Who should have a mammogram?
Many formations in the female breast do not manifest themselves in the early stages.
Mammography can detect cysts, fibroadenomas, calcifications, and cancer. Early diagnosis of cancer is important and has saved the lives of thousands of women aged 40 to 49 years. A tumor detected in a timely manner offers a greater chance of recovery without surgery or chemotherapy. The most common question concerns age restrictions and frequency of passage. If you are concerned about any health problem, sign up for a diagnosis. The success of treatment depends on a correct diagnosis.
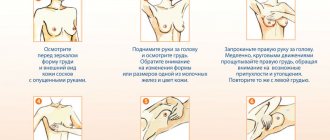
An annual mammogram can detect cancer at an early stage. Therefore, doctors advise regularly undergoing this medical examination. This procedure is especially relevant for women over 40 years old. At this age, hormonal changes begin that can lead to abnormalities in the breast tissue. You should definitely undergo the procedure if:
- there is discharge from the nipples;
- lumps and chest pain appeared;
- deformation of the shape of the breast or nipples has occurred.
Mammography is a diagnostic procedure that is necessary to assess the patient’s condition. After 35 years, it is mandatory for all women. It is enough to undergo the procedure once every 2 years to identify tumors. After age 50, mammograms are performed annually.
If there is a genetic predisposition (there have been cases of breast disease in the family), you should undergo mammography from the age of 30.
If malignant tumors are detected, the procedure must be done once a month. It will allow you to trace the dynamics of the development of formations.
What is mammography and what does it show?
There are types of examinations that need to be completed regularly, especially after reaching a certain age. For women, this is an examination of the mammary glands to identify possible pathologies.
Usually, one of the methods is chosen for the procedure - ultrasound or mammography, that is, examination of the breast using an X-ray machine - mammograph. The procedure is an x-ray examination with the results recorded in the form of an image, computer recording or other method.
It is necessary to be examined for the timely detection of possible tumors in the breast. These formations can be either benign or malignant. But the success of oncology treatment depends directly on early diagnosis.
Identifying the problem at an early stage allows you to avoid surgical intervention even when treating malignant tumors.
Is mammography dangerous? Since this is still an X-ray examination and there is radiation, then yes, of course, mammography is harmful to health, but due to the fact that the radiation dose is only 0.1-0.2 Rad, it is believed that it is small for the development of oncological tumors. And the benefits from it are incomparably greater than the potential harm.
Mammography today
The purpose of mammography is to diagnose and study a wide range of diseases affecting breast tissue.
Currently, mammography is successfully developing: new technologies are being introduced, the range of diagnostic capabilities is expanding, and advanced equipment is being used with minimal radiation exposure to the body.
The capabilities of mammography have expanded significantly in recent years due to the emergence of new types of research: digital, optical, microwave, magnetic resonance methods.
conclusions
Today, mammography is one of the most accurate ways to detect tumor formation in the breast. Mammography makes it possible to obtain the maximum amount of information about the condition of breast tissue.
When comparing mammography with ultrasound and other modern research methods, many experts agree that the effectiveness and reliability of mammography results is much higher.
Is the procedure harmful?
Breast implants are a contraindication for mammography
Mammography can detect cancer 1-2 years earlier than a doctor can do by palpation and examination of the patient. The examination is indicated for patients aged 40-45 years. Contraindications to a mammogram are:
- The woman's age is up to 40 years. This is explained by the fact that young breasts are denser than those of older patients. Therefore, malignant formations are less visible on it.
- The mammary gland is too small, which makes it difficult to fix it in the plates of the device.
- Pregnancy and lactation period. Even minimal doses of radioactive radiation can harm mother and baby, as with fluorography.
- Presence of implants in the mammary gland.
An X-ray examination can be done to determine breast cancer (breast cancer) in public medical institutions or in private clinics. The accuracy of the results is guaranteed. But the price of the service in private centers will be slightly higher than in public clinics. It is advisable to find out about it immediately when registering for the procedure.
The role of mammography in the diagnosis of breast cancer cannot be underestimated.
More precisely, whether mammography is harmful to the body, in principle, everyone will decide for themselves, weighing the benefits and harms. The radiation dose is less than during fluorography. After the introduction of mandatory screening, mortality from breast cancer among women aged 40-55 years decreased by 1/3. At this age, the risk of the disease increases every year and the question of whether it is harmful to do it every year disappears by itself.
How many times a year is it recommended to undergo examination after 50 years? Once every six months. On what days of the cycle should screening be done? It is better to do it during the cycle from days 5 to 10, the deadline is 12 days from the start of menstruation. After menopause, you can do it any day. The timing of the monthly cycle was chosen for a reason.
During this period, the hormonal levels are stable and women do not experience pain, the milk ducts are not enlarged, there is no swelling. Before and during menstruation, any manipulation brings discomfort. Since the procedure involves compression of the mammary glands, this factor is important. In case of an emergency, diagnosis is carried out at any time and the frequency of examination is determined by the doctor.
The procedure is indicated not only for diagnosis, but also for the purpose of assessing the effectiveness of treatment, as well as taking a puncture. In oncology, the doctor decides how often mammography of the mammary glands can be done, taking into account the patient’s condition. After receiving a referral, women want to prepare themselves mentally and learn how a mammogram is performed.
The diagnosis is carried out by a radiologist or mammologist. You don’t need anything with you, food intake is not limited by diet or time frame. The only recommendation from doctors is not to drink energy drinks, coffee and strong tea, as they have a stimulating effect on the emotional state.
Excitement and anxiety during the process increases the perception of pain. Before a mammogram, you should not apply creams, lotions or other cosmetics to the chest and armpits. It is also recommended not to use deodorant, as the substances included in the composition may appear as darkening, thereby distorting the examination result.
Many people do not understand which mammography is better: digital or x-ray. Both are suitable for screening – they are analogous. The advantages of digital mammography include advanced data processing capabilities. The image can be reconstructed, zoomed in, enlarged, increased in clarity, that is, studied in more detail.
In addition, information in electronic format is easier to store and archive indefinitely. Possibility to send to other medical institutions for consultation with doctors via the Internet. The second advantage is the reduction in radiation exposure. The disadvantage of digital mammography can be considered the cost of diagnosis in comparison with film radiography.
Also, digital media is not a document, unlike X-ray film. This inconvenience is faced by people who need to provide research results in court or for a commission in order to confirm their disability. We figured out how digital mammography differs from conventional mammography and how it can be replaced.
