Intestinal polyps are small, benign growths that grow asymptomatically on the inner mucosa. This pathology is considered common. It affects 15 to 20% of people. It is asymptomatic.
On average, the size of polyps reaches 1 centimeter. In rare cases, they reach several centimeters. In the intestines, polyps grow both in groups and alone. They look like small cones and may have a thin or thick compacted stem in the shape of a bunch of grapes or a mushroom.
The polyps themselves are considered benign formations that rarely affect a person’s well-being. But they also transform into malignant tumors that are difficult to treat. If intestinal polyps are detected, they are recommended to be removed.
Types of polyps
There are three types of polyps:
- The first type, adenomatous, is considered the most common. This species can malignize and degenerate into cancerous tumors.
- The second type is serrated. Depending on the location and size, they have a different probability of malignancy. Large polyps, which are still flat (sessile), located in the upper part of the intestine, most often transform. But small formations that are located in the lower part of the colon, also called hyperplastic polyps, rarely turn into cancerous tumors.
- The third type is inflammatory. These polyps occur after inflammatory bowel diseases such as ulcerative colitis and Crohn's disease. Also prone to malignant degeneration.
As already mentioned, polyps are mainly discovered during a routine examination of the large intestine. This is due to the fact that the disease is asymptomatic or the symptoms are characteristic of many pathologies, such as hemorrhoids, inflammatory bowel diseases, and peptic ulcers. Large polyps can only be detected with MRI or CT. Both methods are convenient and painless, but they do not detect small tumors. Therefore, if polyps are suspected, doctors refer patients for examinations such as colonoscopy and flexible sigmoidoscopy.
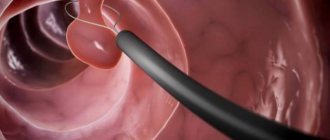
Colonoscopy is the most sensitive test that uses an endoscope to examine the inside of the intestines. The endoscope is inserted through the anus into the rectum, and the entire surface of the colon is displayed on a large screen to the doctor. In addition to the video camera, it is also equipped with micro-instruments. Therefore, tumors can be removed directly during diagnosis.
The doctor may also take a piece of intestine from a suspicious area for histological analysis. Flexible sigmoidoscopy is considered a shortened version of colonoscopy. Using a flexible tube with a video camera, only the rectum and partially the sigmoid colon are examined.
What is a skin polyp
Overweight people are most prone to developing polyps
A polyp is a benign tumor, but there is also a possibility of it developing into a malignant tumor. Typically, these neoplasms do not bother you at all and only cause aesthetic discomfort. The only thing you need to watch out for is accidental damage to it while shaving, wearing tight clothes or jewelry. A large polyp can burst under pressure, which can lead to minor bleeding.
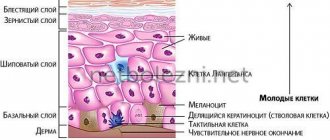
These neoplasms consist mainly of fibers, channels, fat and nerve cells and the epidermis. Those most susceptible to their occurrence are:
- overweight people;
- persons whose relatives have previously observed such neoplasms;
- pregnant women;
- patients with diabetes mellitus.
But it happens that the appearance of polyps occurs unreasonably. Women and older people are most susceptible to their formation, but they can also bother the male half.
Treatment of polyps in the intestines without surgery
Treatment of intestinal polyps without surgery is carried out through the use of tinctures, healing mixtures, microenemas and decoctions. The probability of success of home therapy is quite high in cases where the tumor is small in size and the presence of cancer cells is not detected in the polyps. Mandatory preliminary agreement with the proctologist, as well as systematic monitoring of the patient’s general condition, require events of this kind.
To reduce the risk of degeneration into a malignant tumor, any type of tumor should be removed immediately. Folk remedies are also used to treat polyps in the intestines. Alternative therapy reduces the risk of tumor regrowth, as opposed to surgical removal. However, such treatment requires long courses. The course of treatment should be prescribed by the attending proctologist.
Treatment of intestinal polyps without surgery will give positive results if neoplasms are diagnosed in a timely manner. You should resort to medication if the disease is in an advanced form. Adherence to a proper diet, as well as the use of traditional medicine, will help cure the proliferation of intestinal epithelium or reduce this process.
How to cure skin polyps
https://youtu.be/LPoCb-VFvGw
The most effective treatment method is their surgical removal. As a rule, surgery to excise a single tumor is easily tolerated by the patient and does not require a long rehabilitation period. The procedure can be performed endoscopically and using a laser. During laser exposure, nearby tissues are not damaged, and the wound surface is very small, which ensures rapid healing and tissue restoration. But surgery is not recommended for all patients - with good histology, doctors in some cases use drug treatment.
