Species: Hominis, Genitalium and Pneumonica
Biologists have not yet agreed on whether they should be considered bacteria, viruses or fungi.
Having a cellular structure like a bacterium, mycoplasma, like a virus, does not have a cell membrane and is extremely small in size - 300 nm.
Unlike viruses, these pathogens are able to live outside cells . They settle on the epithelial layer of the respiratory or genitourinary organs and gradually penetrate into its thickness. Microorganisms reproduce by budding.
There are many varieties of mycoplasmas in nature. Only 3 of them are dangerous to humans.
Mycoplasma species hominis, genitalium settle in the urinary system of a woman and cause her damage. And the species mycoplasma pneumonia causes diseases of the respiratory system.
Normally, mycoplasmas can live in small quantities in a completely healthy body without causing pathologies.
But once a woman’s immune system weakens, any adverse effects can cause the activation of microorganisms.
While biologists are dealing with classification problems, doctors have found ways to combat this pathogen .
How to treat colds during pregnancy safely for the unborn baby? Read our article. Do you think it is possible to treat uterine prolapse without surgery? Find the answer to your question in this publication.
Read about how medical abortion works here on the website.
How is mycoplasmosis transmitted?
The main route of transmission is sexual contact with an infected person. Moreover, the risk of developing mycoplasmosis is equally high during both genital and anal or oral sex. The only way to prevent infection is to use a mechanical method of protection. Mycoplasmosis is often characterized as a sluggish disease, and symptoms may not appear immediately, but only a few months after the bacteria enters a healthy body. The danger of mycoplasmosis lies in the fact that due to the absence of signs indicating the disease, most infected people do not even suspect that they are carriers of the infection.
Also, transmission of mycoplasmas occurs at the birth of a child, when he passes through the genital tract of a mother infected with a dangerous bacterium. Since the habitat of microorganisms is the secretions of the genital organs and mucous membranes, due to the large accumulation of mycoplasmas in this area, the risk of the fetus getting an infection is quite high.
Doctors do not rule out infection with mycoplasmosis through household items, however, it cannot be said with one hundred percent certainty that the bacterium can enter the body this way.
Routes of infection
Mycoplasmas cannot live outside the host organism. They do not live long in the environment. This determines the route of infection.
Ordinary household contact will not lead to infection with hominis, genitalium. Handshakes, kisses, shared towels, and dishes will not be a source of infection. Living in the same house with a patient with such mycoplasmosis is not dangerous.
In order for microorganisms to enter a new host body alive, sexual contact must occur.
Therefore, mycoplasmosis can be classified as a group of STDs (sexually transmitted diseases). The presence of gonorrhea or trichomonas will aggravate the course of the disease.
In this case, the carrier of the disease may himself remain just a carrier. If he has a strong immune system, then mycoplasmas will be present in his body in small quantities. This type of mycoplasma is transmitted by the mother to the embryo .
Mycoplasma pneumonia is transmitted by airborne droplets. Therefore, it is possible to become infected with it at home or on the street.
The incubation period of mycoplasma infection lasts quite a long time - 3-5 weeks, although sometimes mycoplasmosis in women can appear after two weeks.
Therefore, due to such a long latent period, identifying the source of infection becomes difficult.
Respiratory mycoplasmosis - infection, symptoms, diagnosis, consequences and treatment:
The main causes of the disease in women
People are infected with this disease mainly through sexual contact. The pathogen can also be transmitted to the newborn during childbirth. Moreover, if this type of infection occurs, boys get sick much less often, since the genitourinary system is anatomically different in men and women.
The disease is also transmitted through personal contact, but this is 5 percent out of 100. In newborns, like in men, there are cases of self-healing. However, this is observed more often in infants.
Causes
So, the disease is caused by mycoplasmas. However, not all carriers of them get sick.
In order for carriage to develop into mycoplasmosis, conditions favorable for the proliferation of mycoplasmas must appear in the body. The first is the weakening of protective forces.
