Question: interpretation of the results of ultrasound of the mammary glands?
The site provides reference information for informational purposes only.
Diagnosis and treatment of diseases must be carried out under the supervision of a specialist. All drugs have contraindications. Consultation with a specialist is required! I am 21 years old. Ultrasound of the mammary glands showed: the ducts on both sides are dilated to 2.5-3.5 mm. everything else is within normal limits, no neoplasms were detected, the nodes are not enlarged. What does this dilation of the ducts mean? not pregnant, haven't given birth
Echographically, the mammary gland has a mesh structure; the size of the ducts does not indicate any pathology.
I am 32 years old and an ultrasound showed glandular tissue of reduced echogenicity, heterogeneous echodensity, fibrous cords. The milk ducts are visible in all areas of the glandular tissue. Anegoic inclusion 5 and 3 mm. The cystic component is pronounced. FCM Focal form
Fibrocystic mastopathy requires observation by a mammologist and complex treatment. Before starting treatment, it is necessary to find out the cause of mastopathy; a specialist doctor will help you figure this out by conducting an examination and laboratory tests.
I am 25 years old. 4 years ago, fibrocystic mastopathy was discovered, and she was treated with mastodinone, iodomarin, and vitamins. then at the age of 23 she gave birth, the child was 2 years old, she breastfed for half a year, six months after the cessation of lactation she had a breast ultrasound, there were brushes in both breasts, she was treated again with mastodinone - a course, vitamins. after a year of repeated ultrasound, the condition improved, all the formations in the left breast disappeared, but something remained in the right. the key phrase that worries me most in this piece of ultrasound is that a hyperechoic formation of 6.5 mm with smooth contours was discovered in the upper outer quadrant. what is it in human language, and is it dangerous.
“ultrasound - in the upper outer quadrant a hyperechoic formation 6.5 mm in diameter with smooth contours was detected” in other words: in the upper outer sector of the mammary gland, according to the results of an ultrasound examination, compacted tissue 6.5 mm in diameter with smooth contours was found
Good afternoon Help me decipher the ultrasound of the mammary gland Left mammary gland - the skin is not changed, the nipple is not changed, tissue differentiation is visualized mainly as fat, the thickness of the fibroglandular layer is 10 mm, milk ducts are up to 1.5 mm, regional lymph nodes are not differentiated Right mammary gland - skin not changed, the nipple is not changed, tissue differentiation is visualized predominantly fatty, anechoic incl. from 5.9 mm to 12 o’clock 9.8-8.6 mm, thickness of the fibroglandular layer 11 mm, milk ducts up to 1.4 mm, regional lymph nodes are not differentiated
According to this conclusion, mastopathy cannot be ruled out, so I recommend that you personally visit a mammologist for an examination and, if necessary, prescribe adequate treatment. You can get more detailed information on the issue you are interested in in the corresponding section of our website by clicking on the following link: Mastopathy
I am 39 years old. There are no complaints of chest pain. The ultrasound protocol indicates: Mammary glands: The ratio of adipose and glandular tissue of both piers. iron 2:1. The skin is not thickened and is visualized as a thin hyperechoic line. Subcutaneous fatty tissue is moderately expressed. Glandular tissue is visualized as a single layer of increased echogenicity, diffusely heterogeneous structure due to the alternation of hyperechoic connective tissue elements with less echogenic glandular structures. In the lower outer square of the right pier. the gland is detected with a formation of increased echogenicity, non-uniform structure, with anechoic inclusions of irregular shape up to 8x6 mm in size, with clear contours, size 39x14x36 mm, the milky ducts are not wide, the retromammary space is not changed. During CDK, no areas of pathological vascularization were identified.
According to the data provided, fibrocystic mastopathy cannot be ruled out, so I recommend that you personally visit a mammologist for an examination and, if necessary, prescribe adequate treatment. You can get more detailed information on the issue you are interested in in the corresponding section of our website by clicking on the following link: Fibrocystic mastopathy. You can also get additional information in the following section of our website: Mammologist and mammology
I am 32 years old. During feeding, 2 lumps formed in one breast; at the first ultrasound, lactostasis was diagnosed. After I stopped breastfeeding, I did a second ultrasound, here is the result: The echostructure is predominantly glandular, glandular tissue with clear contours, the milk ducts are not dilated, additional formations are single anechoic formations in both lobes, 2-3 round, smooth, homogeneous without hemorrhage (I didn’t catch the last word). The lymph nodes of the outflow tract are enlarged - NO. Ultrasound signs: focal formations in both mammary glands, characteristic of thickened glands. Tell me please, what does this all mean?
Existing lumps in the breasts may be associated with lactostasis, and mastopathy may also be the cause. I recommend that you personally consult with a mammologist, who, after conducting an examination and carefully studying the ultrasound results, will select further monitoring tactics and, if necessary, prescribe treatment. You can obtain additional information on the issue you are interested in in the appropriate section of our website by clicking on the following link: Ultrasound. You can also get additional information in the following section of our website: Mammologist
Read more How is hysterosalpingography done?
Normal female breast anatomy
The mammary gland consists of stroma and parenchyma. The parenchymal component of the mammary gland is represented by the ducts and acini of the mammary glands. The stromal component is the support of the mammary gland, i.e. its connective tissue, which connects the parenchyma of the mammary gland itself with adipose tissue. The number and distribution of structural components of the mammary gland are strictly individual, depending on the woman’s age and her hormonal status.
