Features and capabilities of the procedure
Swallowing a probe to check the stomach or FGDS is an endoscopic method for examining the esophagus, stomach and part of the duodenum to confirm suspected tumors, identify sources of bleeding, and generally assess the condition of the mucous membranes. Otherwise, the procedure is called swallowing a light bulb for the stomach.
What is the name of the procedure for swallowing a light bulb for the stomach? The official name of the manipulation is fibroesophagogastroduodenoscopy or FGDS. The procedure is performed using a gastroscope equipped with a long thin probe with a tip. At the end of the tube there is a built-in video camera and lighting device, which transmit the resulting image to a computer monitor.
Possibilities
FGDS combines both diagnostic and therapeutic-diagnostic functions. Fibroesophagogastroduodenoscopy has the following special capabilities:
- detection and management of bleeding sources;
- removal of polyps, tumors;
- treatment of ulcerative-erosive lesions;
- antiseptic treatment of mucous membranes in acute inflammation;
- possibility of taking a biopsy sample for histological analysis.
FGDS allows you to provide emergency care for ulcerative bleeding, suspected perforation of an ulcerative-erosive focus. Biopsy plays an important clinical value in relation to tumor-like neoplasms. The analysis allows you to accurately determine the presence of atypical cancer cells, make prognoses and individual treatment tactics.
Gastroscopy without swallowing the probe
This type of examination also includes transnasal fibrogastroscopy, in which a probe is passed through the nasal passages and descends into the stomach along the back wall of the pharynx. This is a gentle method intended for particularly sensitive patients exposed to stress. For example, in case of hypertension, inserting a fiberscope through the mouth can provoke a surge in pressure or even a hypertensive crisis. With transnasal FGS, these undesirable consequences can be avoided, since negative emotions from the manipulation are minimized.
Gastroscopy of the stomach without swallowing a probe becomes possible in its pure form thanks to capsule endoscopy. The patient is asked to swallow a small capsule, inside of which there is a built-in video camera and a video signal transmitter for it. There are different companies that produce capsules, they may have specific features, for example, there are capsules intended for the small or large intestine, for the stomach. Along with the capsule, the patient receives a signal receiver. Then, from this receiver, the doctor will take the data obtained during capsule endoscopy, but at this stage the patient can leave the hospital and return home. Later, the capsule will naturally leave the gastrointestinal tract, having previously captured the entire picture throughout the gastrointestinal tract. It is disposable and it is not necessary to control its output.
If you experience discomfort, changes in bowel habits or pain, you should immediately contact your doctor. A relative disadvantage of this study is that it is only diagnostic in nature; there is no possibility of conducting therapy or taking material for analysis.
Price issue
The cost of studying the gastric mucosa correlates with the complexity of the study. On average, prices for classic fibrogastroscopy vary from 2 to 4 thousand. With additional manipulations (biopsy, pH measurements) carried out during the study, the price can increase to 10 thousand.
Transnasal gastroscopy is limited to an average of 4 thousand rubles, so it is impossible to carry out additional actions.
Video capsule gastroscopy is the most expensive study, since the most expensive materials and modern technological developments are used to create a disposable capsule (20-50 thousand).
*Prices are indicated in rubles.
Indications and contraindications for FGDS
The main indications for manipulation are patient complaints about the appearance of unpleasant symptoms, as well as dynamic control over the condition of the mucous membranes of the upper digestive system after surgery, for tumors against the background of expectant management. The following indications for use are distinguished:
- pain in the cavity of the stomach, esophagus (painful to swallow, after eating, at night);
- gagging and nausea of unknown origin;
- excessive swallowing of air;
- severe swallowing dysfunction;
- decreased appetite;
- loss of body weight against the background of a preserved diet;
- suspicion of foreign bodies getting inside;
- suspicion of tumors, polyps, oncogenic neoplasms;
- prolonged episodes of heartburn.