This can lead to:
- stress – long-term or acute;
- chronic infections, diseases;
- physical and emotional overload;
- hypothermia;
- climate change, especially abrupt;
- taking antibiotics, hormonal agents such as glucocorticosteroids;
- pregnancy.
Method of infection
Mycoplasma spreads from person to person. There are 3 ways mycoplasmas enter the human body:
- Sexual. The most common method of transmission is sexual intercourse without using a condom.
- From mother to baby. In the process of giving birth to a child. Intrauterine infection of the fetus is possible.
- Domestic. This path is theoretically possible, but in practice it is a very rare occurrence, because mycoplasmas quickly die in the external environment. Using one washcloth, towel, etc.
Signs
For respiratory mycoplasmosis, the incubation period lasts 7-14 days. This form flows more brightly.
With it, patients complain of:
- increased body temperature;
- severe coughing attacks;
- pain and redness in the throat;
- nasal discharge.
The sick person experiences all the signs of intoxication of the body - weakness, fatigue, nausea, chills, fever.
The further you go, the more severe the cough becomes, until purulent sputum appears. But more often the disease affects the upper respiratory tract and proceeds like a mild acute respiratory infection .
The danger of respiratory mycoplasmosis is that it can lead to pneumonia. In this case, classical treatment will not have an effect, which should alert the attending physician and suspect the presence of mycoplasmas.
This complication develops if pathogens affect the lower respiratory tract.
Such pneumonia can lead to bronchiectasis (dilatation of the bronchi) and pneumosclerosis. Urogenital mycoplasmosis has a longer incubation period - from 2 weeks to 3-5 months.
10-40% of sick women do not feel any symptoms at all, and the presence of mycoplasmas is discovered by chance during an STD examination. For others, the manifestations of the disease are quite general.
Because of this, it can be confused with cystitis and other genitourinary infections.
How does mycoplasmosis manifest itself in women in the genital area, what are the symptoms of mycoplasma infection?
The beginning is characterized by:
- discomfort, pain in the lower abdomen;
- itching sensation;
- burning when urinating;
- discharge of a transparent, yellowish or grayish color;
- redness of the mucous membrane in the area of the urethral opening;
- lower back pain.
Pain and discomfort may occur during sexual intercourse. But at first all these symptoms are either ignored or considered the beginning of cystitis.
The acute form tends to become chronic when improvement occurs and the symptoms disappear before new provoking conditions arise.
Any hypothermia, stress, or hormonal fluctuations lead to the activation of mycoplasmas. Often a woman believes that she has again experienced an exacerbation of cystitis, and does not attach any importance to this.
Symptoms depend on where the protozoa are based.
If they affect the external genitalia, then itching, burning, and discharge come to the fore. Or the disease is generally asymptomatic.
If the infection has spread to the internal organs , then the woman will feel pain in the lower back in the abdomen, and the discharge will become more abundant and even purulent.
Burning and itching during urination will be more pronounced. Most often, damage to external organs occurs.
Mycoplasmosis symptoms may resemble pyelonephritis, vaginosis, inflammatory diseases of the uterus and fallopian tubes.
These pathogens can occur in combination with other types of chlamydia and ureaplasma. Manifestations of the disease can be varied.
If the disease affects internal organs, it can lead to the development of adnexitis and salpingitis (inflammatory process in the appendages).
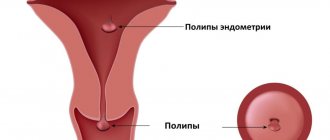
If mycoplasmas enter the uterus , this can trigger the development of endometritis. This variation of endometritis is characterized by cycle disorders and bleeding.
Adnexitis caused by mycoplasmas can result in a severe inflammatory process in the ovaries with an abscess and adhesion of the organ to the fallopian tubes.
Then the woman complains of severe pain in the lower back, cycle disruptions, and painful sensations during sexual intercourse.
