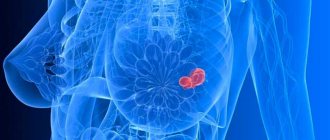
Breast cancer is the scourge of our time. Unfortunately, modern medicine is not able to prevent the occurrence of malignant cells, but timely diagnosis reveals pathogenic processes in the body at the initial stages, when proper treatment can give positive results up to complete elimination of the tumor.
Mammography and ultrasound are the most common methods for examining the condition of the mammary glands. Having an annual mammogram for women once they reach the age of forty is the gold standard for early cancer detection. According to official statistics, regular examination of the mammary glands in patients under 50 years of age has led to a reduction in mortality from cancer by 35%.
Depending on the method of implementation, film, electrical impedance and digital mammography are distinguished. This highly informative non-invasive technique is used for preventive analysis of the condition of breast tissue and monitoring the effectiveness of prescribed treatment.
What is mammography and why is it needed?
Mammography is a medical diagnostic method designed to examine the mammary glands. It is based on the property of soft and hard tissues of the human body to transmit X-rays differently.
Thus, when carrying out film mammography, the rays easily penetrate through soft tissues, the film is exposed, and such areas appear light. Solid substances block rays and therefore appear in dark colors in the photo. Specialists evaluate the resulting images to determine whether these shades correspond or not to the norm and draw conclusions about the absence or presence of pathologies.
A digital mammograph works on a similar principle. The difference is that the result of the conversion of X-rays does not end up on film, but on a special electronic matrix, which transmits the received data to a computer screen.
Mammography is the main form of preventive breast examination in women over 40 years of age. It is recommended to undergo it once every 1-2 years. Breast X-ray allows you to:
- identify neoplasms, including malignant ones, long before the appearance of external symptoms;
- study the localization, shape and size of tumors, cysts, calcifications;
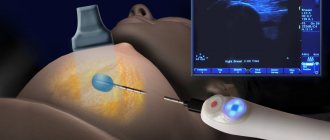
- carry out additional examinations, for example, puncture biopsy;
- evaluate the effectiveness of the completed course of treatment.
What can I diagnose with mammography?
This procedure is considered informative for identifying various neoplasms. What exactly does it show? Quite visible during this examination:
- fibrocystic disease or mastopathy;
- formed calcifications;
- hyperplasia of ducts with fibrous ones.
With its help, doctors recognize cancer. This method is one of the leading ways to identify pathology in its early stages.
If mammography shows the presence of a neoplasm, conduct additional examination. There is a possibility of a false positive result. When the diagnosis is correct, do not panic, start treatment immediately. If you have good results, do not forget to repeat the procedure on time. Since there is a risk of false negative results.
Types of mammography
The following types of mammography are used today.
- Film mammography of the mammary glands. It is based on x-rays that pass through the body's tissues and are displayed on film. The technique is considered obsolete due to increased radiation exposure, less information content and the highest percentage of error compared to newer technologies.
- Digital mammography. The results of the passage of the rays are reflected on the matrix, the image analysis of which is carried out using special software. This diagnostic method produces clear, high-resolution images; it is safer, since the outgoing radiation dose is three times less than when using film.
- Digital mammography with tomosynthesis. This research method is somewhat similar to computed tomography. Unlike conventional digital mammography, it produces not one two-dimensional image of the organ being studied, but several planar sections converted into a 3D projection. This method is the most visual and, at the same time, the most expensive, so its use as a screening examination is considered inappropriate.
- Electrical impedance mammography. This inexpensive and safe study has no contraindications and can be performed on any day of the menstrual cycle. Its essence lies in the effect of weak alternating currents on the studied area for the purpose of subsequent analysis of tissue resistance to electrical impulses.
We should also talk about such a subspecies as contrast mammography. It is prescribed when pathological discharge from the ducts of the mammary glands appears. During the diagnostic process, a special substance is injected into the ducts to increase image clarity. The method is effective for detecting intraductal formations.
At what age do X-rays take place?
As a screening test for the initial detection of pathology, mammography is prescribed after 35 years. At a younger age, due to high hormonal activity, the mammary glands have a high density, which makes it difficult for the rays to pass through and detect changes. Therefore, young women undergoing a medical examination are prescribed an ultrasound of the mammary glands.
At the age of 35-50 years, preventive mammography is mandatory at least once every 2 years, and after 50 years - annually.
Radiation examination in young women - mammography, computed tomography can be performed for diagnostic purposes in case of detection of pathology in the breast, in combination with other methods.
Indications and contraindications
Mammography of breast tissue can determine the development of benign or malignant tumors even before the appearance of specific symptoms. It is used to obtain histological material during a puncture biopsy as part of a corresponding study.
The need for a preventive examination of patients over 40 years of age and those at risk are the main indications for prescribing mammography. It is recommended for:
- fibroadenoma and other benign neoplasms;
- mastopathy;
- mastitis;
- some diseases of the reproductive system;
- endocrine disorders;
- infertility;
- overweight;
- previous operations on the mammary glands.
Mammography is prescribed if there are indications based on complaints of:
- pain in the mammary gland, swelling, change in shape and size;
- compactions in tissues;
- depressions, bulging, redness;
- change in areolas, nipple discharge.
Absolute contraindications, even if a digital mammograph is used, are pregnancy and lactation. Relative contraindication – age under 35 years. this is due to the physiological characteristics of the body. Young women have denser breast tissue, so the information value of the procedure is very low.
