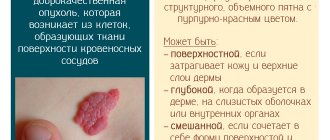
Based on the name of the pathology, it can be understood that hemangioma is a benign tumor, the substrate for which is the cells of blood vessels. Such neoplasms can appear in any part of the body where there is a vascular network. Some hemangiomas can be seen with the naked eye. For example, skin growths look like red birthmarks, slightly raised above the surface. Some are detected only by characteristic symptoms and the results of instrumental examination, for example, spinal hemangioma.
Spinal hemangioma: what is it?
The term vertebral angioma or hemangioma of the spinal column refers to a benign neoplasm formed from vascular tissues. In most cases, the process affects one or more (up to 5) vertebrae, does not have a tendency to malignancy (malignancy) and does not spread to nearby tissues.
Single or multiple hemangiomas of the vertebral body grow slowly, gradually growing through the bone tissue and disrupting their structure, which leads to increased fragility. The degree of danger of the disease to humans depends on several factors, which include:
- gender – in men the disease is much less common, and due to the massive musculoskeletal system compared to women, it develops much more slowly;
- age – in older people, vertebral hemangioma occurs more often and is more severe due to age-related changes in the skeleton;
- localization – tumor of the cervical spine – high risk of complications;
- number of lesions - multiple vascular neoplasms in the vertebrae at the same time are quite rare, however, such cases often have a severe course.
Despite its asymptomatic course, spinal hemangioma is a dangerous disease that, without timely treatment, can lead to irreversible changes in bone tissue.
Kinds
The classification of vertebral (vertebral) tumors is based on several parameters. Depending on the number of affected vertebrae, there are:
- Single hemangiomas, which are found most often.
- Multiple, often small formations that affect 2–5 (or more) vertebrae (diagnosed 2 times less often than single forms).
According to the structure they are distinguished:
- capillary hemangiomas of the spine, consisting of a plexus of capillaries surrounded by fat and fibrous connective tissue. Such formations very rarely cause pain and require surgical removal;
- racematous, woven from large blood vessels;
- cavernous, formed from separate cavities - caverns, connected by fragments of bone tissue. This type of vascular formation is less common and can cause severe pain;
- mixed hemangiomas are formed from vascular and bone tissue with caverns.
In rare cases, an atypical vertebral hemangioma is found, consisting of several sections filled with blood, covered with keratinized tissue cells.
This disease occurs in different parts of the spinal column. Vascular formations are classified according to their location as follows:
- Thoracic hemangioma is the most common anomaly, occurring in almost 60% of patients with vascular vertebral tumors.
- Tumor of the lumbar region (28 – 30%).
- Vascular neoplasm of the cervical spine (in 6% of patients).
- Hemangioma of the sacral region is the most rarely diagnosed formation (no more than 5%), which develops in the vertebrae S1 – S5.
From the point of view of a narrower localization, hemangioma of the vertebral body is most often detected. Less commonly, a vertebral tumor forms in the processes and arches, and very rarely in the spinal canal.
Classification of the disease (types and forms)
Depending on the number of lesions, a single tumor is distinguished, which affects only one vertebra, and multiple hemangiomas of different parts of the spine. In the presence of several neoplasms, the disease is called hemangiomatosis, with this disease the maximum number of lesions reaches five. Other classifications divide vascular neoplasms of the vertebrae according to histological structure, prevalence and aggressiveness of clinical manifestations.
Types of spinal hemangiomas depending on the histological features of the tumor process:
- Capillary - the tumor is formed by many practically unchanged capillaries with layers of fibrous and fatty cells.
- Cavernous - the neoplasm consists of a large number of dilated vessels, which are cavities filled with blood. The walls of interconnected cavities are made of thin connective tissue covered with a layer of endothelial cells, which normally line the surface of blood vessels from the inside. This type of vertebral hemangioma is not prone to destructive growth, but more often than others provokes the formation of compression fractures.
- Racematous - consists of slightly changed large vessels (both veins and arteries).
- Mixed education.
An atypical form of spinal hemangioma is rarely diagnosed. A feature of the histological structure is that its structures are covered with keratinized cells
Based on the prevalence of the process, there are five types of disease:
- first – the neoplasm spreads to all vertebral structures;
- second – the lesion is localized only in the body;
- third – the tumor is localized in the posterior semi-ring of the vertebral arch;
- fourth – the body and partially the posterior semi-ring are affected;
- fifth – characterized by external (periosteal, epidural) or intracanal (intramedullary) localization.
Based on clinical manifestations, two forms of the disease are distinguished (asymptomatic and symptomatic), which can have a non-aggressive and aggressive course.
Causes
After the formation of a pathological formation from the vessels, their destruction often occurs. The blood, leaving the vessels, pours into the formed cavity and soon leaves. In its place, tumors begin to form, filling the entire cavity and growing beyond its size.