Since women receive the results of the examination almost immediately, after reading some of the conclusions they become prematurely frightened and begin to worry. The situation may not be dangerous at all, for example, a diagnosis of fibrofatty involution. Reduction, that is, the loss of the intended function of the female breast, involves the replacement of muscle tissue of the breast with fatty or fibrous tissue.
This process occurs as menopause approaches. The bust loses its shape, the skin wrinkles and loses its elasticity. Such a change is not a disease if detected after 45 years. This is a physiological process that, unfortunately, is irreversible. If fibrofatty involution is detected in a young girl, then this is considered a pathology and requires treatment.
The cause is a hormonal disorder that can be treated with medication. Another diagnosis that occurs quite often is stromal fibrosis. One of the three components of mammary gland tissue is connective; in the breast it is called stroma. The growth of the stroma threatens the replacement of glandular tissue and adipose tissue.
This pathology is not dangerous, however, it can result in complications, discomfort and pain for the woman herself. Therefore, if stromal fibrosis is detected, it is better to contact a mammologist without letting your health take its course. Of the neoplasms in the mammary gland, the most famous are fibroadenoma and cyst. These formations themselves are benign and appear on a mammogram with a clear, even outline.
In the case of blurred boundaries, the study is carried out in more detail, as this is one of the signs of a malignant tumor. Sometimes they ask why fibroadenoma is not visible on mammography? As a rule, fibroadenoma is well diagnosed, but there are circumstances that affect the informativeness of the diagnosis.
The formation may be too small and difficult to differentiate among healthy tissue. It may also be due to high levels of sex hormones or too dense muscle structure at a young age. In any case, if the presence of a formation is suspected, the doctor will prescribe additional examinations.
If you have questions or doubts about the diagnostic results, do not hesitate to ask your doctor. If the answer is unsatisfactory, you have the right to contact another specialist and undergo the study again, possibly in another place. Women's health is sensitive to stress, anxiety and stress.
This article is posted for educational purposes only, does not replace an appointment with a doctor and cannot be used for self-diagnosis.
Mammography can detect benign and malignant neoplasms. The procedure allows you to analyze changes in the mammary gland, their size and distribution.
- Cyst. This fluid cavity is a common occurrence in the mammary glands. It is not a cancerous disease. But mammography, unfortunately, does not allow distinguishing a cyst from a malignant tumor - further examinations are needed.
- Fibroadenoma. Tumor-like formations that are subject to growth. More common in young women. They are not malignant.
- Calcifications. Small, numerous accumulations of calcium salts in tissues can be the first sign of the initial stage of cancer. Large lesions are most often not associated with cancer. However, the presence of calcifications in the mammary gland may be due to the presence of an oncological process.
Even if there is a lump on only one side, both mammary glands are examined. This is done for comparison pictures and to identify changes in the other breast. If you have pictures of past procedures, you need to show them to the radiologist.
Breast mammography is an X-ray with a small dose of radiation. Therefore, doctors do not recommend it:
- pregnant women;
- nursing mothers.
Before the procedure, patients ask: “Is mammography an ultrasound? How is the examination going?” Both methods do not require special training from women. X-ray examination differs from ultrasound examination.
Ultrasound allows you to monitor the condition of soft tissues. And visualization of dense ones is better diagnosed on mammography. Therefore, if the patient’s condition is of concern, then both examinations are prescribed.
X-rays pass through the human body, capturing the image on a special film. Mammography is a procedure that is performed on an outpatient basis. The radiologist places the patient's breast on the platform and fixes it. Several pictures are taken (top to bottom and side), during which the patient changes position.
For a clear image, the woman should freeze and hold her breath. The principle of the procedure is reminiscent of fluorography. But, unlike her, the radiologist takes pictures of each breast separately. During the procedure, the breast is slightly compressed by the device. Why is this being done?
- To even out the thickness and unevenness of the breast.
- To get a clearer image.
- To distribute the soft tissue, visualizing compactions and possible formations.
- To reduce the radiation dose - the smaller the tissue layer, the less dose it requires for a full image.
After receiving the images, the radiologist analyzes them and provides documentation to the attending physician. In some cases, mammography descriptions are received in person. Based on the results of the procedure, the attending physician may prescribe additional examinations to clarify the details of the diagnosis.
Some patients, due to their incompetence, claim that mammography is harmful. Allegedly, the radiation dose is high, so it is better to do an ultrasound. Doctors assure that if the standards for conducting x-ray examinations are followed, the damage to health will be minimal.
What is mammography?
Mammography is a non-invasive screening method for examining the mammary glands, which is based on X-ray radiation.
This type of research is accessible and at the same time highly informative, and also cost-effective. It is used quite often and can detect cancer pathology in the early stages of manifestation.
The essence of mammography
The essence of the method is that body tissues have different sensitivity to X-rays.
Thus, bone tissue has a high absorption capacity, while fat, muscle and other tissue transmit almost all radiation.
Therefore, during an X-ray examination, you can see an image that is based on the difference in resistance of various tissues.
The same applies to the mammary gland, since it contains skin, adipose and glandular tissue, as well as glandular ducts, it must be concluded that scanning produces an image with different media resistance.
Tumor tissue, when formed in the mammary gland, usually has a greater absorption capacity compared to fatty and glandular tissue, so using this method you can see it, determine its size, as well as its structure and the presence of an additional shadow.
The method also displays an enlarged lymph node, which is characteristic of oncological pathology.
It should be noted that in addition to malignant neoplasms, mammography also reveals benign manifestations, the most common of which are fibromas, lipomas, as well as bush-like changes and calcifications. In most cases, benignity is easy to distinguish from pathology.
The method does not diagnose deeper tissues, this is due to the technical features of the method.
Indications for mammography
It should be noted that this method is used for early detection and rapid diagnosis of mammary glands, therefore, without indications, it is performed on all women starting from 40 years of age, and subsequently the frequency increases. But even at a young age there are recommendations for carrying it out.
Whenever such symptoms are detected, an examination should be performed.:
- Pain in the breast area, regardless of its nature. It can be periodic or constant, and also depend or not on the menstrual cycle.
- Detection of compaction in tissue. In this case, localization, size, shape and other indicators do not matter. As soon as the doctor palpates a suspicious area that differs in density from the main gland tissue, it is recommended to undergo this examination.
- The shape and size of the nipple changes. In this case, the manifestations can be very different, but some of the most dangerous are nipple traction, wrinkling, sharp decrease or, conversely, increase, regardless of age. These symptoms are most dangerous in women during menopause.