It is necessary to understand that effective and correct removal of polyps without any complications is possible only under the supervision of specialists who have extensive experience in treating this disease.
During the consultation, they will tell you how they are treated, how tumors are removed, and what restrictions must be followed immediately after surgery. Prepare a detailed list of questions you want to ask your doctor. Before the procedure, a mandatory and thorough diagnosis is carried out, and all existing diseases of the affected organs are treated.
After treatment, the patient must monitor the condition of his body - in no case miss scheduled examinations with a doctor, so that in case of relapse of the disease, polyps can be detected at an early stage.
Traditional methods
Traditional methods of treating polyps are:
- oils and ointments (iodine, honey, sea buckthorn, camphor oil);
- decoctions (pine needles, celandine, sage);
- tinctures (viburnum, celandine, walnuts);
- enemas and compresses from plant extracts, their leaves, fruits and stems.
As a rule, the therapeutic course is designed for a long time, so it will not cause harm to the human body. Before treatment, you need to make sure whether the patient has allergic reactions to certain plants. Treatment of intestinal polyps with folk remedies has a number of advantages. We include:
- environmentally friendly drugs;
- strengthening the immune system;
- subject to dosage, no side effects;
- simultaneous use of several drugs;
- 100% result, proven over centuries;
- during treatment, the body receives vitamins, minerals and other beneficial substances;
- there are no negative effects on internal organs and systems.
Contraindications to surgical treatment
- Pathologies,
- Temporary painful conditions
- Patient distress.
In some cases, surgery may be postponed for the following reasons:
- small polyps without signs of growth, strangulation, or malignancy;
- the presence of combined pathologies of internal organs or systems;
- burdened clinical history;
- pregnancy;
- exacerbation of hemorrhoids.
In some cases, a wait-and-see approach may be prescribed to assess the clinical behavior of the pathogenic tumor. Thus, in the absence of unpleasant symptoms, surgery can be performed only when a more favorable period occurs.
Note! The intervention is contraindicated if:
- exacerbations of inflammatory or infectious diseases;
- hemorrhoidal disease;
- serious internal bleeding.
Features of non-surgical treatment
Treatment of polyps involves a wait-and-see approach with assessment of the dynamics of development of tumor-like growths of the intestinal mucosa, as well as non-invasive treatment methods.
The main drugs are:
- Antibacterial drugs for the treatment of exacerbation of the inflammatory process;
- Antiseptic agents to eliminate pathogenic microflora;
- Hemostatic agents for rectal bleeding (local gels, suppositories and suppositories);
- Iron-containing preparations to increase hemoglobin levels in the blood;
- Vitamin complexes;
- Hormonal drugs for severe dysplasia of the intestinal mucosa.
Enemas with antiseptics, herbal infusions, and medicinal compounds are prescribed in case of low localization of polyps:
- rectal lumen,
- anal hole,
- lumen of the colon and rectum.
For distant localization of polypous lesions, systemic drugs for oral administration are used.
The most effective drugs against polyps are the following:
- Suppositories. Chistobolin with hemlock extract. The drug is absorbed into the circulatory system through the mucous membranes within a few minutes. The suppositories contain many herbal medicinal components that soften the mucous membranes of the rectal lumen, reduce tumors, disinfect and reduce painful syndrome.
- Phytocandles. Many patients noted high effectiveness against single polyps. Herbal components help prevent malignancy of tumor cells and reduce pain. Cocoa butter, thuja, celandine and orange maclura extracts in combination provide excellent therapeutic results. The alcohol extracts of calendula, celandine, plantain and wormwood included in the composition have anthelmintic, antiseptic, and antitumor effects.
- Gepasolone suppositories. A combined action product that contains the hormone prednisolone, heparin, and the anesthetic lidocaine. Suppositories are used in complex therapy for painful defecation, rectal polyps, complicated by hemorrhoidal disease. The duration of treatment is no more than 14 days.
- Relief candles. A well-known drug for the treatment of hemorrhoidal disease, but it effectively eliminates the symptoms of polyposis complications in the intestines. The drug contains shark liver extract, phenylephrine, an anesthetic. Ideal for reducing the symptoms of polyps that are formed from a hemorrhoid.
For bleeding polyps, you can use the following ointments:
- Heparin liniment - suitable for necrotic changes in mucous membranes;
- Hepatrombin - for active bleeding with swelling and inflammation of the intestinal mucosa;
- Heparoid Zentiva - reduction of the inflammatory process and the volume of tumors.