A vertebral hemangioma can form for a number of reasons:
- Genetic predisposition. Hereditary factors can play a huge role in the formation of pathological formations;
- Hormonal level. In the female body, estrogen levels are much higher. It is this hormone that takes part in the formation of hemangioma of the vertebral bodies;
- Increased physical activity. With excessive pressure, the vertebrae age rapidly and microcracks appear in them.
- Effect of radiation;
- The effect of some components of drugs.
The most common hemangioma is the lumbar spine and the thoracic hemangioma. For the cervical spine, this pathology is even more dangerous. But the main division into more and less dangerous conditions is classification according to the degree of aggressiveness:
- Aggressive hemangiomas. This condition is characterized by a rapid increase in tumor size. Soon cracks in the vertebrae and compression fractures will form.
- Non-aggressive hemangiomas. If such tumors are present in the spine, symptoms may be completely absent or very mild. The course of the disease is favorable; the patient may not even know about the presence of such a pathology all his life.
Reasons for the development of the disease
The exact causes of vertebral hemangiomas have not yet been clarified. However, scientists have identified the factors that provoke their occurrence. These include:
- Genetic predisposition - the development of a neoplasm in this case is associated with a hereditarily determined disorder in the structure of the vascular endothelium.
- Changes in hormonal levels - estrogen plays a significant role in the formation of vascular tumors. Since the level of this hormone is much higher in women, they are included in the main risk group.
- Previous spinal injuries - it has been scientifically proven that injuries can provoke the occurrence of vascular tumors, and if present, accelerate their development.
- Impaired blood supply to the vascular walls - insufficient blood supply to the vascular walls leads to the development of local hypoxia and an increase in their lumen.
- Increased physical activity creates conditions for the development of microtraumas of the spinal column.
- The influence of physical factors - radiation, high temperatures, chemicals (including some medications) can cause disruption of the structure of the vascular wall.
- Age-related changes in bone tissue - hemangiomas often form in older people suffering from osteoporosis.
- Intrauterine disorders in the formation of tissues of the vascular walls often cause the development of congenital hemangiomas of the spinal column.
Reasons for the formation of a benign tumor
Hemangioma is considered the most common benign tumor of the spine. In the cervical region it is almost never found, which is due to the predominance of small vessels in this area. In the vast majority of cases, its detection occurs accidentally during the diagnosis of other disorders.
Frequent spinal injuries can lead to the appearance of hemangioma.
Among the suspected causes of pathology, doctors identify:
- Predisposition. Spinal hemangiomas are usually found in people whose relatives had similar problems with intervertebral discs and blood vessels in this area.
- Female. In women, pathology is detected much more often, which may be due to fluctuations in estrogen levels during pregnancy and menopause.
- Frequent or severe spinal injuries. Bruises, excessive stress on blood vessels, and constant tension lead to the expansion of vascular channels and the growth of pathological cells.
Growth is caused by certain disorders in the body, which often occur through the fault of the patient himself due to an incorrect lifestyle, but sometimes they can occur for no apparent reason.
The reliable reasons for the formation of hemangiomas are unknown to medicine. However, doctors assume that heredity plays the most significant role in this.
Symptoms of spinal hemangioma depending on location
Spinal hemangioma often has no symptoms; only 10% of diagnosed cases have clinical manifestations of the disease. Asymptomatic forms are usually diagnosed during a spinal examination for another disease.
Symptomatic forms are manifested by pain, the characteristics of which depend on the size and location of the tumor. Other clinical signs of spinal hemangioma appear only when the tumor is large.
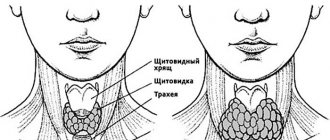
Clinical signs of cervical hemangioma
Hemangioma localized in the cervical spine is extremely rare (in 1 case out of 100), and is almost never located in the upper vertebrae. In most cases, the tumor is diagnosed in the C6 and C7 vertebrae.
Symptoms of hemangioma of the cervical vertebral body:
- headache (depending on the size of the tumor, the intensity ranges from mild discomfort to migraine);
- impaired sensitivity of the upper extremities - tingling or numbness of the fingers, palms;
- decreased hearing and visual acuity;
- sleep disorders;
- unmotivated irritability;
- unstable emotional state.
Doctors believe that this location of the tumor is the most dangerous, since an increase in size leads to disruption of the blood supply to the brain.
If there is a history of cardiac diseases in a patient with a hemangioma of the cervical vertebra, the risk of developing ischemic strokes increases - this is caused by compression of the vertebral artery.
Symptoms of hemangioma of the thoracic spine
The most common (about 65% of cases) hemangioma occurs, localized in the thoracic spine. According to statistics, the typical hemangioma is the body of the Th2, Th9, Th10, Th11 vertebra.