The parenchymal component of the mammary gland consists of 15-25 lobes, which have their own ducts (milky ducts) flowing into the common space under the nipple. This space is called the milky sinus. Each milk duct is successively divided into segmental, subsegmental and terminal. The terminal ducts empty into the mammary acinus.
Breast tissue has three levels. The first, most superficial, subcutaneous layer consists of fat, organized into lobules, bounded by fibrous septa by Cooper's ligaments. Cooper's ligaments connect the superficial layer to the middle layer. The middle layer is the mammary gland itself, the mammary layer is represented by the parenchymatous component. The deepest, retromammary layer, a derivative of fat lobules, is bounded in front by the deep mammary fascia and behind by the pectoral fascia.
Features of the breast associated with the menstrual cycle
The breast is a hormonally sensitive organ of the female reproductive system. During a normal ovulatory menstrual cycle, the changes that occur in the mammary gland are as follows. In the first, follicular phase of the cycle (days 7-14), minimal structural changes occur. The gland ducts are experiencing the proliferation phase of gland development, the alveoli are closed, and the cellular stroma is dense. In the luteal phase of the cycle (days 16-20), the proliferation of the glands ends, and the glands expand, caused by edema and hyperemia of the alveoli. Normally, during ultrasound of the breast, cyclic changes are faintly noticeable.
Features of the breast associated with pregnancy and breastfeeding
With hormonal changes associated with pregnancy and lactation, rapid development of the parenchyma occurs, namely the ducts and acini of the mammary gland. Due to this, the breasts increase in size and often become more sensitive. This is accompanied by regression of the interlobular stroma, the fat lobules of the subcutaneous and retromammary zone are reduced. Only during breastfeeding does a full cycle of development of all mammary gland structures occur, which is of utmost importance in the prevention of breast cancer. But at this time the mammary gland is especially vulnerable to external factors. Therefore, during breastfeeding, especially at the stages of lactation, minimal external influence is very important. Expression should, if possible, be carried out by the nursing mother herself using a breast pump. Spreading with “alien hands” with “crocodile tears” of a nursing woman causes deep trauma to the breast, negates the value of breastfeeding in the prevention of breast cancer, and even vice versa, increases the risk of developing breast cancer in the future.
Anatomical structure of the mammary glands and functions of the ducts
To understand the importance of the functions of the mammary ducts, you need to understand the anatomical structure of the breast. It is quite complex and can change almost throughout a woman’s life, as it strongly depends on hormonal levels. The mammary gland contains different tissues, namely connective, adipose and glandular (and their ratio depends on individual characteristics and may undergo some changes).
The mammary gland is divided into lobes, the total number of which can vary from 8-10 to 25-30. These structural elements, in turn, are divided into smaller lobules. Each lobule contains separate alveoli (about 40-80). A small duct leads from each alveoli, which then connects with others and forms larger elements. Thus, a whole branched complex network is formed, and its final parts are the largest ducts leading directly to the nipple (it contains approximately 5-8 small holes through which milk is released).
There are several types of mammary ducts, and they all differ in function and structure:
- The first type is less developed and is typical for girls who have not gone through puberty. The structure of such elements includes no more than 8-10 milk ducts.
- The second type is formed after puberty, and such lobules can contain up to 35-40 ducts.
- The third type is formed during pregnancy from the second type, characterized by the number of ducts reaching 70-80.
- The last type is the fourth, and these lobes are formed during lactation, and after its completion they regress again to the third type (the number of ducts can reach 100-120).
Ultrasound of the mammary glands is normal
The most superficial structure visible during ultrasound of the mammary glands is the skin. During ultrasound of the mammary glands, the skin looks like an echogenic uniform zone, 2 mm thick; in the area of the areola, the skin is slightly thicker. Fibrocystic disease (fibrocystic mastopathy) Fat lobules in the subcutaneous and retromammary zones with ultrasound of the mammary glands look like low-echoic structures, penetrated by echogenic lines and dotted loci. Fat lobules have a multifaceted or elliptoid shape. The tissue representing the mammary zone consists of closely associated parenchymal structures and connective tissue. In general, this area on breast ultrasound is hyperechoic with small areas of hypoechoic fatty tissue. On ultrasound of the mammary glands in lactating women, the mammary zone is moderately echogenic with the same inclusions of fat of low echogenicity. Hypoechoic linear branching structures during ultrasound of the mammary glands against the background of the hyperechoic mammary zone of the duct. The normal width of the ducts on ultrasound of the mammary glands is from 1 to 2 mm, they do not have expansions, and can evenly narrow towards the periphery of the mammary gland. The exception is the mammary sinuses, which expand directly in the retromamillary region.
An abnormal picture on breast ultrasound is observed in the presence of benign and malignant breast formations.
Normal breasts on ultrasound
During ultrasound of the mammary glands, structures are assessed as hyper-, iso- or hypoechoic in relation to subcutaneous fat.
The skin is a central hyper- or isoechoic stripe bordered above and below by even more hyperechoic lines. The width of the three-layer complex is less than 2 mm, slightly thicker above the areola. Under normal conditions, the skin is visualized as a smooth hyperechoic line up to 7 mm thick. Due to fat deposits, the skin can take on the appearance of two hyperechoic lines separated by a thin hypoechoic layer. The border between the dermis and the underlying tissues is never identified, unlike the mammary gland.