Acute and chronic mycoplasmosis in women - symptoms, treatment and prevention:
Diagnostic methods
Effective research methods:
- PCR. Polymerase chain reaction allows you to identify the pathogen in vaginal discharge by identifying a specific DNA structure. It is considered the most reliable method of research compared to others.
- Flora smear. It makes it possible to suspect the presence of a pathogen, but not to confirm its presence. At the same time, the level of leukocytes increases, which indicates an inflammatory process.
- Bacteriological culture. Allows you to identify the pathogen after sowing the material into a nutrient medium. Once the pathogen grows, the doctor identifies it from others.
An additional research method is ultrasound. Ultrasound diagnostics allows you to determine the degree of organ damage when mycoplasma is activated. In this case, thickening of the walls of the bladder can be detected, inflammation of the uterus and ovaries is diagnosed.
Danger of infection
Discomfort is not the most dangerous consequence of mycoplasma proliferation.
Mycoplasmosis is dangerous not in itself, but because of the consequences that it can cause.
Long-term infection with Mycoplasma hominis in women leads to the development of:
- chronic pyelonephritis;
- urethritis;
- endometritis;
- cystitis;
- vaginitis;
- salpingitis.
Recent studies have shown that people suffering from arthritis are often affected by mycoplasmas, which provoke inflammatory joint diseases.
In severe cases, if the body's defenses are completely depleted, sepsis may develop.
Mycoplasmosis is especially . It can cause fetal development pathologies or pregnancy complications, including miscarriage. Subsequently, secondary infertility may develop.
The main causes and signs of intestinal obstruction are discussed in this material. How to treat uterine fibroids at home? Read our publication!
You can find out how to reduce toxicosis during pregnancy here.
What it is
Mycoplasma is a pathogenic microorganism, the type of which scientists today cannot determine. The absence of a cell membrane makes them similar to viruses, but the properties of bacteria can be noted.
There are many varieties of mycoplasma, but only a few of them are potential pathogens:
- Mycoplasma hominis;
- Mycoplasma genitalium;
- Mycoplasma Pneumoniae and others.
Mycoplasma hominis is found in the flora of healthy people and does not lead to disease.
Mycoplasma genitalium is a pathogenic microorganism. Its presence indicates the development of infection in humans.
Mycoplasmosis in pregnant women
Pregnancy is always an additional burden on all body systems. His defenses are reduced at this time. This can serve as a trigger for the disease if the woman was a carrier of the protozoa.
Developing infection with mycoplasma in women during pregnancy in the first – second trimester is fraught with miscarriages and “frozen pregnancy”, when the embryo stops developing.
In later stages, the risk of premature birth increases . It gets worse if the infection spreads to the amniotic sac, as the water may break prematurely.
During childbirth, the mother infects the child. This is fraught with the development of meningitis.
In the early postpartum period, mycoplasmas can provoke pneumonia or acute endometritis. It manifests itself as a severe postpartum infection.
Therefore, when mycoplasmas are detected, treatment is required. However, it is not recommended to be carried out in the first trimester, since the drugs can negatively affect the development of the fetus and lead to pathologies of its internal organs and systems.
Mycoplasmosis in women during pregnancy:
Symptoms of mycoplasmosis
It is very important to take into account the fact that the main symptoms that can occur with genitourinary infections will immediately make themselves felt if your body is attacked by any stress, overexertion or other diseases. What could be the consequences of such a process?
1. Symptoms of mycoplasmosis in men manifest themselves in the form of nagging pain in the groin area, mild pain and burning during urination, and small clear discharge from the urethra in the morning. In case of infection with mycoplasma of the prostate gland, the symptoms will behave exactly as with prostatitis. Problems with the epididymis manifest themselves in the form of nagging pain in the groin, perineum and scrotum. Under no circumstances should such a process be started; the appendage will significantly increase in size and the skin of the scrotum will turn red. There is also a danger that mycoplasmosis will negatively affect sperm production.