Clinical manifestations:
- pain in the area where the tumor is located, which, as its size increases, spreads along the pinched nerves;
- weakness and numbness of the arms, scapular area;
- with large tumor sizes - the appearance of paresis and paralysis;
- disruption of the digestive tract, cardiovascular system, and urinary tract.
In some cases, a hemangioma located in the th12 vertebral body causes infertility in women.
Clinical signs of a tumor of the lumbar and sacral regions
Hemangiomas in the lumbar and sacral spine have the same manifestations. Neoplasms are more common in the body of the L1, L2, L3, L4 vertebrae, practically without affecting L5. In the sacral region, vascular neoplasms occur in 5 out of 100 people with this disease.
Symptoms of the disease in this case:
- pain localized in the lumbar and groin region spreading to the hips;
- numbness of the skin of the lower extremities;
- development of paresis and paralysis of the legs;
- disruption of the functioning of the pelvic organs if the hemangioma is located in the body of the L4 and L3 vertebrae.
Sometimes lumbar hemangiomas (especially those affecting the L5 vertebral body) lead to decreased potency and male infertility.
Danger and consequences of benign vascular tumor
The main danger of spinal hemangioma in the thoracic region is its intensive growth. Small tumors do not cause harm to health, but large, enlarging tumors can lead to changes in the bone structure of the spine. This causes a compression fracture due to heavy lifting and physical activity.
As the hemangioma grows, it can cause destruction of the vertebra
As a precaution, doctors do not recommend that patients leave the tumor unattended, insisting that the risks of its degeneration cannot be ignored.
The danger of progressive hemangioma of the thoracic spine lies in the following consequences:
- paralysis of the upper limbs;
- compression of the spinal cord, leading to acute disturbances in the functioning of other organs;
- compression of nerve endings, leading to hand weakness and problems with their mobility;
- vertebral injuries and fractures;
- internal bleeding caused by rupture of the soft tissue of the tumor.
Treating benign tumors is much easier than malignant ones. This is important to prevent the hemangioma from growing through the bone tissue.
The risks of developing consequences largely depend on the location of the tumor, the number of vertebrae involved in the process, the age and gender of the person. In men, the vertebrae are larger, and therefore more resistant to pressure and destruction.
Why is spinal hemangioma dangerous?
Due to the predominantly asymptomatic nature of the disease, it is dangerous because complications develop over a long period of time, resulting in the slow destruction of bone and cartilage tissue at the site of the tumor.
Most often, vertebral hemangioma leads to the development of:
- compression fractures when making sudden movements;
- paralysis and paresis due to compression of the nerves and spinal cord by a space-occupying formation;
- massive bleeding caused by tumor rupture;
- dysfunction of internal organs due to compression of the spinal cord and peripheral nerves due to a decrease in the lumen of the spinal canal.
The earlier therapy is started, the lower the risk of developing irreversible changes in the bone tissue of the vertebrae. Therefore, even with minor discomfort in the spine, you should consult a doctor.
Complications
If vertebral hemangiomas reach critical sizes, there is a high risk of compression fracture. The tumor weakens the vertebra, growing from the inside and exerting constant pressure. When a vertebra is fractured, numbness of the limbs and severe pain (local and radiating to other parts of the body) occur. Another complication is a fracture of the vertebral processes, characterized by severe girdle pain, inability to lift the leg and paralysis.
| Please rate the article |
I RECOMMEND ON
Size at which hemangioma becomes dangerous
Not only clinical manifestations, but also the likelihood of developing complications depend on the size of the tumor. The most accurate results of determining the size of the tumor are obtained using MRI.
Whether the size of the tumor is dangerous depends on the location of the spinal hemangioma, since the vertebrae of different parts vary greatly in massiveness. The diameter of neoplasms of the lumbar vertebrae sometimes exceeds 50 mm.
| Spine department | Dangerous size of hemangioma |
| Cervical | With small sizes of the cervical vertebral bodies, a tumor of more than 5 mm becomes dangerous. |
| Chest | A neoplasm over 10 mm in diameter can cause a compression fracture or the development of neurological disorders. |
| Lumbar | A tumor with a diameter of 20 mm or more becomes dangerous, and tumors of 3-5 mm often regress on their own. |
| Sacral | 5% of diagnosed hemangiomas are found in this section; they become dangerous when they reach a size of 10 mm. |
Vertebral hemangioma - what is it?
Some blood vessels, expanding, intertwine with other vessels. Tumors are formed, the inner part of which is the epithelium. It is important to understand that such benign tumors can form in almost the entire body, except for some areas. But a vertebral body hemangioma, like no other, can be truly dangerous. Although the tumor slowly increases in size, it still grows and, sooner or later, can cause a compression fracture of the spine. The most common localization of pathological formations is the thoracic and lumbar spine.
