A biopsy is the study of biological material, which is the tissue of a specific organ. Its collection presents certain difficulties and dangers, so before prescribing this type of study, doctors must be sure of the advisability of the risk.
During operations involving the removal of an organ or part of it, tissue is necessarily sent for a biopsy to confirm the correct diagnosis. Liver biopsy is used when differential diagnosis of diseases is necessary, when other methods require clarification due to their imperfections.
How is a biopsy specimen examined?
The extracted material is called biptate. It is delivered to the laboratory, where it is possible to conduct research in three directions:
- pathomorphological analysis - consists of identifying changes in the composition and shape of cells (cytology), tissue elements (histology), is one of the most common diagnostic methods;
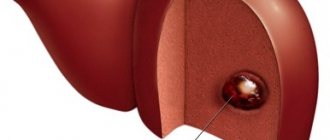
- immunohistochemical method - allows, using special processing, to identify the chemical composition of the material; in the diagnosis of liver diseases, it is important in Wilson-Konovalov disease (a sign is detected - copper deposition in the cells);
- biological culture method - makes it possible to isolate the infectious agent directly from the affected organ, determine its sensitivity to antibiotics for subsequent treatment (important for liver abscesses).
A “column” of tissue 10–40 mm high and weighing 10–50 mg is considered sufficient for analysis.
Summarizing
A biopsy is the intravital removal of a liver fragment for histological examination. The main objective of this technique is to clarify the diagnosis in cases where other detection methods have proven ineffective. A tissue biopsy provides information about the nature of the pathological process, its activity, as well as the degree of change in the organ. The examination is quite painful and can cause serious complications. That is why the indications for its implementation are clearly formulated and strictly assessed in each individual case. Liver biopsy is a necessary diagnostic method when it is impossible to confirm the diagnosis by other research methods. Most often, puncture, or percutaneous, sampling of biological material is performed. A biopsy is dangerous due to the development of bleeding and the spread of infection.
When is a biopsy needed?
No matter how the biopsy is performed, it is always necessary to penetrate the liver (invasive method). The doctor has enough methods in his arsenal, including laboratory and instrumental ones, to resolve the issue of diagnosis. In difficult cases, they resort to laparoscopy - insertion of an optical device through an incision in the peritoneum to examine superficial structural changes in the liver.
Indications for organ biopsy are determined by complex problems, the answer to which can only be obtained through an in-depth study of organ tissue:
- comparative diagnosis of liver diseases with tumors (benign, malignant), identification of signs of hyperplasia, cirrhosis, fibrosis, steatosis;
- detection of liver metastases in cancer of other organs;
- determining the extent and severity of pathological changes;
- elucidation of the aggressiveness of inflammation in viral hepatitis, fibrosis in cirrhosis;
- if a hereditary pathology is suspected;
- the need to monitor the effectiveness of treatment if drugs and methods that require studying the cellular composition are used;
- to assess the condition of the donor liver after transplantation.
In practice, there are patients whose biochemical tests are significantly altered; high levels of transaminases and bilirubin are determined for unclear reasons. It is in the patient's best interest to perform a biopsy to rule out viral hepatitis.
The nature of the detected morphological changes indicates the type of pathology
The study is necessary not only for cancerous liver damage, but also in the following cases:
- non-alcoholic fatty hepatosis;
- chronic hepatitis C or B;
- primary biliary cirrhosis;
- alcoholic liver disease;
- autoimmune hepatitis;
- primary sclerosing cholangitis;
- Wilson-Konovalov disease.
For any disease with unclear symptoms, when the results of other tests do not reflect an accurate picture of the pathology.
Decoding the results
Liver biopsy results can be obtained several days after the procedure. Decoding the examination allows the doctor to obtain a complete clinical picture, make a final diagnosis, and decide on treatment tactics.
The results of histological examination of the liver are divided into the Knodel scale and the Metavir method.