2. Those women who have not recovered from this disease experience symptoms very similar to those that are often transmitted sexually. For example, itching and burning during urination, clear vaginal discharge, pain during intimacy, etc. Mycoplasmosis during pregnancy is extremely dangerous. The consequences can be the most unpredictable: miscarriage, premature birth, early discharge of amniotic fluid. In addition, in the period after childbirth there is a risk of fever, which can cause harm to the newborn baby. Pneumonia or meningitis is guaranteed for him.
3. It is simply impossible to accurately diagnose urogenital mycoplasmosis. And all because such a disease has almost no symptoms, characteristic only of mycoplasmosis. This fact makes it difficult to diagnose all its differences from other difficulties with the genitourinary area.
It is important to remember that all of the above symptoms can be noticed in any inflammatory process of the human genitourinary system. The likelihood of their manifestation is no earlier than 3-5 weeks after infection.
Diagnostics
Diagnosis is difficult due to the extremely small size of mycoplasmas. To accurately identify the pathogen, DNA diagnostics is performed. Its accuracy is 95%.
If there is purulent discharge, then
a culture is done .
Its accuracy is one hundred percent, but the result will have to wait a week. Less informative tests for mycoplasma in women are ELISA and PIF (detection of enzyme-linked immunosorbent antibodies in the blood). But their advantage is speed and low price.
In this case, false positive and false negative results are often obtained; the analysis must be repeated a month after treatment.
To perform the research, a smear is taken for mycoplasma from women in the urethra and vagina, from the cervix. It is necessary to do a urine test, for which a morning portion is taken.
Differential diagnosis of mycoplasmosis: smear, blood, culture, PCR, cultural methods:
Mycoplasma Hominis in women - what is it?
The causative agent of mycoplasmosis, Mycoplasma hominis, is considered a gram-negative and opportunistic microorganism that has microscopic dimensions, which allows it to easily penetrate the human body. A feature of the pathogen is the absence of a structured wall, but it does not miss the opportunity to change and adapt to the conditions in which it finds itself. It is these properties that cause Mycoplasma hominis to be resistant to a large list of antibiotics.
The largest number of cases of the disease are diagnosed in representatives of the weaker half of humanity, although men and children can also suffer from it. As for men, they are most often affected by mycoplasma genitalium.
A feature of the course of the pathological process in women is that the clinical picture can be asymptomatic or have an erased form, it all depends on the level of the body’s resistance. With a normal immune response, an acute inflammatory process will not form; Mycoplasma hominis will be detected in the body only through laboratory tests.
Quite often there are cases when a person is a carrier of the disease, that is, the test results will show a low titer of the pathogen. This pathological condition is explained by the fact that the person will not be bothered by any symptoms of the disease, but it can be dangerous (in terms of infection) for his sexual partners.
Note! Despite its conditional pathogenicity, mycoplasma hominis should not be present in women’s bodies, because there are a considerable number of factors, the influence of which can lead to its activation and the development of the disease.
Treatment regimen
How to cure mycoplasma in women? Therapy must be comprehensive . It includes:
- local treatment;
- taking antibacterial drugs;
- diet;
- physical therapy;
- taking immunomodulatory drugs.
It is possible to choose an effective treatment. It is prescribed only based on test results, since different types of pathogens are destroyed by different groups of antibiotics.
Taking medications - immunomodulators and antibiotics
To enhance the effect of the drugs, immunomodulators Cycloferon or Lykopid are prescribed , which strengthen the body's defenses. Itching, burning, and discomfort are well relieved by local medications - suppositories and ointments.
It is important to realize that the treatment will be long. If you stop it at the first signs of improvement, then very soon the mycoplasmas will multiply again, and a relapse will occur.
During therapy , you need to drink a lot of water to remove toxins from the body that are formed during the destruction of mycoplasmas.
Since these microorganisms are often found together with others, complex therapy may be prescribed.