Pre- and retromammary fat - the fat around the mammary glands is hypoechoic compared to fat in any other area and has a lobular structure, each lobe is surrounded by a thin hyperechoic film.
We have not identified any major differences in the description of the retromammary area among almost all authors working with the mammary gland: the latter consists of fatty tissue, ribs, intercostal muscles and pleura [111,172]. Adipose tissue is visualized as hypoechoic lobules between the hyperechoic lines of the posterior layer of the split fascia and the anterior fascial sheath of the pectoralis major muscle. S. Willson (2007) considered such a constitution to be the term “false gynecomastia”. The pectoral muscles (major and minor) are visualized as multidirectional hypoechoic layers parallel to the skin with a transverse hyperechoic septum. They are bordered by hyperechoic lines of fascia. It is very easy to visualize the ribs as oval formations of high echogenicity with a persistent acoustic shadow. Between the ribs, the operator always notes hypoechoic masses with a typical muscle pattern - intercostal muscles. The deepest hyperechoic line can be visualized in the pleura [7].
Breast parenchyma is a hyperechoic, diffusely heterogeneous layer between the subcutaneous and retromammary fat. The high echogenicity layers represent the supporting stroma, and the low echogenicity layers represent the loose connective tissue around the alveoli and ducts. Ultrasound cannot differentiate glandular tissue (alveoli and ducts) from periglandular stroma. The severity of the periglandular stroma (layers of low echogenicity) surrounding these structural elements is proportional to the development of glandular tissue.
The thickness of the glandular tissue is normal (Trofimova T.N. and Solntseva I.A., 1999): up to 35 years - 9.2-15.6 mm, 35-44 years - 6.7-13.9 mm, 45- 54 years old - 5.2-11.6 mm, over 54 years old - 4-7.2 mm. The change in the thickness of the parenchymal layer of the breast reflects age-related involution: partial and then complete fatty transformation of the glandular tissue. The echogenicity of glandular tissue increases with age, which is associated with fibrosis of the connective tissue components of the fibroglandular zone.
Milk ducts - normally at the base of the mammary gland the diameter of the duct is up to 1 mm, and in the peripapillary region - up to 3 mm. Ducts with a diameter of less than 1 mm are not visible; Normally, they begin to clearly appear in the form of tubular structures at the end of pregnancy and especially during lactation. In 50% of women under the age of 50, ultrasound reveals dilated ducts - anechoic tubular structures with a diameter of up to 5-8 mm.
Cooper's ligaments are hyperechoic processes of the superficial fascia, interlobular layers that stretch from the parenchyma through the premammary fatty tissue to the deep layers of the skin. Cooper's ligaments and Durrett's ridges normally appear after 30 years, before 30 years - one of the symptoms of fibrotic changes.
The ratio of glandular, connective and adipose tissue in the mammary gland depends on age and hormonal status. In young women, glandular tissue predominates, which is good to evaluate using ultrasound, but problematic with mammography. In older women, adipose tissue predominates, which is easy to evaluate with mammography, but problematic with ultrasound.
Drawing. An ultrasound shows a normal breast of a woman of reproductive age: the skin is superficial, a hyperechoic glandular layer is enclosed between the hypoechoic pre- and retromammary tissue, and in the background are the pectoralis major and minor muscles, as well as the pleura. The hyperechoic component of the glandular tissue is represented by the supporting stroma, and the hypoechoic cells are the periglandular stroma around the alveoli and ducts. The severity of the periglandular stroma increases markedly in the second half of the cycle, during pregnancy and lactation, which is due to hyperplasia of the glandular tissue.
The nipple is defined as a round, delimited formation of low echogenicity. The operator can observe an acoustic shadow behind the nipple. Subareolar structures are always hyperechoic
Before the onset of puberty in girls and boys, the structure of the gland is the same - it is represented by adipose tissue, fragments of the ductal and glandular system are in their infancy; Ultrasound shows a hypoechoic structure in the retropapillary region. During puberty, the mammary glands of girls actively develop - the ducts lengthen, branch and final lobular units are formed. By the age of 15, the mammary gland of a teenage girl resembles the structure of the gland of an adult woman.
Until the age of 25, significant changes in the structure of the mammary glands do not occur. At 25-40 years old, the structure of the mammary glands is very diverse. The entire variety of ultrasound images can be grouped according to ultrasound morphotypes. Even in one woman, the morphotype constantly changes depending on age, phase of the cycle, pregnancy, and the beginning and end of lactation.
Types of breast structure according to Kelly Fray
Juvenile morphotype - small in size, behind the nipple or next to the nipple directly under the skin, the glandular layer is highly echogenic, the structure throughout the section is homogeneous, fine-grained, there is practically no pre- and retromammary tissue. In the second phase of the cycle, the milk ducts can be seen.
Early reproductive morphotype - small hypoechoic cells of the same size appear, premammary tissue is present in fragments, more in the lateral sections, retromammary tissue is completely absent, connective tissue structures are poorly differentiated.
With increasing age and the number of pregnancies, a fatty transformation of the glandular tissue occurs; the anterior contour of the gland becomes more wavy due to protrusions at the attachment points of Cooper's ligaments.