If there is a marked decrease in hemoglobin levels, the use of iron-containing drugs is recommended:
A course of vitamin therapy is required to increase local immunity, as well as enhance regenerative processes in the intestinal mucous membranes.
Important! Although drug therapy is effective for small, single polyps, it may be used as symptomatic therapy for painful multiple polyps.
Drug preparatory therapy is necessarily prescribed to reduce postoperative risks, as well as to speed up the recovery period.
Causes of polyps in the intestines
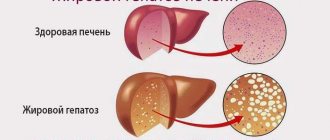
Polyps in the intestines are neoplasms of a benign type, but which are likely to become malignant. The outgrowths are located on the inner walls of the organ or in the lower part of the colon, in the rectum. They can stand on a leg or grow completely into space.
Polyps are soft to the touch, the surface is matte, but sometimes there is mucus. The color is different - varies from brown to pink with a yellow tint. The shape is most often round, but the outgrowths on the stalk are mushroom-shaped, and sometimes branched specimens are found.
Doctors have not yet established the exact reasons for the formation of growths. But this fact does not affect how polyps are treated. There are certain theories (they are based on experimental observations of patients' anamnesis). Among them are:
- Inflammatory processes in the intestines. As a result, epithelial tissues react more quickly, because they need to quickly replace damaged areas. This can trigger uncontrolled growth. Provoking factors include enteritis, dysentery, and colitis.
- Unfavorable environmental conditions. Scientists have proven that people who lack fresh oxygen and are forced to eat food with chemicals are more likely to observe polyps in the intestines.
- Vascular dysfunction. Atherosclerosis and varicose veins lead to the formation of polyps.
- Genetic predisposition. The intestines may inexplicably function differently. This also includes the theory of impaired embryonic development - the structure of the intestine with polyps is formed in the womb, but symptoms appear later, with accompanying factors.
- Gluten intolerance and other food allergies. Products containing gluten are recognized by the intestines as foreign agents, as a result of which the body begins to fight them, which causes damage to the mucous membrane. Repair requires work of the epithelium, which may form new tissue incorrectly.
Much less common, but leading to polyps in the intestines are diseases such as gastritis and gallstone pathology.
There are no specific symptoms that define this particular disease. But you can make an initial diagnosis at home, and then have it checked by a doctor if you experience the following symptoms:
- excretion of blood and mucus in feces;
- pain in the lower abdomen;
- constipation and diarrhea;
- nausea and belching;
- sensation of a foreign body in the anus;
- bleeding from the anus.
Forecast
The prognosis for skin polyps depends on the type of tumor and the treatment tactics used. For neoplastic growth, laser surgery or another progressive and effective method should be used in order to achieve a 100% recovery.
For other forms, in the first stages you can get by with conservative treatment or folk methods. There is a risk of complications only in advanced conditions.
The main factor in recovery is timely detection of the problem and immediate contact with a doctor, followed by the prescription of adequate therapy.
Diagnostics
A common diagnostic method is stool testing. A laboratory test determines whether even the smallest particles of blood are present. But it should be understood that a negative result is not considered an absolute guarantee that there are no polyps in the intestines. The fact is that blood may not be released in the initial stages of formation.
Modern methods such as CT and MRI allow specialists to notice abnormalities in the growth of the intestine and adjacent sections and determine the specifics of growths, if any. Other diagnostic methods are also common:
- irrigoscopy;
- finger diagnostics;
- colonoscopy.
At the stage when growths are discovered, it is important for doctors to determine their specificity. Similar types are fibroids, angioma, lipoma. For this purpose, histological techniques are used.
Diagnostic measures
Skin polyps are an area of research for oncologists, dermatologists and dermatovenerologists. Typically, diagnosing pathological proliferation of epithelial tissues is not difficult. A physical examination of the patient's skin, scraping of the skin in the affected area and histological analysis for atypical cells are sufficient.
Additionally, blood, urine, and stool samples must be taken to reliably assess the patient’s general clinical condition. The final diagnosis is made based on the totality of data from all studies performed.
Treatment of polyps
Polyps in the intestines and other parts of the gastrointestinal tract are mainly treated surgically. But if the disease is at an initial stage, or when it comes to its prevention, then medicinal methods and traditional medicine are effective.
Initially, it is worth noting that traditional medicine abandons the idea that polyps can be cured with medications. For any size of the polyp, surgery is prescribed.
The most popular method is endoscopic resection. The polyp is captured with a loop, and it is removed and removed using an electric current. But other surgical methods are also indicated:
- for polyps in the rectum - polypectomy;
- for large pedunculated polyps, villous polyps - opening of the intestinal lumen;
- for polyps located close to the anus - transrectal excision.