Indications for mammography examination
An annual mammogram helps detect breast cancer at an early stage. A referral for examination is issued by an endocrinologist, surgeon, mammologist or gynecologist. Who should undergo mammography of the mammary glands and under what conditions:
- women over 40 years of age with early menopause;
- when diagnosing benign tumors in the breast (fibroadenoma, mastopathy);
- with deformation of the nipples or the shape of the mammary glands;
- with chest pain;
- if there are seals in the nipples or the shape and color of the nipple circles are changed;
- in case of chronic endocrine or gynecological diseases;
- with a genetic predisposition to benign and malignant tumors;
- for the prevention of disease after cancer therapy.
How often should you have a breast screening?
For preventive examinations, older women (after 40–45 years) are recommended to have a mammogram every three years. Patients with dense breasts (little fat, a lot of fibrous tissue) are at risk of developing cancer. For this reason, they are recommended to undergo the procedure once a year.
If a benign tumor is detected during the examination, a repeat procedure becomes necessary. It is prescribed after 3, 4 or 6 months to assess changes in the structure and size of the tumor. To diagnose an already detected malignant tumor, photographs must be taken once a month. This will help the doctor track the dynamics of the development of the tumor and the success of the prescribed treatment.
Articles on the topic
- Breast tumor - signs of malignant and benign
- Pain before menstruation - why it appears, diagnosis, treatment and prevention
- Breast fibroadenoma - treatment with minimally invasive and non-invasive methods, consequences
How to prepare for a mammogram
The procedure is performed on an outpatient basis, its algorithm is quite simple, and no special preparation for mammography is required. It is enough to follow the following rules.
- Tell your healthcare provider the start date of your last menstrual period.
- On the day of the procedure, do not use antiperspirants for the armpit area or skin care cosmetics for the breasts.
- Remove jewelry and metal objects.
- Strip to the waist.
- Warn your doctor about possible or confirmed pregnancy or breastfeeding.
Before performing medical procedures, the doctor must inform the patient about how mammography is performed and what the possible consequences are.
Decoding the results
What pathologies can mammography of the mammary glands reveal?
- Cysts. This is a benign formation with liquid filling. They can occur at any age, but women during menopause are especially susceptible. As a rule, this is due to a drop in hormone levels. In this case, no treatment is required, only medical supervision. If a cyst in the mammary gland increases in size or multiple cysts form, a mini-surgery is prescribed to remove them. Sometimes a doctor prescribes hormonal medications to balance hormonal levels.
- Fibroadenoma. This formation is also benign. With it, a noticeable proliferation of connective tissue is detected in the mammary gland. Treatment is not prescribed if the fibroadenoma is less than 1 cm in diameter. If the size increases during observation, it is removed surgically.
- Fibrocystic mastopathy in most cases is treated with absorbable drugs. It occurs in the vast majority of cases, also due to hormonal imbalance. If therapy with absorbable drugs does not help, surgical intervention is prescribed for mastopathy.
- Calcifications. Deposits of calcium salts in breast tissue. In most cases, the process is asymptomatic. Sometimes their presence indicates that a cancer pathology has begun to develop. Additional examination is always required. Large calcium deposits rarely indicate cancer.
- Malignant tumor. Further examination and therapy are prescribed.
After the examination, the specialist gives an assessment and interpretation of the results.
- It may indicate the impossibility of determining the pathology without additional analysis. This happens if the images show formations that are blurred or difficult to read. This is a zero rating.
- The first assessment indicates that the patient is in complete health, but in the conclusion it is written that it is normal. Sometimes - with age-related changes.
- The second assessment provides a confident diagnosis of the presence of benign neoplasms. No symptoms of oncology were identified.
- The third assessment identifies doubtful cases that require additional examination and observation of the woman by an oncologist.
- The fourth assessment determines the urgent need for a biopsy to exclude cancer processes.
- The fifth assessment indicates the need for a biopsy due to the high likelihood of developing malignant processes.
- The sixth evaluation diagnoses breast cancer. Further mammography is needed only to monitor the progression of the disease.
The results of mammography are assessed by a radiologist. The conclusion is issued on the same day. The research protocol describes the types of tissues that make up the mammary gland (fibrous, glandular, fatty), their relationship with each other, homogeneity or heterogeneity of the structure.
The shape of the organ is analyzed: round, oval, lobed or irregular. The size of the ducts is indicated (normally up to 0.4 cm in women of childbearing age, up to 0.2 in menopause), whether they are straight or convoluted, contain homogeneous or inhomogeneous contents, in which area they are better developed.
The age of the patient must be taken into account. In women over 40 years of age, involution processes begin (the glandular component is gradually replaced by fibro-fatty component). Mammography for fibrocystic mastopathy shows that during this period the glandular component predominates.
If during this period the glandular component predominates according to mammography, then fibrocystic mastopathy is diagnosed.
Dilated ducts and cysts are also clearly visible on x-rays. The doctor describes in detail their location (using a watch dial for convenience), diameter, contours, and internal contents. Types of cysts are presented as simple and complicated (festering).
The space-occupying lesion stands out quite well on the mammogram, as it is accompanied by a darkening symptom on the X-ray film. Its presence is confirmed in two projections. If visualization occurs in only one projection, then they speak of a focus of compaction in the mammary gland.
Tumors are described qualitatively by analogy with cysts, only the contours (even, uneven, presence of a capsule), density (low, mixed, high, asymmetrical), the presence and main characteristics of calcifications are analyzed in more detail.
