanding the reason.
When a pregnancy is frozen in the second and third trimesters, the symptoms can be hidden and obvious: (more details in the article: how does a frozen pregnancy manifest in the second trimester: hidden and obvious symptoms)
- Stomach. The uterus stops enlarging because the fetus stops growing.
- Bleeding. Discharge during late pregnancy does not always occur. However, any “smudge” and excessive bleeding should be a reason for examination.
- No movement. Usually, the expectant mother begins to feel the baby's kicks from 18-20 weeks. The lack of embryo activity for 1-2 days should alert you.
- Temperature. After the death of the fetus, an infection often develops in the uterus, which leads to an increase in body temperature to critical values.
Candidiasis colpitis
In the treatment of candidal colpitis, suppositories with an antifungal effect are used: nystatin, natamycin, clotrimazole, canesten. Antifungal creams may be prescribed: pimafucort, miconazole and oral tablets (flucostat, pimafucin, see antifungal drugs in tablets), and also see a detailed review of all suppositories for thrush.
After etiotropic therapy (suppression of activity and death of the pathogen), the second stage in the treatment of colpitis begins, aimed at reviving the normal microflora of the vagina. The purpose of the second stage is to create conditions for the proliferation of lactobacilli and increase their number. The list of candles used includes:
- Bifidumbacterin (contains live bifidobacteria) is prescribed 1 suppository twice a day for 5 - 10 days.
- Bifikol (dried bifidobacteria) daily, one course for 7 - 10 days.
- Acylact 1 time per day in the evening for 10 days (about 110 rubles).
- Vagilak (500 rubles), Laktozhinal (400-450 rubles), these are lactobacilli, 1 vaginal capsule in the morning and evening for a total cycle of 10 days.
In addition, the contents of ampoules with bifidobacteria and lactobacilli are diluted with water and administered intravaginally on tampons (colibacterin, bificol, bifidumbacterin).
Suppositories for adnesitis, endometriosis - for inflammation of the internal organs of the reproductive system
Inflammatory diseases of the internal organs of the female reproductive system are caused by both specific (gonorrhea, trichomoniasis, chlamydia and others) and nonspecific microorganisms. Inflammation of the appendages (adnexitis) is said to occur when pain appears in one or both groin areas, dull, aching and cutting in nature.
Endometritis - inflammation of the uterus is characterized by pain in the lower abdomen, above the pubis and often occurs after intrauterine interventions (abortion (consequences), curettage, surgical birth). Both adnexitis and endometritis occur with a pronounced intoxication syndrome, manifested by a significant increase in temperature, weakness, fatigue, and lack of appetite.
The treatment of inflammatory diseases of the internal genital organs includes, first of all, antibacterial drugs. Along with intravenous infusions and antibiotics, suppositories are prescribed for both adnexitis and endometritis.
Treatment with suppositories for adnexitis and endometritis has several goals. Rectal anti-inflammatory suppositories are suppositories whose main components are non-steroidal anti-inflammatory drugs (NSAIDs). NSAIDs have a number of effects:
- anti-inflammatory;
- anesthetic;
- antipyretic.
Anti-inflammatory and analgesic properties are realized due to the ability of drugs from the NSAID group to suppress the synthesis of prostaglandins, which are formed in large quantities during inflammation and cause pain. Rectal anti-inflammatory suppositories are prescribed simultaneously with the start of antibiotic therapy for a total cycle of 7–10 days:
- suppositories with Indomethacin 1 time in the evening
- Movalis suppositories 1 time before bedtime (active ingredient myeloxicam) for 5 - 7 days
- Voltaren suppositories morning and evening
- belladonna suppositories 1 to 3 times a day (strong analgesic)
- Diclofenac suppositories daily, 1 suppository
- Flamax suppositories (active ingredient ketoprofen) once for 7 days
Anti-inflammatory suppositories for adnexitis and endometritis are also prescribed intravaginally. First of all, pursuing the goal of sanitizing the vagina and suppressing anaerobic microflora, in particular Trichomonas.
Vaginal suppositories include fluomizin and terzhinan, the main substance of suppositories is metronidazole. The treatment cycle lasts 7–10 days, 1–2 suppositories are prescribed daily.
After completing therapy with anti-inflammatory drugs (both suppositories and injections or tablets), it is necessary to restore the normal biocenosis of the vagina. For this purpose, suppositories with bifidobacteria and lactobacilli (bifidumbacterin, acylact and others) are prescribed. Also, during the recovery period for inflammation of the pelvic organs, Longidaza suppositories are used.
