Gastroenterologists around the world are very concerned about the sharp increase in reported cases of esophagitis. The availability of exotic foods (excessively spicy, deep fried, scalding hot or frozen, raw) becomes a common cause of inflammation of the esophagus. Mass consumption of alcohol and tobacco plays an important role in the spread of the disease. Esophageal esophagitis was declared a disease of the 21st century by a joint decision of doctors at an American symposium in 2001.
Types of esophagitis
The following types of esophagitis are distinguished:
- Catarrhal. With it, small spots appear on the walls of the esophagus.
- Hydropic. It is characterized by the formation of edema that interferes with the passage of food.
- Erosive. Erosion forms on the walls of the esophagus.
- Hemorrhagic. Characterized by the presence of hemorrhage.
- Fibrinous. Characterized by the formation of a fibrous film. Most often it occurs with diphtheria and scarlet fever.
- Necrotic. Formation of necrotic foci in the esophagus.
- Phlegmonous. The inflammatory process is more acute, with the formation of pus.
Fibrinous esophagitis, features
Fibrinous esophagitis is a special form of the inflammatory process in which the formation of a rather dense film is observed in the walls of the esophagus.
If the disease proceeds calmly, then removing this film using medical equipment is not difficult. There are situations when the disease progresses, while the film is pressed against the mucous membrane. Over time, it detaches itself, but erosion remains in its place.
Focal esophagitis is a consequence of infectious diseases - scarlet fever or diphtheria.
Causes and symptoms of the disease
Factors contributing to the development of the disease:
- Infectious diseases (scarlet fever, diphtheria).
- Non-compliance with diet. Eating fatty and too spicy foods.
- Bad habits (smoking and drinking alcohol).
- Esophageal hernia.
- Sedentary work and a predominantly passive lifestyle.
- Consequences of radiation therapy.
- Infections, fungi.
In order not to start the course of the disease and to receive medical help on time, you need to know the symptoms of the disease. With fibrinous esophagitis there is:
- Severe pain in the area behind the sternum. Gets worse when swallowing or eating.
- The patient may feel a gray film appearing in the mouth. These are the remnants of the film that enters the oral cavity directly from the esophagus.
- The swallowing process is impaired.
- The patient may cough up blood. This occurs due to bleeding ulcers on the walls of the esophagus.
- Heartburn often occurs, even after eating regular foods.
- Often there are attacks of severe pain, which can radiate to the heart or back.
- Nausea, vomiting, severe salivation.
- Belching, bad breath.
Cecum
Inflammation of the cecum (typhlitis) with its symptomatic manifestations is very similar to appendicitis, with the exception of the time of onset of pain. With typhlitis, pain occurs a couple of hours after eating in the iliac region.
Cecum
The patient should take his lifestyle seriously if inflammation is detected in the cecum, the symptoms of which are as follows:
- The appearance of blood impurities in the stool;
- Fatigue and general weakness;
- Anemia;
- Changing your usual bowel movement schedule;
- Sharp weight loss;
- Increased flatulence;
- Regular pain in the lower abdomen.
How to identify the disease
If the patient notices changes in his body that are similar to the first signs of the disease, he should immediately consult a doctor. The following activities will help to make a correct diagnosis:
- General blood and urine tests will determine the stage of the inflammatory process.
- Radiography allows you to track changes in the esophagus and detect a hernia or ulcer.
- Daily pH-metry. The procedure lasts 24 hours. Helps determine the level of gastric oxidation.
- Endoscopy. Determines the degree of the disease, the presence of erosions and edema.
- Biopsy. This is a test that requires taking a tissue sample.
- Diagnosis may consist of an initial examination of the oral cavity and palpation of the abdomen.
Possible complications due to untimely treatment:
- Heavy bleeding.
- Stomach ulcer.
- Scarring.
- Cancer.
Drug treatment
The first step to a cure is to determine the cause that led to the disease. Most often, the doctor prescribes one of the following medications to the patient:
- Almagel, Phosphalugel. They act as protection for the mucous membrane and relieve inflammation.
- Omeprazole, Pantoprazole. These drugs help reduce the acidity of the esophagus.
- Raglan, Cerucal. Helps normalize esophageal motility.
- Vikasol, Ditsinon. These drugs are prescribed in cases where there is hemoptysis. They help stop bleeding from the mucous membrane.
In severe cases, when medications do not help, urgent surgery is necessary.
Recommendations for nutrition in pathology
Nutrition for gastric hyperemia
Very often, hyperemia does not need to be treated, because this means that your body is trying to restore itself, it is self-regenerating. Hyperemia accelerates metabolism in tissues, but such a diagnosis is only normal if it is arterial hyperemia, but more often redness and swelling are harbingers of gastritis.
To treat and prevent the disease, folk remedies use herbal remedies and diets, as well as the diet of the Soviet scientist M. I. Pevzner. The Pevzner diet is a system of therapeutic tables that are differentiated according to various types of diseases. Pevzner's diet No. 1 is intended for people suffering from gastritis and ulcers. It is also prescribed during the recovery period after surgery and for duodenal ulcers.
Hard-to-digest foods, as well as foods that actively irritate the mucous membranes, are completely excluded from the diet. Those who adhere to this diet eat a menu consisting of berries and fruits, condensed milk and cream, rice, buckwheat, oatmeal, fish and poultry. All products included in this dietary table must be used either stewed or steamed. In any case, it is forbidden to eat fatty meat, salted fish, fresh baked goods, hot dishes and dairy products that increase acidity.
Lifestyle and diet for fibrinous esophagitis
If we are talking about the initial stage of the disease, then you can get by with a diet and certain innovations in a person’s lifestyle.
- In the first couple of days, this may be fasting combined with taking certain medications.
- The patient should sleep in such a position that the head is elevated. This is done in order to prevent reflux (belching, heartburn) back into the esophagus.
- You can’t carry heavy objects, you need to bend over less often.
- Meals should be no later than an hour and a half before bedtime.
- Physical activity should be reduced.