Dilated ducts and cysts are also clearly visible on x-rays.
It is now customary to assess the condition of the mammary organs according to the international system for describing and processing data BI-RADS (Breast Imaging Reporting and Data System), which is used in most countries.
The resulting changes are expressed as points. This algorithm accurately indicates to the attending physician further tactics for managing the patient and the necessary therapeutic measures. BI-RADS creates continuity between all treatment and diagnostic links that a woman goes through.
The scale includes 7 categories: 0 and 3 – cases subject to auxiliary research, re-monitoring after six months, 1 and 2 – sent to the treating gynecologist, 4 and higher – consultation with an oncologist, fine-needle biopsy is recommended.
The quality of the examination also depends on the experience and training of the specialist. In addition, there is a small percentage of false-positive diagnoses, which once again confirms the need for an integrated approach to the examination.
How to do a mammogram correctly
Mammography is done according to a standard scheme, usually consisting of the following stages.
- The patient is escorted to a specially equipped room.
- Depending on the parameters of the mammograph and the purpose of the study, the woman takes a lying or sitting position.
- In order to protect the genitals, the abdomen is shielded, that is, covered with a lead apron.
- The mammary gland is located on a horizontal plate, under which there is an X-ray emitter. It is fixed at the top by a second plate, which presses the chest and increases the viewing area.
- The resulting image is displayed on film; if a digital mammograph is used, then on the matrix.
- If necessary, photographs are taken in several projections: frontal, lateral and oblique.
- Similar actions are performed with the second breast.
- If there is insufficient data after an X-ray examination, another form of diagnosis may be prescribed.
The duration of the procedure is about 20 minutes. Immediately after its completion, the client is given a description of the mammography.
Patients with breast implants are diagnosed by specialists with appropriate qualifications and experience.
With old-generation X-ray machines, if a woman had small breasts, it was difficult to conduct a full examination. This problem does not exist with modern mammographs. They allow you to take a full-length informative photo in a side projection.
Can I have a mammogram during my period?
After ovulation of the egg, if fertilization has not occurred, a sharp hormonal decline begins. As a result, the mucous membrane of the uterus peels off, that is, menstruation begins. The glandular tissue of the mammary glands also undergoes reverse development and becomes less dense, but this process is slower. Its lowest density is observed at the end of menstruation. It is from this period that mammography is prescribed.
Planned and preventive examinations are not prescribed during menstruation , but it is possible if there is a need for it, when it is undesirable to wait 5-7 days. Also, mammography can coincide with menstruation in case of an irregular cycle, which is not always possible to predict.
What mammography shows
Early detection of breast cancer is the main goal of mammography. In the images, the presence of cancer cells is accompanied by:
- irregular form of formation - elongated, flattened, amoeboid;
- fuzzy or uneven edges, cords;
- “path” between the tumor and the nipple;
- numerous small calcifications in the ducts;
- signs of infiltration, hypervascularization, sclerosis and fibrosis;
- bulging or recessed nipple;
- changes in the structure of the skin over the tumor.
A benign tumor on mammography looks like a darkening of a regular (round or oval) shape with clear contours. The surrounding tissues are not included in the pathological process. Observation over time demonstrates the slow growth of affected tissues.
Mammography is a universal diagnostic method that shows:
- mastopathy, which is evidenced by cysts, heavy shadows and an increased concentration of glandular tissue;
- calcifications, the accumulation of which can indicate both the current cancer process and more harmless causes - stagnation of milk after lactation, calcium metabolism disorders or the presence of a benign formation;
- fibroadenoma - a harmless tumor characterized by intensive growth and large-scale fibrous proliferation;
- atypical fatty involution, indicating low estrogen levels and possible infertility;
- cysts, which are cavities filled with contents. The result of mammography in this case is ambiguous, since such formations are difficult to distinguish from cancer. If differential diagnosis is necessary, examination using other technologies is prescribed.
What does the procedure reveal and what diseases does it diagnose?
Mammography clearly shows the smallest structural changes in the mammary gland ranging in size from 1-2 mm. This may be a tissue compaction, which appears on the image as a light area, characteristic of fibroadenoma, a cancerous tumor, and high-density white lesions are calcifications.
The thinning of the tissue structure has a dark color in the image; this happens when the tumor disintegrates or there is a purulent process. Dark-colored lesions are cavities in the chest, cysts. also allows you to examine the milk ducts , which are clearly visible as hollow longitudinal formations with clear contours. Their deformation indicates compression by a tumor. Polyps and intraductal cancer can also be found in the lumen of the ducts.
The detection rate of cancer on mammography varies between 92-96%, but none of the known methods gives a 100% diagnosis.
With mammography, one can only suspect cancer with a high probability, and to clarify the diagnosis, additional studies are needed, the most informative of which is a puncture of the gland with a biopsy.
Research results
Mammography of each patient gives different results, depending on the individual characteristics of each of them, so interpretation of the results should be carried out by an experienced mammologist. Their interpretation is based on comparing the image in the photograph with the norm.
Mammography is interpreted in accordance with the generally accepted medical standard, on the basis of which such categories are assigned.
- Incomplete assessment when, for one reason or another, a mammography image is considered insufficiently effective.
- Negative, that is, the woman is considered absolutely healthy.
- A benign formation, which is also considered a negative result, since no oncological processes have been identified.
- Benign formation that requires monitoring over time.
- A suspicious tumor with a low probability of cancer, upon detection of which a biopsy is prescribed for a more in-depth analysis.
