Callous gastric ulcer often provokes the onset of the oncological process in gastroenterological practice. The disease is characterized by persistent ulceration of the gastric cavity and ineffectiveness of therapeutic treatment. Soreness and constant discomfort become the patient’s constant companions. Almost every 3 patients with a history of callous ulcers become patients in oncology departments. During internal instrumental studies, the gastric cavity is represented by scar tissue with a tendency to necrotic changes. Treatment of ulcers is lengthy, often requiring surgery to remove damaged mucous structures of the organ.
Stomach pain due to peptic ulcer
The essence of the disease
A callous ulcer damages the walls of the stomach, its mucosa, muscle tissue and submucosa. As a result, the organ is completely deprived of protection. The acid that is produced in the stomach has an aggressive effect on the defenseless walls.
The ulcer does not heal, resulting in constant relapses. The formation is bordered by hard areas and does not change its shape even when pressed. A lot (symptoms, complications) depends on the location of the ulcer.
The risk of malignancy increases if the defect is very close to the pylorus and the junction with the esophagus. The ulcer forms gradually, in several stages. Over the years, the disease becomes chronic.
Description of the pathology
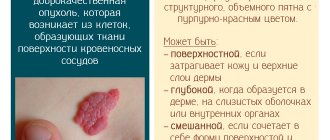
An ulcer is a defect in the mucous membrane, and sometimes, depending on the depth of the lesion, even affects the muscular layers of the stomach. The source of inflammation has clear, even contours of varying diameters. The bottom of the wound is smooth, grayish-yellowish in color, with a callous coating. A callous gastric ulcer is similar to a rough scar formed from connective tissue, which is not capable of regenerating at all, which means there simply can be no chance of restoration of the mucous membrane. Small pockets of point-like inflammation may appear around the ulcer, which aggravate the course of the disease, causing even more discomfort.
Due to the formation of a dense, rough scar in the ulcer itself, proper blood circulation at the site of the lesion is disrupted, the process of innervation of the mucous membrane changes, and this leads to a gradual loss of the stomach area from the proper functioning of the organ. In addition, the hardened connective tissue is no longer able to produce gastric juice, enzymes and digest food. This means that this part of the stomach no longer performs its intended function.
An ulcer is a deep lesion of the gastric mucosa
Causes of the disease
Callous ulcers most often appear due to thinning of the mucosa or its absence. As a result, hydrochloric acid easily corrodes the walls of the stomach. Non-healing ulcers appear at the site of deformation. Other causes of the disease:
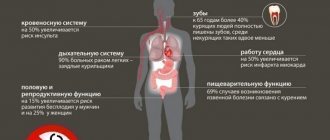
- In 40 percent of cases, the formation of ulcers is caused by the microorganism Helicobacter pylori. It secretes a specific enzyme that produces ammonia. As a result, the mucous membrane is destroyed, and the stomach is unprotected. In this case, the bacterium additionally destroys the walls of the organ.
- Anti-inflammatory nonsteroidal drugs and glucocorticoids. They reduce the production of prostaglandins. This prevents the mucous membrane from recovering. Some drugs destroy it completely (for example, Aspirin, Diclofenac).
- Violation of the integrity of blood vessels.
- Hormonal imbalance.
- Stress (even short-term) or emotional stress causes vascular spasms. As a result, metabolism and cellular nutrition are disrupted and they die. Then the risk of ulcers increases even more.
The development of the disease can be determined by the shape of the scars. If the ulcer has formed in the form of uneven curved outlines, it means that it formed suddenly, impulsively. Even scarring indicates a measured and stable progression of the disease. An already formed callous formation never changes its shape and is not disturbed by palpation or touch of the probe.
Why does the disease develop?
The main cause of the disease is the bacterium Helicobacter pylori.
