Diseases that have an infectious etiology are called viral hepatitis , they have one unifying property - they cause inflammation and provoke liver necrosis.
One of the characteristic symptoms is jaundice. The first mention of the icteric epidemic was described by Hippocrates in the 5th century BC. The definition of hepatitis in current medical practice implies an independent disease or a generalized pathology. Important! The liver affected by the inflammatory process (with hepatitis A, B, C, D) is a concomitant symptom of diseases such as herpes, AIDS, rubella, etc.
What are hepatitis?
Hepatitis is an inflammatory pathology of the liver. Depending on the course, acute and chronic varieties of the disease are distinguished. The acute form is distinguished by pronounced clinical manifestations and has 2 outcome options - complete cure or chronicization of the pathological process.
In most cases, the cause of development is: viral agents, excessive consumption of alcoholic beverages, uncontrolled use for a long time of drugs that have a hepatotoxic effect.
When a diagnosis of “chronic hepatitis” is made, it is assumed that the “experience” of inflammation is more than 6 months. According to the morphological picture, dystrophic transformations are observed in the liver tissues, which do not affect the lobular structures.
Primary chronic forms occur in the absence of symptoms or with minor manifestations. Often the problem is discovered by chance - during a preventive medical examination or during an examination due to other complaints of the patient.
Pathogenesis of the development of acute and chronic forms of the disease
The acute form is a consequence of direct damage to the liver by hepatotoxic substances or the activity of a viral infection, an autoimmune disorder in the body - the immune system produces antibodies that attack its own liver.
Regardless of the cause, an acute inflammatory reaction is observed in parenchymal tissues, hepatocytes are damaged and destroyed, the liver swells, and the functionality of the internal organ deteriorates.
Since the gland tissues are not equipped with pain receptors, pain syndrome develops in exceptional cases against the background of severe hepatomegaly - a significant increase in the right and/or left lobe of the liver.
The cause of the chronic form appears to be the lack of conservative therapy or an incorrect therapeutic strategy of the acute variety. Often anicteric hepatitis is not diagnosed in time, which causes the pathological process to become chronic.
With chronic hepatitis, foci of dystrophy form, liver tissue degenerates, the functioning of the organ is disrupted, and the risks of developing cirrhosis increase.
Classification of hepatitis
In medical practice, several classifications of diseases are used. So, depending on the symptoms and course, acute and chronic varieties are distinguished.
Classification by etiological factors:
- Alcoholic.
- Medication.
- Viral.
- Autoimmune.
- Secondary hepatitis (develops due to concomitant diseases).
- Cryptogenic (idiopathic) hepatitis means that the cause of the disease has not been established.
There is a separate group of specific hepatitis. For example, there is opisthorchiasis (liver damage by opisthorchiasis), echinococcal (against the background of liver echinococcosis).
Classification depending on clinical manifestations - anicteric form, icteric and subclinical. Autoimmune types of hepatitis differ by type; they are caused by antibody targets - type 1, 2, 3.
https://youtu.be/iaZoaWT_TCM
Treatment prices
You can seek help from a public or private clinic. Average prices in Moscow are as follows:
- Ultrasound of the abdominal cavity - 2000 rubles;
- Consultation with a specialist – 1000 rubles;
- Ultrasound of the liver, gall bladder – 1500 rubles;
- AST, ALT – 220 rubles;
- Total bilirubin – 230 rubles;
- Coagulogram – 1200 rub.;
- Biochemical liver tests – 1300 rubles;
- Magnetotherapy – 800 rub.;
- Ceruloplasmin – 700 rub.;
- Hirudotherapy – 1800 rubles;
- MRI of the liver – 8,000 rubles;
- DMV therapy – 700 rubles;
- Bile acids – 1000 rub.;
- Electroneurostimulation – 900 rub.;
- Infrared therapy – 500 rub.
