Relationship between diseases
The mechanism of development of the disease is as follows: with advanced osteochondrosis, destructive processes develop in the osteochondral tissue, provoking severe pain (lumbago) and immobility of the spine.
Pathology can affect any part of the musculoskeletal system , but most often the disease is diagnosed in the lumbosacral spine.
The disease is characterized by fusion of the vertebrae.
Different sources use different names to define fused vertebrae. Therefore, even experts consider the terms “spondylosis” and “spondyloarthrosis” to be synonymous. But the distinctive features between the diseases are clearly visible.
Are spondylosis and spondyloarthrosis the same thing?
In medical terminology, spondylosis and spondyloarthrosis are the designations of the stages of development of osteochondrosis. Both pathological conditions cause degenerative processes in the spine. But with spondylosis, deformation of the intervertebral discs occurs due to the formation of bone growths, and with spondyloarthrosis, the entire structure of the intervertebral joints suffers.
A distinctive feature of pathologies is the location of growths (osteophytes).
- In the first case, they grow between the vertebrae, reducing the clearance.
- In the second - along the edges of the joints.
Forecast and possible consequences
In the initial stages of spondylosis, the prognosis is favorable. By following your doctor's recommendations, you can live with this disease for many years and still feel good. However, remember that spondylosis is a chronic disease with a slowly progressive course. It is impossible to completely cure it.
Cervical spondylosis can cause chronic headaches, motor and sensory disturbances in the arms, muscle paresis, and paralysis. These complications arise due to pinched nerves innervating the neck and upper limb. Thoracic spondylosis can be complicated by intercostal neuralgia, chest pain, and cardiac dysfunction. When the lumbosacral region is affected, a person often develops lumbago, radiculitis, and sciatica.
Disability for spondylosis of the cervical, thoracic or lumbar regions is given only at 2-3 degrees. The presence of the disease must be confirmed by x-ray or MRI. A prerequisite for obtaining a group is a persistent decrease in performance.
Development of the disease
The lack of treatment for “ordinary osteochondrosis” causes the development of non-life-threatening, but unpleasant pathological conditions:
- The tissues of the osteochondral system are destroyed.
- Osteophytes are formed, blocking the mobility of one of the areas of the musculoskeletal system.
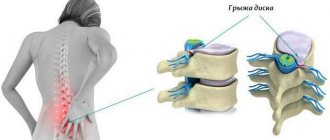
- Destruction of intervertebral discs often leads to a hernia.
In patients with a genetic predisposition to the disease and in those injured in the back, pathological processes develop rapidly.
According to medical research, spondylosis deformans is diagnosed in 80% of patients suffering from osteochondrosis.
A visual video about changes in the spine during the development of spondylosis in the video below:
Exercises to strengthen your back muscles
To relax and strengthen muscles, therapeutic physical training is carried out. Gymnastics is prohibited during periods of severe pain and compression of the spinal cord tissue. Permission to conduct independent training at home must be given by the attending physician.
General rules:
- for the first 2–5 days, do each exercise 3 times, then gradually increase to 10–15;
- the total lesson time is no more than 20–30 minutes;
- training must be carried out daily;
- Make all movements slowly, smoothly, without jerking;
- If pain increases, stop gymnastics.
| Initial position | What to do |
| Sit on the floor, straighten and spread your legs apart | Bend towards each leg in turn, trying to grasp the foot |
| Get on all fours | Arch your back and lower your pelvis, then round your back, trying to touch your chin to your chest |
| Lie on your back, bend and clasp your legs | Round your back, sway, touching the surface with your back Do the exercise on a training mat or carpet |
| Get on all fours | Simultaneously straighten your arms and legs Stay in this position for 10–20 seconds |
| Stand with your feet 25–30 cm apart | Bend left and right, forward and backward Combine bending with rotation of the body around the hips |
| Stand up with your feet together | Lean forward and grab your knees Stay in this position for 10–20 seconds |
Examples of exercises for the lumbosacral spine. Click on photo to enlarge
Operation
If spondylosis leads to pinching or compression of the spinal cord tissue, surgical treatment is performed. It includes:
- partial or complete excision of the intervertebral disc and its replacement with an artificial implant;
- removal of bone spurs;
- fixation of nearby vertebrae with metal structures.
Causes and risk factors
Joint diseases are considered to be age-related pathologies and are attributed to older people. Age-related changes in cartilage tissue provoke spondylosis and spondylarthrosis in certain cases. But there are a number of other factors, independent of age, that cause the development of diseases:
- obesity;
- frequent and heavy loads on the spine (in people of certain professions);
- injuries;
- chronic diseases;
- disruption of the production of the hormone estrogen.
To whom and why does it occur?
The risk group often includes women during menopause, patients with metabolic disorders, with autoimmune disorders and those who are genetically predisposed.
Back pain often bothers people engaged in heavy physical labor in their line of work. But pathology can also arise as a result of single strong loads.
Diagnostics
It is not always easy to determine that spondylosis is the cause of back pain because spondylosis can develop gradually as a result of aging of the body, and pain can also be caused by another degenerative condition such as osteochondrosis. First of all, a neurologist is interested in answers to the following questions:
- Onset of pain
- The type of activity that preceded the onset of pain
- What measures were taken to relieve pain?
- Presence of radiating pain
- Factors that increase or decrease pain
The neurologist will also conduct a physical examination and examine the patient’s neurological status (posture, range of motion in the spine, presence of muscle spasms). In addition, the neurologist also needs to examine the joints (hip joints, sacroiliac joints), since the joints can also be a source of back pain. During a neurological examination, a neurologist will check tendon reflexes, muscle strength, and the presence of sensory disorders.
To verify the diagnosis, instrumental methods are also required, such as radiography, MRI or CT, which allow visualization of changes in the spine. X-rays clearly reflect changes in bone tissue and allow one to visualize the presence of bone growths (osteophytes). But for a more accurate diagnosis, methods such as CT or MRI are preferable, which also visualize soft tissues (ligaments, discs, nerves). In some cases, it is possible to use scintigraphy, especially if it is necessary to differentiate oncological processes or infectious (inflammatory) foci.
If there is damage to the nerve fibers, the doctor may prescribe ENMG, which allows you to determine the degree of conduction disturbance along the nerve fiber and determine both the extent of the damage and the level of damage. Based on the totality of clinical data and the results of instrumental methods, an examination by a neurologist can make a clinical diagnosis of spondylosis and determine the necessary treatment tactics.
Symptoms
Spondylosis is called the result of untreated spondyloarthrosis. With such a close relationship between pathologies, there is a difference in symptoms.