- Changes in shape, symmetry , as well as disruption of the normal contours of the gland.
- The appearance of discharge from the nipple , especially if the woman is not pregnant and is not breastfeeding. The most dangerous are considered to be purulent discharge or mixed with blood. The consistency is also alarming; under no circumstances should there be a heterogeneous consistency of the discharge.
https://youtu.be/FGOQEwsh3Mk
When should you have a mammogram?
Since the mammary gland is a hormonally dependent organ, a study such as mammography should be carried out taking into account the woman’s cycle.
The time for the procedure is selected strictly individually, it depends on the woman’s age, as well as the duration of her menstrual cycle:
- If it is necessary to urgently obtain a result, or the dynamics of the process are being studied, then it is required to be carried out regardless of the day of the menstrual cycle. Mammography is contraindicated for pregnant and lactating women, this is due to the fact that X-rays have a negative effect on the fetus, and the quality of breast milk also deteriorates. If absolute indications are identified, a study is required regardless of the condition. In this case, you should pay attention to the fact that it is necessary to eliminate as much as possible a negative condition in pregnant women on the development of the child. In the early stages of pregnancy, it is better to delay the time at which the formation of the internal organs and skeleton of the child occurs. Protective equipment is used to conduct the study.
- During the menopausal period, as well as in case of disruptions in the menstrual cycle, the study is carried out regardless of the period. Even if abnormal bleeding is noted, testing can be done at this time. If a woman has a regular cycle and a short duration, then the greatest information content of this method will appear in the first 3-5 days. In subsequent days, the procedure will be less informative.
- With a normal length of the menstrual cycle within four weeks, the timing shifts. In this case, the examination is carried out in the time period from six to twelve days after the onset of menstruation. Accurate timing is important to maximize the quality of the examination. The mammary gland is the most relaxed, this is due to the fact that the amount of estrogen is the most increased.
- With an extended menstrual cycle , which exceeds 35 days, the timing changes. Mammography is performed no earlier than the tenth day, but no later than the eighteenth day. It is important to conduct research before the onset of ovulation, this is due to the fact that after it progesterone begins to be produced, leading to compaction in the gland tissue.
Procedure for performing mammography
No additional preparation is required to perform a mammogram.
To perform it, a woman just needs to go to a clinic or private clinic for a mammography room, sign up on the day of the cycle, which is selected by a specialist, if the woman is menstruating, or on any day after menopause.
Order of conduct:
- Before scanning, it is necessary to create sufficient compression of the breast so that the maximum amount of its tissue is included in the overview image.
- The organ is placed on a special installation, after which light pressure is applied from above. Next, X-rays are transmitted.
Often, only two projections are enough to obtain an adequate picture: direct and lateral. If necessary, you can use a scythe if the suspected outbreak is located in areas that are poorly visible using the previous ones.
If diagnosis is very difficult, or it is difficult to describe the identified formation, a targeted image with diagnosis of a specific area is required.
Some medical institutions have mammographs, which, in combination with scanning, carry out targeted puncture of the formation. This way you can most accurately obtain the required material and send it for cytological and histological analysis.
How often should you have a mammogram?
A big issue for many women is determining the frequency of mammography. The World Health Organization has established the following order.
Thus, women under 35 years of age are not recommended to undergo examination at all, unless there is a suspicion of cancer after an ultrasound examination.
In the presence of a family history, especially breast cancer, a woman should undergo examinations from the age of 35. The frequency should not exceed one examination every two years.
After 40 years, it is recommended to undergo more frequent examinations; annual examinations are already recommended at this age.
After reaching 50 years of age, a woman undergoes this procedure twice a year.
If necessary, the frequency of mammograms per month can be quite high; the level of x-ray load allows up to 5 scans.
Is it possible to combine mammography and other studies?
Many women are concerned about the issue of combining mammography and other diagnostic methods.
In order to obtain a more accurate result, mammography is often used with additional studies.
Therefore, even on the day of performing an X-ray scan of the breast, you can resort to other diagnostics.
Also, taking into account the dosage of the x-ray load, you can also use scanning of other organs, for example, perform fluorography.
The restriction is introduced only for women who are currently pregnant or during lactation. In some cases, it is recommended to delay additional diagnostics due to the patient’s severe physical condition.
Mammography results
This method allows you to diagnose formations of both benign and malignant nature.
Among them, the following are the most common:
- Calcifications. This is a grouping of calcium salts in breast tissue. This may be one of the indicators of the onset of malignant growth in tissues. The sizes are usually not large, so it is impossible to see them with the naked eye, as well as to feel them. Determining their number, size and places of accumulation is of great importance. If necessary, additional diagnostic methods are carried out. Scan-based puncture biopsy has a high diagnostic value. With large sizes, the risk of a malignant process is low, while with multiple small formations, the likelihood of developing oncology is high.
- Fibroadenomas. These are formations that have a round shape, which represents a tumor-like structure. Its main difference is the composition of the cells; they are benign in nature. Often these cells have the ability to grow. If one is diagnosed, the tissue requires mandatory removal.
- Cystic formation. This is an encapsulated tumor with thin walls. There is a low percentage of this process transitioning to cancer. In most cases, additional use of ultrasound may be required.
- Malignant process. In this case, the signs can be completely different, which are most often characterized by uncontrolled cell division. The great danger of leaving the formation unattended is the risk of metastasis of the lesion to nearby tissues.
In addition to these formations, the doctor may suspect many other processes occurring in the woman’s body. Very often it is possible to identify pathology of the vascular part of the mammary gland, as well as hormonal dysfunction.
For an adequate picture and interpretation of the image, the presence of blood vessels, milk ducts, and lymph nodes is required. The latter are not normally visible.
In modern mammology, there are certain standards by which one can judge the quality and completeness of the clinical picture in order to make a conclusion.
There are seven assessment categories in total:
- Non-indicative assessment , in which it is impossible to draw a conclusion about the pathological process.
- Negative. In this case, the possibility of a woman having a malignant neoplasm is completely excluded.
- Detection of formations of a benign nature in tissues , but there is no malignant process.
- Identification of a benign formation that requires additional diagnostics. In this case, you may need to repeat the study in a few months, as well as register with a mammologist with regular examinations for two years.
- Identification of compaction that creates a suspicious picture of the process. In this case, the process is most often benign, but a biopsy is required to complete the picture.
- Identification of a suspicious tumor that has a high probability of malignant growth. All women with this picture undergo a biopsy of the lesion.