In general, the cost of treatment is the price of drugs. Expensive effective products such as Pegintron, Pegasys, Rebetol will cost 45 thousand rubles per month. Domestic antiviral interferon will cost 20 thousand rubles. Treatment lasts one and a half years. The entire course will cost at least 800 thousand rubles. As for non-viral hepatitis, treatment is much cheaper, since you will have to buy hepatoprotectors, anti-inflammatory drugs, vitamins, prokinetics, and sorbents. On average, a course for 2 months will cost 10 thousand rubles.
Hepatitis A or Botkin's disease
The viral form of hepatitis A is an acute infectious lesion of the liver, characterized by a benign course, leading to necrosis of liver cells. Botkin's disease rarely transforms into a chronic course.
Causes
The mechanism of transmission of the virus is fecal-oral. An infected adult or child sheds many viral particles into the environment through feces. They get into water, food, and household items.
When pathogens enter the oral cavity of a healthy person susceptible to infection, hepatitis develops.
Infection occurs when swimming in dirty pools or bodies of water. When consuming contaminated foods or poorly purified water. When living together with a sick person, infection occurs when touching household objects - door handles, towels, toys, etc.
Clinical manifestations
The incubation period is 14-28 days. The entire clinical picture can be divided into three periods - pre-icteric, icteric and recovery stage.
In the pre-icteric period, symptoms are scanty, the patient is concerned about signs of intoxication and an increase in body temperature. An increase in temperature is not observed in everyone - in approximately 50% of patients.
The duration of the icteric period is 14-28 days, it is manifested by the following symptoms of hepatitis:
- On days 5-10 the skin turns yellow.
- Change in color of urine - becomes darker in color.
- Discoloration of feces.
- Pain in the right hypochondrium.
- Enlarged spleen.
- Dyspeptic disorders.
- Joint and muscle pain.
- Itching of the skin.
The recovery period lasts from 7 to 150 days. Symptoms gradually weaken and then disappear completely.
Features of therapy
Acute hepatitis A is not a dangerous disease, since it rarely leads to serious complications and does not require specific treatment. In case of severe symptoms, symptomatic therapy is carried out, including drugs from the following groups:
- Vitamin complexes (Aevit).
- Hepatoprotectors (Karsil).
- Enterosorbents (Smecta).
- Enzyme agents (Creon).
- Immunomodulators (Thymogen).
- Choleretic medications (Allohol).
Against the background of a sharp deterioration in health, hormonal therapy is carried out, Prednisolone and Methylprednisolone are prescribed.
Clinical manifestations
In patients with hepatitis, the skin turns yellow.
A clear symptom of liver diseases is a yellowish color of the skin and mucous membranes. Patients suffer from unmotivated weakness, fatigue, decreased appetite, nausea, pain or a feeling of heaviness in the right hypochondrium. Often the patient’s joints ache, the urine is dark, and the stool is light.
There are no special symptoms for chronic hepatitis. Liver damage is often accompanied by skin rashes and itching, allergic reactions, especially to the sun. In most cases, the patient has an elevated body temperature. As the disease progresses, varicose veins of the digestive system may develop, which is accompanied by bleeding.
If you have a combination of the described clinical manifestations, you must contact a medical institution.
Hepatitis B and its dangers
Viral hepatitis type B (another name is serum sickness) is an infectious lesion of the liver tissue, which occurs in different ways - from asymptomatic carriage to destructive processes in the gland.
Etiological factors
The cause of its occurrence is the penetration of the virus into the human blood upon contact with the biological material of the patient.
The danger of the disease lies in the fact that there are no symptoms for a long time, but pathological processes in the liver are detected.
The disease is contagious, and there are several ways of transmitting the pathogen. Thus, virus penetration is possible in the following cases:
- Sexual path. In a sick person, virus particles are found not only in the blood, but also in all biological fluids in the body - sperm, saliva, etc.
- Through saliva is an unlikely but possible variant of infection. During a deep kiss and against the background of a violation of the integrity of the mucous membranes in the mouth, an infection is detected.
- Blood is the most common route of transmission of the virus. You can become infected during any medical intervention/manipulation if unsterile instruments are used. Infection occurs in nail salons and dental offices.