An ulcer of the gastrointestinal tract occurs due to the impact of a certain irritant on the mucous membrane, which causes its protection to deteriorate. As a result of such processes, hydrochloric acid, which is located in the stomach, comes into contact with its unprotected walls, beginning to corrode first the submucosal layer, and then the cell membranes. The following factors are identified that irritate the mucous membrane:
- bacterium Helicobacter pylori;
- certain types of medications, for example, glucocorticosteroids and non-steroidal anti-inflammatory drugs;
- hormonal imbalances;
- constant stressful situations and nervous overstrain.
Symptomatic complex
With a callous ulcer, symptoms may not appear for a long time. Only minor disturbances in the functioning of the gastrointestinal tract become noticeable. As the disease progresses, symptoms appear gradually and become more intense. The main features include:
- severe pain;
- Iron-deficiency anemia;
- indigestion;
- high production of gastric juice;
- metabolic disruptions.
Pain is felt while eating or in the morning on an empty stomach. Seasons do not affect the frequency of exacerbations. Relapses are associated with the characteristics of scar tissue. The affected areas at the site of ulceration lose their ability to recover, which prevents wound healing.
The intensity and duration of pain depends on the location of the ulcers. From the stomach area they spread to the chest and spine. Negative sensations appear within an hour after eating. If the ulcer is located in the duodenum area, pain will appear only after 2 hours or later. When pain occurs at night, it is usually from 23.00 to 03.00 hours.
Minor signs
Secondary signs include dyspeptic disorders and intoxication of the body. All this provokes the appearance of:
- emotional breakdowns;
- headaches;
- bloating;
- irritation;
- hot flashes in women;
- migraine;
- frequent mood changes;
- insomnia.
The pain mainly appears in the stomach. This symptom can be confused with cholecystitis. All of the above signs appear against the background of the development of the disease and in its chronic form. The symptoms manifest themselves most clearly during an exacerbation of the pathology. During the period of remission, the pain becomes much weaker and appears mainly at night.
Since the ulcer does not heal, anemia develops against the background of constant bleeding. An unpleasant and pungent odor appears from the mouth (especially in the morning). Depression quickly gives way to outbursts of anger. Constant irritability appears.
Special signs
Distinctive symptoms include hunger pains that occur mainly at night. There are also other special symptoms:
- bowel dysfunction (constant constipation);
- copious amounts of saliva;
- vomit;
- constant nausea;
- sour belching;
- regular heartburn.
After bouts of vomiting, patients experience temporary relief from pain. People with callous ulcers quickly lose weight. The cause is pain, which causes a psychological barrier before each meal. People are afraid to eat; they do it reluctantly and rarely.
Stomach ulcer: symptoms and manifestations
✓ Article checked by doctor
Gastric ulcer is a chronic pathology characterized by trophic disorders. The disease is most common among middle-aged men. As the disease progresses, remissions may occur, but stomach ulcers often worsen in autumn and spring. In many cases, the disease appears due to severe, prolonged stress and stress on the nervous system. With psychological abnormalities, pathologies occur in the blood supply to the gastrointestinal tract, which is why gastric juice corrodes the mucous membrane. If this process is not stopped, ulceration of the mucous membrane is possible.
Stomach ulcer: symptoms and manifestations
Stomach ulcer: what is it?
Gastric ulcers occur under the influence of Helicobacter pylori bacteria, when the immune system is weakened. The walls of the stomach become more susceptible to microorganisms and other negative factors when the protective functions are weakened. If metabolic processes occur incorrectly, pepsin and hydrochloric acid produced in the stomach corrode it.
On a note! This disease can appear in childhood, but it most often affects adults.
Usually this disease is diagnosed before the age of 40 years. The disease is more common among men than women. The likelihood of developing the disease varies not only depending on gender and age factors, but also depending on the type of activity. The appearance of a stomach ulcer can be affected by severe trauma to the abdomen or eating the wrong foods.
What is a stomach ulcer
Main signs of a stomach ulcer
In order to detect the disease in a timely manner, it is necessary to know its main manifestations. When the first symptoms appear, it is necessary to consult a doctor and carry out diagnostic measures to solve the problem using therapeutic methods without the use of surgery. You should undergo regular routine examinations in order to promptly identify the disease if it does not manifest itself with specific symptoms. There are several factors that indicate the likelihood of an ulcer.
