Over the past decade morbidity cirrhosis increased by more than 10%. The disease affects people of different sexes and ages, mainly the population of developed countries.
The cause of the disease in 52% of cases is excessive consumption of alcohol , which is processed by the liver. There, ethyl alcohol is broken down into compounds that are dangerous to the body: acetaldehyde and acetic acid.
These substances must be removed in a timely manner, otherwise they cause toxic poisoning, which subsequently develops into cirrhosis.
The disease has a very unfavorable prognosis : by eliminating the cause and timely treatment, in half the cases a person can buy himself 10 or more years of life, in other cases – 3-5 years.
Therefore, it is so important to know the symptoms of the disease in order to consult a doctor in time and begin therapy.
Symptoms of liver cirrhosis
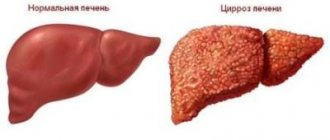
Cirrhosis is a long-term, slowly progressive disease. It manifests itself in modification of hepatocytes - the main functional cells of the liver, proliferation of fibrous tissue, appearance of a nodular structure and, as a consequence, changes in the vascular system. Outwardly, it looks like scarring and shrinkage of the liver.
Ultimately, liver failure develops and is fatal. Often cirrhosis transforms into cancer .
Reference. The word cirrhosis comes from the Greek word "kirrhos", which means "yellow".
And this quite accurately characterizes the symptoms of the disease. Symptoms of cirrhosis depend on the etiology of the disease and the individual characteristics of the patient. In 20% of cases, the initial stage is asymptomatic , which is unfavorable, since early detection allows one to avoid liver failure: with the help of medication and a special diet, the process of cell regeneration can be started.
But in most cases, be determined even at home by the following symptoms:
- Insomnia , impaired concentration, memory impairment, loss of performance.
- Weakness , muscle atrophy.
- Itchy skin is due to the fact that bile acid is not excreted from the body.
- Severe emaciation : thin limbs, cheekbones prominent on the face, significant weight loss.
- Red face due to dilated capillaries.
- Increasing nausea . Blood in the vomit, which is a sign of gastric bleeding. Nosebleeds may also occur.
- Joint swelling , decreased mobility. Swelling of the legs and tongue.
- Low-grade fever appears and disappears depending on the patient’s condition.
How to identify advanced liver cirrhosis:
- The whites of the eyes, the mouth, and later the entire body turn yellow. This is caused by the accumulation of bilirubin in the body.
- Xentelasmas are benign neoplasms in the form of yellowish plaques on the eyelids. They arise due to lipid metabolism disorders.
- Anemic syndrome . Due to insufficient liver function, vitamin B12 deficiency develops. In addition, systemic circulatory disorders occur.
- Ascites is an increase in the volume of fluid in the peritoneum. The internal organs cannot cope with the removal of abdominal fluid, designed to reduce friction between organs and fill voids.
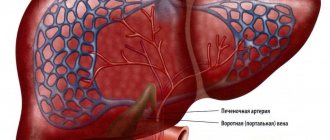
- The flow of blood to the liver is disrupted . The venous network is clearly visible on the abdomen.
Reasons why the disease occurs
Etiology
The causes of liver cirrhosis are varied, among the most common are the following:
- an infectious disease caused by hepatitis B, C, D and newly diagnosed hepatitis G;
- alcohol abuse for 10 years or more;
- diseases of an autoimmune nature;
- pathologies of the gallbladder and ducts, cholangitis;
- disturbance of blood flow in the portal vessels, in which pressure sharply increases;
- genetic predisposition;
- poisoning with toxic substances;
- long-term use of heavy medications.
Pathogenesis
It is important to make a diagnosis on time.
The genesis of cirrhosis progression is closely related to etiology. Long-term exposure to negative factors on the organ causes irreversible necrotic changes in liver hepatocytes, which are replaced by scar connective tissue. The disease progresses rapidly, due to the increase in connective tissue foci, the main functions of the organ are disrupted, and intrahepatic pressure increases.
Liver cirrhosis develops according to the following scheme: necrosis - regeneration - restructuring of the vascular bed - ischemia of the liver tissue - necrosis. To prevent further liver destruction, it is important to accurately determine the etiology and pathogenesis of cirrhosis, then treatment will be effective.