- The vertical path is from a sick mother to a child. Pregnancy proceeds without complications, but during childbirth the child will come into contact with the woman’s biological material, which increases the risk of transmitting the virus. In rare cases, intrauterine infection is observed - with a significant viral load in the mother’s body.
The hepatitis B virus is characterized by increased resistance to aggressive temperatures, alkaline and acidic solutions. The viability of pathogens in dried blood remains for a long time.
Symptoms
The virus can exist in the human body for a long time without manifesting itself. If characteristic signs of a viral disease are observed, then complications have already developed.
The clinical picture is represented by patient complaints - nausea, disturbances in the digestive system, pain in the right side, jaundice, persistent increase in body temperature, fever. Other signs include discoloration of feces, darkening of urine, dizziness, loss of appetite.
Against the background of reactive (fulminant) hepatitis, the symptoms are pronounced, hepatic coma quickly develops, and the mortality rate is over 90%.
Treatment and complications
Therapy is carried out comprehensively - dietary nutrition is prescribed (table No. 5), basic antiviral treatment, etiological and symptomatic medications. If the patient has an acute course of the disease, hospitalization is required.
Basic antiviral treatment includes the use of interferons in combination with the drug Ribavirin. The duration of the therapeutic course and dosage of medications are calculated individually.
Complications of hepatitis B - fatty hepatosis, hepatic cell failure, encephalopathy (leads to damage to the brain and central nervous system), liver cirrhosis, primary cancer, respiratory failure. Such negative consequences have a high mortality rate.
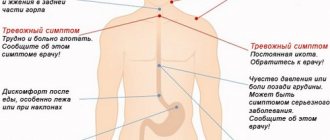
Symptoms of the disease
The inflammatory process occurring in the liver can have varying degrees of severity:
- there are no obvious signs of the disease;
- fever, general malaise;
- detectable main signs of the disease, but without yellowing of the skin;
- vivid expression with all the inherent signs and manifestations.
Despite the different types of the disease, there are common symptoms for a diseased liver. These include:
- pain or tightness in the right hypochondrium;
- constant feeling of fatigue;
- temperature increase;
- joint or muscle pain;
- loss of appetite;
- the appearance of bitterness in the mouth;
- heartburn, nausea or vomiting;
- dark brown urine color;
- light-colored stool;
- yellow color of the sclera of the eyes;
- yellow skin color.
Hepatitis C
Hepatitis C is a liver infection of viral origin. The pathogen is transmitted by transfusion.
The disease is prone to chronicity, leading to cirrhosis and the formation of malignant tumors.
The causative agent HCV mutates in the body. Medicine knows 11 genotypes of the viral agent, although WHO recognizes only 6 types. Genotyping is part of the diagnosis, allowing you to prescribe adequate treatment and determine the prognosis.
Pathogenesis of development
According to statistics, in 30% of cases it is not possible to establish the exact cause of the disease. The most common route of transmission is intravenous administration of narcotic drugs using unsterile syringes.
Transmission of the virus is possible in the following cases:
- During surgery, during blood transfusion.
- Dental procedures.
- Using someone else's toothbrush, nail scissors, or shaving accessories.
- Cosmetic manipulations that are associated with the risk of violating the integrity of the skin.
The likelihood of infection during unprotected sex also remains if the skin and/or mucous membranes are damaged.
How does the disease manifest itself?
The incubation period of the viral disease varies from 2 to 22 weeks. In some cases it is 26 weeks. Against the background of an acute course, no pronounced symptoms are observed, as well as changes in the color of the skin.
Clinically, the disease is manifested by weakness, apathy, decreased appetite, rapid satiety, and weight loss. Sometimes the patient experiences dyspeptic disorders - nausea, heartburn, vomiting, increased gas formation.
Feverish state, increased body temperature - such signs develop in only 35% of patients. The clinic is affected by concomitant illnesses - HIV, autoimmune pathologies. As a rule, the intensity of symptoms is directly determined by the concentration of viral particles in a person’s blood.
Hepatitis C can provoke an exacerbation of concomitant diseases, such as cholecystitis, pancreatitis, etc., as a result of which the clinical picture will be supplemented with uncharacteristic signs.
