Primary liver cancers are uncommon. Mostly, cancer of this organ is secondary, that is, metastatic. Primary liver tumors include cholangio- and hepatocellular carcinoma. Similar types of cancer can develop in both men and (less commonly) women. In childhood, these tumors practically do not occur. Young patients may develop liver cancer originating from germinal tissues - hepatoblastoma. This pathology is rare. Almost all primary liver tumors are considered aggressive. They occupy 5th place in mortality in the structure of oncological pathologies. Currently, new means of combating liver cancer are being sought. Great advances have been made through the discovery of targeted and immune therapies.
Description of hepatocellular carcinoma
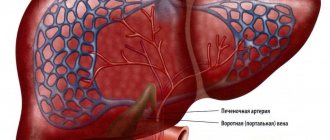
Hepatocellular carcinoma is a tumor arising from liver cells that have undergone atypia. Compared to other primary oncological pathologies of this organ, it is the most common. This tumor is also called hepatocellular carcinoma. In terms of frequency of occurrence, hepatocellular carcinoma among men ranks 5th in the world. This tumor occurs more often in developed countries. It is a severe and rapidly progressing cancer and often leads to death. The point is not only in the late diagnosis of the pathology, but also in its aggressiveness and ability to metastasize to other organs. This is due to the peculiarities of the blood supply to the liver.
All types of cancer are included in the International Classification of Diseases (ICD). Like other oncological pathologies, hepatocellular carcinoma also has its own special code. ICD-10 is used in all countries of the world. In the classification, the disease has code C22.0, which means “hepatocellular carcinoma.” Most often, this pathology occurs against the background of chronic pathologies, under the influence of unfavorable factors.
https://youtu.be/kpoQfdPK-Oc
Prevention
Several recommendations for the prevention of liver disease:
- Reduce alcohol consumption, give up alcohol-containing drinks and tinctures.
- Study the properties of dietary supplements before use, as some reduce blood clotting. A healthy liver produces coagulant substances, but cancer disrupts this function.
- Exclude from your diet foods containing preservatives, smoked foods, fried foods, and fatty foods.
Liver cancer can be prevented by vaccination against hepatitis and treatment of infectious and inflammatory processes.
Causes of liver carcinoma development
As is known, the etiology of malignant neoplasms has not yet been studied. However, scientists have long figured out exactly what factors provoke the development of a particular tumor. Hepatocellular carcinoma is no exception. The following influences lead to it:
- Long-term carriage of some viruses. It is believed that pathologies such as chronic hepatitis B and C increase the risk of developing liver carcinoma by more than 100 times. In addition, these diseases are often asymptomatic. Therefore, to reduce the risk of developing cancer, you should periodically donate blood for hepatitis viruses.
- Liver cirrhosis of any etiology. Replacement of hepatocytes with connective tissue most often occurs as a result of chronic viral infection, alcohol and drug use.
- Eating foods rich in aflatoxins.
- Genetic predisposition to the disease.
- Taking hepatotoxic drugs.
If the listed provoking factors are excluded, the risk of developing hepatocellular carcinoma is minimal. However, no one is immune from this tumor. Like other cancer pathologies, it can occur as a result of exposure to ionizing radiation, smoking, poor diet, stress, etc.
Origin
Hepatocellular liver cancer is a primary and secondary disease, formed from metastases of another tumor. Factors provoking the development of the disease:
- Increased bilirubin;
- Hepatic dysplasia;
- Dilated veins of the esophagus;
- Hepatitis B, C;
- Cirrhosis;
- Increased iron content in the body;
- Steroids;
- Oral contraceptives.
Liver cirrhosis
High aflatoxin B1 content is another reason. The substance is secreted by fungi of the genus Aspergillus, which infect plants such as peanuts. People suffering from diabetes and obesity are at risk. Elevated levels of insulin and cholesterol cause liver damage, against which the oncological process develops.