- Confirmed malignant process in the mammary gland . Mammography is only a dynamic study.
Mammography equipment
A modern mammography complex includes:
- mammograph,
- digital detector,
- laboratory assistant workstation,
- doctor's station
- Printer.
Today, analog (film) and digital mammographs are used. Analog equipment is cheaper, but has a number of disadvantages. Firstly, eliminating the possibility of editing the resulting image, further processing it and transferring it to other media. Secondly, a high radiation dose.
Digital mammographs are modern equipment that has much more image processing capabilities. At the same time, the radiation dose is significantly lower.
Types of mammography
There are 2 types of X-ray mammography according to the research method:
- Film.
- Digital.
Film mammography (from the Greek mamma - “mother” and grapho - “to draw”) has been used since the 60s of the last century. The image in this method is recorded on film.
In recent years, digital mammography has become increasingly popular. It allows a more detailed examination of a woman’s mammary glands and reduces radiation exposure to the body.
Depending on the purpose, there are 2 types of mammography:
- Preventive (prescribed by the attending physician when the patient reaches a certain age).
- Diagnostic (prescribed if a neoplasm is suspected).
The Importance of Mammography
Diagnosis is carried out in an x-ray room; the procedure lasts about 15 minutes. In the office you must undress from the waist up and remove jewelry. The breast is tightly compressed with holders to improve visualization and reduce radiation exposure. When the cycle is taken into account, the process is painless, although unpleasant.
Pain may occur with mastopathy or if the breasts are small. How is mammography done for small breasts? Outdated X-ray machines do not have the technical ability to record a small mammary gland, but modern mammographs are able to take a photo without contact. Another category of women is interested in whether it is possible to do an X-ray examination with breast implants?
Theoretically, the procedure is possible, but if the implant is installed above the pectoral muscle, it blocks the view of a quarter of the breast. If it is installed under the muscle, then almost the entire gland is visible. However, doctors recommend undergoing a preventive examination using an MRI. If a woman comes to check the integrity of the implant, then digital mammography will be uninformative.
Today, we have access to wide diagnostic opportunities that give us a chance to live a healthy, long life. It is in our best interests to listen carefully to our body, conduct an examination and pay attention to changes. Contact a mammologist if you have the following symptoms: the appearance of discharge from the nipples, a change in their shape;
pain in the mammary gland regardless of the menstrual cycle; if lumps are detected in the chest. Noticeable deformation of the mammary glands or nipples is also a reason to consult a doctor. Please note that if a lymph node is found during a mammogram, if a lump or the presence of a tumor is found, the final diagnosis will not be made immediately. First, this formation is further examined or supplemented with other diagnostics.
Another question that doctors are often asked: is it possible to do x-ray mammography while breastfeeding? There are two absolute contraindications for digital mammography: the period during lactation and the woman’s pregnancy. If it is necessary to examine the mammary glands for pregnant or lactating women, an alternative to mammography is breast examination using ultrasound, the method or electrical empidans. We have figured out how mammography of the mammary glands is done, now we will discuss the issue of preparation.
Mammography is the most informative method for diagnosing breast cancer. With its help, you can see the slightest pathological changes in tissues and formations at any stage of development.
Mammography helps detect tumors early and thus reduces breast cancer mortality by 15 percent.
Through mammography, it is possible to determine the form of pathology and understand the cause of many complaints and symptoms.
Using mammography, a doctor can diagnose diseases such as:
- fat necrosis,
- hyperplasia,
- cyst,
- mastopathy,
- fibroadenoma,
- radial scar,
- intraductal papilloma,
- cancer.
For non-palpable formations, mammography plays a vital role, since only with the help of this method will it be possible to establish a reliable diagnosis.
Mammography – when to do it
Mammography is classified as a planned preventive research method.
In this regard, breast mammography is recommended for all women after 40 years of age every two years (in the presence of benign tumors in the mammary glands - once a year). After age fifty, it is recommended to have a mammogram once a year. According to indications, mammography is performed more often.
Additional indications for performing mammography include identifying the following in a patient:
- deformations of the nipples and breasts;
- changes in breast size (without visible weight gain or loss);
- changes in the color of the mammary glands and nipples;
- pathological discharge from the breast (purulent, purulent-bloody, bloody-serous, etc. discharge) when pressing on the nipples or when stains from discharge are detected on the underwear;
- pain on palpation in the mammary gland;
- seals and nodes in the mammary glands, etc.
Also, mammography can be prescribed after surgery on the mammary glands to monitor the effectiveness of the quality of treatment.
Before a mammogram, it is recommended to be examined by a mammologist.
How to prepare for a mammogram
Before the procedure, anxious women often ask: “Does mammography hurt or not? How will I feel? Mammography is an absolutely painless procedure. It lasts about 10–30 minutes. Before the procedure, the doctor will tell patients on what day the mammogram is done. However, for urgent diagnosis, the day of the cycle is not important.
Some women may experience discomfort during the examination if they experience chest pain. Therefore, on the recommendation of a doctor, they may be prescribed painkillers.
Jewelry should be removed during the procedure. The individual characteristics of patients will be fundamental to calculating on what day a mammogram is done. Usually this is 6-12 days from the start of the cycle.
If you have breast implants, you should tell your doctor. On the day of the procedure, you cannot use deodorant or cream. The armpit and chest area must be clean so that darkening does not appear on the film.
Contraindications
Despite the fact that the method is quite informative and accessible, it has certain limitations for its implementation:
- So an absolute contraindication is during pregnancy. This is due to the fact that to scan the gland, a dose of x-ray radiation is applied to the tissue. When exposed to the fetus, a negative effect may occur with disruption of the formation of organs and systems. In the short term, this can lead to spontaneous miscarriage. The screen cannot always act as protection.
- Suspicion of pregnancy should also be considered one of the contraindications. To do this, you either need to wait until your menstruation period or conduct additional tests, such as a laboratory test for human chorionic gonadotropin.
- In addition, mammography should not be performed during breastfeeding. In addition to the negative impact on gland tissue at this time, there is also a violation of the interpretation of the results obtained. In some cases, you can get a false positive result.
- This procedure should be avoided if there is a skin defect both on the body of the gland and in the nipple area. If there is no oncological suspicion, it is recommended to postpone this study until healing occurs.
Relative contraindications should be considered:
- Six-month period after termination of pregnancy.
- The woman is young; up to the age of 35, a woman is examined only if there is a suspicion of cancer.
- Surgical interventions on the organ with the installation of various types of implants . In this case, diagnostic significance is lost.