The FGDS procedure can be carried out to clarify other diagnostic research methods for already identified pathologies. Manipulation allows you to provide assistance with the following clinical tasks:
- diagnosis of anemia of unknown origin;
- study of the hepatobiliary system as a whole;
- confirmation of a family history of tumors and peptic ulcers;
- dynamics of the condition of the mucous membranes against the background of ulcerative gastritis, chronic inflammatory diseases;
- the need to remove polypous lesions and tumors;
- control after surgery to eliminate the risk of relapse.
Usually, to perform gastroduedenoscopy, it is enough only for the patient to complain about uncharacteristic symptoms that are not associated with a change in diet. The manipulation can be performed in the endoscopic procedure room.
Examination of the patient
Examination of the esophagus consists of general examination and palpation. In this case, special attention is paid to examining the larynx, its condition, and the smell from the oral cavity. A general examination is of no less diagnostic importance: the patient’s degree of fatness, skin color and texture, facial expressions, body temperature, swelling.
To treat gastrointestinal diseases, people successfully use Galina Savinova’s method. Read more >>>
Local examination of the esophagus includes palpation of the lymph nodes, neck, auscultation and percussion, as well as instrumental diagnostic methods:
- radiography;
- daily pH measurements;
- computed and spiral tomography;
- esophagofibroscopy.
With painful shock, pale skin is observed, with oncology and hypochromic anemia there is yellowness, with esophagitis there is hyperemia, and with large formations that cause hypoxia there is cyanosis.
The presence of pain is indicated by a grimace on the face and anxiety of the patient. An unnatural position of the body or head with a forward tilt indicates a possible diverticulum or foreign body. The patient in these conditions tries not to make body movements that cause him pain.
The lethargic and indifferent state of the patient signals septic or traumatic shock (for example, with a burn or mechanical perforation of an organ by a foreign body, massive bleeding, a state of severe intoxication).
X-ray of the esophagus
The manipulation is carried out on an empty stomach. Before undergoing radiography, the subject must take a contrast agent (barium sulfate solution). This is explained by the fact that not all organs of the gastrointestinal tract are capable of blocking X-rays, and barium makes it possible to visualize motor functions and contours of organs.
This method is necessary if the presence of neoplasms or foreign bodies is suspected, as well as with achalasia. The procedure for radiography of the esophagus and stomach does not require lengthy preparation. You should refrain from eating for about eight hours or skip breakfast.
Esophagofibroscopy
This highly informative research method helps to find out the cause of pain, dyspepsia and dysphagia of the esophagus. It can be used to determine the presence of varicose veins, tumor formation, and bleeding from the esophagus. It is carried out both for the purpose of diagnosing the esophagus and for providing emergency assistance. Thanks to the method, it is possible to diagnose cancer formations on the walls of the organ and pathological changes in the lymph nodes.
The method makes it possible to determine the condition of the inner lining of the esophagus and obtain material for histology. The manipulation is carried out by qualified specialists under local or general anesthesia. The method requires preliminary preparation of the patient.
Diagnosis occurs by introducing an ultrasound sensor through the larynx to visually examine the mucous membrane and collect biological material for histology. The endoscope has high ultrasound frequencies that detect minimal deviations from the norm, which makes esophagoscopy one of the most highly informative research methods.
Daily pH-metry
The method helps, by measuring the pH level, to determine the nature and severity of esophageal reflux. To do this, a probe with a sensor of one to three electrodes is inserted through the larynx and fixed in a certain place.
The sensor records changes in pH in the lower part of the esophagus during the day. The data is subjected to computer analysis, and on its basis, its compliance with the norm is established.
Bernstein test
Acid perfusion is used when other methods do not show changes in the mucous membrane, but the patient feels dyspepsia, odynophagia, and dysphagia. The method consists of introducing saline and HCl solution into the larynx through a probe alternately at the required speed. In the presence of reflux esophagitis, discomfort and pain in the chest occurs due to irritation by acid.