Treatment of spinal hemangioma is a very real procedure, but the danger lies precisely in the fact that detection of the pathology may be too untimely.
- We advise you to read: tumors of the cervical spine.
Basic methods for diagnosing the disease
To determine the size of spinal hemangioma, high-quality diagnostics is necessary. The following studies are usually prescribed:
- X-ray images in several projections are used in adults for the initial diagnosis of spinal hemangioma. This type of research provides little information. The main advantage is the budget.
- Magnetic resonance imaging is the most accurate research method that helps to most effectively determine the location, size and structure of a vascular neoplasm. A negative feature of the study is the high price.
- Computed tomography is most often used in diagnosis. Combines accurate results with an affordable price.
- Scintigraphy (or molecular diagnostics) is a two-dimensional scanning with a gamma camera after intravenous administration of isotopes of radioactive substances into the body. Detects structural changes in bone tissue even with minimal tumor sizes.
- Ultrasound examination is used to identify impaired blood supply due to compression of the main arteries during hemangiomas of the cervical vertebral bodies.
Leading clinics in Israel
This kind of formation can resolve on its own in newborns up to 3 months. This is observed in 80% of cases. In an adult, the likelihood of the tumor disappearing without the use of a certain type of treatment is much lower. The disease is more common in women, as estrogen hormones accelerate tumor growth.
Also, the reasons for the formation of liver hemangioma include:
- Smoking, drinking alcohol;
- Taking contraceptives and other medications;
- Effect of radioactive radiation;
- Hepatitis;
- acute respiratory infections at the beginning of pregnancy;
- Hormonal therapy;
- Injuries, bruises;
- Obstruction of the biliary tract.
Hemangioma is most often a solitary neoplasm. In a newborn child, the tumor formation is very small, making it difficult to detect during a medical examination.
If there is a tumor whose size exceeds 5 cm, surgical intervention is required. Slight pressure on the tumor, falls and bruises can lead to its rupture, resulting in bleeding.
How to treat spinal hemangioma
In official medicine there are two directions for the treatment of vascular neoplasms of the spinal column. These include conservative therapy and surgical techniques. For hemangioma in the spine, the choice of treatment method can only be made by a doctor, taking into account the size of the tumor, aggressiveness and individual characteristics of the patient’s body.
Conservative treatment
This area includes drug and radiation therapy. Prescribed if the patient has a small hemangioma in the cervical, thoracic or lumbar spine.
Drug therapy
To relieve pain, strengthen vertebral bone tissue and slow tumor growth, the following groups of drugs are used:
- Non-steroidal anti-inflammatory drugs (ibuprofen, ortofen) - have anti-inflammatory and analgesic effects. This group of drugs should not be taken for longer than two months without consulting your doctor.
- Hormonal (usually prednisolone) - used in a course according to the scheme to eliminate the inflammatory process and slow down the growth of the tumor. Due to the many side effects, hormonal therapy is used only in aggressive cases.
- Analgesics (ketorol, ketorolac) – relieve severe pain.
- Beta blockers (obzidan, anaprilin, timolol) - reduce the activity of the renin-angiotensin system, which leads to stimulation of the functioning of peripheral vessels and a decrease in minute blood volume. The action of beta blockers slows down the growth of the tumor and stimulates regression.
- Drugs that enhance regeneration (actovegin) - due to the stimulation of cellular metabolism, natural tissue restoration is enhanced.
Radiation therapy
The method involves dosed exposure of the tumor tissue to ionizing radiation, which allows it to be partially destroyed. This fairly effective technique has several serious drawbacks:
- the patient is exposed to a large dose of radiation;
- hemangioma partially persists, which leads to relapses;
- after treatment, a cavity remains in the vertebral body, which often becomes the cause of a compression fracture.
This method is used mainly for older people who have serious contraindications to other treatment methods.
Surgical methods of treating the disease
Surgical interventions include gentle interventions and traditional surgical treatment. The choice of method is made by the doctor, taking into account the wishes of the patient.
Sclerosing treatment methods
Hemangioma of the lumbosacral and other parts of the spine is treated by injecting chemicals into it or the vessels that feed it. Two sclerosing techniques are used – embolization and alcoholization.
- Embolization - using a thin needle, a solution is injected into the vessels of the tumor, causing an embolism (blocking the lumen). As a result, the blood supply to the neoplasm is disrupted and it becomes sclerotic.
- Alcoholization - a solution of ethyl alcohol is injected into the hemangioma, which causes vascular sclerosis.
The disadvantages of both methods are the same - possible relapse of the disease, disruption of the structure of the vertebral bone tissue and blood supply to the spinal cord.