Problems of modern mammography
Many modern mammographs used today in specialized centers and multidisciplinary clinics can operate with reduced radiation exposure.
Mammography Safety
Despite the advent of modern equipment with minimal radiation doses, mammography is not becoming a completely safe procedure. Negative effects on the body during mammography cannot be completely excluded.
The modern task is to create the necessary and maximally safe conditions for conducting research, reducing the risk of possible complications for the health of patients and medical personnel.
Discomfort during mammography
Another problem is the discomfort that some patients experience during the study.
To obtain a high-quality image, the mammary gland must be tightly compressed with special plates, so with certain types of diseases women may experience pain and severe discomfort.
Modern technologies can reduce compression of the breast during mammography. Manufacturers have recently increasingly produced mammographs with this function.
Ultrasound or mammography
Both ultrasound and mammography are equally accessible and informative in modern medicine. It is difficult to talk about the greatest diagnostic significance of any of them. For the best effect, it is recommended to carry them out in combination.
Since breast cancer has a steady decline in age and mammography has limitations, it should not be performed before age 35. Therefore, the only informatively significant method for diagnosing pathology during this period is ultrasound scanning.
In some cases, these methods alone will not reflect the real extent of the pathological process, but in combination the likelihood of detecting pathology increases.
There are rare cases of insufficient information content, for which a study using a computed tomograph is used.
Types of research
Analog X-ray diagnostics are still performed today, although they have long been inferior to digital mammography. During this study, a projection of X-rays is created onto the film. A specialist can study images of tissues only after special processing.
The image cannot be edited or sent by mail to other clinics. This is a disadvantage of analog mammography, although film mammographs are considered budget (compared to digital equipment).
Digital mammography is the most modern diagnostic method used to prevent pathologies, detect tumor formations and control their development.
Images are output to a computer, can be further processed, and can be edited and transferred to any media. Among the advantages of digital mammography, it is also important to note the reduced radiation exposure.
Digital mammography with tomosynthesis is a unique method that allows you to diagnose pathologies by comparing a series of mammograms in different projections.
Layer-by-layer imaging of breast tissue makes it possible to determine the nature of the contours. Mammographs with tomosynthesis technology allow diagnostics even with high density of breast tissue.
Mammography with a biopsy attachment for conducting targeted studies and further studying the histogenesis of tumor formations.
Optical mammography is a new research method based on infrared radiation and allows to identify benign and malignant tumors, calcifications, and other formations in the mammary glands.
It is also common to consider several types of optical mammography.
Projection optical mammography involves studying a series of images in two projections. Based on infrared laser energy.
Tomographic optical mammography allows you to obtain a three-dimensional image of the breast to determine the exact localization zone of the formation, its type and other features.
Luminescent optical mammography is a technique using special substances that improve the visualization of metastases during the study.
Magnetic resonance imaging (breast MRI) most often involves the use of a special contrast agent to improve tissue visualization. It is believed that this method is one of the most informative.
Radiothermometry is a microwave method for assessing the temperature of breast tissue fibers. Allows you to detect pathological changes at any stage of development. Often combined with mammography.
What does the procedure reveal?
Mammography can detect benign and malignant neoplasms. The procedure allows you to analyze changes in the mammary gland, their size and distribution.
- Cyst. This fluid cavity is a common occurrence in the mammary glands. It is not a cancerous disease. But mammography, unfortunately, does not allow distinguishing a cyst from a malignant tumor - further examinations are needed.
- Fibroadenoma. Tumor-like formations that are subject to growth. More common in young women. They are not malignant.
- Calcifications. Small, numerous accumulations of calcium salts in tissues can be the first sign of the initial stage of cancer. Large lesions are most often not associated with cancer. However, the presence of calcifications in the mammary gland may be due to the presence of an oncological process.
Even if there is a lump on only one side, both mammary glands are examined. This is done for comparison pictures and to identify changes in the other breast. If you have pictures of past procedures, you need to show them to the radiologist.
How to prepare so that you don’t have to repeat the procedure?
For mammography, the day chosen for the procedure is important. All experts are clearly inclined to believe that it is optimal to carry out the procedure on days 5–12 of the menstrual cycle, since during this period the results are the most informative.
And also the mammary glands at this time are in a relatively calm state - not painful and not enlarged, which will relieve the examinee from discomfort during diagnosis due to chest pain that appears in other phases of the cycle. No special preparation is required for this study.
There are a few points to consider:
- on the day of the procedure, do not use antiperspirants for the armpit area and creams for the chest and armpits;
- notify your doctor about the timing of your last menstruation;
- remove all jewelry and undress to the waist.
A woman must inform her doctor about pregnancy or breastfeeding, since in this case mammography is contraindicated and is not informative. The diagnostician, in turn, must explain to the examinee about the possibility of obtaining false results that require re-testing.
Carrying out the examination at the right time during the cycle will save the patient from discomfort and having to undergo a repeat procedure.
How to do a mammogram correctly
Mammography is done according to a standard scheme, usually consisting of the following stages.
- The patient is escorted to a specially equipped room.
- Depending on the parameters of the mammograph and the purpose of the study, the woman takes a lying or sitting position.
- In order to protect the genitals, the abdomen is shielded, that is, covered with a lead apron.
- The mammary gland is located on a horizontal plate, under which there is an X-ray emitter. It is fixed at the top by a second plate, which presses the chest and increases the viewing area.
- The resulting image is displayed on film; if a digital mammograph is used, then on the matrix.
- If necessary, photographs are taken in several projections: frontal, lateral and oblique.
- Similar actions are performed with the second breast.
- If there is insufficient data after an X-ray examination, another form of diagnosis may be prescribed.
The duration of the procedure is about 20 minutes. Immediately after its completion, the client is given a description of the mammography.
Patients with breast implants are diagnosed by specialists with appropriate qualifications and experience.
https://youtu.be/PeBezZv5Oso
With old-generation X-ray machines, if a woman had small breasts, it was difficult to conduct a full examination. This problem does not exist with modern mammographs. They allow you to take a full-length informative photo in a side projection.
Survey results
The most expected mammogram result is negative. This means that no abnormalities were found in the mammary glands. A positive result indicates that pathological formations have been identified in the breast. In this case, you will need to undergo an additional examination: perform a targeted mammography, which allows you to obtain a more detailed image of the area of interest to the doctor.