Complications, consequences
Belching, heartburn, periodic difficulties with swallowing food, cough of non-cold origin, pain radiating to the back... Do we often pay attention to them? Many will probably answer in the negative. Meanwhile, you should never ignore these seemingly harmless symptoms and neglect treatment. The consequences of a negligent attitude towards one’s health will not slow down in the form of serious and sometimes incurable diseases:
- Peptic ulcer;
- Reducing the lumen of the esophagus (so-called stenosis);
- The appearance of bleeding;
- Cicatricial narrowing of the esophagus;
- Malignant neoplasms;
- Death due to asphyxia.
Treatment with folk remedies
It is possible to use folk remedies. It cannot be said that such treatment is effective, but it is excellent as a preventive measure. A course of therapy correctly drawn up by the attending physician can be used in parallel with folk remedies. But only after consulting a doctor.
Examples of home therapy:
- Flax seeds. Their mucus envelops the esophagus, thereby preventing the formation of a fibrinous film and erosion, and reduces acidity. To prepare a healing decoction, just boil one teaspoon of seeds in half a glass of water. You need to take the decoction for up to a week .
- Chamomile. Prepare a special herbal mixture of chamomile, lemon balm, and licorice root. You need to take this decoction about 4 times a week. Chamomile will help relieve inflammation and swelling.
- Dill. Pour boiling water over the ground dill and leave for about two hours. Drink the infusion before meals.
Prevention measures
The best preventive measures are based on a healthy lifestyle. You need to avoid such provocateurs as:
- Spicy and fatty foods.
- Food too hot.
- Bad habits (alcohol and smoking).
- Overweight.
- Products with a high degree of acidity.
- Uncomfortable and tight clothing.
Fibrinous esophagitis is a process of inflammation of the esophagus in the mucous membrane area. In this case, swallowing functions are impaired, heartburn and pain behind the chest appear. For 40% of cases, it does not cause serious symptoms during development. It is typical for all ages, but also occurs in children less than a year old. In rare cases, it occurs independently, but is more often accompanied by other disorders of the digestive system. It occurs in both women and men; in the latter it happens more often, given their lifestyle and bad habits.
Reviews
Dear readers, your opinion is very important to us - therefore, we will be glad to receive feedback about your experience in treating the esophageal mucosa in the comments, this will also be useful to other users of the site.
Agnia, Vologda
“As a gastroenterologist told me, reflux esophagitis cannot be cured, but by following certain rules, you can avoid exacerbation for a very long time: you need to sleep on a bed with a raised headboard (I built a similar structure from pillows - it works great), after eating, walking quietly for half an hour and , the main thing, if you are being treated with herbs, is to make sure that they do not have a choleretic effect. Fried and fatty foods are also not allowed, soda, coffee. It helps me - in two years I had heartburn three times, and even then it was not severe.”
Inna, Tomsk
“I cope with heartburn with oatmeal jelly according to Izotov. The taste, of course, is specific, but the main thing is the result, and it suits me quite well. And it’s safe, unlike pills.”
Causes
Esophagitis is caused by internal (endogenous) and external (exogenous) factors affecting the mucous membrane.
Exogenous ones include:
- Chemical – irritating foods, alcohol, medications, etc.
- Thermal – excessively heated foods and liquids. The burn becomes chronic if the temperature exposure occurs constantly.
Endogenous factors are typical for most cases. They are associated with a weakening of the sphincter at the bottom of the esophagus - the cardia. It is caused by reflux (reverse flow - lat.). If the cardia does not perform its functions, the contents of the stomach cause irritation from the effects of digestive enzymes and hydrochloric acid, partially returning to the esophagus.
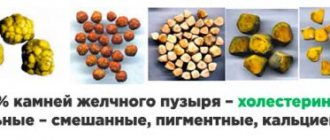
Reflux is caused by various diseases of the stomach - ulcers, hiatal hernia, the formation of gallstones, tumors in the peritoneum, scleroderma of a systematic nature. It is also promoted by pregnancy, weight gain, tube feeding, and damage resulting from abdominal surgery. Reflux itself is not a deviation from the norm - it is a normal physiological process; during digestion, this phenomenon occurs up to 30 times, and a person does not feel discomfort. The disease occurs when the protective functions of the body are disrupted - weakening of the lower sphincter of the esophagus, insufficient blood supply, damage to the mucous membrane.
Another cause of occurrence is infectious diseases affecting the esophageal mucosa.
The gastric mucosa is hyperemic - what does this mean?
It is worth noting the fact that the stomach is one of the most important and functional internal organs in the human system, and therefore diseases of this organ can unsettle the daily life of a modern person for a long time.
In cases of more advanced diseases, they bring with them warnings of the transformation of prolonged varieties and the multiplication of various bacteria in the stomach, because it is for them that such environments are the most favorable. It is in such cases that each symptom worsens and persistent pain syndromes may occur.
What is moderate gastric mucosa and how can one get sick of it?
Very often, during various examinations of the stomachs of each citizen, the doctor may discover that the gastric mucosa is hyperemic, therefore, questions arise about what it is? It is these terminologies that are used when there is an excess of blood in each vessel of all the linings of the stomachs of each person.
Arterial hyperemia is called active, because every artery and small arteriole that carries blood in the stomachs of people can be detected with increased blood flow into each of its stripes. In cases of venous hyperemia, that is, passive, there cannot be moderate blood outflows from each vessel of the membranes of the food organs of each citizen.
They arise as a result of ordinary root causes or during pathological movements. With moderate increases in the rate of each metabolic movement, the number of each capillary in an individual organ that fills with blood increases significantly. Sometimes, as a result of each warm action, similar actions are achieved in an unnatural way to include all vessels in the general vascular microcirculatory beds.
Damage to the functioning of the stomach and diseases of the mucous membrane of this organ.
Any damage to the action of each smooth muscle of the vessel can lead to excessive blood filling, in cases where the gastric mucosa of people with excessive saturation with blood is moderately reddened, because in its normal form it should be pink.
