Indications for use
IgG antibodies are important for diagnosing many diseases. The analysis is prescribed for the following purposes:
- assessment of the ability of local immunity to quickly respond to antigens;
- establishing the causes of common viral and infectious diseases;
- determination of immunodeficiency and its degree;
- assessment of the state of the immune system when identifying autoimmune diseases;
- determination of blood composition in the diagnosis of hematological problems;
- dynamics of myeloma;
- determination of the effectiveness of replacement therapy with immunoglobulin preparations.
Blood tests for antibodies help determine the presence of the virus in the blood and the degree of its activity. Tests are necessary for immunocompromised individuals. These include:
- pregnant women;
- cancer patients;
- HIV-infected people;
- patients who have undergone an organ transplant;
- people who often suffer from viral diseases or have had them (rubella, hepatitis).
| Age category | Floor | IgG, g/l |
| Newborns up to 1 month inclusive | Boy | 3,97 – 17,65 |
| Girl | 3,91 – 17,37 | |
| Children under one year old | Boy | 2,05 – 9,48 |
| Girl | 2,03 – 9,34 | |
| Children 1-2 years old | Boy | 4,75 – 12,1 |
| Girl | 4,83 – 12,26 | |
| Children over 2 years old and adults up to 80 years old | Boy/Man | 5,4 – 18,22 |
| Girl/Woman | 5,52 – 16,31 |
Errors in the results of antibody tests do occur. The following factors can distort the data:
- smoking, alcohol, drugs;
- excessive anxiety, constant stress;
- intense sports training;
- radiation exposure;
- large loss of proteins due to diseases of the intestines, liver, kidneys;
- burns covering more than 40% of the body surface.
Antibody test results are affected by medications taken. These include:
- means to enhance immunity, used for a long time;
- hormonal drugs (oral contraceptives, estrogen);
- artificial immune suppressants;
- gold preparations (Aurothiomalate);
- cytostatics (Fluorouracil, Cyclophosphamide);
- Carbamazepine, Methylprednisolone, Valproic acid, Phenytoin.
The analysis allows us to monitor the dynamics of the development of certain pathologies. The study helps determine why globulins are decreased or increased, what this means, and what to do about it in the future.
A test for antibodies in the blood will be carried out if a deficiency of immunoglobulins is suspected. Their deficiency causes weakened immunity and the development of secondary immunodeficiency.
A test for immunoglobulin levels may be prescribed for the following pathologies:
- the amount of antibodies to TPO (thyroid peroxidase directed against thyroid cells) makes it possible to determine thyroid pathologies of autoimmune origin;
- hepatitis of various types;
- immunodeficiency virus - the test is prescribed 3 times, after which a diagnosis can be made;
- diphtheria, tetanus;
- chlamydia, herpes, syphilis;
- leptospirosis, cytomegalovirus, ureaplasmosis.
There are also general indications:
- recurrent infectious diseases;
- weak immunity, which is manifested by frequent illnesses, poor health, problems with nails and hair;
- severe systemic diseases of any origin;
- persistent inflammatory diseases of the oral mucosa - stomatitis, gingivitis, periodontitis;
- skin rash of unknown origin, the appearance of ulcers on the oral mucosa and genital organs;
- male autoimmune infertility;
- preparation for surgery;
- postoperative recovery;
- undergoing immunoglobulin therapy.
Antibodies in the blood are elevated: what does this mean?
If antibodies are elevated, this means the presence of an infection, exacerbation of inflammation, or an autoimmune disease. If Rh antibodies are not detected in a pregnant woman, then there is no threat to the child. The mere presence of immunoglobulins in the blood does not mean the development of the disease; the analysis is assessed by a doctor.
Possible pathologies
If antibodies in the blood are elevated, this may indicate:
- current infectious process;
- previous illness, injury, surgery;
- exacerbation of chronic inflammation;
- tumor;
- allergic reaction;
- autoimmune disease.
Watch the video about the reasons for increased antibodies during pregnancy:
If Rh antibodies are not detected
Rh antibodies mean that there is a conflict between the positive Rh factor of the fetus and the negative Rh factor of the pregnant woman; when they are not detected, there is no danger to the child. When they appear in the blood there are risks:
- destruction of red blood cells, anemia, jaundice in a newborn;
- intrauterine growth and development delays;
- stillbirths;
- early miscarriage;
- enlarged spleen and liver.