Causes of stomach ulcers
Manifestation of stomach ulcer
The characteristics of the pain syndrome and other signs depend on the location of the ulcer. Based on medical history and the patient’s story about the nature and characteristics of the pain syndrome, doctors often make a primary diagnosis, indicating the appearance of an ulcer in a specific part of the stomach.
Manifestations of gastric ulcer
Ulcer of the subcardial and cardiac region
Expressed in early detection of pain. Patients feel negative symptoms half an hour after eating. Pain is noted near the xiphoid process. Sometimes it radiates to the heart area, which is why patients may confuse a stomach ulcer with symptoms of heart failure. Pain appears depending on the frequency of food consumption, and does not intensify even with physical activity. The pain syndrome may ease if the patient often drinks milk or antacids. Usually the pain is mild, while the patient’s condition constantly worsens as a result of periodic vomiting, belching, and heartburn almost immediately after eating.
Ulcer of the lesser curvature of the stomach
Ulcers of the lesser curvature of the stomach
Identified by pain syndrome spreading to the epigastric region. Patients indicate pain manifested in the upper left abdomen. Usually, discomfort occurs 60 minutes after eating. When food completely passes into the intestines, the stomach is emptied, and the pain syndrome subsides for a while. Sometimes patients report severe pain when they take a long break from eating. The pain often occurs in the evening and at night and is chronic and aching in nature at the initial stage of the disease.
On a note! When the disease worsens, the pain syndrome worsens. Patients often complain of nausea, but practically do not suffer from vomiting.
Ulcer of the greater curvature of the stomach
It manifests itself as a moderate pain syndrome, which is why this type of lesion is detected only in the last stages. This type of ulcer localization is quite rare, but the lesion is malignant.
Ulcers of the greater curvature of the stomach
Ulcer of the antrum of the stomach
It is characterized by severe pain that occurs in the evening or at night. Usually, along with pain, patients feel sour belching and heartburn. Unpleasant sensations appear in the epigastric zone.
Pyloric ulcer
It is characterized by paroxysmal manifestations of pain, and the unpleasant sensations are of high intensity. The attacks last quite a long time, often more than 40 minutes. Typically, patients feel severe pain at night or when they cannot eat. Some patients note that the onset of pain does not depend on food. Patients also notice increased salivation and heartburn, which cannot always be relieved with the help of pharmaceutical medications.
On a note! Sometimes patients suffer from stomach ulcers, which manifest themselves with atypical symptoms. The pain syndrome can affect the area under the ribs on the right side, radiating to the lower back and heart.
Symptoms of stomach ulcer
Pain and other signs of the disease may not appear. This feature leads to the development of complications as a result of untimely detection of the disease.
Signs of complications of a stomach ulcer
The danger of a stomach ulcer lies in the occurrence of complications that provoke the occurrence of a large number of pathologies and death. There are a number of adverse complications characterized by specific symptoms.
Penetration
It is characterized by destruction of the affected wall of the stomach, while the pathological process spreads to nearby tissues. Usually the pancreas is affected by this pathological process, but in some cases the ulcer spreads to the gallbladder and liver. Sulfuric acid produced in the stomach can cause acute pancreatitis.
Complications of peptic ulcer
To prevent penetration, follow these steps:
- step 1. Eliminate signs of an inflammatory process: girdling pain, increased temperature (with penetration, this indicator increases to 40 degrees or more);
- Step 2. Get a blood test. During penetration, an increase in alpha-amylase levels is observed;
- step 3. Pay attention to the characteristics of the pain syndrome. It is often localized in the affected area, appears daily, and occurs regardless of the regularity of food intake or other external factors.
To clarify the presence of a stomach ulcer, an x-ray and FGS are performed.