The results of thrombosis of each vein or narrowing during venous hyperemia can be the concentration of excess fluids through each partition of the blood capillary in the media between the cells, which excite different concentrations of tissue fluids. This is how mucous swelling begins to form, and ultimately each nearby tissue becomes hypoxic.
When mucous membranes appear, any stain appears through the mucous membranes. Subsequent development of pathologies can lead to any inflammatory phenomenon; an intense colored spot appears through each main cell of the human stomach.
Various causes of atrophy of the gastric mucosa.
Very often, atrophy of the mucous membranes of people’s stomachs manifests itself and develops in a person who is no longer young, that is, old; as a result, bacterial gastritis can form. There are some spectrums of motivators that can aggravate the situation of the mucous membranes, in cases of influence by joint forces.
These motivators are the actions of pathologies, age-related changes in bodies, and there is no need to turn off the probable inclinations of genetics. Systematic non-compliance with every basic healthy diet, alcohol abuse and frequent use of each drug that form gastritis, for example, there are substances that provoke regression of the mucous membranes.
There are a huge number of cases of atrophy of the gastric mucosa, which may well be caused by such influences as: non-stop nervous anxiety, the consequences of diseases of the endocrine systems (diabetes mellitus), deficiencies in iron bodies. Thus, we can say with confidence that we are dealing with pathology, which requires urgent and professional intervention from a specialist.
What can be considered the most basic signs of atrophy of the gastric mucosa?
With atrophic gastritis, the efficiency of the stomach is greatly deteriorated, and the main symptom includes dispersion syndromes: decreased appetite in patients, belching, typical smells of rotten food, detection of gag reflexes.
Very often, patients suffer from heavy stomachs after eating, drooling and unpleasant tastes. Rumbling, bloating and acute aversions to fermented milk products, all this can lead to dysbacteriosis. Each painful sensation during atrophy can be characterized by dull, itchy localizations.
Thus, it is worth noting the fact that after the process of treating atrophy has already been completed, former patients often practice a strict diet regarding this disease so that the walls and hyperemic gastric mucosa are not irritated and the most effective methods are created for the fastest healing and eliminating the consequences of the disease mentioned above in this article of our resource.
What is atrophy of focal gastric mucosa.
The gastric mucosa is focally hyperemic and has some dangers that disappear when symptoms are not expressed in cases where pathologies do not develop into dangerous forms until it crosses the area of the mucous membranes of the stomachs of each person. It is worth noting that there are several types of lesions, which exist in different shapes and sizes, located at each stage of the disease course. With timely diagnosis, it is possible to begin treatment at the initial stages, which can give positive results.
The local mechanism of ulcer formation of each body of the stomach can include a decrease in protective mucous barriers as a result of inflammation of the mucous membranes, disruption of mucin formation, regeneration of epithelium, blood flow and local prostaglandin synthesis. One can attribute the slow and irregular evacuations of their contents, the gaping of the gatekeepers.
Antral mucosa and its atrophy
It is the antrum of the stomach that is the spaced parts that combine and crush food, slowly pushing food through the pyloric sphincters. In normal activities, subacidity in them is reduced. Diseases of the antrum of the stomach include, first of all, antral focal gastritis, which are types of pathologies in which iron loss occurs, responsible for the production of hydrochloric acids and pepsins.
Deficiencies in the mucus are discovered that protect each wall of all human stomachs from their acidity, increasing the likelihood of inflammation in each other section. It is worth noting the fact that in the antrum the epithelium has a paler appearance than the body of the stomach. A completely different picture is observed in cases where the organs are diseased.
In cases of more advanced diseases, they bring with them warnings of the transformation of prolonged varieties and the multiplication of various bacteria in the stomach, because it is for them that such environments are the most favorable. It is in such cases that each symptom worsens and persistent pain syndromes may occur. Dysbiosis, pancreatitis and anemia may develop.
The importance of endoscopic examinations
These studies play a huge role, because they help identify ulcerative defects and provide control over scarring of ulcers, and collect materials for biopsies. There are three degrees of this study: in the first, severe inflammation, which is characterized by edematous gastric mucosa, moderately hyperemic, it should also be noted that swelling can be spotty; the second degree is characterized by the fact that the mucous membranes are diffusely edematous, and the gastric mucosa is also hyperemic.
Some more news:
bolzheludka.ru
Classification
Occurs in acute or chronic form. They are distinguished depending on the causes of occurrence:
- nutritional – from the effects of food intake;
- allergic – from the influence of various allergens;
- stagnant – due to stagnant processes in the body;
- professional – associated with a person’s professional activity and exposure to harmful and dangerous factors associated with working conditions in production;
- infectious – from the effects of the above-mentioned infectious diseases.
The role of fibrin in inflammation
Fibrin production and inflammation are two closely related processes. Protein plays an important role in contact with deteriorating, damaged tissue. Thrombokinase released from the tissue comes into contact with fibrinogen.
When blood clots, all toxic substances become clogged in the clot. This feature of the effect of protein during the inflammatory process protects the body from the further spread of toxins and their negative effects. This reaction is called fixation. Thus, fibrin is also a protector of the body from toxins.
Symptoms of the disease
Different types have their own characteristics, but the common symptoms are heartburn, pain in the back of the sternum. Eating is not always associated with unpleasant symptoms. The pain is constant or short-term, and can be aching or severe. Belching, nausea, vomiting, difficulty swallowing food, and difficulty passing food are also noted. Symptoms worsen when lying down, a cough not caused by lung disease, and shortness of breath occur.
The acute form is characterized by a decrease in body tone with an increase in body temperature, intestinal inflammation, etc. In the chronic form, temporary improvements or exacerbations are possible. During the remission stage, symptoms become less pronounced without disappearing.
Causes of inflammation of the large intestine
The main cause of colitis is functional or morphological changes that occur in the intestinal mucous tissues. As a rule, the lesion appears as a result of bacterial dysentery, helminthic infestation, severe poisoning, and the constant presence of foci of chronic infection in the gastrointestinal tract.