- A suspicious tumor with a high probability of cancer, which is also confirmed or refuted by biopsy.
- Cancer confirmed by needle biopsy results.
In addition to searching for dark spots in the breast area, the doctor analyzes the condition of tissues, ducts, vessels, and lymph nodes.
Ultrasound of the breast with elastography
Ellastography is an additional, but completely optional option in the ultrasound machine software. Its presence has a marketing purpose - to attract more patients.
| Ultrasound of the breast with elastography. A relaxed breast cyst is visible - its walls are wavy. | Ultrasound of a tense breast cyst. It is round in shape, almost spherical |
In both cysts - like all benign tumors - the horizontal size is greater than the vertical. It is advisable to puncture the second cyst to relieve tension and pain.
If repeated punctures of the cyst (2-3 times) do not lead to its disappearance, you can consider removing it - excision of the walls of the cyst.
Advantages and disadvantages
Advantages:
- one of the most effective screening methods;
- highly detailed mammography results;
- excellent visualization of the mammary gland ducts;
- high information content when diagnosing cysts;
- distinguishability of the location and size of calcifications, including the smallest ones;
- high resolution, allowing to distinguish formations of any size;
- relative safety. Even film technology requires radiation of no more than 0.4 ml/3v, and digital mammography – even less.
Flaws:
- radiation exposure. Although minimal, X-ray radiation is still present;
- possible pain and some discomfort during scanning;
- the procedure is limited and informative for women under 40 years of age, due to natural physiological characteristics;
- difficulties in conducting research for those with small or very large breasts (for old X-ray machines);
- presence of contraindications - for pregnant women and nursing mothers.
Age restrictions
Why can't you have a mammogram before age 40? There is no such ban. The fact is that in young women the structure of the soft tissues of the mammary glands is denser; they prevent the penetration of X-rays, thereby significantly reducing the quality of the image and the feasibility of the procedure as a whole.
At what age is it customary to have a mammogram? The gold standard is 40 years of age. It is at this age that the first scan is scheduled. In the absence of additional reasons, the regularity of this procedure is once every 24 months.
After 50 years of age, this examination must be completed annually.
Regardless of age, women at risk should be examined with a mammogram according to the schedule established by the doctor. The reasons for falling into this group are infertility, excess weight, dysfunction of the pancreas and thyroid glands, mastopathy, mastitis, and diseases of the reproductive system.
How the mammograph works
The essence of diagnosis is the passage of low-dose X-rays through the tissue of the mammary glands. A mammograph is a special X-ray machine that is designed exclusively for such examination. The entire process is displayed on the developed film or computer monitor screen.
What can you see in the photo
The photo clearly shows the structure of the paired female organ: glandular and connective tissues, ducts, vessels. When abnormal lesions are identified, their shape, location, and size are recorded. Mammography can detect the following pathologies:
- Calcifications. These are groups of calcium salts that have accumulated in the mammary glandular tissues. Large formations are not related to oncology. Minor accumulations of salts indicate an incipient pathological process. Sometimes large groups of calcifications are associated with cancer developing in the body.
- Cysts. These are cavity formations filled with liquid. It is not always possible to distinguish cancer from a cyst, so after they are identified, the patient is sent for additional examination.
- Fibroadenomas. They are exclusively benign formations. Fibroadenomas are more often detected in young women. A benign tumor is prone to uncontrolled growth and therefore requires careful monitoring of further development.
Is mammography harmful?
This question is often asked by women. It is due to the fact that digital mammography of the mammary glands is a procedure with radiation exposure to tissue. The average dose received during the examination is 0.03–0.1 m3v. The overall effect on the body does not cause any harm, since the volume of tissue that is exposed to radiation is small.
Popular questions
Which is better: film or digital mammography? Is mammography harmful, and at what age can it be done? If a mammogram is scheduled, on what day of the menstrual cycle is it best to do it? Can mammography be done for pregnant and breastfeeding mothers? The prevalence of this procedure raises a lot of important questions. We have already answered some of them earlier. Here are answers to questions not included in previous sections.
Does it hurt to have a mammogram?
When performing the procedure between the 7th and 12th days of the menstrual cycle, any discomfort is excluded. If mammography is scheduled for other days, then when the mammary gland is compressed between the plates, it may be painful. Unpleasant sensations are caused by increased breast sensitivity during this period.
How often should I have a mammogram?
To answer the question of how often mammography can and should be done, two aspects of the problem should be considered.
On the one hand, mammography can be harmful. We are talking about the total radiation exposure to the body when exposed to X-rays. However, modern medical equipment has been equipped with technologies that ensure maximum safety: a protection system for activating rays, highly sensitive films, and intensifying screens. All this allows you to significantly reduce the radiation dose.
The second aspect is a comparison of the risk of developing cancer from radiation exposure and the benefits of early detection of cancer with regular examination. According to statistics for Moscow, as a result of systematic screening, the incidence of breast cancer has decreased to 1 person per 256 thousand examined.
The importance of X-ray scanning is obvious. Moreover, it is recommended to undergo it as many times a year as the attending physician considers necessary.
Can mammography be wrong?
Both film and digital mammographs do not guarantee a 100% objective result. In practice, the detection rate of pathology using the method in question is 90-95%.
Mammography, as a method, involves deciphering the results by people who can often make mistakes. Approximately 15% of deviations go unnoticed even by the most qualified specialists.
Mention should also be made of false-positive results, when a positive diagnosis is made based on mammogram data, which is subsequently refuted on the basis of histological analysis of the biopsy specimen.