In 1% of cases, a severe course of the pathology is observed, and serious autoimmune disorders occur.
Treatment Options
The therapeutic strategy is comprehensive; the patient is advised to abstain from alcohol and smoking. A diet is prescribed - animal fats are excluded, while the normal ratio of carbohydrates and proteins remains. Avoid foods that stimulate the production of bile and liver enzymes.
Antiviral treatment involves the use of interferons and Ribavirin, the duration of the course is determined individually. To prevent bile stagnation, the use of ursodeoxycholic acid drugs is recommended. Antibiotics are used for infectious processes.
According to indications, antispasmodics, enzymes, antihistamine tablets, and vitamin-mineral complexes are prescribed. In severe cases, infusion of glucose and electrolyte solutions is required.
Most often, the disease is diagnosed when complications have developed. And this worsens the prognosis and affects life expectancy, since hepatitis C leads to the development of cirrhosis and hepatocellular carcinoma.
Diet
During therapy, you need to avoid alcohol, fatty and fried foods, foods containing preservatives, flavors, flavor enhancers, and other chemical additives. You cannot drink carbonated drinks or strong black tea.
Currently reading: What is hepatic steatosis and how to treat it
Normalize your diet, don’t overeat, don’t starve. It is allowed to eat fermented milk products, cereals, vegetables, fruits, and berries. They prepare soup, porridge, minced meat products, fish, and scrambled eggs. Warm foods should be eaten, cold and hot foods are prohibited. Drink more mineral water, as well as decoctions of medicinal herbs. Helps restore the liver: rose hips, immortelle, celandine, wormwood, tansy, chamomile, mint, lemon balm, calendula. To speed up the flow of bile, it is recommended to consume 1 dessert spoon of vegetable oil in the morning on an empty stomach.
Hepatitis D and differences from other forms
Another name is delta hepatitis. This is an infectious lesion of the liver tissue, coinfection or superinfection of viral form B, which negatively affects the course and prognosis of the disease.
The cause of development is an RNA virus, which belongs to the Deltavirus family. Unlike other hepatitis pathogens, D cannot independently produce proteins for reproduction, and uses substances that are produced by the foreign agent B.
Pathogen D is immune to environmental factors. It is not affected by freezing and thawing, heating, acid, or alkaline solutions. The route of transmission is parenteral, a prerequisite for the disease is the active hepatitis B virus. The pathogen D is introduced into its genome, enhancing the ability to replicate.
The disease comes in several varieties:
- Coinfection is when viruses D and B are transmitted at the same time.
- Superinfection is the joining of virus D to B.
Pathogen D aggravates the clinical picture of hepatitis B. The incubation period is no more than five days (coinfection), and with superinfection it is about 3-7 weeks. The pre-icteric period is characterized by a rapid course.
The combination of viruses in the body can be diagnosed using laboratory methods - in the acute period, IgM antibodies are observed, during the subsequent period, exclusively IgG is determined. The only reliable method of diagnosis is PCR analysis to detect RNA viruses.
Hepatitis G and F
Hepatitis G is a pathology of viral origin, the causative agent of which is an RNA virus. The properties of G are similar to C. The reason is the parenteral route of infection, that is, contact with infected blood. Medicine knows cases of vertical transmission of the virus during sexual intercourse.
The clinical picture of G-infection is mild; rarely the disease leads to the development of cirrhotic processes and functional disorders of the liver. This is subject to monoinfection. If there are several pathogens in the body at the same time, they enhance the harmful effects of each other.
Hepatitis F develops due to the penetration of a pathogen into the body, which in structure resembles an adenoviral infection. The source is a sick person or a carrier who himself is unaware of his illness.
The main route of transmission is fecal-oral, less often hematogenous - due to the transfusion of contaminated blood, from mother to child, when using unsterile instruments. There are no exact data on the incubation period. Most doctors stick to 2-4 weeks of variability.
Clinical manifestations of hepatitis F at the initial stage:
- Weakness.
- Lethargy.
- Chills.