Metavir method
The Metavir method is used for liver damage with hepatitis C. It is determined by certain points:
- 0 degree – liver cells are not affected by fibrosis;
- 1st degree – organ tissue has grown in the portal tract;
- 2nd degree - pathological tissues have gone beyond the liver structure;
- 3rd degree – there is pronounced fibrosis;
- Grade 4 – cirrhosis is diagnosed with damage to a large part of the organ structures.
Who should not undergo a biopsy?
Contraindications for the biopsy procedure are severe bleeding disorders, bleeding, decompensation of cardiac and respiratory function, severe failure, comatose state of the patient, liver cancer with a decompensated stage of cirrhosis.
If there is a suspicion of hepatic hemangioma (tumor from a plexus of blood vessels), the approach to biopsy should be very careful. The method is justified only if it is necessary to exclude another neoplasm.
With subcapsular localization, hemangioma can cause severe internal bleeding. In each specific case, the doctor chooses the acceptable type of biopsy, taking into account the purpose of the study, the risk of complications and the patient’s condition.
Copper deposition in liver cells in Wilson-Konovalov disease
Contraindications
Liver biopsy is a fairly complex diagnostic procedure that has a number of absolute and relative contraindications. The first includes:
- increased tendency to bleed;
- poor blood clotting;
- liver hematoma or other vascular tumors;
- hydatid cyst;
- refusal of the patient to undergo the procedure.
Relative contraindications include:
- hemophilia;
- obesity;
- severe ascites;
- amyloidosis;
- mental disorders, neuroses;
- infectious diseases of the right pleural region;
- allergy to anesthetics and analgesics.
To exclude possible contraindications to a biopsy, it is necessary to conduct examinations, collect anamnesis, and study the patient’s medical history before performing it.
What types of biopsies are used in practice, what should a patient choose?
There are different biopsy methods, they have their advantages and disadvantages. Percutaneous or puncture biopsy is the most common method and is less traumatic for the patient. It can be performed both in the operating room of a clinic and in a hospital setting.
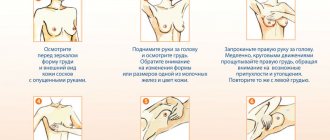
The patient is placed on his back, with his right arm placed behind his head. A puncture biopsy of the liver requires practical skills from the surgeon and a preliminary study of the research results. The intended puncture site is treated with antiseptics, and Novocain is injected with a syringe for pain relief. A small skin incision is made between the lowermost ribs.
A special needle with a wide lumen is inserted into it. To prevent the possibility of injury to the lung tissue, the puncture is performed against the background of exhalation. An additional needle may be needed to insert at a different angle. From the puncture of the liver, the doctor makes a suction movement with the piston of the syringe (the method is also called “aspiration”).
Liver tissue enters the needle. After the biopsy, the patient is advised to lie on his right side. For observation, two hours to a day is enough. There is a “blind” method, when the doctor uses only his knowledge of anatomy, and a “targeted” method, carried out under ultrasound control.
It is clear that in the first case, highly qualified personnel are not required, the risk of complications is higher, and one cannot count on good quality of the material. If there is hardware control, the result will be more reliable, but the research method is also more expensive for the medical institution or patient.
The first signs of liver cirrhosis from alcohol
Transjugular biopsy is performed in a hospital setting under the control of an X-ray machine. The patient lies on the X-ray table. The place of anesthesia is the projection of the jugular vein in the neck.
A small incision is made in the skin and a catheter with a flexible probe is inserted into the jugular vein using screwing movements. When approaching the hepatic vein, a contrast agent is injected, and photographs are taken to confirm the location of the catheter. Next, the probe takes the material for analysis. The catheter is carefully removed and a bandage is applied to the wound.