Pathogenesis of hepatocellular carcinoma
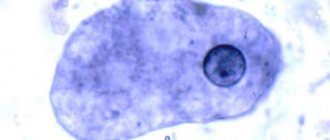
As a result of a chronic inflammatory process, normal liver cells begin to transform into tumor elements. What exactly leads to this is not known exactly. Due to the action of the virus, the liver tissue becomes inflamed, the organ becomes swollen and painful. The permeability of blood vessels increases, they become full-blooded. As a result, liver function is impaired. In addition to the fact that the organ is destroyed by viral particles, it is also affected by other harmful substances coming from food. All this leads to cellular transformation. The nucleus increases in size, the cytoplasm and other organelles shift to the periphery. After this, the cell begins to divide unmotivatedly. Many nuclei appear, metabolic processes in the hepatocyte are disrupted. Tumor proteins begin to be synthesized in the cell, which quickly spread through the bloodstream. Thus, hepatitis C and hepatocellular carcinoma are interrelated.
It should be remembered that this viral disease almost always leads to the development of liver cirrhosis or cancer. In most cases, it is diagnosed when complications occur. Another name for viral hepatitis C is the “gentle killer.” This is due to the complete absence of clinical manifestations of the pathology for many years and inevitable death as a result of cessation of liver function.
Surveys
Diagnosis of this disease is carried out using special clarifying techniques:
- General blood analysis . Allows you to identify an inflammatory malignant process in liver tissue by altered blood composition.
- Liver function tests . They represent a group of special tests aimed at studying and diagnosing the main functions of an organ.
- Determination of HBV/HCV antigens . This is a test designed to detect the hepatitis virus, which causes liver cancer.
- Determination of serum alpha protein (AFP) level. An analysis to detect the amount of this substance, which increases in the presence of cancerous damage to the organ.
Also, the well-known ultrasound method is used for diagnosis; what the disease looks like on the monitor screen is shown in this video:
https://youtu.be/Cznbl55-LlE
Classification of hepatocellular carcinomas
Hepatocellular carcinoma of the liver is divided into several morphological and clinical forms. In addition, the tumor is classified according to stage of development and severity. Depending on the macroscopic picture, nodular, massive and diffuse forms of liver cancer are distinguished. Fibrolamellar hepatocellular carcinoma is considered a separate type. According to the clinical picture, 6 forms of hepatocellular carcinoma are distinguished. Among them:
- Hepatomegalic variant.
- Jaundice form.
- A febrile variant of liver cancer.
- Ascitic form.
- Acute abdominal variant.
- Metastatic form of liver cancer.
Most often, a combination of several clinical variants is observed. The stage of hepatocellular carcinoma depends on the size of the tumor and its spread to nearby lymph nodes and other organs.
Stages
To assess the patient’s condition, doctors divide hepatocellular cancer into several stages:
- compensation stage – normal functioning of the liver;
- subcompensation stage – regular medical intervention is required;
- stage of decompensation - in order for the patient to live, constant treatment is needed.
To determine the prevalence of pathology in the body and the degree of its development, doctors use the following stages:
- The first is the formation of one to three solitary nodes with a diameter of about two centimeters. There are no vascular invasions at this stage.
- The second is that the solitary nodes are not enlarged, but vascular invasions or multiple malignant foci are formed in one lobe of the liver.
- Third - solitary nodes with a diameter of more than two centimeters grow. The nodes combine with vascular invasion and spread throughout the liver. Regional lymph nodes and adjacent tissues are also affected.
- Fourth, the cancer process spreads to the hepatic and portal veins, to the peritoneal wall, as well as to distant organs.
The sooner the pathology is identified and appropriate treatment is started, the greater the chance of a favorable prognosis.
Hepatocellular carcinoma: symptoms
Symptoms of the disease depend on the clinical form of carcinoma. In most cases, in the early stages, cancer has no symptoms. In addition, diagnosis is difficult due to the fact that the symptoms of the tumor resemble the clinical picture of other liver pathologies (chronic hepatitis, cirrhosis). Late manifestations of cancer include low-grade fever, loss of appetite, general weakness, swollen lymph nodes, and weight loss. With the hepatomegalic form of carcinoma, there is a pronounced enlargement of the liver and pain in the right hypochondrium. A third of patients have an icteric variant of the pathology. It has a poor prognosis. Jaundice develops in the first or second stage of the tumor process.