Factors that may contribute to the development of inflammation:
- hereditary predisposition;
- poor nutrition;
- congestion in the pelvic area and impaired blood supply to the intestines;
- vital activity of parasites;
- dysbacteriosis;
- long-term use of antibiotics;
- weak immunity;
- physical exhaustion;
- nervous overstrain.
Against the background of favorable factors, when for one reason or another the protective functions of the intestine are reduced, exposure to the pathogen leads to damage to the mucous cells lining the walls of the colon from the inside. A focus of inflammation develops, which at first may exist asymptomatically.
If acute colitis occurs for a long time with a blurred clinical picture, the inflammation can progress to the chronic stage. It is important to promptly identify the primary disease, paying attention to even minor signs of pathology. Acute colitis responds well to treatment, but in the absence of adequate therapy and chronicity of the process, the disease becomes long and painful.
Symptoms of colon inflammation
Acute colitis can occur violently, with pronounced general and local symptoms:
- bloating;
- pain;
- discharge of mucus from the anus;
- purulent-bloody impurities in feces;
- frequent painful urge to defecate;
- diarrhea.
These manifestations are often accompanied by general malaise, vomiting, fever, weakness, and weight loss. Such pronounced signs force the patient to consult a doctor and carry out timely diagnosis.
When examining the colon, the following is revealed:
- swelling of the mucous membrane;
- thickening and hyperemia of the walls of the affected area of the intestine;
- secretion of large amounts of mucus, and sometimes purulent discharge;
- erosion and ulceration of the mucous layer;
- minor hemorrhages.
A clinical blood test demonstrates elevated ESR and leukocyte counts.
Another picture of the disease is possible. For several weeks, the patient may experience problems with loose stools, gurgling and discomfort in the abdomen, and other local symptoms. But, since they are insignificant, the patient does not attach importance to them for a long time and does not associate them with a serious inflammatory process. During the period of latency, colitis becomes chronic.
Signs of chronic inflammation of the colon
Chronic colitis, in addition to inflammation of the mucous membrane, acquires other unpleasant manifestations. Changes occur in the intestinal walls themselves: they shorten, and a narrowing of the lumen occurs in the affected area. The blood supply to the diseased area is disrupted, superficial ulcers become deeper and go deeper into the muscular layer of the intestine, suppuration develops, and neoplasms - pseudopolyps - may appear.
A blood test gives a clear picture of inflammation (severe leukocytosis), a large amount of leukocyte mucus is also detected in the feces. The results of the coprogram show the presence of pathogenic flora and red blood cells.
The patient notes the following symptoms:
- problems with stool: frequent diarrhea, constipation, their alternating combination;
- pain throughout the abdomen without specific localization;
- frequent unproductive urge to go to the toilet with the release of mucus streaked with blood instead of feces;
- increased gas formation and constant bloating;
- foul-smelling stool.
The general health of the patient can be either quite satisfactory or extremely uncomfortable. Abdominal pain is aggravated by nausea, belching, lack of appetite, and a bitter taste in the mouth. Against the background of weakness and malaise, performance decreases, irritability and nervousness appear.
Types of disease
Colitis is the general name for inflammatory diseases of the large intestine, which includes a number of individual diagnoses. Colitis is divided into types depending on the cause and specific manifestations of a particular pathology.
Nonspecific ulcerative colitis
One type of chronic inflammation of the colon is nonspecific ulcerative colitis. The etiology of this disease is not fully understood. It is associated with a defect in the immune system, as a result of which irritants that normally do not cause any reaction in a healthy body provoke severe inflammation in a patient with ulcerative colitis. One of the hypotheses for the origin of the disease is genetic predisposition.
According to statistics, this pathology is more often diagnosed in young women from 20 to 40 years old, mainly in urban residents, which may indirectly indicate the influence of environmental factors and lifestyle on the pathogenesis.
Nonspecific ulcerative colitis is expressed in hemorrhagic inflammation of the colon with the following manifestations:
- severe pain, more often in the left half of the abdomen;
- chronic constipation;
- low-grade fever;
- discomfort in the joints;
- bleeding from the rectum;
- discharge of blood and pus from the anus.
Over time, these symptoms become less pronounced, forming a state of remission, but with exacerbation of the disease, the patient’s condition becomes serious. He suffers from pain, diarrhea, anemia and physical exhaustion develop due to blood loss.
Nonspecific ulcerative colitis is extremely dangerous due to its complications:
- formation of intestinal expansion;
- the occurrence of internal bleeding;
- the possibility of perforation of the intestinal walls;
- risk of peritonitis;
- creating conditions for the development of oncology.
Spastic inflammation of the large intestine
Based on the name of this pathology, it is logical to assume that it is based on intestinal spasms. And this is indeed true: contractions of the intestinal walls of varying strength and frequency lead to the appearance of unpleasant symptoms in the patient:
Spastic colitis refers to functional disorders, that is, in fact, it is not a severe pathology. The reason for it lies in the psychological and neurological planes. Involuntary spasms most often appear against the background of stress, chronic fatigue, physical and nervous overstrain, and shock. This disease is treated by relaxing the smooth muscles of the intestines, and most importantly - with restoratives and sedatives.
Pseudomembranous colitis
Pseudomembranous inflammation is the result of intestinal dysbiosis with uncontrolled proliferation of opportunistic microorganisms.
This form of colitis develops while taking antibiotics, which upset the balance of intestinal microflora in favor of potentially dangerous microbes.
Symptoms accompanying pseudomembranous colitis:
- Diarrhea that appears during antibacterial therapy, especially when treated with tetracycline drugs. If, a few days after the end of the course, normal stool is restored, a mild form of colitis is diagnosed.
- Moderate inflammation is characterized by persistence of diarrhea after discontinuation of antibacterial drugs. The stool is watery, containing mucus and blood. Abdominal pain, worse during defecation. There is a frequent urge to go to the toilet, including false ones, when bowel movements do not occur. Signs of intoxication appear and increase: fever, chills, weakness, nausea.