Spondyloarthrosis is characterized by:
- feeling of stiffness in the back (disturbing in the morning);
- joint pain;
- amyotrophy;
- crunch in the spine;
- circulatory disorders;
- development of meteosensitivity and accompanying headaches;
- neuritis;
- development of contracture (inability to fully bend or straighten).
Spondylosis is determined by the following symptoms:
- sharp and severe pain in the coccyx area;
- numbness of the lumbar region;
- "goosebumps" in the legs;
- decrease in body temperature (local);
- feeling of pain when walking;
- it becomes difficult to move.
Additional symptoms may also occur: lameness, loss of sensation in the legs. In this advanced case, the patient loses the desire and ability to move, spends more time lying in the fetal position - this position somewhat alleviates his condition.
Spondylosis - what is it?
The structure of the spine is a combination of vertebrae, which are rigid bony bodies, and intervertebral discs, which are flexible structures with a nucleus pulposus inside and a hard ring outside. In the presence of risk factors, severe pinching of the intervertebral discs occurs, as a result of which the fibrous ring gradually collapses, the nucleus pulposus falls out, and the entire disc loses volume. As a result, the vertebrae located on both sides of the disc come closer together and begin to touch; the absence of a shock-absorbing layer, the role of which was played by the discs, leads to deformation of the vertebrae. In an attempt to “support” and fix the discs that are approaching and subject to degenerative changes, the body stimulates the growth of bone tissue. As a result, osteophytes are formed - bone growths on the vertebral bodies. Since the growth is uncontrolled, under the influence of the growths, pinching of blood vessels and nerves occurs, and in some cases, compression of the spinal cord.
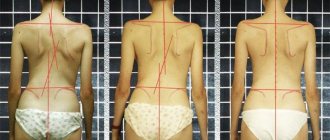
In this case, we can already talk about the presence of lumbar spondylosis. The structure of the spine is very disturbed, so the position of the ligamentous apparatus also changes. Muscles and ligaments peel off from their previous attachment points, due to severe pain to which a person tries to adapt, posture is disrupted, which leads to stretching of some muscles and pinching of others.
Based on the mechanism of occurrence, we can say that spondylosis is a complex degenerative-dystrophic destruction of individual structures of the spine.
The symptoms of this disease are pronounced and may vary depending on the location of the pathology.
Symptoms:
- acute back pain;
- numbness of the lower back;
- increased fatigue;
- impaired mobility of limbs;
- pins and needles sensation in the arms and legs.
Since, due to a violation of the structure of the spine, pinching of large vessels could occur, the patient may be concerned about disturbances in the functioning of internal organs, which are not always correlated specifically with lumbar spondylosis. There are problems with the intestines, genitourinary system, and digestion.
Varieties
There are several types of pathology that arise as a result of “undertreatment” of osteochondrosis , which many do not even consider a disease. Complications develop gradually, some of them have vague symptoms and are difficult to identify.
Deforming
This complication is characterized by abrasion of the intervertebral discs.
The main symptom is aching back pain . Pain is possible both when running and walking, and when sitting or lying down and after it.
Another symptom is a feeling of tightness in the sacral area (usually goes away on its own within 2-3 hours).
Degenerative
It represents damage to the joints - facet and spinal-costal. Restricting the movement of the spinal column is dangerous.
In the early stages, symptoms are not clear . As the pathology develops, pain in the back and impaired range of motion appear.
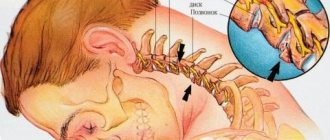
Uncovertebral
Localized in the cervical spine. It is characterized by the appearance of bone formations on the joints of the neck. People of all ages are susceptible to the disease. The main risk group is representatives of sedentary professions.
Main symptoms:
- pain in the back of the head;
- pain in the neck, moving to the area of the shoulder blades and arms;
- frequent dizziness and loss of balance;
- crunching sound when turning the head.
Sometimes patients with uncovertebral spondyloarthrosis suffer from hearing or vision impairment.
Facet joints
Chronic joint disease that occurs against the background of inflammatory processes . Impairs the mobility of the spine.
Symptoms depend on which part of the spine is affected by pathology.
- At the first stage of the disease, the patient suffers from constant aching pain, intensifying in the evening.
- The second stage is the appearance of a crunch in the spine and a violation of its mobility.
- The third is constant severe pain, plus complete immobility of the affected area.
Ankylosing
A rare chronic disease affecting the intervertebral discs , costotransverse, and sometimes other joints of the spine. In medicine it is known as ankylosing spondylitis.
It appears in patients aged 15-30 years. Occurs due to autoimmune disorders, chronic diseases, viral and bacterial infections.
Polysegmental
A pathology of heterogeneous composition and origin that affects cartilage, muscles, ligaments and capsules of the spine. It spreads to several segments of the spinal column at once. The main cause of the disease is the patient’s old age.
Symptoms:
- pain with “shooting”;
- feeling of joint stiffness;
- loss of spinal mobility;
- fast fatiguability.
Dysplastic
The pathology is accompanied by structural changes in the shape of the joints, disturbances in their size and structure. Dysplasia is not diagnosed as a separate disease; it is an accompanying element of spondyloarthrosis.
Symptoms of spondylosis in various parts
Cervical spondylosis. The complex anatomical structure of the cervical spine and wide range of motion make this part of the spine very susceptible to disorders associated with degenerative changes. Neck pain with spondylosis in this area is common. The pain may radiate to the shoulder or down the arm. When osteophytes cause compression of the nerve roots innervating the limbs, in addition to pain, weakness in the upper limbs may also occur. In rare cases, bone spurs (osteophytes) that form in the front of the cervical spine can lead to difficulty swallowing (dysphagia).
When spondylosis is localized in the thoracic spine, pain caused by degenerative changes (spondylosis) often appears when bending the body forward and hyperextension. Flexion causes facet-related pain.
Spondylosis of the lumbar spine often occurs in people over 40 years of age. The most common complaints are lower back pain and morning stiffness. Changes usually occur in several motor segments. The lumbar spine bears most of the body's weight. Therefore, when degenerative changes compromise structural integrity, symptoms, including pain, may accompany any physical activity. Movement stimulates pain fibers in the annulus fibrosus and joints. Sitting for long periods of time can lead to pain and other symptoms due to pressure on the lumbar vertebrae. Repetitive movements such as heavy lifting and bending may increase pain symptoms.
Symptoms of spondylosis can range from mild to severe and can become chronic or even disabling. These may include:
- Cervical Pain that comes and goes
- Pain that radiates to the shoulders, arms, hands, fingers
- Morning stiffness in the neck or shoulder or limited range of motion upon waking
- Neck or shoulder soreness or numbness
- Weakness or tingling in the neck, shoulders, arms, hands, fingers
- Headache in the occipital region
- Balance imbalance
- Difficulty swallowing
- Pain in the upper and middle back
- Pain that comes and goes
Stages and forms of pathology
The initial form of spondyloarthrosis is asymptomatic . Symptoms of osteochondrosis or spondylosis come to the fore during diagnosis, but damage to small joints is still difficult to notice.