If the presence of a tumor is confirmed, you will be prescribed a puncture biopsy of the breast. Under ultrasound or X-ray guidance, the doctor will use a thin needle to remove a small area of tumor tissue for histological analysis. It is the pathologist who will make a conclusion about the nature of the tumor process, since it is impossible to accurately determine the nature of the tumor from a mammogram.
Unfortunately, with mammography, as with any other method, diagnostic errors are possible. False positive result – something that is not there is detected. A more in-depth examination does not confirm the presence of a tumor.
False negative result – the existing tumor is not detected. In what cases is this possible? The accuracy of mammography in detecting tumor processes reaches 70-80%. However, the likelihood of error increases with high breast tissue density, as well as with breast implants.
When should diagnostics not be carried out?
Since mammography is an X-ray examination in which the patient receives a small dose of radiation exposure, its contraindications are similar. There are two types of contraindications.
Absolute contraindications are pregnancy and lactation
Relative:
- violation of the skin of the breast and nipples;
- presence of implants;
- age up to 35 years;
- less than six months after termination of pregnancy.
In case of the latter contraindications, the decision on the need for mammography is made by the doctor, weighing the possible risks and the usefulness of the data obtained for making a diagnosis.
Detected pathologies
Using digital mammography, it is possible to identify the following pathological conditions: malignant neoplasms, calcifications, which appear as accumulations of salts. Sometimes they are a sign of early stage cancer. Most often, these formations are not palpable during the examination. During the study, the size and shape of calcifications are determined.
Cystosis is diagnosed. Breast cysts appear as a cavity with thin walls that contain fluid. This is a common type of pathology that is rarely associated with the development of cancer. You can also detect fibroadenoma, which is represented by mobile tumor formations formed from healthy breast cells.
Preparing for the study
To take a high-quality photo, you must follow certain rules:
- on the day of diagnosis, you cannot use cream, perfume, deodorant and other cosmetics;
- before the procedure, you should remove jewelry that falls into the field of study;
- a week before the diagnosis, you need to give up coffee, as it has a diuretic effect, causing the gland tissue to thicken;
- The day before you need to take a pregnancy test if there is a possibility of pregnancy.
The woman should tell the mammologist the last time her breasts were examined, and also provide previous images (if available).
False negative and false positive results
Ducts and capillaries should be clearly visible on the images. If there are disturbances in the structure of the breast tissue or enlarged lymph nodes, the presence of pathology is diagnosed.
With the help of deciphering mammography of the mammary glands, it is not difficult for a specialist to determine the foci of development of a neoplasm, its quality, shape, and size.
If the outcome of the examination shows the likelihood of cancer in the mammary gland, the doctor recommends additional testing. It should be borne in mind that mammography does not always give unambiguous and correct results.
If a specialist has even the slightest suspicion of cancer, he sends the patient for additional studies. If the mammologist’s diagnosis is not confirmed, we are talking about a false-positive mammography result. In this case, the woman is considered healthy.
A false negative breast mammogram result can be due to several factors:
- The neoplasm is small in size.
- The doctor who performed the examination is inexperienced or incompetent.
- An increased level of sex hormones is observed in a woman’s body.
- A malignant neoplasm grows dynamically.
This result is dangerous because a woman may postpone a visit to a mammologist even if she has obvious symptoms of cancer. This approach to one’s health often leads to death. It is important to remember that breast mammography cannot be used to judge cancer. If undesirable symptoms are present, the woman should immediately consult a doctor for advice.
After mammography, its results are deciphered. They are of the following nature:
- If the structure of the organ, lymph nodes, ducts and vessels is uniform and there are no compactions or darkening on it, this indicates a zero probability of the presence of a pathological process;
- In the absence of a tumor, the vessels are clearly visible in the photo, and the lymph nodes are of normal size;
- With enlarged lymph nodes and a changed structure, we can talk about the presence of cancer. In addition, the doctor determines the number of pathological foci, their size, shape and location;
- If there is an oncological process, irregularities in the area of the tumor can be distinguished in the image;
- The presence of calcifications in the image indicates some kind of formation.
The conclusion is issued by a radiologist after analyzing the images obtained. Interpretation of mammography of the mammary glands takes from one hour to several days. Private clinics send descriptions by email. If the result is questionable, the doctor recommends that the patient undergo other types of examination. A woman should have a repeat mammogram in 4–6 months.
The radiologist analyzes the condition of the breast tissue, its structure, the presence of metals and calcium. In the image you can see compactions and darkening in the mammary gland, which indicate pathological processes. Vessels, ducts and lymph nodes are examined.
When decoding images, a scale is used to determine changes:
- The result does not provide information.
- Normal (no deviations detected).
- Benign neoplasm. There are no symptoms of cancer.
- Tumor. The likelihood of the lesion being malignant is negligible.
- Suspicion of cancer. Microscopic examination of suspicious tissue is needed.
- The malignancy of the tumor was confirmed.
- Monitoring cancer treatment - comparing previous and current results.
Calcifications
Calcium deposits appear on the image as white spots or stripes. Often observed after 50 years. Small accumulations, similar to grains of salt, signal the development of a cancerous tumor. Large calcifications are benign - they are found even in normal conditions.
Creams and deodorants that women apply to their skin before the test make diagnosis difficult.
Seals and lumps
The likelihood of cancer is indicated by a blurry light area with uneven borders. A round spot on a mammogram with clear contours indicates a benign lesion. A mobile lump can be easily felt when palpating the mammary gland and does not degenerate into a malignant formation.
Mastopathy is characterized by thickening of the mammary glands. In the nodular form, a cyst is formed - a cavity with clear liquid; it rarely degenerates into cancer.
Why is it needed?
Mammography is used to diagnose changes in the mammary glands. Low doses of radiation will not harm the patient's health. Minor discomfort during the procedure makes it optimal for detecting cancer at an early stage.
Finally, we list the unfavorable factors that contribute to the development of cancer at an early age:
- abortions;
- early menstruation (up to 11 years);
- hormonal changes (taking oral contraceptives, thyroid disease, being overweight or underweight);
- late menopause (after 55 years);
- first birth at a late age (after 30 years);
- gynecological diseases;
- genetic predisposition;
- regular stressful conditions.
Early diagnosis will allow you to cure the cancer completely or perform surgery with minimal damage (for example, remove only the tumor, do without chemotherapy). Regular examination will help maintain health for many years.
Features of digital mammography
In digital and film mammography, for a better image, the breast is sandwiched between two plates. Studies have shown that in 20% of cases, film examination does not detect the presence of breast cancer.