- Severe pseudomembranous colitis is a critical condition in which intoxication of the body and local symptoms are accompanied by serious complications in the form of cardiac dysfunction (tachycardia, drop in pressure), the development of electrolyte imbalance, and metabolic failure.
Enterocolitis
Enterocolitis is a disease that combines an inflammatory process in the large intestine with damage to the gastric mucosa. Acute enterocolitis occurs in response to an infection or non-infectious exposure: allergens, chemicals, poisons, food poisoning. Primary inflammation develops suddenly:
- cramping abdominal pain;
- bloating and rumbling;
- nausea, possible vomiting;
- severe diarrhea.
If enterocolitis is of infectious origin, dyspepsia is accompanied by blood and mucous impurities in the stool, increased body temperature, and a state of intoxication. When palpating the abdomen, pockets of pain are identified, and a heavy coating appears on the tongue.
Treatment for acute enterocolitis:
- Symptomatic – pain relief with antispasmodics.
- Reducing the load on the gastrointestinal tract - liquid diet for 2 - 3 days.
- In case of poisoning, it is necessary to rinse the stomach.
- To avoid dehydration in case of severe diarrhea and vomiting, control the flow of fluid into the body and take Regidron.
- If an intestinal infection is detected, antibiotic therapy is prescribed.
- Intoxication is eliminated through detoxification treatment.
Untreated inflammation can transform into a chronic disease. In this case, superficial damage to the mucous membranes develops further and penetrates deep into the intestinal walls and into the submucosal layer of the stomach. The course of the disease is characterized by periods of exacerbations and remissions; over time, persistent disturbances of intestinal function are formed.
Colon ischemia
Ischemic colitis is a form of intestinal inflammation caused by impaired blood supply to the colon. The lesion can occur in any area, but more often it is the area of the splenic curvature, less often the sigmoid colon, descending or transverse colon becomes inflamed.
Poor blood circulation leads to limited nutrition of the intestinal walls, as a result of which foci of ischemia arise in them. Symptoms of this condition: episodic pain in the epigastrium that occurs after eating, diarrhea and bloating after meals, and sometimes vomiting. Over time, there is a loss of body weight.
In case of acute disruption of blood supply associated with blockage of blood vessels, necrotic processes occur, which are expressed by:
- sharp pain localized in the left side of the abdomen;
- signs of intestinal obstruction;
- bleeding from the anus;
- development of peritonitis.
Treatment of inflammation of the large intestine (lower section)
Treatment for colitis depends on the specific diagnosis and severity of symptoms. If mild inflammation caused by poisoning can go away in a few days as a result of gastric lavage, taking sorbents, drinking plenty of fluids and diet, then more serious illnesses require a longer and more serious approach, often in a hospital setting.
Lack of proper treatment can lead to dangerous complications: intestinal obstruction, peritonitis, liver abscess. To avoid unpleasant consequences, if signs of inflammation of the colon occur, you must consult a specialist - a proctologist or gastroenterologist. You especially need to hurry if the symptoms arose against the background of an infectious disease or immediately after it, as a result of food poisoning, chemical poisoning, or taking medications.
Diet for colitis
For any form of colitis, a strict therapeutic diet is indicated. More often, patients begin to follow it on their own, intuitively relieving the gastrointestinal tract. The doctor prescribes table No. 4, which excludes foods that provoke fermentation and putrefaction in the intestines. Nutrition for colitis involves avoiding foods that irritate the mucous membranes: spicy, salty, fatty, fried foods, sour foods, spices, milk.
Vegetables, fruits, berries, and sweets are temporarily prohibited. Food should be liquid or semi-liquid, pureed, at a comfortable temperature - neither hot nor cold. A gentle regimen should be followed throughout the treatment and for some time after it. At the beginning of the disease, it is better to completely refuse food for a couple of days and limit yourself to drinking plenty of fluids.
Therapeutic enemas
Enemas for colitis are done only as prescribed by a doctor if it is necessary to rinse the intestines from infectious agents and contents, direct delivery of medicinal substances to the mucous membrane.
- Antiseptic enemas with infusions of chamomile, calendula, and collargol help relieve swelling and hyperemia, soothe the mucous membranes, and destroy pathological microflora at the local level.
- The introduction of sea buckthorn oil into the colon promotes healing and restoration of the mucous membrane.
In case of intestinal inflammation, prolonged sitting is contraindicated. Lack of movement provokes congestion in the colon area, leading to poor blood supply to the walls, poor peristalsis, causing constipation and fecal intoxication.
To activate the intestines and restore blood circulation, feasible physical activity is necessary: walking, high knee raises while standing, Kegel exercises, etc. Simple exercises can be done even while in bed.
Drug therapy
Taking medications for colitis depends on its form and is prescribed only after the diagnosis has been clarified and its cause has been established:
- Antibiotics, sulfinamides, antiviral drugs, antiparasitic drugs are indicated when a pathogen is detected: a virus, infection, worms, protozoan microorganisms, etc.
- In case of pseudomembranous colitis, antibiotics, on the contrary, should be stopped.
- To relieve spasms and pain, no-shpu is prescribed in tablets or injections, rectal suppositories with papaverine.
- In case of poisoning, signs of intoxication, or infections, enterosorbents (Polyphepan, Enterosgel) are recommended.
- To relax the intestinal walls and eliminate constipation, you can take antihistamines - Bicromat, Intal and others, only as prescribed by a specialist.
- In case of dehydration, sodium chloride solution is administered intravenously.
- Loose stools are fixed with the help of astringent drinks: decoctions of oak bark, pomegranate peel, chamomile, and St. John's wort.
- For nonspecific ulcerative colitis, necrotic and erosive damage to the mucosa, treatment is carried out with suppositories with methyluracil, sea buckthorn oil, and other healing drugs.
- In severe cases of inflammation, glucocorticosteroids (hydrocortisone, betamethosone and others) are prescribed.
- To restore the intestinal biocenosis, it is recommended to take probiotics.
Surgical treatment of inflammation of the large intestine
Surgical intervention for inflammation of the colon may be necessary if complications develop (perforation, peritonitis), necrotic processes, obstruction of the intestinal lumen, obstruction, or spread of infection to surrounding tissues.