Puncture vertebroplasty
A fairly recent invention by French researchers has become a real breakthrough in the treatment of vascular neoplasms of the vertebrae. Vertebroplasty of hemangioma of various parts of the spine involves the introduction of special cement mixed with a radiopaque substance (barium sulfate) and titanium into the tumor cavity. This causes the tumor to shrink and stop its growth, and also strengthens the vertebral structures. The technique is used as an independent treatment or in combination with other methods. Recovery (rehabilitation) after vertebroplasty of spinal hemangioma takes two to three weeks.
Traditional surgery
This operation has been used since the 30s of the twentieth century and is prescribed when there is no effect after the use of conservative and gentle treatment methods. Surgery can lead to bleeding, disruption of the blood supply to the spinal cord and vertebral fracture. Therefore, it is used only in the presence of serious indications, which include:
- large size of spinal hemangioma is the main indication for surgery, which is prescribed if the diameter of the tumor reaches more than 1/3 of the vertebral body;
- aggressive clinical course;
- acceleration of growth;
- development of complications.
Removal of the tumor with resection of part of the vertebral bone tissue is performed from an open approach. It is impossible to cut out the entire tumor. In order to eliminate compression of the spinal cord and its roots, only the part that is located in the spinal canal is removed.
Non-traditional treatment methods
Treatment of spinal hemangioma with traditional methods and remedies is ineffective; the tumor can only be removed using traditional medicine.
However, to maintain health, you can use some decoctions and infusions of medicinal plants, but this should be done only after consulting a doctor.
Also, for the purpose of maintenance therapy for spinal hemangioma, homeopathy treatment is used, carefully observing the dosage of drugs. Not all homeopathic remedies can be combined with traditional medications and you should consult your doctor before using them.
Leeches are often used in alternative medicine. But spinal hemangiomas cannot be cured with hirudotherapy.
Treatment
The choice of treatment method for spinal hemangioma depends on the size, growth rate of the vertebral formation, severity of manifestations and signs of damage to the nervous system.
If a small vertebral hemangioma is detected, the doctor’s main task is to monitor the dynamic behavior of the tumor, monitor its growth, so as not to miss the spread of the tumor to the vertebral body, compression of blood vessels, nerve nodes and destruction of bone tissue.
Rapid growth of hemangioma in the spine, tumor involvement of 50–60% of the vertebral body, appearance of neurological symptoms, severe pain in the spine and other organs are indications for immediate treatment. As a rule, this occurs when the vascular tumor grows to 25–30 mm or more.
Drug therapy
There are medications that slow down the growth of hemangioma in the spine.
These are mainly glucocorticosteroids, which are taken in doses strictly calculated by the doctor and according to an individual regimen. Efficacy has been proven in 30–60% of patients, but hormonal drugs have a lot of contraindications and adverse reactions, so their need for the treatment of vertebral hemangioma is determined only by a specialist. Main medications: Prednisolone, Diprospan. Hormonal medications such as Vincristine and Cyclophosphamide have particularly severe side effects.
Today, the administration of Propranolol (Anaprilin) or Timolol is considered an effective and safe therapeutic method for suppressing the growth of spinal hemangiomas. But treatment is provided only in doses calculated according to the patient’s body weight, that is, strictly individually and always under the supervision of a cardiologist.
Percutaneous sclerotherapy (sclerotherapy)
The method is used to remove small tumors and is based on the injection of ethanol and other sclerosants into the vascular tumor. This leads to gluing of the walls of blood vessels in the hemangioma and gradual resorption of the formation.
Despite the effectiveness of this technique for treating vertebral body hemangioma, doctors rarely use this method due to possible complications. Sometimes, when it gets into the spine, the sclerosant destroys not only the tumor, but also the bone tissue of the vertebrae, leading to the appearance of foci of necrosis, which can lead to suppuration and a compression fracture.
Limitations for vertebral hemangioma
With a vascular neoplasm of the vertebra, regardless of its size and clinical course, some restrictions are necessary. If a hemangioma is diagnosed in the spine, you need to know the following contraindications:
- The spine should not be subjected to increased physical stress during sports training or work. Especially if the hemangioma is located in the thoracic spine.
- It is not recommended to overheat the tumor site - do not get carried away with going to the beach, solarium or sauna.
- For spinal hemangioma, massage and manual therapy are also prohibited.
- It is important not to gain excess weight, as this will increase the load on the musculoskeletal system.
Whether it is possible to do physiotherapeutic procedures (such as UHF and electrophoresis) for spinal hemangioma is decided only by the attending physician, based on their necessity and possible risk for the patient.
Before the invention of modern diagnostic methods, people lived to a ripe old age, not knowing that a vascular tumor had formed in the vertebra. And now, with its small size and non-aggressive course, hemangioma does not create problems and does not change the quality of life. You just need to periodically consult with your doctor, avoid heavy physical work and not gain excess body weight.