After any type of removal, the patient must follow a diet for several months.
Although drug treatment is not practiced by medicine, some patients still note its effectiveness. Doctors say that the tablets can be used before surgery or to relieve symptoms, but they cannot replace surgery. Antiflatulents and antispasmodics are used.
Treatment of rectal polyps with folk remedies is not recommended by doctors. But you can still find a lot of recipes and positive reviews on the Internet. Popular:
- Enemas with celandine for polyps. One teaspoon of celandine is brewed in liters of water, and the intestines are washed twice for 15 days. After a two-week break, enemas are done in the same way, but at a rate of 1 tablespoon per liter.
- Viburnum decoction with agrimony. Pour 2 tablespoons of viburnum and two tablespoons of grass with 300 ml of water. Leave for 4 hours, take a third of a glass before meals.
- Tampons with camphor oil. 4 tablespoons of oil are mixed with a spoon of honey. Soak a cotton swab in the mixture and insert it into the anus overnight. The course consists of 10-15 procedures.
Also tried are tinctures made from pumpkin seeds, egg yolks, sea buckthorn oil, golden mustache and others.
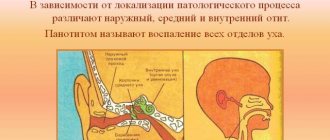
A detailed review of nasal drops for polyps
Today, in the treatment of polyps, it has been proven that only surgery is an effective remedy. It is carried out in a severe stage of pathology, when serious complications are noted. At the stage of formation of formations, the patient is prescribed medications that can reduce the size of growths and remove them completely. Medication assistance is especially important for those who are contraindicated for surgical intervention. Using drops for nasal polyps is a chance to alleviate your condition and even get rid of the formations forever.
A polyp is a tumor, growth, formation that grows on the mucous membranes. They appear in the nose due to frequent runny noses, allergies, and improper development of the nasal septum. This is a pathology, but at the same time it is a natural reaction to constant irritation of the mucosal area. The immune system acts for the purpose of protection, triggering mechanisms that lead to thickening of the membrane and an increase in its area. Over time, polyps grow and problems begin:
- The patient snores;
- Cannot breathe through one or both nostrils;
- Sinusitis and sinusitis appear due to the formation clogging the sinuses with infected contents;
- It happens that the growth blocks the entrance to the auditory tube, then hearing loss appears;
- The nasal receptors cannot function normally, which leads to loss of smell and partly taste;
- There is a risk of pus from the sinuses entering the brain, which causes sepsis or meningitis;
- Discomfort due to a constantly open mouth;
- Hypoxia of the central nervous system, as a result, inhibition of all body functions.
As a rule, in this condition the patient is prescribed surgery. But not everyone is allowed to do it. There are temporary prohibitions on removing formations:
- Pregnancy and lactation;
- Days of menstruation;
- Presence of infection;
- Allergy in acute form.
And also categorical contraindications to nasal surgery:
- Oncology;
- Pathologies of the heart, kidneys and liver with serious disorders, the so-called stage of decompensation;
- Reduced clotting. Such a patient can bleed even from an injection;
- Severe form of hypertension.
Above we talked about scientifically proven products with hormonal content. Only they are recognized by official medicine as an effective medicine. However, there are drops with natural ingredients that can help in the fight against nasal formations.
The drug in drop form contains green tea, Kalanchoe, propolis, thuja, juniper, wild rosemary, which are the main ingredients of many folk remedies. The action of the medicine is aimed at eliminating the root cause of formations - infection, congestion, irritation of the nasal mucosa. Initially, it is positioned as a remedy against frequent runny noses, sinusitis, and sinusitis. According to patient reviews, a regressive property in relation to polyps was noted. Much is known about cases of complete deliverance. The drug is prescribed as an adjuvant for hormonal treatment, as well as after removal of formations.
You can buy the finished drug at a pharmacy or make it yourself. The solution is alcoholic, so before use it should be diluted with water in half. It is acceptable to use as drops, 2 in each nostril.
There are many reviews about completely getting rid of polyps in the nasal cavity. The method was different. The drug was not dripped, but soaked into tampons and inserted into the nostrils for 10 minutes, 2-3 times a day. They say that a complete cure can be achieved within 1-2 months.
A very effective remedy for a runny nose, sinusitis, and the causes of polyps. Apply 2 drops morning and evening. Contraindicated for children and pregnant women. Helps reduce nasal formations.
The main effective cure for polyps in home treatment is celandine. For drops, you can use diluted plant juice. Or put tampons soaked in the drug. It should be diluted in half.