Esophagotonokymography of the esophagus
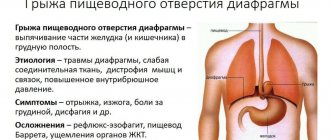
The essence of the method is to obtain images that record decreased tone and contraction of the esophageal muscles. In this way, the initial form of dysphagia, hernias and muscular pathologies of the esophagus without severe symptoms is diagnosed.
During the study, a multichannel probe with a catheter or rubber balloon is used to measure intraesophageal pressure. The gastroscopy method allows you to obtain complete information about all possible decreases in the muscle tone of the sphincters.
Computed and spiral tomography
The study is used to diagnose neoplasms and metastases, enlarged lymph nodes, and determine wall thickness. This diagnostic method is also radiation, but unlike X-rays it allows you to obtain a higher quality image. The procedure involves preparing the patient for the study, which consists of administering externally and internally contrast solutions containing iodine.
Spiral tomography is a method of x-ray examination. During it, the tomograph moves in a spiral, creating highly accurate 3D models. The devices automatically convert the received data into digital form. With the help of such a study, pathologies of almost all internal organs are diagnosed. The method is characterized by high information content and accuracy of research with a minimum degree of radiation from devices.
It is used for a comprehensive diagnosis of the esophagus, determining the exact location and boundaries of the lesion or the presence of a foreign body. It is used as an additional research method if previous measures did not give the desired result.
Chromoendoscopy method
The method reveals pathological changes in the esophageal mucosa using staining with Lugol's solution, phenol, and methylene blue. The procedure helps determine the location of the lesion by changing the shade of the tissue. It is used primarily for the diagnosis of oncological tumors.
Radioisotope research
When diagnosing oncological formations, the RI method is used. It is used quite rarely, but it has a number of advantages: it is harmless and allows one to obtain data that is not available with other research methods. The method is recommended for the differential diagnosis of esophageal cancer. In this case, radioactive phosphorus is used, which accumulates in tumor formations, which makes it possible to determine their presence. The method does not require preliminary preparation.
Today, there are many modern, highly informative methods for diagnosing diseases of the esophagus, which makes it possible to qualitatively examine the patient. However, one research method is not enough to determine the final diagnosis. Only the attending physician, after a comprehensive examination, questioning and examination of the patient, can establish the disease and prescribe adequate therapy.
Main contraindications
Despite the high information content of the method, the use of the FGDS procedure is unacceptable in the following conditions:
- abnormal body weight according to age (up or down);
- a sharp narrowing of the esophagus and gastric sphincters (there are risks of traumatizing the mucous membranes);
- exacerbation of inflammatory diseases (with active inflammation, the mucous membrane becomes thinner, and the probe can increase irritation);
- heart failure;
- pulmonary failure;
- serious mental illness;
- dysfunction of the respiratory system of various origins;
Important! Indications can be relative or absolute. In the first case, it is recommended to wait for a favorable period to conduct an endoscopic examination. The second is to choose alternative diagnostic methods.
What alternative methods are there?
In the arsenal of a gastroenterologist, in addition to examination, history taking and general tests showing the general condition of organs and systems, there are also instrumental techniques, such as FGDS.
Among the alternative methods for examining the stomach, the following are used:
- ultrasonography;
- X-ray;
- video capsule endoscopy;
- CT;
- MRI;
- transnasal FGDS;
- gastropanel;
- desmiod test.
They differ in the degree of information content and have some contraindications.
How to prepare for the procedure
How to swallow a stomach light bulb safely and how to prepare? The reliability and information content of the study largely depends on preparation for the FGDS procedure. For proper preparation, it is recommended to follow a number of rules:
- the procedure is carried out on an empty stomach (the last meal should be no later than 10-12 hours before the procedure);
- 2 days before FGDS, fatty, aggressive foods, alcohol, and tobacco are completely excluded;
- exclusion of medications on the day of endoscopy.