Type of reproductive flourishing - the number and size of hypoechoic areas increases, a reticular pattern appears, premammary tissue is a continuous layer, retromammary tissue is absent.
Mature morphotype - fatty lobules appear in the glandular layer, size 1-2 cm, retromammary tissue can be fragmentary or continuous.
Premenopausal morphotype - there is no layered structure, almost complete replacement of the parenchyma with adipose tissue, the remains of glandular tissue are represented by a thin homogeneous hyperechoic strip, there is no mesh pattern, premammary fatty tissue with many fascial partitions.
Postmenopausal morphotype - fat lobes and connective tissue occupy the entire volume of the mammary gland, you can see small hyperechoic areas of a round shape, small in size (3-5 mm) - islands of glandular tissue.
Lactation morphotype - the entire gland is represented by a layer of medium echogenicity of coarse-grained glandular tissue, against which, closer to feeding, multidirectional hypoechoic tubular structures of 2-2.5 mm appear - dilated ducts; Premammary fat is almost absent, fat lobules are not detectable.
In fact, the structure may differ in different parts of the gland, so Zabolotskaya N.V. depending on the ratio of glandular and adipose tissue, it distinguishes:
- The glandular type of mammary gland structure is an early reproductive type;
- The fat type of the breast structure is postmenopausal type;
- Mixed type (with a predominance of glandular tissue, with a predominance of adipose tissue) - normally, most of the glandular tissue is located in the upper outer quadrant - the type of reproductive blossoming, in the center - the mature type;
- A specific type of structure of the mammary gland during lactation.
Drawing. Ultrasound shows normal breasts: a prepubertal girl (1) is a juvenile morphotype, nulliparous (2) and multiparous (3) women in the reproductive period are a morphotype of reproductive prime, a postmenopausal woman (4) is a premenopausal morphotype. With age, the thickness of the glandular layer gradually decreases and the proportion of adipose tissue increases.
With the onset of menstruation, under the influence of sex hormones, cyclic changes occur in the mammary gland: 1-3 days - resorption of secretions from the ducts, 4-8 days - tubuloacinous involution (rest period), 9-16 days - proliferation of the ductal epithelium, hypervascularization of connective tissue, 17 Day 28 - acinar proliferation, glandular hyperplasia and a gradual decrease in connective tissue vascularization. In the second phase of the cycle, in response to the secretion of progesterone, the milk ducts and blood vessels of the parenchyma dilate.
Drawing. Echostructure of the mammary gland in phases I and II of the cycle: in phase II, Durette's ridges and Cooper's ligaments are emphasized, as the surrounding adipose tissue accumulates fluid and makes the image more contrasting, and tubular anechoic structures also appear - galactaphores of the 2-3rd order accumulate the secretory component.
At the end of pregnancy, the mammary gland acquires a large mesh structure due to the development of glandular tissue. With hypogalactia, the mesh pattern is preserved; with well-defined lactation, the mammary gland loses its mesh structure and represents a zone of reduced echogenicity, against which dilated ducts can be detected. In the areolar areas during lactation, groups of significantly dilated ducts are detected. After completion of lactation, the mesh structure of the mammary glands is restored again.
Drawing. On an ultrasound scan of the breasts of a nursing woman: pre- and retromammary fatty tissue is not expressed; the parenchyma is abundant, of reduced echogenicity, thin-walled anechoic tubular structures are identified - dilated ducts (1); milk sacs in the nipple area (2, 3).
At the age of 40-50 years, there is an increase in the proportion of adipose tissue, a decrease in the degree of development of the glandular tree, and the number of glandular lobules. At the age of 50-60 years, compared with the previous period, no significant changes in the structure were detected, but attention is drawn to the intensification of the processes of fibrosis of the intralobular stroma. At 60-70 years of age, the mammary gland is represented by fatty lobes that have low echogenicity, against the background of which stringy structures of high echogenicity are determined, which are thinned glandular tissue and compacted supporting stroma, located in the mass of adipose tissue.
The mammary gland is under compression due to endoprosthetics.
Breast skin
Breast fat
Accessory mammary glands on ultrasound
Often in the armpit area, in rare cases, additional breast tissue may be located on the face, neck, chest, back, buttocks and limbs. Scattered glandular tissue without an excretory duct is called an accessory lobe, and the formed structure with an areola and nipple is an accessory gland.
Accessory nipples can easily be confused with birthmarks. During puberty or pregnancy, pigmentation increases, swelling and even lactation appear. Tumors, mastitis and fibrocystic changes can form here. In rare cases, the inconvenient additional tissue is removed.
Benign formations on ultrasound of the mammary glands
Benign breast formations are divided into cystic and solid.
Breast cysts are:
Often cysts are a component of fibrocystic mastopathy (dysplasia) of the mammary glands. Fibrocystic mastopathy is the most detected condition during ultrasound of the mammary glands in women of reproductive age. The reason for seeking an ultrasound of the mammary glands is most often pain. In case of mastopathy, a characteristic sign of ultrasound of the mammary glands is compaction of the connective tissue, moderate dilation of the ducts of the mammary glands, and the presence of small cysts. These manifestations are completely individual for each woman.
Solid benign formations on ultrasound of the mammary glands:
- Breast fibroadenoma is a benign tumor of the breast.
- Galactocele is a formation associated with the accumulation of secretions from the mammary gland ducts.