- Increased sweating.
- Emotional instability.
- Slight increase in body.
During the extended clinical period, patients complain of vomiting, nausea, headaches and dizziness, increased gas formation, and jaundice. After a kind of exacerbation, the symptoms subside, the disease becomes chronic.
Reasons for development
Alcoholic hepatitis is caused by regular consumption of alcoholic beverages over a long period. Once in the body, alcohol is broken down by enzymes produced in the stomach and liver, and then the breakdown products are excreted through the lungs, skin and urinary system.
The liver bears the main burden - it processes more than 80% of incoming alcohol. At the first stage of alcohol processing, acetaldehyde is formed - a highly toxic substance, which is then broken down into acetic acid, and that in turn into water and carbon dioxide. These substances are ultimately eliminated from the body.
Alcohol and the liver
With large doses of alcohol, the liver does not have time to process all the toxins and they begin to gradually accumulate in the cells, causing pathological changes. At the first stage, the process of formation of fatty acids is disrupted, fat accumulates in the cells, which leads to alcoholic fatty liver degeneration. Then the inflammatory process begins, and healthy cells are gradually replaced by connective tissue - liver fibrosis develops.
The risk of alcoholic hepatitis increases significantly under the influence of the following factors:
- large amounts of alcohol drunk at one time;
- genetic characteristics;
- history of viral hepatitis;
- deficiency of nutrients caused by improper, poor nutrition;
- overweight;
- autoimmune diseases;
- long-term use of medications, with side effects such as negative effects on liver function.
Gender matters - women are significantly more likely to develop the disease.
Toxic hepatitis and liver damage
Toxic liver damage can be acute or chronic. It develops due to the penetration of dangerous substances into the body (alcohol, toxins, mushrooms, poisons, etc.).
Reasons and factors
Ingestion of harmful substances into the body can be accidental (for example, during professional activities associated with hazardous components) and intentional (intentional).
Medical specialists identify a lot of compounds that have hepatotoxic properties - they have a detrimental effect on liver cells, promoting the death of hepatocytes.
Pathogenesis of the toxic form of hepatitis:
- The use of medications (antiviral, antituberculosis, anticonvulsant, antibacterial agents).
- Poisons of industrial origin (phosphorus, arsenic).
- Alcoholic drinks.
- Poisonous plant substances (mushrooms, poisonous herbs).
Toxic damage from alcohol develops in experienced alcoholics who often and in fairly large quantities consumed alcoholic beverages.
How does gland damage manifest?
The acute form of the pathology in mild cases practically does not manifest itself at all; only general signs are revealed in the form of weakness, lethargy and weakness.
In case of severe toxic damage, the symptoms are as follows:
- Severe pain in the right hypochondrium.
- Significant increase in body temperature.
- Feverish syndrome.
- Progressive jaundice of the skin.
- Severe form of hepatomegaly.
With chronic toxic damage, pain periodically occurs on the right side, body temperature rises to 37 degrees, and dyspeptic disorders are present. Such signs disappear during remission and reappear during exacerbation.
Treatment methods
Treatment of toxic hepatitis involves eliminating the provoking factor, dietary nutrition, and the use of hepatoprotectors - a group of drugs that help restore the liver and accelerate regeneration processes. Representatives: Heptral, Karsil, Essentiale Forte.
Diagnostics
If you find any of the listed signs, you must have your liver examined. Modern medicine has a whole arsenal of tools and methods for detecting liver diseases. All methods of examining a patient can be divided into general clinical, instrumental and specific.
General clinical examination methods include:
- general blood analysis;
- blood chemistry;
- general urine analysis;
- coagulogram;
- liver tests, etc.
By analyzing the patient’s blood, you can determine with maximum accuracy the presence of the disease, its type, viral nature, and obtain other important information. Liver tests can show the degree of liver dysfunction.
The main instrumental methods for studying a patient’s liver can be named:
- Ultrasound of the diseased organ;
- MRI or CT;
- liver biopsy;
- diagnostic laparotomy, etc.