Signs of spondyloarthrosis begin to clearly appear after a significant proliferation of osteophytes. Bone growths change the contour pattern of the joints and narrow the lumen of the joint spaces.
There are 4 degrees of development of the disease:
- Ligaments, joint membranes and intervertebral discs lose elasticity, and the range of motion of the spine decreases.
- Increased load on the discs, partial loss of functioning of the fibrous rings.
- Increased bone growths, ligament degeneration.
- The bone growths are so large that they compress blood vessels and nerve endings and significantly limit mobility.
Prevention of spondylosis
The development of age-related spondylosis of the lumbosacral segment cannot be completely prevented, since this is a natural process of aging of body tissues. But it is quite possible to slow down the process of degeneration (destruction and damage) of intervertebral discs.
Prevention goals:
- improve blood supply to the spine;
- strengthen the muscle frame;
- reduce the load on intervertebral discs.
To achieve them, you must follow a number of simple rules:
- Keep your body weight within normal limits.
- Avoid staying in one position for a long time.
- Do gymnastics daily.
- Do not engage in intense, traumatic sports.
- Control blood glucose levels and high blood pressure.
- Do not lift weights exceeding 12–15 kg.
- Maintain correct posture.
- Include collagen-containing foods in your food weekly: jellied meat, gelatin, fatty red fish.
Diagnostic methods
Signs of spinal damage, depending on the stage of the disease and location, may become similar to the symptoms of stomach ulcers, cardiac diseases, etc. If spinal diseases are suspected, the patient is referred to an appointment with a neurologist. For an accurate diagnosis, anamnesis is important - the medical history will help determine the duration and extent of the disease.
How does a doctor make a diagnosis?
Diagnosis begins with physical tests that determine:
- range of motion;
- the effect of spinal compression on gait;
- reflexes and muscle strength.
To obtain a more accurate clinical picture, the doctor may refer the patient to:
- radiography (the image will show all spinal abnormalities);
- computed tomography (for a more detailed image);
- MRI – to identify the area of pinched nerves;
- myelography - the introduction of a tracer dye into the patient’s spinal canal for a clearer image on an X-ray or tomograph;
- Electromyography – measurement of electrical activity in muscles.
What does it mean?
A definite diagnosis implies the beginning of therapeutic procedures. Most often, this is conservative treatment. Surgery is used only in exceptional cases - in case of serious complications that negatively affect the patient’s lifestyle (mobility).
Surgery is also necessary to free up space for the spinal cord and nerve roots:
- hernia removal;
- removal of part of a vertebra;
- graft implantation.
Diagnosis and treatment of spondylosis
Spondylosis in the picture
The pathology develops gradually, so it is easy to miss. At the beginning, a person does not experience any special sensations. Then, when the growths appear, the first, still minor pains arise. Over time, the motor functions of the spine, joints and lower extremities are gradually impaired.
In order to determine how to treat spondylosis, it is necessary to conduct a thorough diagnosis. Typically used for this:
- radiography;
- Magnetic resonance imaging;
- CT scan;
- ultrasonography.
They make it possible to determine the degree of development of the disease, the exact localization of the pathological process, the condition of the cartilage tissue and blood vessels, the presence of complications, the formation of an intervertebral hernia, etc.
X-ray examination must be carried out in two projections. It is this method that allows you to most clearly diagnose such a disease.
Usually, they first try to treat spondylosis with therapeutic methods. For this purpose, analgesics, muscle relaxants, antispasmodics, anti-inflammatory drugs, chondroprotectors, sedatives, diuretics, vasoactive drugs, immunostimulants, tranquilizers, vitamins, antidepressants are used. They make it possible to eliminate pain, relieve swelling, and reduce pressure on nerve endings and blood vessels.
In addition, these medications prevent further progression of the pathology, reduce the inflammatory process, and strengthen cartilage tissue. They enhance the body's protective properties, promote tissue regeneration and restore basic cell functions.
Typically, treatment of the disease is supplemented by physiotherapy, ultrasound, laser, UHF, phonophoresis, electrophoresis. Massage, manual therapy, physical therapy, acupuncture, the use of balneology, paraffin, mud, ozokerite, special diet, etc. are required.
These methods help:
- eliminate signs of spondylosis;
- facilitate its course;
- stop the growth of osteophytes;
- improve the patient's well-being;
- relax the lower back muscles;
- normalize motor activity of the spine;
- restore flexibility to him;
- facilitate the activity of nerve roots;
- increase lymph outflow;
- activate blood circulation;
- lose extra pounds.
General clinical picture
The disease is classified based on severity . The first stage is asymptomatic or with vague symptoms. Occasionally, discomfort appears in the back, but few take them seriously.
This is followed by thinning of the cartilaginous tissues, and the mobility of the cartilaginous vertebrae decreases. In advanced forms of the disease, their movement can be completely blocked. Further development of pathology can be avoided by using conservative treatment methods and performing special exercises.
The development of dangerous complications begins with stage 2 spondylosis deformans. With this form of the disease, it is impossible to heal with just gymnastics and massages. To eliminate symptoms, blockades are used.
Prevention
Carrying out such measures is aimed at eliminating the disease in the initial stages or preventing its development. The patient must adhere to the following recommendations:
- lead an active lifestyle, but do not overload your body;
- follow a diet that limits salt and animal fats;
- Carry out exercise therapy 2-3 times a week, alternating exercises with lower back massage;
- Visit an orthopedist every six months.
Lumbar spondylosis is characterized by the formation of bone spurs in the connective tissue. The clinic is accompanied by pain and limited mobility, sometimes asymptomatic. The pathology is incurable, but conservative therapy in the early stages allows you to avoid serious complications.
Author: Denis Filin, doctor, especially for Vertebrolog.pro
Goals and methods of treatment
The main method of treating spinal pathologies is conservative. Its task is to relieve painful symptoms and increase the mobility of the affected area.
Surgical intervention is used less frequently. It is used after drug therapy and physical therapy have not given the expected positive effect. Or in a complex and advanced stage of the disease.
Drug therapy
To reduce pain and inflammation in spondylosis and spondyloarthrosis, analgesics and non-steroidal anti-inflammatory drugs are used.
Over-the-counter pain relievers you can use:
- Ibuprofen.
- Naproxen sodium.
- Acetaminophen.
Attention: Information on the use of drugs is provided as a guideline. Before starting therapy, be sure to consult with your doctor!