Sluggish colitis, which does not respond to conservative therapy, serves as a permanent source of infection and poor condition of the patient, is also recommended to be eliminated through surgery. Nonspecific ulcerative colitis often requires intervention.
Maintenance therapy for chronic colitis
In case of chronic proctitis without exacerbations, it is recommended to carry out general strengthening and preventive measures in sanatorium-resort conditions:
- mud treatments;
- radon baths;
- mineral water treatment;
- massotherapy;
- gymnastics;
- physiotherapy.
Treatment of inflammation of the large intestine requires a long-term and comprehensive approach to prevent relapses, and in the acute form, transition to the chronic stage. Under no circumstances should you take medications on your own or ignore the symptoms of inflammation. If you experience complaints that do not go away within 2-3 days, you should consult a doctor.
Intestinal inflammation
The intestine is considered one of the most important elements of the gastrointestinal tract, consisting of the large and small intestines, and the duodenum.
The main purpose of this organ is to digest food and break it down into elementary compounds through digestive enzymes. Intestinal inflammation, the symptoms and treatment of which are extremely unpleasant and long-lasting, is considered one of the most common diseases of the gastrointestinal tract, regardless of gender and age.
Inflammatory processes in the intestines arise as a result of various causes, divided into several groups:
- Infections. Inflammation occurs as a result of various bacteria entering the intestines - salmonella, shigella, E. coli; viruses, as well as protozoa;
- Parasites;
- Autoimmune processes. This is a special situation in which the immune system sees the cells of the intestinal mucosa as foreign and begins to produce antibodies to fight against them, resulting in inflammation;
- Genetic disposition. Some intestinal diseases and congenital enzyme deficiencies can be inherited;
- Non-compliance with the diet. Excessive consumption of smoked, salty, fatty foods, overeating can cause inflammation of any part of the gastrointestinal tract, in particular the small intestine and duodenum;
- Inadequate blood supply to the vessels passing through the intestinal walls as a result of atherosclerotic changes and thinning of the artery bed;
- Changes in healthy microflora. Inflammation of the intestinal mucosa occurs due to the dominance of pathogenic flora.
Causes
Diagnostics
Only a doctor can make a correct diagnosis, so it is important to consult a doctor if symptoms appear. The acute form of the disease does not present difficulties in making a diagnosis, but more often diagnostics requires research:
- endoscopic examination - the presence of damage in the mucous membrane is established;
- X-ray of the esophagus and stomach;
- esophagoscopy;
- histology of mucosal biopsy – required to clarify the diagnosis;
- esophagomanometry. Motility disorders of the esophagus characteristic of the disease are determined.
Treatment
Treatment is carried out depending on the nature of the disease, it is important to eliminate the cause of the disease, otherwise complete recovery is impossible. In the acute form, a diet is prescribed that reduces inflammation. Reduce the consumption of foods that negatively affect the mucous membranes, carbonated drinks, and alcohol. If the acute form of the disease is mild, abstinence from food will be required for up to 2 days. For serious inflammation and infection, antibiotics are prescribed.
If the disorder is caused by reflux, it is recommended to reduce physical activity, bending, and abdominal tension. Traditional methods of treatment are used. When sleeping, your body should be elevated. Drugs are prescribed that reduce spasms in the esophagus and envelop.
If the methods are not successful, surgical intervention is indicated, especially in the presence of acute forms and complications. Diet, lifestyle, and diet contribute to recovery from the chronic form of the disease.
Prevention
For prevention, paramount importance is given to eliminating the influence of factors leading to the occurrence and development of the disease. Refrain from smoking and drinking alcohol. Avoid eating junk food. It is advisable to reduce weight.
Timely consultation with a doctor is important. Any disease, including this one, is much easier to overcome if preventive measures are taken. You should lead a healthy and active lifestyle.
Hello! My daughter is 12 years old. A week ago she suffered from scarlet fever, and her health has improved. For the past 3 days she has been bothered by acute pain in the chest while eating. We went to the doctor, and after an endoscopic examination he was diagnosed with fibrinous esophagitis. Please tell me, could this be a consequence of scarlet fever? Will we be able to cure the disease completely, or will there be consequences?
Fibrinous esophagitis develops acutely, specific symptoms are minimal, therefore, without additional research, it is difficult to make a diagnosis even for an experienced doctor. But still, this form has some features, which allows you to choose the right treatment tactics.
Hyperemic gastric mucosa - what to do?
What should you do if in the description of the examination the doctor wrote about hyperemic gastric mucosa?
The medical term hyperemia means redness and swelling. In itself, hyperemic mucosa is not dangerous - it is just a symptom that signals that the stomach is sick.
What diseases does hyperemic mucosa indicate?
The stomach lining becomes red and swollen because the blood vessels in the walls of the organ become overfilled with blood. It is not for nothing that in the old days this condition was called “plethora.”
Excessive filling of blood vessels with blood can be due to two reasons:
- due to impaired blood flow from the stomach;
- due to excess blood flow into the stomach.
The first type is called venous or passive hyperemia, the second - arterial or active. There is a significant difference between active and passive hyperemia.
Only active action leads to tissue healing, while passive action, on the contrary, contributes to further damage to the organ due to lack of oxygen in the tissues.
The gastric mucosa becomes hyperemic in most diseases of the gastrointestinal tract.
Based on the condition of the mucous membrane and the location of redness and swelling, the type of disease can be determined.
Most often, hyperemia is diagnosed as one of the types of gastritis, but it can be a symptom of duodenitis, stomach ulcers, or diseases of organs that are not related to the gastrointestinal tract at all.
Normally, the gastric mucosa should be pink, shiny, and well reflect the light of the endoscope.
The folds of healthy mucosa are 5–8 mm thick; when air is blown in, they straighten well, allowing the doctor to view all parts of the organ through an endoscope.
The thickness of the folds increases closer to the pylorus. In the antrum, the epithelium is slightly paler than in the body of the stomach. A completely different picture can be observed if the organ is sick.