Risk factors and causes
To date, the causes of tumor development are not fully understood. However, scientists are inclined to believe that hemangioma develops due to genetic predisposition , and the prerequisites for its development are laid in the womb.
Studies designed to determine the causes of tumor formation have produced conflicting results.
It turned out that the risk of developing hemangioma increases in the presence of:
- weak vascular walls;
- excess estrogen in the blood (pathology occurs 5 times less often in men than in women);
- local tissue hypoxia.
Consequences
With an aggressive course, spinal hemangioma can cause the following complications:
- fractures of the spinal column (at the site of growth of a vascular tumor);
- paralysis of limbs;
- disturbances in the functioning of the pelvic organs.
Pathogenesis
It grows quite slowly. As it grows, destruction of the bone tissue of the vertebrae occurs, which leads to rupture of blood vessels. Vascular rupture occurs due to the formation of sharp bone edges that catch the vessel and tear it. When a vessel ruptures, the blood stops quite quickly, forming a blood clot, which in turn is destroyed after some time. After the blood clot is destroyed, the patency of the vessels is restored, but when the vessel is restored, osteoclasts manifest themselves.
Osteoclasts are bone cells that are destroyed when tumors grow. And in their place, vascular tissue is formed, which replaces osteoclasts. As a result, the spinal column is damaged and its strength decreases. As it grows, multiple hemorrhages occur in the spine, which cannot but affect the patient’s general well-being.
Symptoms and signs of the disease
The disease rarely makes itself felt, as it is often asymptomatic. This is due to the small size of the formation. The tumor can reach large sizes at the age of 50 and manifests itself depending on its location and size. The tumor manifests itself depending on its location and size. With a size of about 5 cm, hemangioma is difficult to detect even in the laboratory.
When a focal neoplasm reaches a size of more than 10 cm, the following symptoms may appear:
- Pain under the right hypochondrium;
- Discomfort in the stomach area;
- Enlarged liver;
- Nausea and vomiting;
- Feeling of heaviness in the stomach;
- Heartburn, increased gas production, belching, problems with stool;
- Hyperhidrosis at night (increased sweating);
- Yellowness of the mucous membranes;
- Fatigue, weakness;
- Temperature.
The tumor grows due to vascular dilations, thrombosis and hemorrhages. Its average weight is from 500 to 1500 g. The maximum size of such a tumor reaches 5 kg or more. At later stages of development, an atypical hemangioma occurs. It differs in structure in that the tangle of vessels acquires keratinized edges and scars. Having reached a certain size, the tumor can rupture and cause bleeding.
What to do if you identify symptoms of the disease? Which doctor should I contact? A feeling of heaviness under the right hypochondrium does not arise just like that. When it appears, immediate consultation with a gastroenterologist is necessary.
Pregnancy and hemangioma
If a hemangioma is present in the liver, a factor such as pregnancy can provoke its accelerated growth. As long as the tumor is small, it does not pose a threat to the patient’s life. But as soon as the tumor begins to actively grow, involving other tissues in this process, the benign nature of the tumor becomes conditional. There is a risk of hemangioma transforming into a cancerous tumor.
The growth of the tumor is accelerated due to the production of estrogen hormones in the pregnant woman’s body, which are necessary to increase the volume of the uterus and relax the pelvic muscles.
If the hemangioma has reached a size of more than 6 cm, there is a risk of rupture, which is life-threatening! Rupture of a liver hemangioma can lead to the death of the mother or fetus during pregnancy.
Hemangioma of the cervical spine
This type of tumor most often occurs without symptoms. This pathology can develop in people of all genders and ages, but most often women after forty are susceptible to this disease. Cervical hemangioma is less common than all other vascular inflammations.
Hemangioma of any part of the spine, including the cervical, is dangerous due to the potential for a pathological fracture.
Pathological fracture of the spine is a condition when, under the influence of a tumor, a vertebra breaks under the slightest load.
As long as the tumor does not grow and does not cause pain, it is not dangerous. Those tumors that grow, putting pressure on the tissues of the spine, must be examined dynamically and treated.
For pain associated with cervical hemangioma, any physical activity is contraindicated to avoid the risk of a pathological fracture of the spine.
Treatment options
Various therapeutic techniques are used to treat vertebral hemangioma. Methods for treating a tumor must be used by doctors very carefully to avoid injuries to the spinal canal. A neurosurgeon treats hemangioma located in the vertebra.
Therapy without surgery is possible only when the pathology occurs without symptoms. Doctors only observe small tumors using periodic MRI. Medications can only relieve pain and relieve inflammation.
Surgical intervention
Before the operation, the patient is fully examined, because surgery carries many risks.
Indications for surgical removal of a tumor are:
- Rapid growth of vascular formation.
- Hemangioma affects more than half of the vertebra.