For severe pain, your doctor may prescribe corticosteroids and muscle relaxants.
Medical studies have found that some antidepressants and anti-seizure medications can effectively relieve pain.
What are the benefits of exercise therapy?
Specially designed physical exercises relieve pain, stabilize muscle tone and help restore mobility. But physical therapy only works in combination with drug therapy and other procedures.
The peculiarity of gymnastics is that it must be performed in between attacks, starting with simple exercises and gradually complicating them.
When performing a physical therapy complex, sudden and rapid movements should be avoided; at the first feeling of pain during exercise, they should be interrupted. Properly performed physical exercises strengthen the lumbar region and help maintain the spine.
Physiotherapy
The physiotherapist teaches exercises aimed at stretching and strengthening the muscles of the cervicobrachial region. “Stretching” helps free up space in the spine when nerve roots are pinched.
Also used:
- electrophoresis;
- baths with mineral water;
- cold and hot shower.
Massage
Massage for spinal pathologies, especially during periods of exacerbation, should be light and gentle using anti-inflammatory drugs or natural honey.
Massage of the cervical region relieves spasms, lumbar and thoracic - helps strengthen the muscle corset. Carry out courses of 10 procedures, as prescribed by the doctor.
Manual therapy
One of the alternative methods in which the spine is applied with hands . The effect is possible in combination with other physiotherapeutic procedures.
Traditional medicine recipes
Treatment of the spine at home is carried out using ointments made from natural ingredients.
Popular recipe:
- 1/4 cup honey;
- 1/3 cup grated radish;
- 1/3 glass of vodka;
- 2 tsp. sea salt.
Keep in the refrigerator and heat before use.
In addition to massage with ointment, you can apply compresses of hop cones and fir oil to the affected area.
Components for the compress can cause allergies!
Surgery
If all of the above procedures are ineffective, the doctor may prescribe surgical treatment.
The main methods of surgical intervention:
- blockade - the surgeon destroys the nerve endings of the joint, thereby relieving pain;
- artificial joint transplantation.
Treatment
In most cases, the course of spondylosis is quite slow and requires virtually no treatment. With active spondylosis, treatment is required, which can be either conservative or, in some cases, surgical. Most often, spondylosis requires conservative treatment. Various treatment methods are used to treat spondylosis.
Acupuncture . This treatment method can reduce back and neck pain. The needles, which are inserted into specific points, can also be stimulated either mechanically or using electrical impulses. In addition, acupuncture increases the production of your own painkillers (endorphins).
Bed rest. In severe cases, severe pain may require bed rest for no more than 1-3 days. Prolonged bed rest increases the risk of developing complications such as deep vein thrombosis and back muscle wasting.
Traction therapy . In most cases, spinal traction is rarely needed or is used to relieve symptoms associated with spondylosis.
Manual therapy . Manipulations by a chiropractor using various techniques can increase the mobility of motor segments and remove muscle blocks.
Drug treatment . Drugs for the treatment of spondylosis are mainly used to relieve pain. These are drugs such as NSAIDs. In addition, muscle relaxants can be used if there are signs of muscle spasm. Tranquilizers can also be used to relax muscle spasms, which can also improve sleep. Opioids are used in the treatment of pain only occasionally, with severe pain. Any drug treatment should be carried out only as prescribed by the attending physician, since almost all drugs have a number of side effects and have certain contraindications.
Epidural steroid injections are sometimes used for pain syndromes and can relieve pain, especially when there is swelling and inflammation in the area of the spinal roots. Typically, the steroid is given in combination with a local anesthetic. The effect of such injections is usually limited to 2-3 days, but this allows you to remove the pathological process and use other treatment methods.
Injections into the facet joints are also used in the treatment of spondylosis and improve the mobility of the facet joints and reduce pain caused by arthrosis of the facet joints.
Exercise therapy . This treatment method is one of the most effective methods for treating spondylosis. Dosed physical activity allows you to restore normal muscle corset, reduce pain, increase spinal stability, improve the condition of the ligamentous apparatus and stop the progression of degenerative processes in the spine. As a rule, exercise therapy is prescribed after relief of acute pain.
Physiotherapy . Modern methods of physiotherapy (for example, HILT therapy, UVT therapy, electrical stimulation, cryotherapy) can not only reduce pain, but also influence to a certain extent the development of degenerative processes in the spine.
Corseting . The use of corsets for spondylosis is possible for a short period of time, since long-term use of a corset can lead to atrophy of the back muscles.
Lifestyle changes. Losing weight and maintaining a healthy lifestyle with a balanced diet, regular exercise, and quitting smoking can help treat spondylosis at any age.
Surgical methods of treatment
Only a small percentage of cases of spondylosis require surgical treatment. Surgical treatment methods are mainly necessary in the presence of persistent neurological symptoms resistant to conservative treatment (weakness in the limbs, dysfunction of the bladder, intestines or other manifestations of compressive effects on the spinal cord and roots). Surgical treatment consists of decompression of nerve structures (for example, removal of osteophytes that have a compressive effect on nerve structures). Depending on the extent of the operation, spinal fusion may be performed to stabilize the vertebrae. Currently, minimally invasive methods of surgical treatment are widely used, which allows you to quickly restore spinal function and normalize the quality of life.
Forecast
With timely diagnosis and proper therapy, the development of the disease can be stopped at its first stage . The difficulty lies only in the disdainful attitude of most people towards osteochondrosis or ignorance of the seriousness of the complications of this pathology.
Risks of complications
A sedentary lifestyle, heavy lifting, intense physical activity (excessive involvement in the gym, for example), a sharp change from a passive lifestyle to an active one - all these are risk factors for the appearance and complications of osteochondrosis.
The development of spinal pathologies is enhanced by metabolic disorders, poor blood circulation, and lack of fluid in the body. These factors provoke flattening of the fibrous ring and thinning of the spinal disc. And then the body turns on protection and begins to build bone tissue in order to distribute the increased load on the spine.
Complications
Incorrect treatment or lack thereof can lead to various complications:
- intervertebral hernia;
- spondyloarthrosis;
- muscle atrophy;
- complete immobility;
- the appearance of paresis in the limbs;
- paralysis;
- spinal cord injury;
- second degree disability;
- spinal stenosis;
- urinary incontinence (in some cases, fecal incontinence).
To avoid such consequences, it is necessary to consult a doctor in a timely manner and not put too much strain on the spine. It is worth noting that adults with this illness are not taken into the army.
Preventive measures
If you are prone to diseases of the musculoskeletal system, or if pathology is suspected, it is necessary to modify your lifestyle:
- lose weight;
- start actively engaging in physical activity (or simply walk more);
- adjust your diet in favor of healthy foods.