With superficial gastritis, the gastric mucosa is moderately hyperemic. Redness can be either focal or diffuse.
The mucous membrane is swollen, white foam is visible on its surface. The folds of the stomach are thickened. When air is blown into the stomach through a probe, the folds do not straighten completely.
With atrophic gastritis, the mucous membrane is not hyperemic, but on the contrary, it is thinned and has a pale color.
The atrophic zone is located locally, in one of the sections of the stomach. The folds in this zone are thin, and the vascular pattern is clearly visible on them.
The mucous membrane is severely hyperemic with fibrinous gastritis. In addition to hyperemia, purulent manifestations are visible in the stomach.
Fibrinous gastritis begins as a result of a severe gastric infection caused by measles, scarlet fever or other infectious diseases.
With this type of gastritis, the patient vomits blood - this is how the purulent film is rejected from the mucous membrane.
With phlegmous gastritis, the mucous membrane is focally hyperemic. Phlegmous gastritis appears as a result of an object traumatic to the mucous membrane, such as a fish bone, entering the stomach.
With bulbitis, hyperemia is concentrated in the antrum and duodenal bulb. The folds of both organs are thickened, the mucous membrane looks reddened and swollen.
Bulbitis begins due to poor nutrition or infection of the gastrointestinal tract with Helicobacter pylori bacteria.
The mucous membrane can be hyperemic not only in diseases of the gastrointestinal tract.
For example, during an examination of the stomach in patients with renal failure, it was discovered that 90% of patients had various pathologies in the condition of the gastric walls, including hyperemic mucosa.
Treatment of the stomach with hyperemic mucosa
Actually, hyperemia does not need to be treated in any way. This is a beneficial process, indicating that the body is trying to heal itself.
Hyperemia helps accelerate metabolic processes, which leads to tissue restoration and healing.
In some cases, doctors even artificially induce blood flow to a diseased organ in order to speed up its recovery.
With a little thought, everyone can give an example of the use of hyperemia for medicinal purposes.
These are cups and mustard plasters, with the help of which you can cause a rush of blood to the inflamed bronchi and lungs, thus speeding up their recovery.
Most often, redness of the mucous membrane indicates one or another form of gastritis. This disease is a consequence of errors in nutrition or the result of colonization of the gastrointestinal tract by pathogenic bacteria of the Helicobacter genus.
Treatment of gastritis consists of a set of measures: a special diet and medication, including antibiotics (if Helicobacter pylori infection is detected).
When the cause of the redness of the epithelium is discovered, the doctor will prescribe treatment aimed at eliminating the disease itself.
After curing gastritis, ulcers or other ailments, the gastric walls will independently acquire normal color and thickness.
Hyperemic epithelium can be a consequence of not only inflammatory processes. The mucous membrane turns red due to problems in the person’s mental state.
Chronic stress, prolonged depression and fear cause a rush of blood to the stomach walls, causing them to become red and swollen.
Gastroenterologists warn that often problems with the gastrointestinal tract do not have an anatomical or infectious basis, but are only a consequence of a person’s severe psycho-emotional state.
You can find out that the walls of the stomach are red and swollen from the inside only after a special examination - gastroscopy.
During this study, a flexible probe with a miniature video camera at the end is inserted into the organ.
Such equipment allows the doctor to see on the monitor screen everything that is happening in the gastrointestinal tract, and, if necessary, to take a sample of the epithelium for analysis or carry out local therapeutic measures: remove a polyp, inject medicine into the affected area of the organ.
Gastroscopy is a painful and unpleasant examination for the patient, but it is absolutely necessary, as it allows the most accurate diagnosis to be made.
The patient needs to strictly adhere to the prescribed treatment, only in this case can one count on its success.
Very often they try to treat stomach ailments on their own, using traditional methods, relying on herbal remedies, honey, special diets, etc.
Indeed, traditional medicine has accumulated vast experience, but it should only complement the treatment prescribed by a specialist, and not replace it.
Before starting any herbal treatment, you should always consult your doctor.
Video:
As for diets, for hyperemic mucous membranes it is best to adhere to the therapeutic diet developed by Professor Pevzner: if necessary, the gastroenterologist will definitely recommend one of his diets.
Errors in nutrition and stress have long become the norm for modern city dwellers.
So is it any wonder when the doctor writes on the examination form that the epithelium in the stomach is hyperemic, that is, red and swollen? This means that the patient will have to be treated for gastritis or some other stomach ailment.
protrakt.ru
When does the disease occur?
- Inflammation in the distal parts of the esophagus occurs after scarlet fever, diphtheria. The lesion can be primary, that is, it begins in the esophagus, or secondary, that is, it enters the organ through the bloodstream.
- Fungal infections are a risk factor.
- In adults, this condition can occur after radiation therapy, with blood diseases, and malignant neoplasms.
- The presence of reflux (reflux of gastric contents into the esophagus) additionally injures the mucous membrane of the distal section.
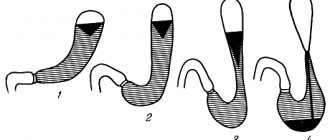
Differences from other forms of esophagitis
Esophagitis combines inflammatory processes of the esophagus, but changes in the organ itself can be different, depending on the cause of the disease, the presence of reflux. In the fibrinous form, films form on the walls of the esophagus; in most cases, they are easily removed, since they are associated only with the mucous membrane. This disease is also called pseudomembranous esophagitis.
In severely ill patients, fibrin plaque grows into the submucosal ball, firmly connecting to the esophagus. After removing the films, erosions and shallow ulcers remain that bleed for a long time. Treatment in this case will be aimed at speedy healing of the defect. The result of reflux in the distal esophagus is catarrhal (superficial) inflammation.
Fibrin and inflammation
The main function of fibrin is the formation of a coagulation and stopping bleeding, of course, there is no doubt about its significance, however, the role of this substance in the course and completion of the inflammatory process is also important, but is not so widely known to people in non-medical professions, so I would like to dwell a little on the topic: “ Fibrin and inflammation."