Is it harmful to have a mammogram?
Considering that X-ray radiation is involved in the mammography process, the conclusion suggests itself that this procedure is dangerous. Is it so?
Let's give a few numbers. The radiation dose during a mammographic examination ranges from 0.1 to 0.4 ml/3V, while the radiation dosage during plain radiography reaches 0.8 ml/3V, and even more during fluorography. The total ionizing radiation from the environment is approximately 4 ml/3v, and the dose incompatible with life is 150 ml/3v.
The harm of mammography cannot be denied. According to statistics, out of 200 thousand women examined, the likelihood of developing a malignant tumor falls on one of them. However, from the above figures it follows that the risk is minimal, especially considering the importance of early detection of oncological processes.
You should not refuse screening out of fear of radiation exposure. Let us recall that there are methods that do not involve transillumination with rays, for example, electrical impedance mammography.
On what day should you have a mammogram?
According to doctors, the optimal period for mammography is between the 7th and 12th days of the standard 28-day menstrual cycle. Depending on its phase, hormonal transformations occur in a woman’s body, which directly affect her mammary glands.
From the 1st to the 13th day of the menstrual cycle, the maturation of the egg occurs. At this time, estrogen hormones predominate, which contribute to an increase in the number of glandular and connective tissues in the breast.
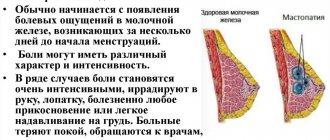
From the 14th to the 16th day, ovulation occurs, or the release of a mature egg from the ovary. The concentration of estrogen at this point reaches its maximum. The resulting glandular elements merge with each other, forming cysts. This process causes pain in the chest.
From the 17th to the 28th day, the corpus luteum matures, and the uterus is ready to receive a fertilized egg. The dominant hormone in this phase is progesterone. It increases blood circulation in the mammary glands, which causes their swelling. A woman experiences increasing feelings of pain and bloating, which persist in the first days of menstruation.
It is during the period from the 7th to the 12th days that there is no swelling in the mammary gland, its sensitivity is reduced, which is especially important when the breast is compressed between the plates. In addition, swelling negatively affects the clarity of the images, which reduces the information content of the study.
With a short cycle (21 days), the examination is scheduled between the 3rd and 5th days, with an extended cycle (more than 35 days) - between the 10th and 18th days.
During menopause, mammography can be done on any day, no matter what the doctor prescribes.
What to choose: mammography or ultrasound?
Mammography and ultrasound are different methods for diagnosing breast pathologies.
Thus, ultrasound is based on the action of ultrasonic waves, and mammography is based on X-ray radiation.
It doesn’t matter at what age an ultrasound is performed; mammography is prescribed for women who are over 40 years old.
Ultrasound examination is less informative. The detection rate of pathology is 85-90%. This form of research is also characterized by overdiagnosis - up to 66% of false-positive diagnoses.
Using ultrasound, you can identify the smallest neoplasms, examine objects from different angles, assess the condition of the lymph nodes, and check the blood flow in the organ. Breast size does not matter for ultrasound, which makes it the optimal form of examination for men. This technique is convenient for performing puncture biopsy. It is painless and safe, approved for women during pregnancy and lactation, and suitable for young patients under 40 years of age.
Unfortunately, ultrasound diagnostics are ineffective for identifying cysts, calcifications and analyzing milk ducts.
The information provided indicates that both methods are relevant. They are not intended to replace each other, but to complement each other.
Mammography or ultrasound of the mammary glands - which is better?
Which method of examining the mammary glands in women should they choose?
This is not an idle question. Some patients are afraid of receiving a large dose of radiation during mammography, especially amid rumors and speculation on this topic. In fact, these doses are so small that the procedure can be repeated more than once throughout the year without harming the patient’s health. The mammography method is much more accurate than any other, allowing you to detect even the slightest lumps in the breast. These can be cysts, fibroadenomas (benign formations), calcifications (deposits of calcium salts that can lead to cancer). A tissue biopsy is required to make an accurate diagnosis.
Ultrasound is not always able to detect the beginning of the process. At the same time, when a neoplasm is detected, ultrasound allows you to “see” immediately what exactly is developing - a tumor or a cyst.
Ultrasound waves are reflected by the dense structure of the tumor and freely passed by the cyst with its liquid filling. An ultrasound will better show the abscess area with mastitis.
Today, more than 80% of patients choose mammography as a more reliable and accurate research method.
If the results of a mammographic examination raise doubts and discrepancies, and do not allow an accurate diagnosis, specialists often insist on performing both procedures.
This may happen:
- with high breast density; when a tumor is detected without visible symptoms in a woman.
Additional measures may include ultrasound, MRI, and repeat mammographic examination.
If we are talking about prevention, then no special reasons for conducting a mammography examination are required. After age 40, all women should undergo mammography annually. It often happens that women are reminded of this during their next medical examination.
If there is no suspicion of pathological processes, patients under 40 years of age are prescribed only ultrasound. The exception is young women, starting from the age of 30, with a hereditary predisposition to cancer, in particular breast cancer. They are at particular risk and should undergo preventive examination along with older patients. This is a preventive mammography of the mammary glands.
There is also a diagnostic mammography, which is necessary if the development of a neoplasm is suspected.
Obvious symptoms that should alert a woman (can be detected by breast self-examination) and prompt an early examination are as follows:
- Lumpiness in the chest, pain when pressing on the affected area.