Laparoscopic biopsy is only permissible in a hospital; anesthesia is required. To do this, the patient is injected intravenously with a substance with a general analgesic effect, and he quickly falls asleep. A small incision is made in the abdominal area above the projection of the liver. Through it, the necessary instruments with a video camera at the end are inserted into the peritoneal cavity.
Modern technology allows you to display an image on a monitor screen, shows the liver to the surgeon, and allows you to select an area for collecting material. The possibilities exceed the puncture method. At the end of the manipulations, the instruments are removed and 1–2 sutures are placed on the incision. The method is contraindicated for peritonitis and severe obesity.
The biopsy kit includes a thin, long needle and a wider trephine
Targeted trephine biopsy is performed using a special instrument (trephine), wider than a needle. Therefore, a massive area of tissue falls into it, and a dense fibrotic lesion can be captured. Open method - used during a surgical incision, when the patient is given full anesthesia and intervention is expected. Seems to be the most reliable and effective.
After determining the indications, specialists inform the patient how a liver biopsy is performed in a particular institution. According to the law, the patient must sign an informed consent, the same as when preparing for surgery. Parents make decisions for children.
The doctor chooses the best method. For example, if a cancerous tumor is suspected, it makes no sense to conduct a “blind” puncture study. The method also depends on the equipment available in the clinic and trained specialists. Therefore, when deciding where it is best for a patient to undergo an examination, it is necessary to take into account all aspects of the issue and read reviews about a specific clinic.
Fine needle aspiration BP (FNA) under ultrasound or CT control
The area where the needle will be inserted is numbed with a local anesthetic. TIBP makes it possible to obtain material for cytological examination of focal liver lesions, including those of a malignant nature. The information content of the study depends on the experience of the morphologist evaluating the obtained material.
It must be remembered that the absence of atypical cells does not allow 100% to exclude the malignant nature of liver damage. This procedure is safe for cancer patients, as it eliminates the “scattering” of atypical cells. In addition, TIBP is safe for vascular and echinococcal liver lesions.
How is the preparation carried out?
To determine indications and exclude contraindications before the procedure, the doctor must check blood clotting indicators, an ultrasound of the liver and abdominal organs is performed, and women are examined by a gynecologist. Blood tests are taken for viral hepatitis and AIDS.
A patient taking anticoagulants or non-hormonal anti-inflammatory drugs should stop taking them a week before the expected biopsy. This is necessary to prevent bleeding. The doctor should be informed about all chronic diseases and allergic reactions that the patient suffers from.
It is forbidden to eat food 10 hours before, and drink 8 hours before the procedure. Before being sent to the operating room, you are asked to urinate.
Indications
A liver biopsy helps verify the diagnosis of many diseases of this organ.
As a rule, a liver biopsy is performed when it is necessary to confirm or clarify the diagnosis and nature of the disease after performing an ultrasound, CT, MRI or PET scan:
The advisability of prescribing a liver biopsy is determined jointly by several doctors: the attending physician and the head of the department or a council meeting.
Before the study, the patient is prescribed the following diagnostic measures:
- blood tests: (with determination of platelet levels), for HIV and blood type and Rh factor;
- Ultrasound of the liver (if necessary, CT, MRI and PET);
The research results obtained make it possible to identify the presence of possible contraindications for the procedure and determine the most appropriate liver biopsy technique.
After eliminating contraindications, the patient signs an informed consent for the diagnosis.
Tips after the procedure
Although a biopsy is not considered a highly traumatic operation, it requires recovery, like any intervention. Minor pain at the puncture site may last up to two days. The patient needs to be monitored, blood pressure and pulse are measured, and breathing is listened to.
Strict bed rest is required for 2–4 hours during a puncture biopsy; after other types, the doctor allows you to get up. If the procedure was carried out in a clinic, you are allowed to go home after 4 hours. During the day, you should follow the regime, move less, and do not lift heavy objects.