- Breast abscess formation of purulent-inflammatory origin. Etc.
How to eliminate pathology
In some cases, the expansion is normal and reversible, and then only monitoring of the condition will be required, involving regular examinations by a mammologist. If the diameter is increased to 8 mm or more, and ectasia is caused by pathologies, then medical attention will be required.
Therapy, depending on the causes of the problem, may include the following:
- Antibiotics may be recommended for tissue infections.
- In case of hormonal imbalances, doctors often prescribe hormonal drugs, not only for oral administration, but also local ones, for example, creams or gels applied directly to the chest.
- For neoplasms, surgery will be required, which may involve removal of the tumor or complete excision of the affected duct.
Dilation of the breast ducts can be either a normal or a pathological condition, but in any case you should consult a doctor to avoid undesirable consequences.
When to do a breast ultrasound
Ultrasound of the mammary glands is recommended to be performed on certain days of the menstrual cycle if the woman does not use hormonal contraceptives and is not in menopause. Breast cyst
Cycle days for breast ultrasound from 8 to 14 are the most preferable. If a woman no longer menstruates, or she uses hormonal contraception of any kind, the day of the cycle for performing an ultrasound of the mammary glands does not matter.
Read more Scaly spots appeared on my head, what are they?
Symptoms that require an ultrasound of the mammary glands:
- Pain in the mammary gland, associated or not associated with the menstrual cycle.
- Breast injury.
- Changes in the color, density, appearance of the skin of the breast, the appearance of retracted areas on the mammary gland, including when the nipple is retracted.
- If a lump or lumps are detected during self-examination of the mammary glands.
- Enlargement of one or both mammary glands.
- Enlarged axillary lymph nodes.
- Genetic predisposition to benign or malignant breast formations.
- Detection of gynecological pathology, for example, during ultrasound of the uterus, ultrasound of the ovaries (transvaginal ultrasound), in the presence of cervical dysplasia, cervical erosion. This is due to the fact that the female reproductive organs (uterus, appendages) in their work, as well as the mammary glands, are highly sensitive to hormonal changes and together can demonstrate this clearly in the form of a combined pathology of these organs.
Symptoms of pathology and diagnostic techniques
Clinical symptoms of breast ductectomy are quite widely described in the specialized literature, so diagnosing the disease does not cause difficulties. First of all, this is the age of the patient. If a woman aged 40-45 years old, during an examination of the mammary gland, is diagnosed with a lump in the area of the areola and nipple, and yellow or dirty brown discharge is observed, we can confidently speak about the development of ductectasia of the mammary gland.
Often patients note itching and burning in the nipple area; the nipple itself takes on a retracted shape and moves away from its main axis. The skin of the breast becomes hyperemic, swollen, and pain is possible, which intensifies before menstruation.
It should be remembered that dilation of the milk ducts is not a separate pathological process, but becomes an integral part of another disease of the mammary gland.
Basically, there is no threat to the woman’s life and health, but constant discomfort in the area of the nipple and areola of the affected breast causes discomfort and some physical suffering to patients.
We must not forget about the psychological aspect of the problem. Any pathology in the mammary glands causes fear of breast cancer in patients, which can lead to serious mental disorders.
Diagnostic measures for suspected breast ductectasia are as follows:
- Primary examination of the mammary glands.
- Carrying out mammography and ultrasound of the breast.
- Cytological laboratory examination of discharge from the nipple of the affected breast.
- Fine needle puncture of the breast for the purpose of biopsy.
All these methods allow specialists to differentiate the problem as benign or malignant. Benign processes in breast ductectasia include the presence of polyps or intraductal papillomas in the patient. Moreover, strictly speaking, a bleeding mammary gland or bloody discharge from the nipples is most often caused by intraductal papilloma, although in 15% of cases the cause of such pathology is breast carcinoma.
Modern non-invasive techniques for examining the affected female breast using ionizing radiation provide great assistance in establishing the correct diagnosis for dilated mammary ducts.
Preparing for breast ultrasound
No special training required. Preventive examination of the mammary glands is carried out in the first phase of the cycle. If the alarming symptoms listed above are detected, an ultrasound of the mammary glands is performed as soon as possible.
Ultrasound of the mammary glands is recommended for all women without exception once a year as a preventive screening. Ultrasound of the mammary glands is an absolutely safe and informative form of diagnosing the condition of the mammary gland and eliminating the risk of breast cancer. The age range for using breast ultrasound to exclude breast cancer is no longer limited to 35-year-old women with the advent of high-resolution equipment with elastography effect and sensitive duplex scanning of blood vessels. Elastography allows for differential diagnosis of formations based on their density and displacement in women of any age. Our clinic has a modern ultrasound scanner with elastography, which allows us to perform ultrasound diagnostics of the mammary glands in the most informative and high-quality manner.
LLC "Medical © 2020 – 2019
All iLive content is reviewed by medical experts to ensure it is as accurate and factual as possible.
We have strict sourcing guidelines and only link to reputable sites, academic research institutions and, where possible, proven medical studies. Please note that the numbers in parentheses ([1], [2], etc.) are clickable links to such studies.
If you believe that any of our content is inaccurate, out of date, or otherwise questionable, please select it and press Ctrl + Enter.