Gastric perforation
Occurs when the stomach wall is destroyed with the movement of its contents into the abdominal cavity. Perforation of the stomach often occurs with increased physical activity, frequent consumption of spicy foods, and also when taking large amounts of alcohol-containing drinks. Patients indicate severe pain, corresponding to the localization of the ulcerative lesion, a feeling of weakness, and general symptoms indicating intoxication also appear. If gastric perforation occurs without predisposing factors, painful shock may occur. After a few hours, peritonitis may develop.
Tips for stomach ulcers
On a note! X-rays are used to clarify the diagnosis.
Bleeding
This complication often leads to death. In many cases it occurs in conjunction with penetration. The appearance of internal bleeding is indicated by vomiting, and the color of the discharge is similar to the color of coffee. General symptoms appear indicating the loss of a large amount of blood. The stool is dark in color. With gastric bleeding, pressure drops sharply, shortness of breath, symptoms of tachycardia appear, and patients suffer from hyperhidrosis. If these symptoms are detected, you must contact a medical facility to stop the bleeding as quickly as possible.
Signs of bleeding from a stomach ulcer
Malignancy
This complication is characterized by the degeneration of the affected area into a malignant tumor. Malignization occurs quite rarely and is diagnosed in 3% of patients suffering from chronic gastric ulcers. Typically, a cancerous tumor occurs at the site of callous ulcers, as well as in the affected area where scars have formed. When a cancerous tumor forms, the patient experiences a sharp weight loss and loss of appetite. Patients practically cannot eat dishes containing meat. As the symptoms of the disease worsen, the body temperature rises, which practically does not subside, and vomiting with blood often occurs. If you do not seek medical help in a timely manner, your body may become completely exhausted.
On a note! In order to make a diagnosis, FGS with a three-point biopsy is performed.
Pyloric stenosis
It is one of the most dangerous complications of stomach ulcers. Manifests itself in the pyloric region of this organ. The likelihood of stenosis increases with the occurrence of persistent diseases. A decrease in the lumen in the pyloric region provokes constant stagnation of food, the appearance of difficulties with its passage into the intestines.
There are several stages of pyloric stenosis:
- Compensated. Sour belching and a feeling of heaviness in the stomach appear. A person may feel full even when eating a small amount of food. The patient's general condition is not affected.
- Subcompensated. There is an almost constant feeling of fullness and heaviness in the stomach. Often, at this stage of the disease, vomiting occurs, after which the listed symptoms subside for a while. Patients refuse to eat because they are afraid of unpleasant symptoms. There is a sharp decrease in body weight.
- Decompensated. It is manifested by frequent mouth, which occurs immediately after eating food. Patients suffer from dehydration and severe weight loss. After some time, muscle cramps appear. Food practically does not enter the intestines due to the severe narrowing of the pylorus.
To avoid deterioration of the general condition of a stomach ulcer, it is necessary to promptly detect its symptoms and consult a doctor for diagnosis and treatment. If therapeutic measures are taken in a timely manner, a stable remission may occur. Recovery is indicated by the absence of symptoms of a stomach ulcer for three years or longer. The prognosis for this disease is conditionally favorable, provided that the disease is identified and treated in the initial stages.
Video - Stomach ulcer
Did you like the article? Save so you don't lose!
Sources used: med-explorer.ru
Diagnosis of callous ulcer
When a callous ulcer appears, an external examination of the patient is initially performed. When palpating the area of the stomach and its bend, a slight compaction is felt. Next, the patient donates blood for analysis. It is done to exclude inflammation or other similar diseases. Important indicators are the level of feritin and hemoglobin (to rule out anemia).
X-ray allows you to determine the exact location of the ulcer and visualize its edges and bottom. Endoscopy helps to examine the defect and its rim in more detail. The callous ulcer does not deform when touched by the probe. The mucous membrane around the affected area is covered with folds and erosions directed towards the main defect.
A biopsy of the edges of the ulcer is required. This helps to identify the malignancy of cells and the early stage of development of cancer.
Treatment
For callous gastric ulcers, treatment with medications is useless. The disease is not amenable to conservative therapy. Treatment with medications is aimed at eliminating or reducing the intensity of symptoms. The only way to completely remove an ulcer is through surgery.