General recommendations
Rushing home after work in the office only to spend the entire evening on social networks again is a bad habit. The same bad thing is to stay glued to the TV while eating heavily on fast food. Prolonged stay in an uncomfortable position also negatively affects the condition of the spine.
Such habits must be eradicated. Even when working sedentarily, you can take a few minutes to take preventive measures:
- walk through the offices or floors;
- perform a simple head turn exercise.
To soothe the back muscles, it is necessary to maintain a comfortable temperature in the room.
What principles should be followed?
The algorithm for maintaining the spine in good condition is as follows:
- Increase physical activity.
- Do not overestimate your strength and do not lift weights.
- Don't overeat and watch your weight.
- Avoid fluid deficiency in the body (drink those notorious 1.5 liters of water per day).
- Regularly engage in preventive physical exercise.
The development of spondylosis and spondyloarthrosis can be avoided provided that osteochondrosis is diagnosed and treated in a timely manner. But since most neurology patients do not do this, they need to carefully listen to the body’s signals at the first stage of pathology development. It can still be stopped with drug therapy and therapeutic massage.
Topical warming agents, taking vitamin and mineral complexes, and introducing dairy products and fatty fish dishes into the diet will help prevent serious complications and the second and subsequent stages of the disease.
Spondylosis of the lumbosacral region - protection of the body
If the formation of protective spines did not occur, the spine would suffer from unbearable pain, and it would be impossible to move at all.
Nature created our skeleton so cleverly that the breakdown of some individual parts does not lead to disaster. This is especially confirmed by such a disease as deforming arthrosis. According to textbooks, the last stages of arthrosis are generally incompatible with movements, but in practice we very rarely encounter complete disability of the joint.
This disease causes a significant deterioration in quality of life and is completely incurable.
Relieving the patient of pain and preventing complete ossification (ossification) of the external cartilaginous tissues and the anterior longitudinal ligament of the spine.
- With age, metabolic processes in bone tissue, as in the entire body, slow down. This is an inevitable picture of aging. The result is:
- Lack of essential substances in the vertebrae
- Replacement of areas of destruction with bone growths
Destruction of cartilage surfaces and discs as a result of deficiency of chondroitin and collagen
Osteophytes, increasing the contact surface of the vertebrae, relieve the segment from excess load, preventing complete destruction
- Fractures, ligament injuries and other injuries
- The disease develops slowly and initially manifests itself in mild pain, with pain symptoms occurring both during movement and after rest
- Just like arthrosis, spondylosis gives a feeling of stiffness in the morning
- Pain reduction is observed in the bending position
- Another symptom is intermittent claudication: Due to pain while moving, a person is forced to periodically stop. After rest, the pain temporarily subsides. However, the same symptom occurs not only with spondylosis. Its reasons may be:
When nerve roots are irritated, symptoms also occur:
- Tingling sensations on the skin of the lower back and legs
- Feelings of “cottoniness” in the limbs
Symptoms of spondylosis
The first stage of the disease may not manifest itself in any way, however, with the progression and increase in osteophytes, symptoms appear that are useful for diagnosis:
- stiffness of the lumbar region - as was noted earlier, spikes reduce the intervertebral distance, as a result of which the flexibility of the back deteriorates;
- pain - can be either acute, when a spinal nerve is pinched, or chronic (i.e. constant). The main diagnostic sign of spondylosis is a decrease in pain when bending the whole body forward or lying on the side, curled up. This is explained by the fact that decompression of the spinal nerves occurs;
- false lameness - appears due to damage to the sacral nerve, but pain in the legs does not disappear with rest, which helps differentiate with obliterating vascular endarteritis;
- loss of sensitivity of the skin at the site of nerve damage;
- during an examination by a neurologist, the patient feels pain upon palpation of the spinous processes, at the site of compression of the spinal nerves;
- tingling of the lower extremities, inability to straighten the knee - these are signs of the last stage.
Features and causes of the disease
Spondylosis is characterized by a number of signs that must be taken into account when suspecting or diagnosing this condition.
- As a rule, pathology develops in the area between the 4th and 5th vertebrae. Damage does not affect the entire intervertebral disc, but is observed only on the outer part of the so-called fibrous ring.
- If the pathology is not treated, the vertebral bone tissue can grow, forming osteophytes (“spikes”).
- Due to dystrophic changes, the condition of the spine deteriorates greatly. The patient often feels pain, which can be relieved by changing body position.
- The severe stage of the disease is characterized by a strong proliferation of osteophytes, which leads to the development of spondylosis deformans in the lumbar region.
- The patient's nerve endings suffer, lameness may develop, limbs often go numb, and blood circulation noticeably deteriorates.
If proper therapy is not carried out on time, a person will constantly struggle with severe pain.
A characteristic feature of spondylosis is the presence of osteophytes, which, during the course of the disease, grow in different parts of the spine. With the help of such bone growths, the body fights fibrous deformation. Thanks to osteophytes, the spinal column becomes less mobile, so the vertebrae do not move.
To date, doctors cannot explain what exactly causes the negative changes. But most experts say that spondylosis deformans develops most often in people with abnormal metabolism. Another reason may be prolonged compression of the vertebrae during heavy physical labor or excess stress.
We invite you to familiarize yourself with: Physical therapy exercises for protrusion of the intervertebral discs of the lumbar spine. Therapeutic exercises for the lumbosacral region
In addition, the following factors may influence the development of the disease:
- excess weight;
- endocrine diseases;
- passive lifestyle;
- minimal physical activity;
- chronic diseases of the liver, kidneys, diabetes mellitus;
- professional sports;
- eating the “wrong” food (too much fat and carbohydrates in the diet);
- elderly age;
- hard physical work;
- some features of work (for example, long periods of driving).
This pathology is associated with wear and aging of the anatomical structures of the spine. Dystrophic changes occur in the outer fibers of the annulus fibrosus; it puts pressure on the nucleus pulposus, which leads to its protrusion. In this case, osteophytes are formed.
The development of spondylosis is provoked by degenerative changes in the intervertebral discs. The body exhibits a compensatory reaction to this in the form of pathological growths of bone tissue - osteophytes, which are designed to support the intervertebral discs and prevent their loss.
Spondylosis manifests itself by the appearance of growths. They usually affect the fourth or fifth vertebra on one or both sides, deforming and destroying it.
Spondylosis of the lumbar spine occurs as a complication of osteochondrosis. In cases where the patient does not receive full treatment, the cartilage tissue begins to undergo significant destructive changes. Intervertebral discs lose their shape, lose their basic functions, and become deformed. Such processes affect bone tissue, joints, blood vessels and nerve endings.