- The occurrence of complications.
The disadvantages of the surgical method include the risk of bleeding and the return of the disease after some time.
Puncture vertebroplasty
This is a new method of therapy during which medical cement, titanium and barium sulfate are injected into the affected area. The latter acts as a radiopaque substance necessary to control the filling of the vertebra. The method reduces the tumor and stops its growth. The vertebra is stabilized and compacted, which reduces the risk of pathological fractures. Vertebroplasty is used for rapid growth of the tumor and can be an independent or additional method of therapy.
We recommend reading Ewing's Sarcoma - what kind of disease it is, survival rate, types
Embolization
This treatment method is considered minimally invasive. A synthetic embolic substance is injected into the main vessel feeding the neoplasm, which promotes blockage of the vessels. The formation stops developing and then gradually decreases in diameter.
Alcoholization
During therapy, ninety-six percent ethyl alcohol is injected into the formation. This method of therapy is not widespread, as it sometimes leads to complications. The patient's bone tissue may become necrotic, and there is a risk of compression fracture and compression of the spinal cord by fragments.
Radiation therapy
The diameter of the formation can be reduced and pain can be relieved using radiation exposure. This method of therapy is safer than surgery, but has contraindications. Radiation therapy is not used during pregnancy, to treat children, or when the tumor is large.
Folk remedies
Therapy using traditional medicine will not help get rid of hemangioma, but it can reduce the severity of pain and stop inflammation. Patients make lotions and compresses on the back from peony, wormwood, and St. John's wort.
The use of any folk remedies must be agreed with the attending physician.
How to behave
We hasten to console the reader - a huge number of patients live with spinal hemangioma all their lives, unaware of its existence. If the diagnosis is determined by chance, during an examination for another disease, there is absolutely no need to panic.
First of all, you need to visit a neurologist and tell him about the problem. The doctor will explain how the vascular formation is monitored and tell you when you will see your next appointment for a follow-up examination.
Important! Hemangiomas of the vertebral bodies are not prone to malignancy (degeneration into malignant tissue). Therefore, they extremely rarely pose a threat to life and health.
The asymptomatic process does not require treatment with medications; the only thing to avoid is injury. Although they should be avoided in case of any diseases or even without them.
"Kind" character and aggression
Bone tumors, of all locations, most often choose the spinal column. Hemangioma in this regard is not one of the exceptions. This benign formation especially “loves” the vertebral body, so it is often called a vertebral body hemangioma or, even more simply, a vertebral hemangioma, at the same time indicating which one (l1, l2, l3, l4, th12). The vertebrae listed in brackets are affected more often than others. In general, in terms of the “inception” of a tumor from parts of the spine, the thoracic (Th1 – Th12) segment is the most vulnerable (among all similar lesions it accounts for up to 80%), followed by a significant lag behind the lumbar (l1 – l5).
The cervical spine and sacrococcygeal segment are left with very little (about 1%) - hemangiomas do not “like” these places. Meanwhile, even within a tumor department, not all levels are given equal preference (not everyone is “loved” equally). A tumor of the thoracic region often “looks” for vertebrae from 3 to 12 (Th3 – Th12), losing “interest” in the cervical region. In the lumbar region, the tumor tends to settle on the first four lumbar vertebrae (l1, l2 l3, l4), usually ignoring the fifth (l5), as well as the sacrum and coccyx. In addition to localization, spinal hemangioma is characterized by the following features:
- The tumor has a “good” character, grows slowly, without degenerating into a malignant neoplasm, and usually proceeds without treatment, because in most cases no one knows about its presence. It should be noted here that a benign course is not characteristic of all spinal hemangiomas; among them there are quite aggressive forms, which will be discussed below;
- Women are more susceptible to this pathology than men;
- The favorite age for hemangioma in adults is the second or third decade of life; in childhood, the disease is diagnosed extremely rarely, but, in principle, cannot be completely excluded;
- Most often, the pathological process affects one vertebra, although there are known cases of multi-level tumor location (hemangiomatosis);
- Most of these vascular tumors proceed for years without any symptoms and are discovered by chance during the now fashionable studies, such as CT and MRI, for a completely different reason.
But if this tumor is so good and harmless, maybe it’s not worth paying attention to it at all, especially since there are only 1 to 10% of them in the human population? However, as time has shown, not all vascular formations in this category always remain “good” - 3-4% (according to other sources - from 10 to 15%) of them occur with symptoms that interfere with the patient’s quality of life. Hemangiomas become “bad” when they acquire dangerous sizes. Affecting the entire vertebral body, they behave aggressively towards their “neighbors” (they compress the spinal cord) and provoke compression fractures.