- Nipple discharge.
- Changes in the color and texture of the skin on the chest area.
- Changing the shape of the breasts or nipples.
The only contraindications for the procedure are pregnancy and breastfeeding. In these cases, if urgent examination of the mammary glands is necessary, electrical impedance mammography is prescribed. With this method of examination, the woman is not exposed to x-rays.
There is no reason not to have a mammogram. The examination lasts 10-15 minutes and does not cause any discomfort during the procedure. A woman can experience pain only if her breasts are sore from a lump. The plates of the device, slightly compressing the chest, cause such symptomatic pain.
Preparing for the study is not difficult. The doctor prescribes mammography individually, but most often in the period from 6 to 12 days from the beginning of the cycle. If there is a need for urgent examination, these indicators are not relied upon.
Before the procedure, patients should not use deodorants and creams in the armpits, décolleté and chest areas. These products can “smudge” the picture, appearing as dark spots on the film.
A woman should not be wearing jewelry or other adornments.
Mammography is carried out as a preventative measure for all women over 40 years of age once every 2 years. At the discretion of local institutions for the female population over 50 years of age - once a year.
In addition, there are unscheduled indications for this type of examination.
Carrying out a mammogram while breastfeeding is completely acceptable.
During pregnancy at any stage, it is preferable to use the ultrasound method due to the absence of side effects, primarily radiation exposure to the body of the mother and fetus. Carrying out a mammogram during breastfeeding is quite acceptable, but it is not very informative for a doctor. It is recommended to use other auxiliary studies.
It is considered most correct to undergo a mammological examination on days 5-13 of the menstrual cycle, i.e. in the first phase. In the second phase, the breast tissue undergoes some hormonal changes: the ducts expand, the structure of the glandular component changes, and swelling of the soft tissues may appear. In this case, the result may be unreliable, and the examination will be endured with a feeling of discomfort and pain.
According to basic recommendations, mammography should be performed no more than once a year. But in urgent cases, up to 2-3 times are allowed. If more frequent examinations are necessary, it is reasonable to use auxiliary methods - ultrasound (ultrasound), magnetic resonance imaging (MRI).
Mammography is carried out in the X-ray room, where the mammography machine is located. The woman is shown how to position herself next to him. The position depends on the type of equipment (standing or sitting). Next, a protective apron made of lead material is placed on the waist area, covering the lower abdomen.
The mammary glands are placed on a plate intended for this purpose, and the chest is pressed on top with a similar plate.
If a pathology is detected, the woman may additionally undergo radiography in a different projection - lateral and/or oblique. At the discretion of the doctor, a targeted mammography is possible, when the affected area of the gland is directly imaged on an enlarged scale.
A photo with a description can be received on the same day. Some clinics are equipped with digital equipment that provides more detail in the resulting image. All information can be saved on electronic media and used at any time.
On the first day, a woman may complain that her breasts hurt after a mammogram. This is due to the mechanical pressure of the plates, does not last long and eventually goes away on its own.
Other X-ray examinations should be rescheduled on this day so as not to exceed the permissible radiation dose.
Both methods, mammography and ultrasound, are highly accurate and specific for the presence of breast tumors. Ultrasound is preferable if visualization of areas located near the chest from different angles is necessary. These areas are difficult to reach for x-rays.
In addition, the ultrasound method more accurately differentiates the cystic and solid components of the tumor, identifies small pathology, and shows the presence of blood flow. It is also more informative in young females due to the increased density of organ tissue at this age. Ultrasound can be used at any stage of pregnancy.
Ultrasound is preferable if visualization of areas located near the chest from different angles is necessary.
Ultrasound allows you to analyze the size and shape of lymph nodes - an important marker for differential diagnosis between benign and malignant formations.
However, mammography makes it possible to detect single or multiple small calcifications, extensive tissue restructuring, and precise identification of the type of cyst, which is impossible with ultrasound.
Ultrasound of the mammary gland does not replace mammography! If you are over 35 - 40 years old, in addition to ultrasound of the mammary glands, you need to have a mammogram.
Young women rarely get cancer. Benign tumors are more common - cysts, fibroadenomas, ductal papillomas, localized FAM.
Up to 35 years of age, for the purpose of “just checking”, or if the woman herself has found a “breast lump”, it is enough to do an ultrasound.
An ultrasound shows only that part of the gland on which the sensor is placed - a lot depends on the specialist.
Mammography and MRI show the entire gland at once - it’s harder to miss something.
For fibroadenoma, we can combine its removal with plastic surgery. For breast cancer, we perform oncoplasty or one-stage reconstruction.
In many women, in the last days of the cycle, the breasts “fill up” or become hard and become sensitive. If this occurs in you, do an ultrasound of your breasts after menstruation - after the indicated manifestations of premenstrual tension disappear. For some it is on the 7th day of the cycle, for some it is on the 5th, ... for some it is not at all. It doesn’t matter to them when to do a breast ultrasound - it can be done on any day of the cycle.
Although, having a good ultrasound machine, an experienced specialist will perform an ultrasound of the mammary glands on any day of the cycle.
We recommend having an ultrasound scan from OUR PARTNERS
In our country, underperforming medical students are not screened out. Everyone gets diplomas. Well-performing specialists do not receive tangible legal financial incentives. Today “only the lazy” don’t do ultrasounds.
A weak specialist avoids precise formulations in his conclusion: in the middle between cancer and a benign process; always prescribes “ultrasound control after 3-4 months”; everyone gets Bi-RADS 3.