It’s better not to drive a car, you may feel dizzy
Reviews
Reviews from patients who have undergone a liver biopsy are often positive, since the procedure is most often well tolerated and rarely causes complications. The examinees note almost complete painlessness. This is achieved using local anesthesia. In this case, the feeling of discomfort may persist for 24 hours. It is much more painful, according to many reviews, to wait for the result of the analysis, which can both reassure and encourage the doctor to take active treatment tactics.
Tatyana A year ago I had a liver biopsy. Fortunately, the doctor’s fears were not confirmed. I had a percutaneous biopsy using a fine needle. So, specialists take a tissue sample directly from the liver. For about a week I had discomfort in my right side. I did not experience any complications. The doctor said that tests would be done within a week. This period was especially painful for me. I'm glad I agreed to the biopsy, otherwise I would have tormented myself and tormented myself with assumptions about possible cancer. The procedure clearly shows the condition of the liver tissue and helps the doctor decide on subsequent treatment tactics.
Vladimir My grandmother was prescribed a biopsy several months ago. The doctor's disappointing predictions were confirmed. Fortunately, the cancer was detected in time. Treatment is still ongoing. The grandmother complained of severe abdominal pain after the biopsy. They passed in about a week. During the day she was in the hospital under the supervision of doctors. The next day she was discharged. The doctor warned her that she should not lift weights or take a bath for a while. To monitor the condition of the body, doctors performed ultrasound several times.
Julia It’s not for nothing that they say that fear has big eyes. I didn’t want to do a biopsy, but the doctor reassured me and assured me that everything would go well. It was difficult for me to cope with my feelings, so the doctors even prescribed sedatives. Everything went well. The study helped to identify the pathology in time and begin treatment. I did not experience any pain during the procedure itself. During the week there was slight discomfort at the puncture site, but it was tolerable.
What are the possible complications?
Conducting a controlled biopsy and sufficient qualifications of the doctor guarantee the absence of complications. They occur very rarely in the form of:
- internal bleeding (hitting a hemangioma, a vessel);
- wounds with perforation of the bile ducts, intestines, stomach with peritonitis;
- damage to lung tissue with the development of pneumothorax;
- introduction or activation of the spread of infection with subsequent formation of liver abscess and general sepsis.
If complications require additional treatment, they significantly aggravate the clinical picture of the disease.
Possible consequences
Early complications occur in the first few hours after the procedure. If the integrity of the branches of the portal vein is damaged by a needle, bleeding may occur. This condition occurs in 0.2% of needle biopsy cases. Every third patient complains of pain at the site of material collection. The pain may radiate to the stomach area and right shoulder. Treated with conventional painkillers.
A condition called hemobilia may develop. This is bleeding into the intestinal tract from the biliary tract. Develops within three weeks from the moment of liver biopsy. Patients complain of pain, jaundice, change in stool color (it turns black).
The puncture should be carried out exclusively by a qualified specialist, since the possible risk of damage to the walls of the large intestine and neighboring organs is quite high.
You should consult a doctor if you develop hyperthermia, chills, swelling or redness in the puncture area. Severe pain, attacks of nausea and vomiting, dizziness, shortness of breath and cough should alert you.
Diagnostic methods for studying the liver
Hepatest. Clarification of the clinical picture by taking an anamnesis: general condition; hereditary predisposition; presence of subcostal pain; color of skin, feces, urine, etc.); Blood and urine examinations. Collection of general and biochemical analysis; Examination using ultrasound. Detection of stones in the gall bladder and expansion of bile channels in the liver, tumor processes, determination of the density, boundaries and size of the organ and its circulatory system; X-ray examination. Angiographic method of introducing a contrast agent into the hepatic ducts; Gland biopsy. Excision of an area of parenchymal tissue or blood of the inferior vena cava.
To establish a final diagnosis and prescribe the correct treatment for liver diseases, the results of collecting anamnesis, clinical symptoms and a superficial examination are not always enough.
To identify deep structural tissue disorders, the liver puncture method is used.