Longidaza suppositories are a drug that has proteolytic properties and prevents the formation of adhesions or resolves them. In addition to enzymatic activity, longidase normalizes immunity and has antioxidant and anti-inflammatory properties. The course of treatment is long, from 14 to 21 days, suppositories are administered rectally, 1 at a time before bedtime.
Rehabilitation after frozen pregnancy and curettage
Fetal death is one of the reasons why women do not carry a pregnancy to term, regardless of their socioeconomic level and lifestyle.
The danger is that it appears only after the death of the fertilized egg. Sudden spontaneous termination of pregnancy is stressful for the body and psychological trauma for the woman and her family members. Hope for the future is planning a new conception, the success of which is determined by quality treatment and rehabilitation after a missed pregnancy.
Treatment methods
It is impossible to revive a dead fertilized egg. It gradually decomposes, over time an infection begins to develop in it, which causes intoxication and can result in sepsis.
Therefore, treatment is aimed at removing the fetus from the uterine cavity without any residue, and restoring the woman’s body after this. The choice of technique depends on her state of health, the duration and development of pregnancy until the moment of fading.
The following removal methods are used:
- Spontaneous miscarriage.
- Vacuum aspiration (mini abortion).
- Medical (tablet, pharmaceutical) abortion.
- Curettage (cleaning) of the uterine cavity.
The most commonly prescribed methods are tablet abortion, curettage, mini-abortion, and less commonly, miscarriage. If the fetus freezes in the later stages, artificial birth is performed.
Use of spontaneous miscarriage and vacuum aspiration
Fading pregnancy is accompanied by a decrease in the concentration of a specific hormone in the woman’s body - human chorionic gonadotropin. The uterus reacts to this by contracting, rejecting the dead fetus and pushing it out through the slightly open cervix. The method is prescribed if a woman has no symptoms of inflammation.
Complete miscarriage without complications is confirmed by ultrasound examination. If fetal remains are found in the uterus, a vacuum or curettage is performed.
The first week after a spontaneous miscarriage may be accompanied by slight pain in the lower abdomen and discharge with a small amount of blood. After a few weeks, the woman’s body recovers, and a month later her period begins. The method is used in the absence of signs of inflammation and intoxication in the woman’s body.
If the fetus is frozen at 5-6 weeks, vacuum aspiration of the contents from the uterine cavity is prescribed using an inserted catheter. In this case, only the top layer of mucous membrane is removed and the embryo is removed. A control ultrasound is performed.
The detected remains of the fetus in the uterus are sucked out again with a vacuum, or mechanical curettage is performed. 2 weeks after the mini-abortion, the woman’s body is restored, menstruation appears on the 35th - 40th day.
Tablet removal of a frozen fetus is performed during the period of embryonic development - no later than the 7th week of pregnancy.
The woman takes drugs that block the action of progesterone in two stages according to the scheme - Mifepristone, Mifegin. Their properties are enhanced by Misoprostol. Under the influence of drugs, the uterus actively contracts, rejects and, with bleeding, pushes out the embryo. After its release, the bleeding gradually stops, but it is smeared for several more weeks.
On the first day, the woman feels pain in the lower abdomen, which is relieved with the help of an antispasmodic - No-shpa. Painkillers are taken only as prescribed by a doctor. Uncontrolled use of such drugs significantly weakens the immune system.
The menstrual cycle starts from the start of bleeding after taking the pills. Within 2 - 3 months it will normalize. The first menstruation lasts up to 2 weeks.
2 weeks after the abortion, the remains of the fetus in the uterine cavity are examined by ultrasound. During this time it should be completely cleansed. If this does not happen, vacuum aspiration or curettage is performed.
Rehabilitation after medical termination of pregnancy comes down to following a number of doctor’s recommendations that help restore the woman’s body. He reviews the patient’s diet, helps balance it, and includes vegetables and fruits in the menu.
To strengthen the immune system, the doctor prescribes a vitamin complex. He also recommends following simple rules:
- avoid psycho-emotional stress, learn to manage it;
- exclude any physical activity;
- include rest and walks in the fresh air in your daily routine;
- give up smoking, alcohol, strong coffee;
- exclude the use of water procedures in baths, saunas, baths, swimming in pools, ponds;
- monitor the restoration of the menstrual cycle, the nature of vaginal discharge after an abortion;
- begin sexual activity after the end of the first menstruation;
- It is necessary to protect yourself from pregnancy for the first 6 months, and discuss contraception with your doctor.
Every woman after an abortion thinks about how to quickly recover and conceive a child again. This should not be allowed until the body is fully rehabilitated. This can negatively affect pregnancy.
The pharmaabortion method is the simplest and most accessible; it is easily tolerated by women. But it should be used only as prescribed by a doctor and under his supervision.