If it is necessary to perform an FGDS under anesthesia, the preparation remains the same. After the preparatory measures, the endoscopic procedure itself begins. There is an endoscopist and a nurse in the office. If anesthesia is necessary, an anesthesiologist is required. Parents may be present during the examination of the child.
Advantages of the technique
In addition to obvious advantages, such an examination of the stomach also has disadvantages. First of all, we are talking about the fairly high cost of the procedure. It is several times higher than the price for the classic version of gastroscopy. As a result, the patient will have to pay up to 10,000 rubles. Such a high cost is due to the use of expensive instruments and, above all, a video capsule during the procedure.
An even greater disadvantage of such an examination of the stomach is the fact that during its implementation it is impossible to perform a biopsy. It will also not be possible to take a closer look at the pathologically changed area.
Often, during classical gastroscopy, patients have various types of polyps removed. This is necessary for the reason that these formations tend to become malignant. Unfortunately, this is not possible when using a video capsule.
How is FGDS performed?
How to swallow intestines to check the stomach? Before the procedure, a Lidocaine solution is injected into the patient’s throat or a Falimint tablet with eucalyptus extract is allowed to dissolve. After reducing sensitivity, the patient is undressed to the waist and lies on the left side on the couch. The left cheek is pressed tightly against the pillow, the right hand is pulled behind the back.
First, a mouthpiece is inserted into the mouth, which protects the probe from being squeezed or bitten by the teeth, then a tube is inserted through the mouthpiece to the root of the tongue. The patient is then asked to take a deep breath or swallow, after which the probe penetrates the esophagus. It is recommended to breathe deeply as the endoscopic equipment moves. This expands the respiratory tract, saturates the brain with oxygen, and prevents gagging.
The total duration of the study varies within half an hour. If it is necessary to carry out therapeutic surgical procedures, the time can be increased to an hour. If local anesthesia is used, the patient can go home immediately after the procedure.
Important! If sedation or general anesthesia was used, the patient is transferred to a temporary ward to restore clarity of consciousness. Children are left in the hospital for a day to exclude long-term unforeseen complications after anesthesia.
Basic diagnostic criteria
During the examination, doctors can evaluate the functional, anatomical and structural features of the digestive system. The following criteria are distinguished:
- conductivity of the stomach, esophagus, small intestine;
- the presence of stenoses, strictures, scar tissue;
- inflammatory foci, ulcerative and erosive changes;
- gastroesophageal reflux (reflux of food from the stomach into the esophagus);
- protrusion of the muscular structures of the diaphragm;
- presence of neoplasms.
The FGDS procedure is absolutely indispensable as a differential diagnosis in oncology, surgery, and gastroenterology. When performing FDS under anesthesia, it can be performed in combination with colonoscopy for an extensive assessment of the clinical picture.
Fibrogastroscopy
Fibrogastroscopy is the most common way to examine the gastric mucosa by inserting a fibrogastroscope into the organ cavity. This procedure is indicated for patients who are suspected of having gastritis, stomach ulcers, tumors, or polyps. Sometimes FGS is prescribed to identify possible causes of allergies or neuroses; the range of diseases is quite wide. Now the study is carried out in two versions of the probe: through the mouth and through the nose.
The procedure lasts only a few minutes, and the doctor can announce preliminary results immediately after the manipulation.
The patient is in a reclining position on his stomach, holding a special plastic mouthpiece in his mouth. The gastroenterologist endoscopist passes a probe through it and asks the patient to swallow the tube. Since light anesthesia was administered in advance, his gag reflex is weakened, and the patient does not feel the urge to gag, only discomfort and a sensation of a foreign body.