We recommend having an ultrasound of the mammary glands from our partners
Mammography results
An independent attempt to study the photographs and descriptions sent to your home can only intensify the panic state and lead to a nervous breakdown. Therefore, the study of the examination results should be entrusted to the attending physician. He will examine the images, make a conclusion about the presence or absence of cancer, and also talk about the next steps to combat the disease or prevent it. Perhaps such a study will help identify what was missed in the picture. Mammography can detect the presence of neoplasms only in 85% of cases.
Mammography after menstruation
It has already been described above how hormonal levels affect a woman’s breasts every month, but what to do if menstruation stops and menopause occurs? If a woman is fifty years old, then she is close to the onset of menopause - the period of preparation for menopause. Menstruation stops, hormonal levels stop creating the usual “roller coaster” and stabilize.
On what day should I have a mammogram if I don’t have my period? Often women after reaching the age of 45-50 worry that hormonal fluctuations will distort the results. Doctors say that after menopause you can come for a breast examination any day; mammograms will correctly show the condition of your breasts.
You should not have a mammogram before your period, just like during your period. This is due to the fact that the mammary gland swells during this period, and the density of its texture increases. This is a problem for research, since X-rays do not pass through well, and the result may be unreliable. Moreover, during menstruation the breasts are painful, diagnosis can cause severe discomfort. It will not be possible to fix the breasts in the desired position during menstruation; the woman will not be able to stand for the required amount of time in the desired position.
A factor in favor of refusing diagnostics before and during menstruation is that the breasts accumulate fluid at this point. It does not allow tumors and other neoplasms to be recognized.
The issue of irregular periods deserves special attention. If a woman has them 1-2 times a year or are absent for a long period of time, and then suddenly appear, a mammogram is scheduled for the nearest possible date.
The best time to undergo diagnostics is 3-6 days after the end of menstruation. But strictly before the period of ovulation. It is at this time that the data obtained will be reliable and informative. If the time for undergoing diagnostics has already been missed, the woman is advised to postpone mammography until the next good period.
Since the duration of the menstrual cycle is different for all women, you need to choose the day of diagnosis based on the total number of days. In most cases, women begin menstruation with deviations of 2-3 days. The cycle can be short, medium or long.
During menopause, when reproductive functions decline and menstruation has been absent for a long period of time, mammography can be done on any convenient day.
Due to the individual characteristics of each patient, the date of mammography is agreed upon with the doctor:
- With a short cycle. If bleeding occurs after 21-23 days, diagnosis is prescribed between 3 and 5 days. At this time, the breast does not hurt, it is easy to squeeze, mammography gives a good result. It is not recommended to undergo examination immediately after menstruation for the same reason of high hormone activity.
- With a standard cycle. If it lasts 28 days, diagnostics are prescribed with a wider margin - from 6 to 12 days.
- With a long cycle. For some women, the cycle lasts over 35 days. In this case, diagnosis is prescribed 10 days after the end of bleeding. The maximum period of time is from 10 to 18 days.
The situation in which menstruation is not stable and lasts either 20, then 30 or more days deserves special attention. Then the day of the examination is also selected with the doctor based on observations.
If you are scheduled for a mammogram, on what day of your cycle is it best to do the screening during menopause? Since in most cases diagnostics are prescribed to representatives of the fair sex after 40 years of age, this issue is quite relevant.
If a woman has already reached menopause and her cycle has become irregular, then the examination can be carried out on any day. You should not wait for the next bleeding, as it can occur only after six months. When a representative of the fairer sex talks about the onset of menopause (there has been no menstruation for several years), diagnostics are carried out immediately.
Many women worry that diagnostics may give false results. It is worth reassuring such patients. Their hormonal background of the reproductive system has already stopped working. There is no way he can distort the result.
Contraindications
Prohibitions on the use of mammography include pregnancy and lactation. It is also prohibited for women who had an abortion less than 6 months ago. If the patient has breast implants, mammography is also prohibited.
On what day of the cycle is mammography examination preferable?
To answer this question, you need to take into account each representative of the fair sex separately. So, it is better for some women to undergo examination on the 3rd day of the menstrual cycle. For others, it is preferable to carry out diagnosis on the 8th day from the beginning of menstruation. Examinations are prescribed completely differently for women in menopause. Let's take a closer look at the mammography procedure (on what day of the cycle it is performed).
The information content of the mammography technique is determined by what day of menstruation is done.
The female mammary gland belongs to the hormone-dependent organs. The features of the structural composition, volume and density of these organs are determined by the presence and quantity of estrogens in the body - specific female hormones.
If a patient who needs to be diagnosed with mammography is far from menopause, she should take into account the characteristics and specific days of the cycle.
It is important to understand that this examination on critical days and immediately before menstruation is undesirable.
According to experts, the optimal time to undergo a mammogram is after menstruation, from the 5th to the 12th day of the cycle. The corresponding point of view of doctors is easy to explain: before menstruation, with the assistance of the sex hormone progesterone, there is an accumulation of fluid structures in the lobules of organs and in intertissue structures.
If you decide to undergo a mammogram when your period begins or a day or two before it starts, you should not count on the information content of the result.
Having a mammogram during your period is also not a good option. Although the period of menstrual flow is not a contraindication for such a diagnosis, doctors recommend waiting three to four days until the swelling of the tissue goes away and the primary structure of the glandular lobules is restored.