Curettage of the uterine cavity is prescribed in cases of fetal death at 7-8 weeks of pregnancy and later. Before the operation, the woman is examined and given special training. Cleaning is performed in a hospital setting, under anesthesia (general or local), with dilation of the cervix.
They are scraped with a special instrument (curette). The top layer of the mucous membrane is cleaned and removed along with all the contents of the uterine cavity. Cleaning materials are sent for histological examination to determine the cause of fetal death.
Treatment after a frozen pregnancy and curettage begins during surgery - drugs are administered to quickly contract the uterus (Oxytocin, Pituitrin).
The complex of therapeutic and restorative measures after surgical removal of a frozen fetus includes:
- antibacterial drugs that prevent the development of infection in the uterine cavity (Ceftriaxone, Metronidazole, Gentamicin);
- contraceptive hormonal drugs that protect against pregnancy and restore hormonal levels in a woman’s body (Regulon, Marvelon);
- vitamin complexes to support immunity;
- proper nutrition with the inclusion of meat, vegetables, fruits, lactic acid products, juices in the menu;
- conducting a control ultrasound to identify fetal remains in the uterine cavity.
Incomplete curettage is an indication for repeated cleaning. If severe pain occurs after surgery, your doctor may prescribe painkillers.
It is recommended to start sexual activity no earlier than a month after cleansing. During this period, the endometrium is restored, and the likelihood of penetration and development of infection in the uterine mucosa is significantly reduced.
Menstruation begins 2 to 8 weeks after surgery. If the menstrual cycle is not restored, hormonal medications are prescribed - analogues of progesterone (Duphaston, Utrozhestan).
At the first fading of pregnancy, the doctor most often finds them in the woman’s health problems in the first trimester. No additional research is being carried out.
The histology of curettage materials provides an answer to the reasons for repeated fetal freezing. In some cases, the doctor prescribes a comprehensive examination of both spouses. After this, if necessary, treatment is performed.
A sudden miscarriage is a psychological trauma for a woman and develops into depression. She blames herself for the death of the fetus. Therefore, the gynecologist refers each patient to a psychologist to receive professional help.
It is important for her family, especially her husband, to surround her with care and attention and be patient. The woman is depressed, loses interest in life, is indifferent to everything, and cries. She needs to be convinced that motherhood will happen, but for this she needs to recover.
It is more correct to discuss this topic rather than feel sorry for the woman. During this period, it is better to protect her from contact with small children and pregnant women.
Communication with family and friends, practicing your favorite hobbies, meditation, walks will help you find peace of mind and confidence in future motherhood. This takes 1 – 2 months. Prolonged depression can last up to 6 months.
In this case, to restore the woman, they involve a psychiatrist who prescribes drug treatment using antidepressants and tranquilizers. The heartache subsides, life goes on, and the family plans a pregnancy again.
The success of re-conception depends on following all the prescriptions and recommendations of the attending physician, and observing the recovery time after cleaning. A healthy lifestyle, a good family climate, harmony in family relationships and observation by a gynecologist will help you safely endure your next pregnancy.
A dead embryo poses a great threat: due to the decomposition of fetal tissue, an infectious process begins to develop in the uterus, and the pregnant woman’s body becomes intoxicated. For this reason, curettage should be carried out as quickly as possible. As soon as a stoma is diagnosed by ultrasound, the gynecologist should conduct an examination and direct the woman to the safest and most effective method of cleansing. They come in several types:
- Medicinal cleaning. The doctor prescribes special medications to be taken orally. They provoke miscarriage of a dead fetus. This method is relatively safe. The only caveat is that after the 5th week of pregnancy, such drugs cannot be used, because they will be ineffective.
- Vacuum aspiration. This intervention is carried out using a special device that is inserted into the uterus to suck out the fertilized egg. The vacuum is always carried out in a state of medicated sleep, because otherwise, the woman will be forced to endure severe pain. The advantage of the method is minimal trauma to the tissues of the reproductive organ. Doctors resort to this method of cleansing until the 8th week of pregnancy. The discharge after cleaning a frozen pregnancy in this way will not be abundant. However, it is better for the patient to stay in the hospital for some time under the supervision of gynecologists.
- Scraping. The most traumatic method, which is also performed under anesthesia. It is carried out through the use of gynecological instruments inserted into the uterine cavity. The main danger of this method is that in the future a woman may have problems conceiving. Another significant drawback is the long rehabilitation period.
- Artificial birth. If fetal death occurs during a long period of pregnancy, doctors induce artificial birth. To do this, the uterus is stimulated with special drugs that promote its contraction. Often, artificial birth is not enough, which is why doctors resort to curettage.