Thanks to the use of modern equipment, cancer can be recognized quickly and with high accuracy. It is for this purpose that mammography is performed - a method for examining the mammary glands, which allows identifying pathology at the earliest stages of development, and also indicates the presence of fibrocystic disease. In this case, the procedure is carried out using a special device - a mammograph, and its information content is over 90%.
Advantages of the method
- Maximum information content (90-96%);
- The optimal option for examining the mammary glands in women over 40 years of age;
- Ability to detect non-palpable tumors;
- Ability to diagnose the presence of cystic formations and calcifications;
- Determination of the nature of development of malignant formation;
- Identification of the exact location of the tumor;
- Assessing the effectiveness and correction of treatment;
- Minimum radiation dose to the patient;
- Possibility to obtain images of the breast in different projections;
- Identification of the exact causes of pathological secretion (in the case of administration of a contrast agent into the milk ducts);
- Ability to control puncture of cystic formations.
Principle of operation
This type of examination is carried out on an outpatient basis. To do this, the patient’s mammary glands are placed on a special platform and fixed. To obtain clearer results, the doctor asks the woman to hold her breath for a few seconds. Pictures are taken in different positions in order to obtain several projections of the breast.
During the procedure, the mammary glands are slightly compressed, which allows for a more even distribution of soft tissue, equalization of thickness and clearer photos.
Currently, an improved method of x-ray examination is widely used - digital mammography with tomosynthesis. The advantages of this technique include:
- Minimum radiation exposure. Due to the fact that a computer is used to transfer the resulting images, rather than X-ray film, the radiation dose is reduced several times.
- More accurate assessment of results. Digital images obtained during the study can be worked with using special computer applications. At the same time, there are ample opportunities for enlarging images, changing their contrast, improving clarity, converting, etc. Today, programs have been developed that allow you to quickly analyze the results and make a preliminary diagnosis. This has a positive effect on the information content of the survey.
- Possibility of storage on electronic media. The results of digital mammography can be stored for a long time, and can also be sent to any clinic in the world for consultation with other specialists. The ability to transfer data via the Internet allows you to control the treatment process, that is, compare the results obtained before and after it.
- It is an ideal method of breast screening, which is carried out annually.
- The ability to visualize the structure of breast tissue in three projections, which eliminates additional biopsies.
- Assessment of breast condition after implant surgery.
- Can be performed on patients with any breast size.
- Reducing research time.
The technique of mammography with tomosynthesis is similar to the standard x-ray method, but there are some differences.
Firstly, with tomosynthesis the pressure on the mammary glands is significantly minimized - it is only necessary to fix the breasts during the screening period.
Secondly, with conventional mammography, only two images are taken: in direct and oblique projection. In turn, with the tomosynthesis technique, several images are obtained from different angles.
Thirdly, pain is reduced.
Fourthly, the procedure time is significantly reduced - down to several seconds.
Diagnostic progress
Mammography is a convenient and safe diagnostic method. There is no need for preliminary preparation. Before the examination, the patient must undress to the waist.
First, the woman must remove all chains and other neck jewelry, and also stand near the device. Modern devices make it possible to undergo the examination in a supine position. However, new equipment cannot be found in every medical institution. During the examination, the woman will need to hold her breath when the doctor tells her to. Typically it takes 15 seconds to take one photo. You can't breathe at this time.
Before taking the picture, the patient must remove any jewelry from her neck.
Regardless of the lesion, both mammary glands are always examined. The examination is easier if one breast is completely healthy. In this case, any negative changes can be easily traced.
During the examination, the patient may experience minor discomfort. The chest is placed on a special plate, and the plate is pressed on top. After completing the diagnosis, the doctor takes a digital image. The doctor evaluates the received photo and reports the final diagnosis.
What is mammography and how the examination is carried out, you will learn from the video:
Preparation
How often should you have a mammogram?
- Carrying out diagnosis a week after the end of menstrual flow. Otherwise, discomfort may develop and the diagnostic algorithm may change;
- Before the procedure, you must show the doctor previous photographs, records, and medical history. This is important for assessing the dynamics of the disease;
- within 2 days it is necessary to exclude the use of products containing caffeine and energy drinks. This is due to the fact that caffeine increases susceptibility to painful sensations, negatively affects the emotional state, and enlarges blood vessels. This may negatively affect the results of the study.
You should dress for the diagnosis, taking into account the fact that during the procedure you will need to remove your outer clothing. It is important to tidy up the chest and armpit area. However, it is not recommended to use creams and lotions. This is due to the fact that the device contains metal elements that distort the examination results.
Advantages
Digital mammography has a number of advantages over standard examination. The main ones are listed below and discussed below. The most important advantage is the significant reduction in X-ray exposure. To obtain an image of high quality, 30% of the power of the rays that are used during the film method of studying the structure of the breast is required.
The result is a picture with clarity and contrast. It will become much easier to analyze. Because of this, additional diagnostics are not required. An important advantage is the increased power during the procedure to be able to detect any changes in the structure of the mammary gland.
Mammography of the mammary glands or ultrasound of the mammary glands in modern diagnostics
Breast mammography or ultrasound can correctly diagnose the condition of the breast. It is typical for the mammary glands to respond particularly sensitively to any stressful situations, hormonal imbalances and other problems in the development of various pathological conditions.
Mammography
The mammographic type of examination is preferable for all women over 45 - 55 years old. With its help, it is possible to detect at least 95% of all pathologies characteristic of the female mammary glands.
The procedure is carried out from the 5th to the 10th day of the menstrual cycle. The results obtained during this period are considered the most accurate. Shortly before the procedure, patients are warned that there should be no cosmetic or hygiene products on the area being examined.
Otherwise, the shadow from cosmetics will negatively affect the quality of the drawing. Sometimes fuzzy lines or spots can be mistaken for pathological manifestations in the tissues of the gland.
When you can't do without mammography
Which method of examination is better: mammography or ultrasound of the mammary glands, the attending physician decides on an individual basis. Typically, mammography techniques can be performed both for preventive medical examinations and in the process of diagnosing pathology.
It is the overview diagnostic format for medical examinations that is practiced (the breast is examined completely, not segmentally). But the diagnosis of a particular disease can only be carried out on a specific area of the gland. Segmental research is carried out using special tubes.
It is advisable to perform mammography under the following circumstances:
- In the presence of mastopathy of various origins. The glands are regularly examined for possible changes for the worse and the formation of other negative manifestations;
- In order to identify a benign or malignant tumor conglomerate;
- Women diagnosed with breast cancer undergo this procedure regularly, both during treatment and during long-term remission.