Progressive dilated mammary duct is not a very common, but quite dangerous condition. Inflammation easily begins in the dilated ducts, various bacteria and pathogenic microorganisms accumulate in them, and painful discharge from the mammary glands appears.
This phenomenon is more often observed in premenopausal patients, as well as during pregnancy and breastfeeding - in such cases, expansion is considered a natural phenomenon. However, sometimes this may indicate the initial stage of development of certain breast diseases. We will tell you about the causes and possible treatment in this article.
[1], [2], [3], [4], [5]
Causes
Most often, ectasia develops in women of premenopausal age (45-50 years), but it can also occur after the physiological cessation of menstruation. Infants and children of primary school age (in the prepubertal period) are much less likely to suffer, both girls and boys. In children, one mammary gland is affected; in adults, there is also a bilateral process.
The main causes of dilation of the mammary gland ducts are previous breast trauma or an inflammatory process (mastitis). As a result of mechanical damage, the glandular lobules are deformed, which leads to radial (circular) expansion of the ducts in the nipple area. A similar mechanism is observed after mastitis. In this case, the factor leading to deformation of the ducts is the proliferation of connective tissue. It occurs as a result of the replacement of inflamed glands with cells that resemble scar cells in nature.
Ectasia of the milk ducts can occur against the background of other diseases of the female reproductive system. This is ovarian pathology (polycystic disease, endometriosis, chronic salpingoophoritis), fibrocystic disease of the mammary glands (mastopathy), intraductal tumor, Paget's gland cancer.
Periductal mastitis occurs infrequently in young women. Its cause is stagnation of colostrum at the beginning of lactation.
Among the provoking factors:
- smoking;
- pituitary adenoma;
- increased levels of the hormone prolactin in the blood, which occurs against the background of hypothyroidism, liver and kidney failure, increased secretion of estrogen in the ovaries.
There is also an association between the development of the disease and low weight, as well as rapid growth in childhood, drinking alcohol before the first birth, consuming more than 3 servings of meat products per day in adolescents, and taking female sex hormones for more than 8 years.
No association with breastfeeding (or lack thereof) was found.
Causes of dilated mammary duct
The reasons for this diagnosis must be sought in changes in the balance of hormones within the female body, therefore the level of the disease is higher during menopause and in the initial stages of menopause.
In addition, natural expansion of the ducts may occur:
- during pregnancy and lactation;
- with hormonal changes in the second phase of the monthly cycle.
The last listed reasons are considered a natural physiological process in the female body. For this reason, it is advisable to carry out an ultrasound examination of the breast no later than from the sixth to tenth day of the monthly cycle.
In pregnant and lactating women, dilated mammary duct in most cases is a natural phenomenon that does not require any treatment.
Dilated ducts, as a pathology, are considered in the presence of an inflammatory reaction in the nipple area, with the appearance of cracks in the nipples and the nipple area, and with intraductal mastitis.
A locally dilated mammary duct is observed against the background of fibrocystic (nodular or diffuse) mastopathy, when papillary growths form inside the duct.
However, the pathogenesis and some aspects of the etiology of dilated ducts still remain unstudied, there is no systematization of this disorder, and a clear pathogenetic connection between the state of hormonal dysfunction and the appearance of intraductal dilatation has not been proven. Moreover, most experts do not classify dilated ducts as a disease - it is usually just a sign that is used to describe the results of a breast ultrasound.
[6], [7]
Forms of ectasia
At its core, the disease has similar symptoms to mastitis. But the forms or types of ectasia are different, it all depends on what became the root cause of the disease and led to its development.
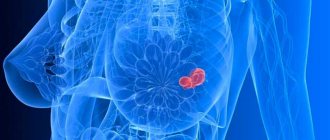
Often, dilation of the ducts is associated with the development of a tumor in the area of the mammary ducts. The formation compresses the duct, leads to deformation of the walls and causes expansion.
A tumor or neoplasm can be either benign or malignant. For this reason, ectasia is often a sign of cancer. In any case, you should not ignore the appearance of unpleasant symptoms.
So, the main types of ectasia:
- Hormonal - caused by a violation of the stability of hormonal levels. It is more often diagnosed in middle-aged patients (over 40 years old). But it can also be detected in younger patients if there is an imbalance in the body.
- Natural - a condition when dilation of the ducts occurs during pregnancy or lactation and does not entail any consequences
- Oncological - diagnosed if there is a cancerous tumor in the ducts of the gland. It closes the passage and leads to deformation, resulting in ectasia.
Attention! Often the disease is associated with endocrine disorders in a woman’s body. It can be diagnosed in the presence of diabetes mellitus.
If the root cause of the disease cannot be determined, a number of additional diagnostic procedures are performed.
Symptoms of a dilated mammary duct
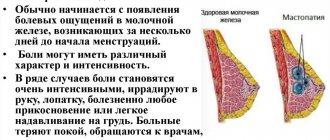
Typically, the following symptoms indicate possible dilation of the ducts:
- the appearance of discharge from the ducts;
- feeling of soreness in the mammary glands;
- swelling, hyperemia in the peripapillary area;
- itching sensation in the nipple area;
- nipple retraction.
The first signs of a disorder can appear at different periods of a woman’s life. Typically, the following symptoms may indicate the presence of enlargement:
- feeling of constant discomfort in the chest area, mainly closer to the nipple area;
- discharge from the nipples, and in advanced cases – signs of intraductal inflammation;
- slight pain (not always).