Spondylosis manifests itself by the appearance of growths. They usually affect the fourth or fifth vertebra on one or both sides, deforming and destroying it. Gradually, the fibrous ring is drawn into the development of the disease, in which cracks appear.
As a result, the muscular-ligamentous apparatus suffers, exfoliating from its base under the influence of osteophytes. They themselves continue to grow, leading to the final destruction of surrounding structures.
Therefore, the answer to the question of what spondylosis is is that it is a pathology that occurs due to a number of reasons. Most often it develops due to:
- age-related changes;
- injuries;
- obesity;
- metabolic disorders;
- hereditary predisposition;
- physical inactivity;
- posture disorders;
- unbalanced diet.
Endocrine diseases contribute significantly to the progression of lumbar spondylosis. Chronic internal pathologies, diseases of the spinal column and joints can also provoke its development.
The reasons for its onset can also be excessive physical activity, prolonged weightlifting, or working in an uncomfortable position.
The effect of vibration and elevated temperature on the spine also has an adverse effect. Therefore, treatment of this disease should be preceded by a thorough study of its symptoms, the general condition of the patient and the internal processes in his body.
Stages of the disease
The classification of pathology has several criteria, thanks to which different stages are distinguished:
- X-ray;
- functional failure;
- degree of the pathological process.
X-ray stage
This stage of the disease, in turn, has several sub-stages-levels, which characterize the degree of spread of the disease and damage to bone tissue.
The first determines osteophytes at the initial stage, when the structure of the discs has not yet been damaged.
The second one helps to notice the formation of a new joint by osteophytes that extend beyond the discs.
Third, a pathological process appears, which indicates initial changes in the spinal column and narrowing of the canal.
Most often, the stages are mixed and can only be identified at the last stage of the process. Radiological criteria remain the basis for an accurate diagnosis, but can be used in conjunction with others.
Types of pathology
There are several classifications of spondylosis, each based on a specific criterion.
For patient management and treatment process, it is important to determine the severity of the pathology.
- 1st degree. Degenerative processes are just beginning to take shape. The patient does not feel any symptoms, X-rays show no pathology.
- 2nd degree. Symptoms such as lower back pain and limited mobility appear. A person feels difficulties at work if during his activities he experiences stress on the lower back.
- 3rd degree. The ability to work is impaired, the pain syndrome increases. This may result in the person being classified as disabled.
An X-ray can also determine the stage of lumbar spondylosis:
- Initial stage. Osteophytes are observed, most of which are located on the anterior portion of the vertebra. Due to them, the spinal canal narrows. A distinctive feature is that the growth of osteophytes does not spread to adjacent vertebrae.
- Second stage. Osteophytes pass from the anterior edge and cover the vertebral body with an arch. These bone growths can merge and deform the spine. Thus, the formation of a false joint occurs.
- Third stage. Osteophytes fuse completely and form a single bone bracket. At this stage, the process turns into spondyloarthrosis.
We suggest you familiarize yourself with: MRI of the temporomandibular joint in Moscow
These stages of the process allow you to clearly see why stiffness of movement occurs in the affected area. As a result, the intervertebral discs are flattened by neighboring vertebrae.
There is another type of classification, which is based on the speed of development of the pathological process. There are slowly, moderately and rapidly progressive spondylosis of the lumbar spine. There is also a lightning-fast form. This explains the fact that in some patients, changes on the radiograph take a long time to form and sequentially, while in others the disease goes through all stages in a short period of time and quickly leads to disability. As a rule, the rapid development of the disease is observed when the growth of osteophytes is caused by another, primary disease.
Prevention of exacerbations and prevention of spondylosis
Methods for preventing spondylosis:
- Compliance with a balanced nutrition system;
- Performing gymnastic exercises aimed at developing the muscle corset and strengthening it;
- Active lifestyle, lots of movement;
- Avoiding prolonged exposure to water-like poses;
- Curtain control;
- Avoiding hypothermia;
- Avoiding overload of the spinal column.
Prevention of exacerbations of spondylosis:
- Constant control of the correct position of the back;
- Maintaining correct posture;
- When the body is in an upright position for a long time, lean on something to evenly distribute the body weight;
- Correctly lift heavy objects: gradually, avoiding jerks;
- Do periodic warm-ups during sedentary work;
- Avoid a bent back position;
- Swimming;
- Special gymnastics.
| Spondylosis is completely treatable. It is important to “catch” the disease at an early stage and carry out timely diagnosis. | |
Recovery prognosis
It is impossible to cure spondylosis completely, but you can significantly improve your well-being with the help of medical procedures.
Timely therapy can reduce or eliminate pain, improve blood supply to the tissues of the lumbosacral region, strengthen muscles and ligaments, reduce friction between the vertebrae, and improve the structure of cartilage discs.
Competent actions of the doctor contribute to the complete cessation or slowdown of the formation of new osteophytes, which has a positive effect on the functionality of the spinal column.
Signs of spondylosis
Lumbosacral spondylosis does not always present with any symptoms; it can be an incidental finding on an x-ray. The most common complaints of patients are rapid fatigue when walking, sitting, periodic mild pain in the back after exercise, when the weather changes, some limitation of spinal mobility, stiffness, and sometimes lower back pain radiating to the buttock and leg.
On examination, limitation of movements in the lumbosacral region can be noted. The patient can independently assess the mobility of the spinal column. To do this, you need to put your feet together and bend over without bending your knees, you need to try to touch the floor with your third fingers. If this is not possible, there is limited flexion in the spine. An orthopedist can also assess the range of motion specifically in the lumbosacral region. He makes a mark in the projection of the spinous process of the 5th lumbar vertebra and asks the patient to bend over as much as possible. In healthy people, at the moment of tilting, this distance increases by 4-5 cm; with severe spondylosis, it practically does not change.
Other signs of spondylosis: pain when feeling or tapping on the spinous processes of the lumbar vertebrae, with sudden movements, pain in the lower back when going down stairs, turning the body.
How is the diagnosis done?
To confirm the diagnosis, it is necessary to carry out:
- comprehensive neurological examination of the patient;
- X-ray examination of the spine - images should be taken in standard and lateral projections. This research method is used to assess the condition of the vertebrae, identify osteophytes, pathological mobility of individual elements of the spine at extreme degrees of flexion and extension, and detect displacement;
- computed tomography and magnetic resonance imaging – used to determine the height of the intervertebral discs, the width of the spinal canal and its condition.
Surgery
Surgery can get rid of osteophytes, but surgical intervention is indicated only in cases of a serious complication of spondylosis - “cauda equina syndrome,” which occurs when the protrusion of bony protrusions into the lumen of the spinal canal leads to compression of the bundle of nerve roots. The syndrome can manifest itself as acute pain, paralysis of the legs, and urinary incontinence.