Using instrumental methods for examining the organ, it is possible to obtain accurate and complete information about the actual size of the liver, the presence of any changes, damage and compactions. A liver biopsy will not only determine the extent of damage to the organ, but also establish the cause.
Especially for viral, autoimmune hepatitis, more labor-intensive and expensive, but ultra-precise, specific research methods can be used:
- PCR;
- RIA;
- XRF;
- ELISA, etc.
Based on diagnostic findings, a qualified doctor will be able to determine the type of hepatitis and draw up the correct effective treatment regimen, and make a prognosis of the outcome of the disease.
Autoimmune hepatitis
Autoimmune hepatitis is understood as a progressive and chronic inflammatory process in the liver, which occurs with signs of extensive damage to the organ, the presence of autoantibodies to the gland’s own cells. In the structure of hepatitis, autoimmune forms account for about 10-15% of cases.
Women are diagnosed with the disease 8 times more often than men. The course of the pathological process is characterized by a rapid nature, in which serious complications develop relatively early - portal hypertension, cirrhosis, hepatic cell failure.
The etiology of the disease is not fully understood. The basis of genesis is a lack of immunoregulation. Depending on the antibodies produced, the following types of autoimmune hepatitis are distinguished:
| Type of disease | Description |
| First type | Most often found in patients 10-20 years old and after 50 years of age. The prognosis is favorable, since in 90% of cases immunosuppressive drugs help, which allows achieving stable and long-term remission. If there is no therapy for 3 years, cirrhosis of the liver develops. |
| Second type | Type 2 is characterized by high biochemical activity and manifests itself in childhood. The response to immunosuppressive treatment is insufficient; when medications are discontinued, a relapse of the disease is quickly detected. According to statistics, with this type, cirrhosis develops several times more often. |
| Third type | In type 3, the presence of rheumatoid factor and antimitochondrial antibodies is determined. |
Manifestations in children and adults
The disease manifests itself suddenly, the clinical manifestations are practically no different from the signs of acute viral diseases. At first, patients complain of severe weakness, loss of appetite, and intense jaundice.
After 1-1.5 months, symptoms appear:
- Pain in right side.
- Skin itching.
- Nausea, vomiting.
Against the background of pathology, the liver and spleen enlarge. The autoimmune process in 50% of cases occurs along with other diseases - myocarditis, type 1 diabetes mellitus, vitiligo, Sjögren's syndrome.
Diagnostics
The criteria for the disease are biochemical, serological and histological markers detected. An autoimmune form of pathology is said to exist if the following criteria are present:
- If the patient has not taken hepatotoxic medications, there is no alcohol dependence.
- When there are no markers of viral pathogens in the blood.
- The concentration of γ-globulins and IgG is higher than normal.
- AST and ALT are above normal.
- Antibody titers (SMA, ANA and LKM-1) for an adult from 1:80; for a child from 1:20.
A biopsy is required. Using manipulation, a chronic disease with signs of pronounced activity is diagnosed. Histology shows stepwise or bridge-like necrotic transformations and lymphoid infiltration.
Therapeutic strategy
Doctors prescribe immunosuppressive treatment. Thanks to this, the activity of destructive processes in the gland is reduced, the intensity of T-suppressors is increased, and autoimmune reactions that provoke the destruction of liver cells are eliminated.
Prednisolone is usually used in a dosage of 60 mg (first 7 days), 40 mg (next 7 days) and 30 mg (3-4 weeks). As a maintenance dosage, it is recommended to take 20 mg every day. Reduce the dose slowly, taking into account the clinical picture and the concentration of autoimmune markers.
Without therapy, the disease progresses and spontaneous remission is impossible. Pathology leads to liver cirrhosis and hepatocellular failure. With adequate treatment, the ten-year survival rate is over 80%.
Serious complications
If hepatitis is untimely or incorrectly treated, there is a high probability of various complications that can lead to death of the patient. The most common complications include:
- acute liver failure;
- liver cancer;
- cirrhosis of the liver;
- portal hypertension;
- hepatic coma, etc.
https://youtu.be/tUPXWPrqFaw