Advantages
The main advantages of mammography include:
- The ability to recognize formations of the smallest size, study the shape, size, nature of possible pathology;
- An extremely high degree of probability of detecting microcalcifications;
- A good way to determine how healthy the breast ducts are;
- Since X-rays are used to obtain a high-quality image, this method cannot be called completely harmless. However, women who are over 45 years of age do not have to worry about the potential danger, since x-rays at this age do not have any particular negative impact.
Flaws
Like any technique, mammography also has a number of certain disadvantages. Perhaps the most important drawback, which causes concern on the part of patients, is the possible harm from X-rays. Radiation is especially dangerous for young girls and women in the active reproductive period.
These diagnostic measures are carried out no more than once a year. Modern devices for carrying out the procedure are as safe as possible: with a minimum amount of “dose” it is possible to obtain the clearest images, valuable from the point of view of information potential.
Ultrasound
The ultrasound diagnostic method is popular for women of all age groups. Using ultrasonic waves, it is possible to thoroughly examine delicate glandular structures. Regarding the time of the procedure, ultrasound and mammography do not differ from each other.
When to use ultrasound
Already at the first visit to the patient, the doctor, forming a plan of diagnostic measures, already presumably knows what is better in each specific case - ultrasound or x-ray. Ultrasound is successfully used in the following cases:
- Problems with the menstrual cycle of unknown origin;
- The presence of inflammatory processes in the mammary gland;
- Monitoring the health status of women at the time of menopause;
- Control the growth of cystic or fibromatous formations;
- After surgical treatment of benign or malignant pathologies of the gland;
- If there is suspicious discharge from the nipples;
- Monitoring the condition of implants after cosmetic surgery.
We also recommend viewing: Symptoms and causes of burning in the mammary gland
Advantages of the technique
Experts are inclined to believe that it is better to use the ultrasound method for diagnosing pathologies. Ultrasound is informative for diagnosing the smallest formations. An important difference from radiography: the breast can be examined from several angles at once.
Using ultrasound, you can study the condition of regional lymphatic vessels. If a patient suffers from cancer, there is always a risk of metastasis. The formations of the lymphatic system are the first to be affected. Using ultrasound, it is possible to study the condition of tissues in as much detail as possible.
The technique is safe for girls and women of any age. The study is practiced by gynecologists during the treatment of pregnant women or nursing mothers. The method has proven itself well in diagnosing pathologies of breast vessels, as well as in the presence of injuries to glandular formations.
Flaws
Unfortunately, even such a progressive and safe diagnostic technology also has a number of disadvantages:
- Results obtained at different periods of the menstrual cycle may vary significantly;
- When using old equipment, the risk of “false” results increases;
- It is the diagnostician who influences the final conclusion. The specialist performing the procedure, at his own discretion, analyzes indirect and direct signs indicating the development of a particular disease. Thus, we can say that the level of professionalism of the diagnostician is directly related to the quality of the data obtained.
Safety
In fact, every person can tell the difference between mammography and ultrasound of the mammary glands. The main point is safety. The use of ultrasound does not cause any harm to the human body. Until the age of 40, it is advisable for women to be prescribed only such diagnostic methods. In addition, this is the only method acceptable for pregnant women.
Breast screening with X-rays allows you to take 4 full pictures. X-rays are not used for pregnant women, and the frequency of events is not abused.
Patient amenities
Ultrasound is convenient, painless, and does not require any preliminary preparations. A certain amount of time is required so that the diagnostician can thoroughly study the picture and form a conclusion.
Screening is done somewhat faster, also without causing pain or any discomfort. An important nuance: to make the picture as clear as possible, the doctor asks the patient to hold his breath for a few seconds.
Financial aspects
In the vast majority of government medical institutions, both procedures are performed free of charge. If we talk about private hospitals, then in this case, each diagnostic center forms a pricing policy at its own discretion. Typically, breast screening costs much more than ultrasound examinations of glandular structures.
myzhelezy.ru
Kinds
There are several variations of mammography: digital, film (X-ray), electrical impedance, magnetic resonance, etc.
Digital mammography photo
- Traditional X-ray diagnostics is the oldest technique that uses film technology. Such a study is a classic in breast diagnostics, since it has been used since the last century. The technique is almost never used in modern medical institutions, although it is still used in regional hospitals. The procedure is not a priority in comparison with other mammography methods, since it has the highest percentage of errors in the results.
- Digital mammography is one of the more modern diagnostic methods that have many undeniable advantages. For example, the radiation dosage received during digital examination is significantly lower than during film examination (three times). The quality of the resulting images is also significantly higher, which is much easier to analyze, which simplifies the reliability of the diagnosis and also eliminates the need for repeated examination. In addition, digital mammography can be performed using computer technology to detect structural changes in mammary tissue.
- Magnetic resonance mammography is performed without x-rays. This technique is characterized by maximum accuracy and high information content, but it also has the disadvantage of high cost. If necessary, to obtain a more complete clinical picture, MRI mammography is performed using contrast.
- Electrical impedance mammography diagnostics is the latest method for studying mammary glandular structures, based on differences in current conductivity between pathologically altered and healthy tissues. The electrical conductivity of unhealthy areas differs significantly from normal values, therefore, in a three-dimensional projection of the study results, tumor formation will be clearly visible. This method is more informative, does not use X-rays, has no contraindications and is not tied to the cycle, and is able to detect breast cancer in its infancy.
Decoding the results
Using mammographic images, a specialist studies the structure of tissues, ducts, capillaries, and lymph nodes. There are no pathologies if the structure of the breast tissue is uniform, the network of capillaries and ducts is clearly visible. Pathological changes are indicated when the tissue structure is uneven and the lymph nodes are enlarged.
An experienced doctor can easily determine the type of tumor, its size and configuration.
Mammologists distinguish 7 degrees of research results:
- zero – the information is unreliable, additional tests are needed;
- 1 – there are no suspicious lesions, the patient is healthy;
- 2 – there is a benign formation, there is no suspicion of malignant degeneration;
- 3 – there is a benign tumor that is suspicious, additional tests are needed;
- 4 – there are dense formations, a biopsy is needed to clarify the diagnosis;
- 5 – there is a neoplasm similar to a malignant tumor, a biopsy is necessary;
- 6 – the presence of a malignant tumor is confirmed.
If stage 6 is diagnosed, there is no need to despair and panic. The fact is that mammography data can be false.