Before taking medications that negatively affect the mucous membranes, you need to eat a couple of tablespoons of unleavened boiled liquid oatmeal. This will protect the stomach from the aggressive effects of drugs. Traditional methods help to relieve pain. For example, put a heating pad on the affected area or drink milk. This will reduce the intensity of pain.
Prevention
The following expert recommendations aimed at preventing damage to the mucous membrane of the organ can prevent the development of callous gastric ulcers:
- proper organization of nutrition;
- rejection of bad habits;
- minimizing stress;
- correct preparation of work and rest schedules;
- taking medications only as prescribed by a specialist;
- timely treatment and prevention of pathologies of the digestive system and other diseases.
Sources
https://dolgojit.net/kalleznaia-iazva.php https://myfamilydoctor.ru/kalleznaya-yazva-zheludka-chem-opasna-kak-ot-nee-izbavitsya/ https://zhktok.ru/bolezn/yazva /kalleznaya-yazva-zheludka.html https://zhkt.expert/yazva/kak-osuschestvlyaetsya-lechenie-kalleznoy-yazvy.html https://zheludok24.ru/zabolevaniya/yazva/kalleznaya-yazva-zheludka/ https:/ /vnorg.ru/zheludok/yazva/250-kalleznaya-yazva-zheludka.html https://ozhivote.ru/kalleznaya-yazva/ https://gastromedic.ru/yazvennaya-bolezn/zheludka/kalleznaya-yazva.html
Radical treatment
A rough, hard scar does not have regenerative properties, so conventional treatment with medications is ineffective. The only way to remove an ulcer is through surgery. After this, the resulting hole is sutured.
If necessary, the surgeon performs a vagotomy. This helps reduce stomach acid. As a result, the aggressive effect on the walls of the organ is reduced, which prevents relapses of the disease in the future.
Surgery is necessary to prevent stomach cancer. In 93 percent of cases, rehabilitation goes well and patients return to a good quality of life.
Diet
Since the stomach is directly related to food, food must be proper and healthy. Then it will not harm the mucous membrane of the organ. After resection and vagotomy, a strict diet is the most important factor in preventing relapses. And if the disease is detected at an early stage, proper nutrition will prolong the period of remission and delay the exacerbation of the disease.
What foods should never appear on your table if you have such a stomach problem? You should give up sweets and confectionery, smoked, fried and spicy foods, rich meat broths, fatty fish and pork. You should forget about pickles, fresh and sauerkraut. Black bread and lard are prohibited.
But fermented milk products may appear more often in your diet. It is recommended to eat porridges from various cereals (the consistency should be semi-liquid), cutlets from lean meat (rabbit, poultry), vegetable broths and raw and boiled vegetables. You can drink compotes or sweet juices. Rusks are an excellent substitute for bread.
If you feel worse after eating, do not delay visiting a doctor. Take care of your stomach, otherwise you risk losing your health. Following a diet and taking special medications will allow you to forget about callous ulcers for a long time, and a healthy lifestyle and proper nutrition will be an excellent means of preventing it.
Forecast
The prognosis for the presence of callous ulcers is unfavorable. The disease is incurable, with constant and frequent relapses. Surgical operations can return a person to a good quality of life for a long time. However, in every third case, a callous ulcer turns into a cancerous disease. Lack of timely treatment leads to serious complications and death.
Prevention of disease development
To prevent the disease, you need to adhere to a strict diet throughout your life. Stop smoking and drinking alcohol. It is important to take time to rest, avoid stress, and get enough sleep. To prevent nervous conditions, drink sedatives (tincture of motherwort, valerian) daily.
Callous ulcers cannot be treated with medication. Self-medication can only lead to exacerbation of the disease, severe complications, deterioration of the condition and provoke the development of cancer.