Attention! Such products can help with nasal therapy, however, the components they contain are not always tolerated by allergy sufferers.
Most often, topical corticosteroids are used in the medical treatment of polyps. Tablets are used in difficult cases, as they have serious side effects.
It's an aerosol spray, that's all. The drop form is not possible, as there is a risk of overdose. One injection provides an accurate single dose of the drug. Active substance – Mometasone furoate. A hormonal drug that is acceptable for use in children from 2 years of age. The main purpose is the treatment of allergic exacerbations and conditions. In addition, such drugs have anti-edematous and anti-inflammatory properties. Based on these actions, the drug is an effective remedy for getting rid of the initial stage of polypous rhinosinusitis, as well as for alleviating the condition of large choanal formations. In case of serious pathology, it is prescribed to pregnant women. The dosage and frequency of use should be agreed with your doctor.
Attention! Nasonex has a number of contraindications that must be taken into account when using it.
Nasal spray with an active hormonal substance – Fluticasone furoate. The effectiveness of Avamys and Nasonex for polyps inside the nose is the same, but the former has fewer contraindications. That is why the drug is more preferable for treating pregnant women. Application for a child is similar - from 2 years. Patients with liver pathologies will have to refuse this drug. The dosage is calculated by the number of injections, as with Nasonex. For an adult, 2 in each nostril, for a child - 1. It is important to use at the same time.
Or Budesonide is also a corticosteroid in aerosol form. The action and effectiveness against polyps is similar to previous drugs. However, it is worth noting that the spray is not used for young children; it is approved for the treatment of nasal pathology from 6 years of age. For the same reason, it is contraindicated for nursing women. However, use by pregnant women is acceptable under a certain risk ratio.
There are other drugs with corticosteroids, they contain the same active substances, but have different names: Nazarel, Beconase, Nazofan, Budenofalk, Flixonase and others. All of them are in spray form to regulate the exact dose. They have almost the same effectiveness against formations inside the nose, the difference is in contraindications and side effects. However, Nasonex and Avamis are leaders in use for this pathology, as the most optimal option.
If hormonal and natural drugs are intended to treat, then there are drops that allow the patient to cope with the manifestations of the pathology:
- Most often these are vasoconstrictors, for example, Nazivin, Naphthyzin, Rinonorm, Nazol. They are used to facilitate nasal breathing. With polyps, such an effect is actually observed due to the removal of tissue swelling. In addition, such events will facilitate the passage of accumulated mucus. You cannot use the drugs for a long time, as they are addictive.
- Another auxiliary remedy is antiseptic drops - Protargol, Collargol, which allow you to fight an existing infection and prevent its occurrence.
- Saline solutions for irrigating and rinsing the nose will be a good help. They also relieve swelling and have antiseptic properties, but unlike vasoconstrictor drops, they do not cause habit. These are Aquamaris, Quix, Physiomer. The drugs have no contraindications and are suitable for patients of any age, pregnant women and those with severe pathologies.
Treatment of polyps must be comprehensive, since the problem is a consequence of serious disorders. Therefore, drops alone will not be enough. Only a doctor will be able to select a combination of drugs and actions for a complete cure for the pathology. You should not refuse removal, which is carried out today using gentle and precise methods.
Disease prevention
There are no specific preventive measures. But based on the reasons, we can conclude that you should not abuse bad habits, eat right, regularly check with a doctor and treat diseases of the gastrointestinal tract in a timely manner.
About ten percent of Russians who have reached the age of forty have polyps in the intestines. Most of them are men - it occurs one and a half times more often than in women. With timely diagnosis (stool test), the disease is diagnosed. Therefore, it will be possible to cure him. On average, 90% of patients who promptly sought help have a positive outcome.
Doctors answer unequivocally that questions about how to get rid of polyps without surgery are meaningless. This definitely cannot be done. Moreover, treatment with tablets and herbs can lead to injury to the intestinal walls and the growth of polyps.
If you find an error, please select a piece of text and press Ctrl+Enter.
Where do skin polyps form?
Such neoplasms appear anywhere on the surface of the body and often form small groups. Most often localized where rubbing of the skin surface occurs:
- in the area of the eyelids;
- in the armpits;
- in the groin;
- on the back and neck;
- under the breasts of women.
The polyp is usually darker or the same as the skin, and the surface of the polyp is smooth or rough. The polyp is very similar to cauliflower. It is easily injured by clothing, razors or jewelry. Skin polyps can form in a person for the first time only in old age, when there is a gradual loss of immunity and the body is under the influence of infection. Their appearance in a young person can be observed as a result of stress, infectious diseases or long-term use of antibiotics, hormonal or other medications.