In the simplest case, the operation to remove osteophytes looks like this: the surgeon makes an incision in the projection of the affected area of the spine, then, using special tools, saws off or trims the bone growths. This way the diameter of the spinal canal in the area of compression or the opening through which the suffering nerve exits can be expanded. It is possible to completely remove the affected vertebra or replace it with an artificial prosthesis.
Recently, minimally invasive surgical methods have been increasingly used. The work is performed using a microscope and micro-instruments, the incision is 2–4 cm (as opposed to 10 cm in a classic operation). Trauma to surrounding tissues is reduced and the healing period is shortened.
Description of the disease
Spondylosis is a progressive chronic disease that affects the joints of the spinal column. Being a degenerative-dystrophic pathology, spondylosis leads to the formation of bone growths in the vertebral bodies.
Ultimately, bone formations reduce intervertebral spaces, leading to compression of nerve roots, vessels and tendons, which manifests itself in the form of neurological disorders. In some cases, against the background of spondylosis, fusion of adjacent vertebrae is possible, which leads to partial immobilization of the affected part of the spine.
In most cases, spondylosis occurs in people over 50 years of age, but cases of the disease in people under 30 years of age are very rare and are usually associated with total physical inactivity and detraining.
Reasons for development
As a rule, spondylosis is localized in the lumbar region of the spine (approximately 70% of all cases). The reason is quite banal: it is this part of the spinal column that bears the maximum load.
In general, the reasons for the development of spinal spondylosis in most cases are as follows:
- the presence of chronic untreated degenerative-dystrophic pathologies of the spine (for example, osteochondrosis);
- inactive lifestyle and accompanying physical inactivity with detraining;
- excessive physical activity leading to overstrain of the spinal column;
- frequent consumption of fatty and overly salty foods;
- Causes of spondylosis that require more in-depth research also include smoking, alcohol and drug use;
- incorrect posture along with excess weight;
- as a risk factor – old age.
Classification of the disease by degree
Spondylosis is divided into three degrees, which is obvious; the higher the degree, the more serious the patient’s condition.
In the vast majority of cases, first-degree spondylosis remains unnoticed by the patient and surrounding people for a long time. However, if there is damage to the cervical spine, then at the first stage of the disease a moderate disturbance in the blood supply to the brain may develop.
In the presence of the second degree of the disease, fairly pronounced symptoms are noted. If the cervical spine is affected - dizziness, fainting, tinnitus, visual artifacts in the field of vision (for example, floaters).
When the lumbar region is affected, there is impaired coordination of movement when walking, frequent urge to urinate and paresthesia in the lower extremities (usually in the fingers).
The third degree of spondylosis is very difficult. Severe neurological disorders, unsteadiness of gait, falls, serious pain in the back and sometimes in the peritoneum are noted. With the third degree of spondylosis, partial or complete loss of spinal mobility is possible.
How dangerous is the disease?
In the early stages of spondylosis, there are no health- or even life-threatening symptoms. The only problem is the presence of a disease, which, in the absence of adequate therapy, will tirelessly progress.
At later stages, serious damage to the spine develops (the specific part where the pathological process is localized). When the cervical spine is damaged, a disruption of blood flow in the vertebral arteries develops, which can lead to loss of consciousness and even ischemic attacks.
Read also: Lower back pain causes in men treatment
At the most advanced stages, partial loss of motor skills, inability to move normally, and immobilization (immobility) of the spinal column are possible. Simply put, spondylosis can be disabling.
Causes of lumbar spondylosis
Intervertebral disc herniation. This may occur due to problems with degeneration of the central pulp nucleus or due to disruption of the surrounding fibrous ring. The main reasons that can contribute to the occurrence of a herniated disc are the following:
- Deformations. They can be congenital or acquired. Those that appear may be the result of surgery, trauma, etc.
- Degenerative processes. The reasons that can initiate processes of this type are varied: first of all, age, which causes dehydration of the fleshy core of the intervertebral disc, but also the deposition of collagen, which strengthens it and ultimately causes it to lose its natural elasticity characteristics.
- Cracks. These injuries can be caused by either severe trauma or continuous microtrauma, such as in people who perform heavy portering jobs or require constant heavy lifting. Correct spinal posture is important. In fact, disc degeneration can also be caused by sedentary work that forces you to remain in an abnormal position for long periods of time, with severe muscle tension placing abnormal stress on the spine.
Spinal stenosis. The spinal canal consists of a sequence of vertebral bodies, which, one after the other, have openings in the center. The canal contains bone marrow, meninges, and nerve endings that branch from the dural sac to the meninges of each intervertebral disc. The cause of stenosis may be:
- congenital malformation;
- degenerative malformation acquired as a result of problems with arthrosis;
- hypertrophy of the ligaments that stabilize the joint formed by two overlapping vertebrae (ligamentum flavum);
- unevenness of the plate of bone tissue that covers the vertebra at the level of the arch.
The appearance of osteophytes is a natural reaction of the body to disturbances in the functioning of the intervertebral discs. In other words, the body tries to independently adapt to new living conditions.
Degeneration of intervertebral discs causes the development of spondylosis. Some people think that osteophytes are salt deposits, but in fact they represent the growth of bone tissue - this is how the body strives to “support” the vertebral discs and prevent their loss.
Factors that provoke spondylosis:
- Excess weight. Throughout a person’s life, the spinal column (in particular, the lumbosacral region) experiences enormous loads. Excess weight increases the load on the spine and negatively affects health.
- Dietary disorder. Degenerative changes can be triggered by “improper” nutrition: a predominance of carbohydrate and fatty foods in the diet, a lack of fresh fruits and vegetables in the daily menu.
- Exercise stress. Both professional athletes and people leading a sedentary lifestyle can become the owner of spondylosis. Doctors advise not to go from one extreme to another, but to find a “golden mean”, because sport should bring health.
- Metabolic disorders. Some chronic metabolic disorders (atherosclerosis, diseases of the endocrine system, diabetes mellitus) are a favorable background for the development of spondylosis.
- Professional activity. Most often, spondylosis develops in people who constantly experience vibration loads, for example, truck drivers.
- Age-related changes. With age, various pathological processes occur in the intervertebral joints, and the bones become less strong. All this serves as fertile ground for the development of spondylosis.
- Spinal injuries.
Experts classify spondylosis as a pathology, the occurrence of which is caused by many factors, the main of which are natural age-related changes in the intervertebral discs, ligaments and bones of the spinal column.
- A sedentary lifestyle, which causes muscle weakening. Moreover, occasional physical activity can lead to microtrauma of the spine or its ligaments and further provoke the replacement of injured ligaments with bone tissue.