Stomach ulcer
Stomach ulcer
– a chronic polyetiological pathology that occurs with the formation of ulcerative lesions in the stomach, a tendency to progression and the formation of complications. The main clinical signs of peptic ulcer disease include pain in the stomach and dyspeptic symptoms. The diagnostic standard is an endoscopic examination with a biopsy of pathological areas, radiography of the stomach, and detection of H. pylori. Treatment is complex: diet and physiotherapy, eradication of Helicobacter pylori infection, surgical correction of complications of the disease.
Stomach ulcer
Gastric ulcer (GUD) is a cyclically relapsing chronic disease, the characteristic feature of which is ulceration of the stomach wall. PUD is the most common pathology of the gastrointestinal tract: according to various sources, from 5 to 15% of the world's population suffer from this disease, and among urban residents the pathology is five times more common. Many specialists in the field of gastroenterology combine the concepts of gastric ulcer and duodenal ulcer, which is not entirely correct - ulcerations in the duodenum are diagnosed 10-15 times more often than ulcers in the stomach. However, PU requires careful study and development of modern diagnostic and treatment methods, since this disease can lead to the development of fatal complications.
About 80% of cases of primary detection of gastric ulcers occur in working age (up to 40 years). In children and adolescents, gastric ulcers are diagnosed extremely rarely. Among the adult population, there is a predominance of men (women suffer from peptic ulcers 3-10 times less often); But in old age, sex differences in incidence are smoothed out. In women, the disease is milder, in most cases asymptomatic, and is rarely complicated by bleeding and perforation.
Gastric ulcer ranks second among the causes of disability in the population (after cardiovascular pathology). Despite the long period of study of this nosology (more than a century), therapeutic methods of influence that can stop the progression of the disease and completely cure the patient have not yet been found. The incidence of gastrointestinal ulcers throughout the world is continuously growing, requiring the attention of therapists, gastroenterologists, and surgeons.
Classification of gastric ulcer
Until today, scientists and clinicians around the world have not been able to reach agreement on the classification of gastric ulcers. Domestic experts systematize this pathology according to the following criteria:
- causative factor
– ulcers associated or not associated with H. pylori, symptomatic ulcers; - localization
- ulcer of the cardia, antrum or body of the stomach, pylorus; greater or lesser curvature, anterior, posterior wall of the stomach; - number of defects
- single ulcer or multiple ulcers; - size of the defect
– small ulcer (up to 5 mm), medium (up to 20 mm), large (up to 30 mm), giant (more than 30 mm); - stage of the disease
- exacerbation, remission, scarring (red or white scar), cicatricial deformation of the stomach; - course of the disease
- acute (the diagnosis of gastric ulcer is established for the first time), chronic (periodic exacerbations and remissions are noted); - complications
- gastric bleeding, perforated gastric ulcer, penetration, cicatricial ulcerative gastric stenosis.
Causes and pathogenesis of gastric ulcer
The main etiological factor in the formation of gastric ulcer is infection with H. pylori - more than 80% of patients have positive tests for Helicobacter pylori infection. In 40% of patients with gastric ulcer infected with the Helicobacter bacterium, anamnestic data indicate a family predisposition to this disease. The second most important cause of gastric ulcer formation is considered to be the use of non-steroidal anti-inflammatory drugs. Rarer etiological factors of this pathology include Zollinger-Ellison syndrome, HIV infection, connective tissue diseases, liver cirrhosis, heart and lung disease, kidney damage, exposure to stress factors that lead to the formation of symptomatic ulcers.
The main significance for the formation of gastric ulcer is an imbalance between the protective mechanisms of the mucous membrane and the influence of aggressive endogenous factors (concentrated hydrochloric acid, pepsin, bile acids) against the background of a disorder of the evacuation function of the gastrointestinal tract (gastric inactivity, duodenogastric reflux, etc.) . Inhibition of protection and slower recovery of the mucous membrane is possible against the background of atrophic gastritis, with chronic Helicobacter pylori infection, ischemia of stomach tissue against the background of collagenosis, long-term use of NSAIDs (the synthesis of prostaglandins slows down, which leads to a decrease in mucus production).