The first signs of liver cirrhosis
Even during the initial examination, the doctor can recognize liver cirrhosis :
- Palpation reveals an increase in the size of the liver and spleen. This occurs at the stage when cirrhosis begins. In the last stage, the liver shrinks in size and becomes harder.
- The surface of the liver is uneven, nodular, the lower edge is rounded.
- When percussing the abdominal cavity, a dull percussion sound is heard, indicating the presence of fluid. The volume of fluid can be determined using ultrasound.
- The radiograph shows an elevated diaphragm.
- Ultrasound shows a gradual weakening of the signal due to the progression of liver atrophy. The portal vein is poorly visible, the vascular pattern is not visible at all.
- Telangiectasia on the face. At the same time, the skin has a specific dark shade.
A blood test allows you to diagnose cirrhosis at an early stage using the following indicators:
- Reduction of hemoglobin below 120 g/l.
- A decrease in leukocytes below the level of 4.9*109/l.
- A decrease in the number of red blood cells below 4.9*1012/l.
- The platelet count drops below normal 180*109/l.
- The increase in ESR in men is more than 10 mm/h, in women it is more than 15 mm/h.
- Increase in globulins.
Important. It is necessary to monitor the first signs of cirrhosis, although the symptoms may be mild and may be felt as a slight discomfort. This is of fundamental importance for the patient’s life expectancy.
How does liver cirrhosis manifest itself at an early stage in terms of symptoms :
- Bitterness and dry mouth in the morning.
- Diarrhea, increased gas formation, lack of appetite.
- Nervous system disorder: irritability, fatigue.
- Bleeding gums.
- Sometimes signs of jaundice can be seen at an early stage.
Child-Pugh classification
It is based on the analysis of the performance of liver cells in cirrhosis. The following parameters are taken into account:
- Ascites (may be absent, mild or severe);
- Encephalopathy (absent, mild or severe);
- Bilirubin (estimated values: less than 35 µmol/L, from 35 to 50 µmol/L and more than 50 µmol/L);
- Albumin (more than 3.5 g%, from 2.8 to 3.5 g% and less than 2.8 g%);
- PTV, magnification factor (from 1 to 3, from 4 to 6 and more than 6);
- Food (good, satisfactory or poor).
Small nodular cirrhosis of the liver
The disease is assessed according to all the given parameters. For the first values 1 point is awarded, for the second - 2 points and for 3 - 3 points, respectively. The class of cirrhosis is determined as follows:
- A class – 5-6 points;
- To class – 7-9 points;
- C class – 10-15 points.
Patients whose disease falls under class A have the best prognosis; doctors are able to extend their life to 15-20 years. Surgery at this stage gives good results (survival rate is up to 90%), while a liver transplant is extremely rarely required.
Class B is much more difficult to tolerate, people live in this situation for no more than 10 years, and about 70% survive the operation.
Class C is the most severe, it has the lowest survival rate after surgery (18 out of 100), although the need for surgical intervention is the highest, since a donor liver transplant is required. With the most positive development of the disease in this case, doctors give 1-3 years of life. The clinical picture of class C cirrhosis includes:
- jaundice;
- high temperature;
- problems with stool;
- internal and external bleeding;
- poor appetite.
In some cases, only a liver transplant can prolong the patient’s life.
Other signs of cirrhosis
There are a number of external symptoms , the totality of which can accurately diagnose cirrhosis of the liver:
- Dark colored urine, which results from excess bilirubin in the blood. Breaking down in the liver, it is excreted by the kidneys.
- Change in color of stool, first to light, then to white.
- Colic in the right hypochondrium. The peculiarity of pain with this disease is that it intensifies after physical activity or fatty foods. The pain increases in proportion to the development of the disease.
- Red palms . This is due to poor circulation. In addition to the palms, there is redness of the last phalanges of the fingers on the inside.
- Characteristic external signs are “ drum sticks ”: the fingers become noticeably thicker towards the end.
- Nails become brittle and fragile, taking on a rounded shape, like “watch glass”. There is also redness around the nail holes.
- Bright crimson color of the tongue . The tongue itself becomes glossy, as if coated with varnish.
Manifestations of the disease are grouped according to functional disorders into syndromes. The following syndromes are distinguished in liver cirrhosis:
- Cytolytic syndrome. It is characterized by massive cytolysis (destruction) of liver cells. The severity is determined by the degree of increase in the level of AST and ALT enzymes.