The first choice drugs are considered to be tetracycline antibiotics, macrolides, lincosamides and fluoroquinols - Tetracycline, Ofloxacin, Ciprofloxacin, Doxycycline . Erythromycin and Sumamed give a good effect .
Antibiotic therapy usually lasts 10 days, depending on the severity and symptoms of the disease. At the same time, anti-inflammatory and antipruritic vaginal suppositories are prescribed for 5-7 days.
To treat the vagina and destroy mycoplasmas, tampons with Chymotrypsin or Trypsin .
After two weeks, a repeat analysis is done. Based on its data, the doctor decides whether it is necessary to continue treatment and whether there is a need to change the drug.
Taking antibacterial drugs should be combined with the use of probiotics such as Acipol to prevent the destruction of intestinal microflora.
Sexual intercourse and partner treatment
Both partners need to be treated for mycoplasmosis at once. Otherwise, it is completely pointless due to constant re-infection. It is better to avoid sexual intercourse during treatment.
How to treat with folk remedies
You shouldn’t even look for traditional methods of treatment. There are no herbs that can destroy mycoplasma. The only way traditional medicine can help is to strengthen the immune system.
Immunomodulatory herbal decoctions can be used in complex therapy. After treatment, they will help prevent weakening of the body and re-infection.
Treatment of acute and chronic mycoplasmosis:
Treatment of mycoplasmosis
What is the essence of treatment for mycoplasmosis? First of all, the complete condition of the patient’s genitourinary system is assessed. If signs of inflammation are not detected and there are no complaints, then mycoplasmosis cannot be treated at all. Treatment of mycoplasmosis in women who want to become pregnant is urgently needed. It is impossible to say for sure that such a disease will have serious consequences, but it is also a mistake to neglect this problem.
It is very important to undergo a complete examination to treat the disease.
Tablets and medications are suitable for antibacterial therapy; it is worth taking a course of antibiotics. In most cases, erythromycin, doxycycline, tetracycline, and ciprofloxacin are excellent. An experienced doctor can prescribe other medications from the erythromycin group. For example, azithromycin and clarithromycin have fewer side effects on the digestive system, so they are prescribed in the treatment of mycoplasmosis in children.
There are two treatment options: 1. A comprehensive course that lasts one or two weeks. Especially popular for various complications of the disease and chronic process. For example, inflammation of the testicles and prostatitis. Combination therapy consists of a course of antibiotics and enzymes, vitamin therapy, immunomodulators and other local procedures. To prevent any side effects, additional medications are prescribed.
2. Taking a course of a single dose of antibiotics. This is not only a new, but also a fairly safe option. Must be assigned on an individual basis only. Antibacterial treatment is also possible. Serological diagnostics are at your service. With its help, the degree of activity of mycoplasmas and the dynamics of their development are accurately determined. In this case, two groups are useful - doxycyclines and fluoroquinolones.
Don't forget that your treatment will be more effective if your immune system is active enough. Having gotten rid of the causative agents of mycoplasmosis, it is worth undergoing a diagnosis of cure. What is prevention? If such a problem is detected, then there is an urgent need to undergo examination and strictly follow the prescribed course of treatment. Remember that re-infection is possible, since the body does not develop resistance to mycoplasmas.
Prevention
Since mycoplasmosis is a sexually transmitted disease, the method of prevention here is standard - the exclusion of casual sexual partners, the use of barrier means - condoms.
In case of casual sexual contact, douching with Chlorhexidine can be recommended. However, this does not provide a 100% guarantee that infection will not occur.
If you suspect an infection, you should consult a doctor who will prescribe medications for preventive treatment.
This must be done no later than a few days after unplanned casual sex.
Factors contributing to infection
The main reasons for the spread of infection are as follows:
- promiscuous sex life;
- refusal of barrier methods of contraception;
- weak immunity;
- lack of stress resistance.
Mycoplasmosis is not a sexually transmitted disease. A high concentration of mycoplasmas can be observed in the female body even in the absence of sexual intercourse. Mycoplasmosis occurs in most cases hidden.