The morphological picture of gastric ulcer undergoes a number of changes. The primary substrate for the occurrence of ulcers is erosion - superficial damage to the gastric epithelium, which forms against the background of necrosis of the mucous membrane. Erosions are usually detected on the lesser curvature and in the pylorus of the stomach; these defects are rarely isolated. The size of erosions can range from 2 millimeters to several centimeters. Visually, erosion is a mucosal defect that does not differ in appearance from the surrounding tissues, the bottom of which is covered with fibrin. Complete epithelization of erosion with a favorable course of erosive gastritis occurs within 3 days without the formation of scar tissue. If the outcome is unfavorable, erosions transform into acute gastric ulcers.
An acute ulcer is formed when the pathological process spreads deep into the mucous membrane (beyond its muscular plate). The ulcers are usually single, take on a rounded shape, and look like a pyramid when cut. In appearance, the edges of the ulcer also do not differ from the surrounding tissues; the bottom is covered with fibrin deposits. Black coloration of the bottom of the ulcer is possible when the vessel is damaged and hematin is formed (a chemical substance formed during the oxidation of hemoglobin from destroyed red blood cells). A favorable outcome of an acute ulcer consists of scarring within two weeks; an unfavorable outcome is marked by the transition of the process to a chronic form.
The progression and intensification of inflammatory processes in the area of the ulcer leads to increased formation of scar tissue. Because of this, the bottom and edges of a chronic ulcer become dense and differ in color from the surrounding healthy tissue. A chronic ulcer tends to enlarge and deepen during an exacerbation; during remission it decreases in size.
Symptoms of stomach ulcer
The clinical course of gastric ulcer is characterized by periods of remission and exacerbation. Exacerbation of peptic ulcer is characterized by the appearance and increase of pain in the epigastric region and under the xiphoid process of the sternum. With an ulcer of the body of the stomach, the pain is localized to the left of the center line of the body; in the presence of ulceration of the pyloric region - on the right. Pain may radiate to the left half of the chest, shoulder blade, lower back, and spine. Gastric ulcer is characterized by the onset of pain immediately after eating with increasing intensity within 30-60 minutes after eating; pylorus ulcer can lead to the development of night, hunger and late pain (3-4 hours after eating). The pain syndrome is relieved by applying a heating pad to the stomach area, taking antacids, antispasmodics, proton pump inhibitors, and H2-histamine receptor blockers.
In addition to the pain syndrome, ulcerative gastrointestinal tract is characterized by a coated tongue, bad breath, and dyspeptic symptoms - nausea, vomiting, heartburn, increased flatulence, and stool instability. Vomiting mainly occurs at the height of stomach pain and brings relief. Some patients tend to induce vomiting to improve their condition, which leads to progression of the disease and complications.
Atypical forms of gastric ulcer can manifest as pain in the right iliac region (appendicular type), in the heart (cardiac type), and in the lower back (radiculitis pain). In exceptional cases, pain syndrome with gastric ulcer may be completely absent, then the first sign of the disease is bleeding, perforation or cicatricial stenosis of the stomach, for which reason the patient seeks medical help.
Diagnosis of gastric ulcer
The gold standard for diagnosing gastric ulcers is esophagogastroduodenoscopy. Endoscopy allows you to visualize the ulcerative defect in 95% of patients and determine the stage of the disease (acute or chronic ulcer). Endoscopic examination makes it possible to promptly identify complications of gastric ulcer (bleeding, cicatricial stenosis), conduct endoscopic biopsy, and surgical hemostasis.
X-ray of the stomach (gastrography) is of paramount importance in the diagnosis of cicatricial complications and penetration of ulcers into nearby organs and tissues. If endoscopic visualization is not possible, radiography can verify a gastric ulcer in 70% of cases. For a more accurate result, it is recommended to use double contrasting - in this case, the defect is visible in the form of a niche or a persistent contrasting spot on the wall of the stomach, to which the folds of the mucous membrane converge.
Considering the huge role of Helicobacter pylori infection in the development of peptic ulcer, all patients with this pathology undergo mandatory tests to detect H. pylori (ELISA, PCR diagnostics, breath test, examination of biopsy specimens, etc.).