Consequences of the disease
When formations of this kind grow to a critical level, then you should be afraid of a compression fracture of the spine. After a fracture, there is a risk of experiencing numbness in the limbs. In addition, the patient is accompanied by constant, aching pain in the area of the fracture, which can radiate to other organs. After such a complication, it is difficult for a patient to raise his leg; the risk of paralysis is very high.
Liver hemangioma on MRI, ultrasound and computed tomography
In this case, consultation with a gastroenterologist without preliminary diagnosis is of little use, since in most cases hemangioma has no visible signs and can only be detected during various types of diagnostic measures. Examinations that allow you to see a hemangioma and determine its diameter are:
- ultrasonography. Liver hemangioma on ultrasound is often noticeable in the liver parenchyma in the form of a round formation with heterogeneous contents and clear contours;
- MSCT of the abdominal cavity;
- hepatoscintigraphy is a method that allows you to examine soft tissues for malignancy. A biopsy for this diagnosis is prohibited, since damage to the tumor can cause massive internal bleeding, since the tumor itself consists of blood vessels;
- MRI and CT scan of the liver and biliary tract. These studies allow us to see the tumor more accurately from different angles. Before these examinations, the patient must be injected into a vein with a special drug - contrast, since liver hemangioma on CT with contrast is outlined more clearly, and the chance of confusing it with another neoplasm is significantly reduced.
Doctors at the Yusupov Clinic are constantly improving their skills, which allows them to stay up to date with the latest methods for studying liver diseases. Our doctors are competent and attentive to drawing up a treatment plan for each patient, because only an individual approach to recovery gives the expected results.
Symptoms of liver hemangioma
The disease can manifest itself with the following symptoms:
- nausea;
- frequent aching pain under the ribs on the right side;
- constant bitter taste in the mouth;
- increase in liver size;
- jaundice;
- dyspeptic disorders;
- feeling of tightness in the stomach area.
In order to diagnose hemangioma, the following laboratory tests are necessary:
- Ultrasound;
- MRI;
- multislice CT.
Even with an asymptomatic course of the disease, mandatory confirmation of its benignity is required. For this purpose, the doctor prescribes a radioisotope study to help identify lesions in the liver, if any. This method allows you to determine the type of tumor, recognize a formation with a cyst, detect its location, etc.
If the formation was diagnosed in the right lobe of the liver, then additional antiography of the black trunk will be prescribed. This is necessary in order to assess blood flow and exclude the presence of blood clots in any of the phases (venous, capillary, arterial).
Diagnostics
When the disease is asymptomatic, liver hemangioma is discovered completely by accident, during examination of the patient for a completely different reason. If you complain about the appearance of one or more symptoms, it is necessary to perform instrumental studies. But before prescribing them, the specialist must familiarize himself with the life history of the patient and his closest relatives in order to identify possible hereditary factors in the formation of such a disease. After which, a survey and physical examination are required - this is necessary to identify the intensity of the symptoms.
Laboratory tests of blood and urine usually have no diagnostic value. Only a microscopic examination of stool can indicate the presence of hidden bleeding in the peritoneum.
The basis for diagnosing liver hemangioma are such instrumental techniques as:
- MRI and ultrasound of the liver - enable the specialist to identify round formations;
- computed tomography using a contrast agent to detect characteristic signs of bleeding;
- liver scintigraphy;
- angiography - performed to ensure that the detected tumor is a hemangioma. Used in cases where CT and MRI have failed.
During diagnosis, it is very important to differentiate such a disease from other benign liver tumors, oncology, cystic tumors, as well as from cancer metastases on nearby organs.
Let's take it apart piece by piece
Let's get acquainted with the “responsibility” of each segment of the spine for a specific organ or system. We do this so that you have a clear idea of what defects can arise from aggressive formations of a particular vertebra.
The cervical region is responsible for everything that is in the head. The last vertebra, C7, is related to the upper limbs. Let's take a closer look at the functionality of the thoracic spine, where the disease is localized in most cases, and the lumbar spine.
| Thoracic vertebrae | |
| Th 1 | Upper limbs, trachea, esophagus. |
| Th 2 | The same areas as Th 1, additionally the heart area. |
| Th 3 | Bronchi, pleura, lungs. |
| Th 4 | Gallbladder. |
| Th 5 | Solar plexus area, liver. |
| Th 6 | Stomach, liver, gall bladder. |
| Th 7 | duodenum, pancreas. |
| Th 8 | Spleen, diaphragm. |
| Th 9 | Adrenal glands. |
| Th 10 | Kidneys. |
| Th 11 | Kidneys, ureters. |
| Th 12 | Large, small intestine. In women, fallopian tubes. |
| Lumbar vertebrae | |
| L 1 | Abdomen, cecum, thighs. |
| L 2 | Intestines. |
| L 3 | Reproductive system, bladder, knees. |
| L 4 | Prostate gland, legs, feet. |
| L 5 | Ankles, feet. |