- Spinal overload
- Poor nutrition
- Overweight
- Hard physical labor
- Chronic diseases (diabetes mellitus, atherosclerosis)
- Constitutional predisposition
- Previous spinal injuries
- Poor posture (scoliosis, kyphosis, etc.)
If the height of the intervertebral discs remains unchanged for a long time, spondylosis of the lumbar spine may not reveal itself. And only in the later stages or the appearance of other degenerative-dystrophic pathologies, in which compression of the nerves occurs, pain, impaired sensitivity and motor activity may appear.
Depletion of cartilage tissue causes injury to the vertebrae and the appearance of notches on them
With this disease, the affected area of the spine becomes fixed, causing spasm of nearby muscles and irritation of the nerve endings of the ligaments. With lumbar spondylosis, the 4th and 5th vertebrae are most often deformed. Osteophytes cause irritation of nerve endings, causing radicular symptoms. There is a feeling of discomfort in the buttock, thigh and leg, and the so-called symptom of spinal (false) intermittent claudication may appear.
The sensations intensify when walking or staying in an upright position for a long time. At the initial stage of the disease, there may be no pain symptoms and the only manifestation of spondylosis will be limited mobility. In the later stages, the main symptoms are dull aching pain, a feeling of heaviness in the spine and limited mobility. The pain intensifies during the day and does not go away at night.
Only a doctor can prescribe a course of therapy for such a disease. He must conduct a detailed diagnosis and, having made a diagnosis, prescribe a course of treatment. A disease such as spondylosis of the lumbosacral spine is treated by taking non-steroidal anti-inflammatory drugs. Only a doctor can prescribe the exact dosage.
In addition, there are other ways to treat osteochondrosis and spondylosis. Quite often, patients turn to the methods of Tibetan medicine. This treatment is preventive in nature and can relieve pain, inflammation, and prevent drying out of the vertebrae and their deformation. Such methods slow down the progression of the disease and prevent it from becoming chronic.
The patient is offered a course of massage therapy, acupuncture, heating and physiotherapy. Herbal medicines are used to improve blood circulation and supply tissues with nutrients. They significantly improve the effect of conventional procedures. After a course of such treatment, the patient’s back pain disappears, muscle spasms stop, disc nutrition improves, and metabolism accelerates.
Factors influencing the occurrence of spondylosis and contributing to its development:
- Intense physical activity that puts pressure on the spine.
- Disorders of nutrition of the cartilage tissue of the intervertebral discs due to negative changes in the metabolic system.
- Incorrect posture.
- Atrophy of the back muscles and ligaments, which occurs due to a sedentary lifestyle.
- Mechanical injuries of the spine.
Spondylosis: misconceptions associated with the disease
There are a number of signs and statements that are erroneously attributed to the disease we are considering. Let us dwell on their main variants, explaining at the same time the essence of the processes opposed to such misconceptions.
- Spondylosis is the result of salt deposition in the affected area
This misconception is one of the most common in connection with spondylosis. The course of spondylosis is determined by degenerative-dystrophic changes that develop in the affected discs; these changes have nothing to do with salt deposition.
Osteophytes (also known as spondylophytes), which look like spiky formations that form along the edges of the vertebrae, are formed, as we have already noted, from bone tissue, that is, by nature they can no longer be saline or, as another example, calcareous. The root cause of spondylosis, as well as osteochondrosis, the signs of which are also associated with this disease, is a violation of metabolic processes against the background of insufficient nutrition of the vertebral tissues with the concomitant irrationality of the distribution of loads placed on the spine. The main factor accompanying the disease is muscle spasms that occur in the back, lumbar and cervical spine, and it is these spasms that cause the effect in the form of a constricting load on it, also acting as a cause of impaired blood supply and, accordingly, nutrition of the tissues of the discs and vertebral joints.
- Spondylosis is an independent disease
This statement is also erroneous, let us explain exactly why. The fact is that spondylosis itself is not a disease, but a kind of defensive reaction that occurs on the part of the body as a response to current destructive processes affecting the intervertebral discs. For this reason, treatment of spondylosis is focused on the root cause, which is considered nothing more than spinal osteochondrosis. It is also important to understand the fact that it is impossible to get rid of already formed bone growths. Meanwhile, a completely acceptable option is to influence the disease in terms of its further progression, or more precisely, to prevent it and, accordingly, exclude further deformations that the spine is subject to against the background of spondylosis.
- Ointments with an anti-inflammatory effect help cure spondylosis
This opinion is also a misconception, the reason for this is the peculiarities of the processes inherent in this disease. After all, as we found out, spondylosis is a degenerative-dystrophic disease, but not inflammatory. Accordingly, the use of anti-inflammatory drugs simply does not make sense for spondylosis. The reason for the existing misconception regarding the effectiveness of using such ointments is the mistake of many patients, in which they associate the symptoms of spondylosis with the manifestations of an inflammatory disease affecting the intervertebral joints; in particular, ankylosing spondylitis is considered such a disease.
- Manual therapy is an effective method of treating spondylosis
Again, this belief is a misconception, which is due to the confusion that arises regarding spondylosis and a disease such as spondylolisthesis (vertebral subluxation). Manual therapy can really cope with subluxation of the vertebrae; moreover, it can also eliminate the state of compression in which the nerve roots are located, and accordingly, the pain that accompanies this can also be eliminated. Meanwhile, the restoration of metabolic processes, as well as the stop of compensatory processes caused by spondylosis along with the accompanying bone growths due to manual therapy, is a result that is considered impossible. Thus, we add that stopping (eliminating) an acute attack of pain is one thing, but preventing its reoccurrence is another. In this case, complex treatment is necessary, and manual therapy is only one of the measures, but not the main and only one.
- Spondylosis can be cured only through surgical intervention, that is, through surgery
As in previous cases, this statement is incorrect. Surgical treatment is not necessary in most cases of spondylosis. Indications for surgery appear only when the disease has progressed to a form of damage in which the spinal cord has been subjected to extremely strong compression, which occurs extremely rarely. Most often, surgery becomes necessary for such a complication of osteochondrosis (the basis of spondylosis) as an intervertebral hernia - here surgery is considered as the main treatment option.
- Spondylosis is a constant companion of elderly patients; a cure for this disease is impossible.
In old age, when reaching the later stages of spondylosis, you really shouldn’t count on an absolute cure. Meanwhile, through the implementation of certain treatment methods, the possibility of truly effective results is possible, thereby significantly improving the quality of life. In addition, there is the possibility of influencing the mobility of the spine due to them. If treatment begins in the early stages, the development of spondylosis can be significantly slowed down and even stopped. For this reason, the “sentence” of incurability can be considered as a flexible option that is subject to correction, and the sooner the appropriate impact is provided as part of the treatment of this disease, the greater the chance of eliminating its development.