In addition, patients complain of pain and itching. In the febrile form, there is a constant increase in body temperature and an unpleasant, aching sensation in the upper abdomen. Ascites appears in the later stages of cancer and is accompanied by general symptoms of tumor intoxication. The acute abdominal form is less common. It is characterized by severe pain and tension in the abdominal muscles. In the metastatic version of hepatocellular cancer, signs of damage to other organs predominate. Among them are bones, lungs, and intestines.
Morphological forms of liver carcinoma
Based on morphology, the following forms of tumor are distinguished:
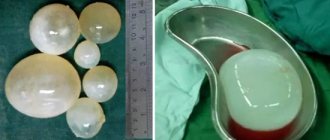
- Massive hepatocellular carcinoma. It occupies an entire segment or even a lobe of the liver. When cut, it has clear boundaries. Also, small foci (satellites) may be present inside the tumor node. One of the types of massive liver cancer is the cavitary form. The section reveals a tumor node, inside of which there is a brown liquid. The walls of the cavity are thick and smooth.
- Nodular carcinoma of the liver. It is characterized by many tumor foci located over the entire surface of the organ parenchyma.
- Diffuse liver carcinoma. Most often develops against the background of cirrhosis. The entire parenchyma consists of elements of connective tissue and atypical cells.
Fibrolamellar carcinoma consists of one or more large nodules. More often it is localized in the left lobe of the liver. The color of the tumor is yellow or green. Another separate form is considered to be encapsulated (small) hepatocellular carcinoma. It is characterized by a favorable prognosis and slow growth, the tumor size does not exceed 5 cm in diameter.
Diagnosis of hepatocellular carcinoma of the liver
Many tests must be performed before a disease such as hepatocellular carcinoma is diagnosed. Diagnosis of pathology consists of several stages. First, the doctor listens to all the patient’s complaints and conducts an examination. Particular attention is paid to the skin (color, scratches, hemorrhages), lymph nodes, and palpation of the liver. With cancer, the organ has a lumpy surface, a dense consistency, and pain is noted. After this, a series of examinations are performed. Among them:
- CBC, biochemical blood test.
- Determination of the level of a special marker - alpha-fetoprotein.
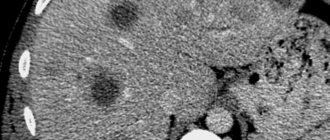
- Ultrasound of the abdominal organs.
- CT scan.
- Studies of liver vessels. These include angio- and portohepatography.
The diagnosis is made on the basis of cytological and histological findings. To conduct these studies, an organ biopsy is performed.
Hepatocellular carcinoma of the liver: treatment of the disease
The choice of treatment tactics depends on the morphological shape and size of the tumor, as well as the stage of the oncological process. In the initial stages of cancer, surgery, aspiration of nodular formations, and chemotherapy are performed. For diffuse tumors, hepatic artery embolization is performed. This helps slow down the growth of the tumor and limit the process. Hepatocellular carcinoma of the liver is insensitive to radiation treatments. In addition, it rarely responds to chemotherapy; only 15-20% of patients experience a temporary positive effect. One way is liver transplantation. This method is widespread in developed countries. Donor organ transplantation is performed only in the initial stages of cancer. In the presence of distant metastases, the only treatment option is symptomatic therapy. It includes palliative care (patient care, psychotherapy) and pain management.
Forecast
The prognosis for treatment of this type of liver cancer will directly depend on the stage of the pathology and the age of the patient. In the initial stages of the disease, after surgery, 80% of patients cross the five-year survival threshold.
Liver transplantation is successful in 85% of cases, but 17% experience organ rejection. Treatment in the final stages mostly produces unfavorable results. 30% survive for 5 years . For stage 4 these figures are even lower. As a rule, only 20% of patients manage to live more than 3 years.
In the absence of any treatment, liver cancer of the hepatocellular type develops rapidly, which allows a person to live for about 6 months.
If you find an error, please select a piece of text and press Ctrl+Enter.
Source: stoprak.info
Surgical treatment of liver cancer
Surgery is performed on almost all patients diagnosed with hepatocellular carcinoma. Treatment includes resection of the liver within the anatomical zone (segment, lobe, half of the organ). If the node is small in size, it is enucleated with a special aspirator. Another method of surgical treatment is percutaneous hepatic artery embolization.
The most effective way is to transplant an organ or part of it. Liver tissue has the ability to regenerate. As a result, a complete cure of the patient is possible.