The choice of the day when it is better to diagnose mammography of the mammary glands is also determined by the characteristics of a woman’s menstrual cycle, in particular, its duration:
- if the duration of the cycle is very short (less than 25 days), diagnosis should be carried out on days 3-5 or after menstrual flow stops;
- if the cycle lasts approximately four weeks, the most appropriate mammography diagnosis will be in the period from the 6th to the 12th days (during this period of time the mammary glands will feel most relaxed due to the influence of hormones);
- during particularly long cycles exceeding 35 days, the greatest reliability of a mammography examination is expected between the 10th and 18th days from the start of menstruation;
- if the cycle is irregular, mammography is preferable after the complete cessation of bleeding;
- at the stage of menopause and later, the time of diagnosis does not affect its results.
It should also be taken into account that the duration of the menstrual cycle is determined by the individual characteristics of a woman’s body, in particular, age. Its duration can be influenced by various factors, including the level of sexual activity of women.
Mammography: pictures, technique.
Mammography is a radiation research method most suitable for screening studies of the mammary glands. It is characterized by high sensitivity when examining glands with a large content of adipose tissue and the ability to visualize microcalcifications well, making it possible to detect small carcinomas at an early, prognostically favorable stage.
In addition to high sensitivity and satisfactory specificity, mammography has a number of advantages: non-invasive and cost-effective method, ease of study documentation.
Compared to radiographic examinations of other parts of the body, mammography has more stringent requirements for image quality and equipment, which makes mammography one of the most complex examinations in traditional radiology.
To ensure a uniform understanding of the X-ray image of the breast, mammograms should always be performed in generally accepted, strictly standardized projections. There are main and additional projections. The main ones are the mediolateral oblique and craniocaudal projections. Taking images in these two projections should be considered mandatory for any mammographic examination.
Considering that mammograms in the main projections with a high degree of reliability make it possible to identify or exclude a malignant process, additional projections are used to clarify the results or for more complete visualization of the organ.
The mediolateral oblique view is the most important because it best visualizes the tissue close to the chest wall, the axilla, and the upper outer quadrant of the gland. Most cancers are detected on mammograms taken in the mediolateral oblique projection.
The craniocaudal view is also the second projection for visualizing the axillary region. This area is rich in glandular tissue and should be carefully examined, as it is a common location for malignant neoplasms.
If images in standard projections completely visualize the mammary gland and clearly show or exclude a malignant formation, mammograms in additional projections are not required. However, if the slightest doubt arises, performing mammograms in additional projections should be considered mandatory.
The most important additional projections are:
• 90º lateral projection; • lateral and medial craniocaudal projections with direct image magnification; • tangential projection; • axial projection;
Diagnosis of breast diseases
All diseases of the mammary glands are usually divided into two large main categories: benign and malignant.
The first category is the most extensive and includes diseases of an inflammatory and dyshormonal nature:
- The most common inflammatory diseases of the mammary glands include mastitis and abscess. This is an initial inflammatory process in the tissue, which subsequently leads to the fact that the purulent focus is encapsulated and manifests itself as severe pain, an increase in the size of the gland, as well as symptoms of general intoxication. In this case, surgery is required. Mammography has no diagnostic value. The risk group for this pathology is nursing women who develop lactostasis or infection due to a violation of the integrity of the skin, does not depend on the cycle.
- Tuberculosis of the mammary gland. A specific disease that leads to inflammatory damage to the skin and the gland itself. In this case, the menstrual cycle is disrupted more often due to intoxication.
- Mastopathy. It may appear diffuse or focal in nature. These changes are associated with the action of hormones, especially with a violation of their cyclicity. In rare cases, these may be pathologies that lead to the development of a malignant process. The consequence of their progression are cysts and fibromas, as well as the phenomena of diffuse and confluent fibromatosis. Diagnosis by mammography requires cycle dependence. Mammography is one of the most reliable diagnostic methods.
- Intraductal papillomatosis. A growth of duplication of the mucous membrane, which opens into the area of the milk duct. In severe cases, obstruction and congestion may occur. If its integrity is violated, the phenomenon of bleeding from the nipple occurs. Rarely, a malignant process may develop.
- Oncological process. It can have various forms of manifestation; if it is not diagnosed in time, the risk of death increases. Detected using mammography.
Currently, there are not many methods that are used to clarify any pathology, as well as determine further management tactics:
- The main one for many years has been mammography. Due to its effectiveness and economic accessibility, the method is considered to be screening. But it also has some disadvantages, which create a lot of problems in use, especially if the woman is young.
- Ultrasound examination is also an equally common method that has proven itself to be the safest. In some cases, it can be used to complement the previous one or remain basic. In the case of inflammatory processes, radiologically negative formations are considered the only diagnostically significant.
- CT scan. A more cost-effective method that serves as a complement to the first two. The method is based on more high-precision tissue scanning.
- Percutaneous biopsy. A method of puncturing organ tissue to determine the nature of the pathological focus. Allows you to most accurately assess the nature of the process, as well as decide on further tactics.
Biopsy method Tomography Mammography Ultrasound of the mammary glands
Before you learn everything about a study called “mammography” (on what day of the cycle it is performed and what indications it has), it is worth finding out what female breasts are. Every girl has mammary glands from birth. However, during the first years of life, the breast does not perform any functions. With the onset of the menstrual cycle, restructuring and development of these glands occurs.
The main function of the female breast is to feed the baby. During pregnancy, the mammary gland undergoes enormous changes, and after childbirth it begins to produce milk. The female breast functions exclusively until the onset of menopause or menopause.