Of auxiliary importance for gastric ulcers are ultrasound of the gastrointestinal tract (detects concomitant pathology of the liver, pancreas), electrogastrography and antroduodenal manometry (makes it possible to assess the motor activity of the stomach and its evacuation ability), intragastric pH-metry (detects aggressive factors of damage), stool analysis for hidden blood (done if gastric bleeding is suspected). If a patient is admitted to the hospital with a clinical picture of an “acute abdomen,” diagnostic laparoscopy may be required to exclude gastric perforation. Gastric ulcers must be differentiated from symptomatic ulcers (especially medicinal ones), Zollinger-Ellison syndrome, hyperparathyroidism, and gastric cancer.
Treatment of gastric ulcer
The main goals of therapy for peptic ulcer include repair of the ulcer, prevention of disease complications, and achievement of long-term remission. Treatment of gastric ulcer includes non-drug and medicinal treatments, and surgical methods. Non-drug treatment of peptic ulcer involves following a diet, prescribing physiotherapeutic procedures (heat, paraffin therapy, ozokerite, electrophoresis and microwave exposure), it is also recommended to avoid stress and lead a healthy lifestyle.
Drug treatment should be comprehensive and affect all parts of the pathogenesis of ulcerative gastrointestinal tract. Anti-Helicobacter therapy requires the use of several drugs to eradicate H. pylori, since the use of monoschemes has shown to be ineffective. The attending physician individually selects a combination of the following drugs: proton pump inhibitors, antibiotics (clarithromycin, metronidazole, amoxicillin, tetracycline, furazolidone, levofloxacin, etc.), bismuth preparations.
If you seek medical help in a timely manner and carry out a complete anti-Helicobacter treatment regimen, the risk of complications of gastric ulcer is minimized. Emergency surgical treatment of gastric ulcer (hemostasis by clipping or suturing a bleeding vessel, suturing the ulcer) is usually required only for patients with a complicated pathology: perforation or penetration of the ulcer, bleeding from the ulcer, malignancy, and the formation of scar changes in the stomach. In elderly patients, if there is a history of indications of complications of gastric ulcer in the past, experts recommend reducing the duration of conservative treatment to one to one and a half months.
Absolute indications for surgical intervention: perforation and malignancy of the ulcer, massive bleeding, cicatricial changes in the stomach with disruption of its function, ulcer of the gastroenteroanastomosis. Conditionally absolute indications include penetration of ulcers, giant callous ulcers, recurrent gastric bleeding during conservative therapy, and lack of ulcer repair after suturing. A relative indication is the absence of a clear effect from drug therapy for 2-3 years.
For decades, surgeons have been discussing the effectiveness and safety of various types of surgical interventions for gastric ulcers. Today, gastrectomy, gastroenterostomy, and various types of vagotomies are recognized as the most effective. Excision and suturing of a gastric ulcer is used only in extreme cases.
Forecast and prevention of gastric ulcer
The prognosis for gastric ulcer largely depends on the timeliness of seeking medical help and the effectiveness of anti-Helicobacter therapy. Peptic ulcer is complicated by gastric bleeding in every fifth patient, from 5 to 15% of patients suffer perforation or penetration of the ulcer, and 2% develop cicatricial stenosis of the stomach. In children, the incidence of complications of gastric ulcer is lower - no more than 4%. The likelihood of developing stomach cancer in patients with peptic ulcer is 3-6 times higher than among people who do not suffer from this pathology.
Primary prevention of gastric ulcer includes preventing infection with Helicobacter pylori infection, eliminating risk factors for the development of this pathology (smoking, cramped living conditions, low standard of living). Secondary prevention is aimed at preventing relapses and includes following a diet, avoiding stress, and prescribing an anti-Helicobacter drug regimen when the first symptoms of peptic ulcer appear. Patients with gastric ulcer require lifelong monitoring, endoscopic examination with mandatory testing for H. pylori once every six months.
Sources used: www.krasotaimedicina.ru