- Cholestatic syndrome. Occurs when bile stops flowing into the duodenum. Accompanied by a decrease in cholesterol and protein against the background of liver failure, and an increase in bilirubin and alkaline phosphatase.
- Hepatorenal syndrome. In addition to liver dysfunction, renal dysfunction is added, most often due to toxicosis.
What stages do doctors distinguish?
There are four stages of cirrhotic damage. Only the last two of them are usually accompanied by the accumulation of ascitic fluid.
- Initial, or stage of compensation. The liver tissue is greatly changed, with the formation of scars (cirrhosis) mainly along the periphery, but there is no portal hypertension and ascites.
- Subcompensation. Compensatory mechanisms begin to fail. Fibrosis (scarring) moves from the periphery to the center of the organ. Portal hypertension is noted. At this stage, minor but more pronounced health complaints appear. Fluid in the abdominal cavity may accumulate in small quantities, and the abdomen is not yet very enlarged.
- Decompensation. It is characterized by an increase in the amount of scar tissue, which already occupies from half to 2/3 of the volume of the organ. A large amount of fluid accumulates in the abdominal cavity, and the abdomen increases in volume. The patient has a large number of different health complaints.
- Terminal. New dangerous symptoms are added to decompensation, the prognosis for health and life is questionable, the condition is serious, possible impairment of consciousness, the abdomen is tense due to ascites.
The degrees of ascites are related to the volume of accumulated fluid:
- Ascites is determined only by ultrasound.
- Moderate increase in abdominal volume due to ascites.
- Severe tense ascites.
A separate problem for the patient and the doctor is if ascites becomes refractory, that is, does not respond to drug treatment. Then it is possible to use surgical methods for treating ascites, but the prognosis in general is not very favorable.
Differences in symptoms of cirrhosis in women and men
Liver cirrhosis is half as common in women as in men. The main symptoms of the disease are the same, but there are characteristic differences by gender.
The first signs of cirrhosis in men are:
- Growth of the mammary glands, appearance of sagging breasts.
- Testicular shrinkage.
- Hair loss on the pubis and armpits.
Symptoms of liver cirrhosis in women:
- Heavy menstruation.
- Irrhythmia or absence of menstruation.
- Lack of sexual desire. Infertility.
Men suffer from alcoholic cirrhosis in 90% of cases. Women mainly suffer from secondary cirrhosis of the liver due to gallstones, tumors, or arising as a complication after operations on internal organs.
Diagnostics
Cirrhosis and pre-cirrhosis are treated by a hepatologist; he is the one who will be able to make an accurate diagnosis and prescribe effective treatment. After an initial examination, palpation, history taking and clarification of the genesis of the pathology, the doctor gives a referral to undergo a number of such diagnostic procedures:
- biochemical and general blood test;
- coagulogram;
- Ultrasound of the abdominal organs;
- esophagogastroduodenoscopy;
- MRI or CT;
- scintigraphy;
- liver biopsy.
Modern view on the development of ascites
Modern scientists consider portal hypertension, hemodynamic and neurohormonal regulation disorders to be trigger factors in the development of ascites. Pathogenetic disorders are considered as a combination of different levels of a progressive process. All of the above reasons are classified as systemic or general. But greater importance is attached to local factors.
These include:
- increased vascular resistance inside the hepatic lobules, they can be reversible and irreversible (complete block);
- the intrahepatic block enhances the formation of lymph, it leaks through the vascular wall and liver capsule directly into the abdominal cavity or “floods” the portal vein and the thoracic lymphatic duct;
- accumulation in the blood of patients of unsplit substances with a vasodilator effect (vasodilators such as glucagon), which lead to dilation of peripheral arteries, open arteriovenous shunts in organs and tissues, and as a result, the filling of arteries with blood decreases, cardiac output increases, and portal hypertension simultaneously increases;
- a significant part of the plasma is reflexively deposited in the vessels of the abdominal cavity;
- the effect of vasodilators is enhanced by insufficient production of nitric oxide by the liver.
Proponents of local disorders believe that the main mechanism for the development of ascites is formed inside the hepatic sinusoids
It is from the sinusoids that fluid comes out into the veins and lymphatic vessels. An increase in pressure inside the lobules leads to its penetration into the parasinusoidal space and then into the peritoneum.