If such signs appear, you should consult a doctor for a more thorough diagnosis.
[8], [9], [10], [11]
Complications and consequences
The dilated duct itself is not dangerous, but requires constant monitoring. Therefore, regular visits to a mammologist with ultrasound or mammography are mandatory.
If this sign is ignored, then various not entirely pleasant complications may appear:
- mastopathy, mastitis - develop as a result of infection in the dilated ducts;
- ectasia is a process in which the expansion begins to progress, over time causing inflammatory reactions and the appearance of pathological discharge from the nipples;
- the development of cysts is a pathology characterized by the fact that in the expanded lumen of the ducts there is an accumulation of secretions, which take the form of a capsule and are subsequently transformed into a cyst;
- the development of papillomas is a dangerous process, reminiscent of the formation of cysts, which, however, can subsequently become malignant (malignantly degenerate).
Read more Method of propagation of malarial plasmodium
It is precisely because of the possible appearance of additional diseases that the dilated duct requires constant supervision by a specialist in order to promptly identify and treat the emerging pathology.
[21], [22], [23], [24], [25], [26], [27]
Reasons for the development of the disease
The risk zone includes women whose age has approached menopause. Age-related hormonal changes contribute to the development of pathology. The ducts are located in the alveoli of the chest. Normally, the milky ways have a narrow, winding structure. All paths unite and exit to the nipple. The onset of a dangerous disease can begin suddenly. Among the causes of dilated mammary ducts, a distinction is made between natural and pathological.
Natural causes include:
- premenstrual period
- gestation
- menopause
During menstruation, the female body undergoes certain changes. The breasts swell, become especially sensitive and painful when touched, as during mastitis. The body is on the eve of fertilization, so the milk ducts undergo certain minor changes. If pregnancy does not occur, the mammary duct narrows and its structures return to normal.
When conception occurs and the further development of the embryo, the woman’s body begins to prepare for lactation after childbirth. Throughout pregnancy, the mammary glands increase in size, and the ducts expand for better milk flow. Only after breastfeeding is completed, the mammary ducts begin to narrow. The process of feeding a baby milk should be reduced gradually. It is important to express the remaining milk to prevent lactostasis.
With hormonal changes during menopause, the structures of the mammary gland also undergo certain changes. Due to hormonal imbalance, dilatation of the duct occurs. This phenomenon is not pathological, but requires careful monitoring. A woman during menopause needs to undergo regular examinations, breast ultrasound and mammograms. Preventive examinations with a mammologist and gynecologist will allow you to promptly notice the pathology and begin to treat it.
Among the pathological factors for dilatation of the ducts:
- ectasia
- development of mastopathy
- presence of a cyst
- inflammatory process
- formation of neoplasms
A characteristic sign of mastopathy is an increased amount of estrogen. This is what provokes an increase in the structure of the mammary gland and the expansion of its ducts. Large amounts of fluid can also accumulate in the ducts. This leads to the formation of cysts and tumors.
Diagnosis of dilated mammary duct
Diagnosis is carried out primarily based on existing symptoms:
- the patient complains of discomfort and minor pain;
- the nipple can be retracted (when the isola is pinched between two fingers, the nipple is hidden inward);
- there is slight swelling around the nipple, redness, and discharge may be present.
Further, additional diagnostic methods may be prescribed to clarify the diagnosis:
- tests (examination of discharge from the ducts, blood testing for hormonal status);
- Instrumental diagnostics (ultrasound examination, ductography, mammography);
- immunohistochemical analysis of an element of gland tissue.
The latter analysis is a study of a small element of a biopsy (or material removed during surgery), which is carried out to exclude a malignant disease.
If the ducts are dilated on an ultrasound of the mammary glands, then this is not a reason for concern. Normally, the ducts should be about 0.5-1 mm, a slight expansion is allowed during the lactation period, after the lactation period, before the onset of menopause. In other cases, an enlarged duct also does not indicate any pathology, but may only indicate a tendency to its occurrence.
[28], [29], [30], [31], [32], [33], [34]
Diagnostics
The first stage of diagnosis is examination and palpation of the breast. At the same time, discharge from the breast is assessed.
When appropriate symptoms are identified, diagnostic studies are aimed primarily at excluding a malignant tumor:
- Ultrasound of the mammary glands - prescribed for women under 40 years of age.
- Mammography is informative in patients over 40.
- In women under 40 years of age, if ultrasound is not informative, it is possible to use breast MRI, which provides accurate information about minor anatomical changes (in particular, local dilation of the mammary duct is diagnosed).
- Ductography is an X-ray examination of the ducts after the introduction of a contrast agent into them; it is prescribed if a malignant tumor is suspected; before it, a cytological examination of the discharge is necessary to detect cancer cells.
- In unclear cases, a biopsy is prescribed.
A biopsy is performed using a thin or hollow needle through which a small amount of material is withdrawn. Such a study is necessary to obtain a sample of altered tissue and examine it microscopically (histologically). It is usually performed under ultrasound guidance.
If bacterial inflammation is suspected, a microbiological examination of nipple discharge is prescribed. It helps determine which pathogens caused the disease and which antibiotics they are sensitive to.