The advantages of this method include:
- short duration of the study (only 2-5 minutes);
- quick receipt of visual observation results;
- the ability to manipulate a video camera under eye control to study areas of particular interest;
- the possibility of carrying out therapeutic measures (biopsy, coagulation of bleeding vessels, removal of polyps);
- minimal risk of complications.
The disadvantages of fibrogastroscopy include:
- long period of preparation for the study, dietary restrictions;
- discomfort during gastroscopy;
- a large number of contraindications.
This test is not yet widely used; transnasal testing means passing a flexible probe through the nose, along the back of the throat and down the esophagus. Since the fiberscope does not affect the root of the tongue and the uvula of the soft palate, the patient is not bothered by the gag reflex. The patient no longer requires local anesthesia or sedation. If there are allergic reactions to the anesthetic, this will be a separate point in favor of the transnasal method.
Obviously, the tube in this case will be much thinner than with fibrogastroscopy through the mouth. The diameter of the tube should not exceed half a centimeter, which means that the additional capabilities of gastroscopy will be significantly limited (you cannot take a biopsy through a thin channel, you cannot perform coagulation during bleeding). Such a tube is easier to insert, and the quality of the study itself does not deteriorate at all.
Scheme of passing the tube through the nose.
In addition, with the transnasal route of administration, the patient’s verbal functions are preserved; he can immediately report any unpleasant sensations to a specialist, which significantly reduces fear and anxiety before the procedure.
But, like any procedure, transnasal FGS has its drawbacks. Some patients report the appearance of nosebleeds after gastroscopy through the nose.
Possible complications
Modern equipment and the professionalism of the doctor greatly reduce any risks of complications. However, with a burdened gastroenterological history, the following complications may occur:
- vessel damage and bleeding;
- perforation of the walls of the esophagus or stomach due to inaccurate insertion of the probe (usually against the background of deep ulcerative-erosive lesions)g
- entry of stomach contents into the respiratory tract (due to poor preparation).
Note! Normally, after the manipulation, there is a slight feeling of fullness in the throat, soreness and dryness. This is caused by friction of the probe. Discomfort in the stomach area often occurs. All these unpleasant symptoms disappear after a few hours.
CT scan
This method is also considered one of the most relevant and informative. It is more difficult to perform. As a rule, a computed tomograph is available only in relatively large cities and not in every medical institution. It requires a special room for the device and special training for the doctor.
A large number of photographs are taken, layer-by-layer sections of the human body in the area of the esophagus. They are used to judge the condition of the esophagus and surrounding tissues. Conclusions are drawn about the thickness of the organ, its walls, internal lumen, and defects in its structure. Using this method, the exact boundaries of organ structures are checked and pathological changes are determined. The method allows you to see even beginning pathological changes, the initial stages of cancer...
Computer tomograph
Results of esophagogastroduodenoscopy
Gastroscopy of the esophagus and stomach allows you to study in sufficient detail the condition of the mucous membrane of the upper gastrointestinal tract. Erosion, ulcers, foci of cellular transformation (leukoplakia, Barrett's esophagus), and tumor formations can be detected. If necessary, tissue sections can be removed immediately for biopsy. It is necessary to understand that the result of gastroscopy of the esophagus is not yet a diagnosis, but only a component of a comprehensive diagnostic plan.
A diagnostic procedure can turn into a therapeutic one. For example, if there is bleeding from varicose veins of the esophagus, during gastroscopy of the esophagus, ligatures can be applied or cauterization of the bleeding areas can be performed.
Among diseases of the digestive system, pathologies of the esophagus receive special attention. This is due to the trend of increasing precancerous diseases based on existing chronic pathologies of the organ.
How to check the esophagus in order to make a timely diagnosis of a particular pathology and receive adequate and timely treatment? This issue will be discussed in this article.
Treatment of diseases of the esophagus is one of the most complex surgical interventions of modern surgery. This is explained by the topography of the organ and the close location of the organs bordering it. The more the role of such an event as a high-quality diagnosis of the esophagus increases .