Fibrin formation occurs immediately after fibrinogen comes into contact with tissue thrombokinase, released from damaged (wound) or destroyed (ulcer) tissue. This local reaction, in which toxins are captured by fibrin and enclosed in a bundle, is adaptive and is called the “fixation reaction.” It is very important for the body, because at the very early stages, even before white blood cells - leukocytes, “feel” that the scene of an accident awaits them, fibrin will create a barrier around the source, which will counteract the spread of infection throughout the body. That is, it should be recognized that immediately deposited fibrin can rightfully claim a very important and necessary protective role. And the negative changes, which, one way or another, will be present in a small area, will try to take on the problem, protecting other, more important organs (internal) from evil.
- At the moment of transition of fibrinogen into fibrin (1st stage of fibrin formation), enzymes present in the inflammatory focus, which are capable of subjecting proteins having disulfide bridges to tryptic hydrolysis (fibrin monomer, as is known, has them), already begin their activity, acting as inhibitors inflammatory process;
- At stage 2 (formation of fibrin polymer), tryptic enzymes try in every possible way to inhibit fibrin polymerization. These proteases, breaking down fibrin and other protein macromolecules into smaller organic compounds (amino acids, peptides), transform the viscous thick exudate formed on the wound into a more liquid state, in addition, they inhibit the formation of new large molecules that are difficult to dissolve;
- Proteolytic enzymes - proteases (for example, plasmin) at the repair stage trigger the mechanism of destruction of fibrin clots and, thus, restore tissue.
By the way, thanks to numerous and comprehensive studies, it was found that the introduction of proteolytic enzymes before the inflammatory reaction on the wound takes effect makes it possible to prevent its development, which means that, in fact, a person receiving proteases from the outside after various traumatic situations is prevention of inflammation.
Upon completion of the inflammatory process, scars often form in its place - it is the fibrin formed in this area and preserved for a long time that provides the basis for the proliferation of connective tissue cells.
Symptoms
- The pain intensifies while eating. Food irritates erosive areas, promotes the separation of films and the appearance of new defects. This applies to a greater extent to spicy, hot, coarse dishes.
- Swallowing problems (dysphagia).
- Belching, bad breath, heartburn in the presence of reflux are common complaints of patients.
- Nausea can result in vomiting with blood and the presence of fibrin films. Erosive changes are manifested by hemoptysis.
Diagnostics
For successful treatment, the doctor must conduct a full examination.
- Careful collection of complaints plays a key role. Chest pain while eating, heartburn, vomiting with blood or fibrin films are key signs of pseudomembranous esophagitis. If it is possible to find a connection with scarlet fever or diphtheria, this simplifies diagnosis and treatment.
- A general blood and urine test is necessary to determine the severity and severity of the inflammatory process.
- pH testing can indicate the presence of reflux; this method measures the acidity in the distal esophagus.
- The main diagnostic method is endoscopy. The doctor visually assesses the condition of the mucous membrane, catarrhal or fibrinous inflammation, and the degree of damage. If necessary, a biopsy is taken.
Colon
One of the most common diseases of the gastrointestinal tract is inflammation of the colon or colitis. The causes of colitis are considered to be infections, unhealthy diet, as well as the ingestion of poisons used in everyday life and industry.
This type of disease can occur as a separate disease, due to disturbances in the immune system, or be the result of certain dysfunctions of the stomach and small intestine.
Medicine distinguishes four types of inflammation of the large intestine:
If a diagnosis such as inflammation of the large intestine is made, the symptoms and treatment are different for its different types.
Symptoms of inflammation of the large intestine
Acute colitis is characterized by the following symptoms:
- Periodic abdominal pain accompanied by unstable stools;
- The appearance of mucus and blood impurities in the stool;
- Lethargy and increased temperature against the background of the patient’s general malaise;
- Painful urge to defecate.
With insufficient therapy or its absence, acute colitis can become chronic, the symptoms of which are in many ways similar to acute colitis, however, treatment is much longer and more complex. The main signs of chronic colitis are:
- Cramping pain in the abdomen;
- Weakness and nausea;
- Lack of desire to eat;
- Increased abdominal volume and flatulence.
Ulcerative colitis is an inflammation of the colon mucosa with the appearance of ulcers. This inflammation can develop over a long period of time with periodic exacerbations. The most common symptom of this disease is pain in the lower abdomen, manifested by periodic attacks. After a short period of time, defecation involves blood, and the amount of blood released often reaches 300 ml at a time.
During exacerbations, blood can flow in a stream, which leads to a sharp drop in blood pressure. Distention of the colon with the formation of peritonitis is also possible.
With spastic colitis, the patient passes feces in the form of small dense lumps. With such a symptom, it is necessary to carry out the necessary tests and examination of the patient using special equipment.
Treatment tactics
The doctor’s initial task is to determine the cause of esophagitis. Scarlet fever and diphtheria require specific treatment. Only by coping with the underlying disease can we hope for a speedy recovery.
Diet
It is recommended to eat bland food. All dishes should be pureed and at room temperature. Too cold or hot food injures the mucous membrane in catarrhal fibrinous esophagitis. The optimal serving size is 200-250 g. Avoid fatty, fried foods, spices, marinades, smoked foods, sour apples, citrus fruits, these foods increase reflux.
Drug treatment
- Bismuth preparations (de-nol, vikair), almagel, phosphalugel, and sea buckthorn oil will help protect the mucous membrane and reduce inflammation.
- The main drugs used in the treatment of reflux are acid-reducing drugs (omeprazole, pantoprazole) and H2-histamine blockers (famotidine).
- Pokinetics (Raglan, Cerucal) improve motility of the esophagus.
- If hemoptysis is observed, hemostatic drugs are indicated: vikasol, dicinone.
- In severe cases, surgery is necessary.
Attention! At the first manifestations of the disease, you should immediately go to the hospital. Early initiation of treatment improves prognosis. Fibrinous esophagitis has severe complications: scarring, narrowing of the lumen of the esophagus, in such cases it is no longer possible to do without surgery.