Differential diagnosis
Ectasia of the milk ducts must be differentiated from diseases of the mammary glands such as:
- Mastitis. Characterized by throbbing, shooting, bursting pain, swelling, increased skin temperature, redness of the gland. When palpated, a rounded cavity is determined, initially dense, then it softens.
- Fibroadenoma. A round or oval formation is determined in the gland tissue, dense, with a smooth surface, easily movable when palpated, painless.
- Cyst. The formation is round or irregular in shape with a smooth contour, moderately painful.
- Tuberculosis. An uneven, painless lump may be accompanied by nipple retraction, characterized by enlarged axillary lymph nodes, a constant increase in body temperature, and night sweats.
- Paget's cancer. Differential diagnosis is carried out using additional research methods - ultrasound/mammography, biopsy.
- Pituitary adenoma. If there is constant discharge from the nipples, an MRI or x-ray of the sella turcica area in the brain is necessary.
Treatment of dilated mammary duct
Since dilation of the milk ducts is not considered a pathology as such, conservative and especially surgical treatment is not necessary. However, attention should be paid to the causes of this condition and concomitant diseases of the reproductive system.
For example, if during an ultrasound examination the doctor discovered a pronounced expansion of the lumen in the ducts, then, first of all, it is important to check the state of hormones in the body. The doctor will analyze the level of prolactin, estrogen and thyroid hormones, after which he may prescribe treatment aimed at normalizing the hormonal balance.
If the reasons for the increase in the diameter of the ducts are inflammatory reactions, and the tests performed indicate the presence of infection, then antibiotic therapy is prescribed. Often such treatment is carried out against the background of anti-inflammatory, immunocorrective and restorative treatment.
If the expansion is associated with age-related changes in the body, then a wait-and-see approach is used - the doctor monitors the condition of the epithelial tissue lining the milk ducts, monitors the appearance of discharge and other symptoms. If the process of inflammation develops, then most often they resort to surgical intervention.
In most cases, intraductal cystic formations are not removed. Surgical treatment is indicated only when there is a malignant process, or the cyst appears in the same place repeatedly.
A diagnosed papilloma is usually removed due to the high likelihood of the tumor becoming malignant.
Homeopathy
Homeopathic medicines are used not so much for treatment as for the prevention of complications during the expansion of the milk canals. The decision on the advisability of prescribing homeopathic remedies is made only by the doctor, based on the results of tests and studies.
- Cyclodinone is a drug that normalizes the level of sex hormones, restores the amount of prolactin, which at the same time has a positive effect on the condition of the mammary gland.
- Mastodinon is a herbal preparation that normalizes prolactin production, thereby stopping the development of diffuse forms of mastopathy.
- Viburkol is a remedy that eliminates pain, inflammation, spasms, including in the reproductive system.
- Gynekohel is a complex herbal preparation that normalizes the functional ability of the female reproductive system. It is used for infectious and inflammatory processes in the reproductive sphere, for age-related and other disorders of the monthly cycle.
- Dysmenorm is a complex homeopathic remedy that eliminates hormonal dysfunction in women of any age. Normalizes the ratio of estrogen and progesterone.
- Klimaktoplan is a homeopathic medicine that is used in the premenopausal and menopausal periods. Stabilizes hormonal levels in the adrenal cortex, pituitary gland and appendages.
Dilation of the ducts: normal or pathological
If the milk duct of the breast is dilated, then in medicine this condition is called ectasia. First, it’s worth finding out how much the diameter of one structural element should be. Normally, it varies from 1.5-2 to 3 mm. But in some cases the figure may increase. Sometimes, if the milk ducts are dilated, this is a variant of the norm and is caused by natural physiological processes occurring in the body. But sometimes an increase (especially up to 5-8 mm or more) is regarded as a pathology, is provoked by certain disorders or diseases and requires medical attention.
Acceptable and normal ectasia may be due to the following reasons:
- Hormonal changes observed in the second phase of the menstrual cycle. At this stage, the female body begins to produce an increased amount of progesterone, thus, as if preparing for a possible pregnancy. And this hormone triggers a number of processes, including the expansion of the milk ducts, but, as a rule, it is insignificant.
- Pregnancy. During this important period, progesterone continues to be produced by the woman’s body, and in increased volumes compared to the usual state. And due to the increased synthesis of this hormone, the ducts expand, preparing for the upcoming breastfeeding.
- Lactation. At this stage, the ducts perform very important functions, namely, they ensure the transport of milk produced in the gland to the openings located in the nipples. And if milk is synthesized in increased volumes or does not have time to leave the breast, this can provoke ectasia. Expansion is usually observed immediately during breastfeeding and for some time after its completion, then the breast structure gradually becomes the same as it was before pregnancy.
- Menopause or menopause. During these periods, hormonal changes are inevitable and irreversible, so dilation of the ducts often occurs in women over 45 years of age.
Pathological causes of dilation of the milk ducts:
- The ducts can dilate due to mastopathy, in which there is often an increased synthesis of progesterone, which has a direct effect on the structure and diameter of the ducts.
- An increase in diameter to 8 mm or more can be caused by neoplasms localized in the ducts. Usually they are benign in nature, and these include cysts, papillomas, and polyps. But there is such a disease as intraductal cancer, and with it ectasia also occurs.
- Inflammatory processes affecting the milk ducts. Thus, expansion can develop with mastitis - inflammation of the glandular tissue.
- Various chest injuries.
- Previous operations on the mammary glands.