If I have antibodies, will I definitely get sick?
Antibodies are a protective reaction, so if they are present, the risk of disease is lower. Their appearance in the blood reflects the functioning of the immune system. They show existing contact with a foreign protein (virus, microbe, allergen, toxin). A blood test can only determine the type of antigen and how the body responded to it. The main criterion for diagnosis will be clinical symptoms.
Indications for use
Antibodies (AT) are cells of the immune system that can recognize and destroy foreign microorganisms, including viruses, toxic components and bacteria. Their main task is to perform the protective function of the body. At their core, antibodies are proteins formed from white blood cells.
During pregnancy, ATs can be produced against the fetus itself, since it contains genes from the father that are foreign to the mother's body. Most often, this happens when the Rh factor and blood group are incompatible. There are several types of antibodies, each of which belongs to one of 5 classes of immunoglobulins: IgA, IgE, IgM, IgG, IgD.
Each of these subspecies is responsible for a specific function. Thanks to AT testing, it is possible to identify a fungal, viral or bacterial infection. Based on the amount of proteins in the blood serum, we can conclude whether such changes are a protective reaction or whether the body is fighting an infection.
The analysis also makes it possible to determine whether medications are required to combat the disease or whether the immune system can cope on its own. The study also allows us to identify the stage of the disease and predict the further course.
If a woman was already pregnant, but had a miscarriage, an analysis is prescribed to determine the antibodies to the partner’s sperm. Often, fetal rejection occurs precisely because ATs perceive it as a foreign object and turn on the protective forces of the immune system.
What are antibodies
Antibodies are immunoglobulins or globulins that are produced by the immune system to identify and destroy harmful and pathogenic microorganisms. But their production is not always aimed at protecting against various types of pathogens. In various pathologies and autoimmune diseases, they can attack healthy tissues of the body. A blood test for antibodies helps identify what exactly the patient is facing.
The formation of specific proteins in human blood begins only in the following cases:
- the body is attacked by harmful agents leading to further infection;
- during vaccination (introduction of artificially weakened bacteria into the body).
The development of immune memory is the most important process for humans, in which globulins remember antigens with antibodies attached to them. If they enter the body again, the immune system can neutralize them. Doctors warn that the presence of antibodies in blood serum is the most important indicator of the state of the immune system. Any deviations from reference values indicate the development of pathology.
How to get tested during pregnancy?
During pregnancy, all women need to be tested for antibodies. This will help:
- Determine whether the mother has developed immunity to diseases that are dangerous to the health of the fetus;
- Provide adjustments to the health of a pregnant woman with a tendency to thrombosis;
- Detect a conflict between the Rh factors of mother and child.
To prepare for the test in the days leading up to it:
- Avoid fatty and salty foods. Eliminate coffee and carbonated drinks;
- Avoid taking medications. In cases where this is not possible, the laboratory and the treating gynecologist must know what exactly you are taking;
- Take the test itself in the morning, on an empty stomach.
Various deviations from the norm in the body of a pregnant woman can become critically dangerous for her unborn child. Whereas a timely detected violation will be stopped, and you will be able to carry and give birth to a healthy baby under the supervision of a doctor.
The number of antibodies is determined by testing the serum. This analysis allows you to assess immunity, confirm or refute the presence of an infectious or parasitic disease.
Based on which globulins are detected in the blood, a specialist can make a diagnosis and determine the period of pathology. So, when class G is detected, a specialist can judge the presence of fungi, viruses and toxins secreted by various microorganisms.
It is G globulins that form immunity that prevents re-infection with already suffered diseases. Also, these immune proteins are responsible for the formation of protection during the period of intrauterine formation.
Venous blood is taken to determine specific proteins. The procedure is performed on an empty stomach. When preparing for the analysis, you should avoid alcoholic beverages. Blood can be collected only 4 hours after eating if the test is scheduled during the daytime.
A test aimed at determining antibody levels is called an immunofluorescence test or ELISA. The antigen and antibody are attached to each other, then a special substance is added to the material that stains these immune complexes. The color determines the concentration of immune proteins in the blood.
ELISA is highly specific and gives the correct result even in the presence of a small number of immune complexes. You will need to wait about 2 days to receive results. An urgent conclusion can be obtained within a few hours.
You can donate blood to determine the quantitative indicator of immune proteins in a diagnostic laboratory. It is better to choose a clinic located close to home, because the journey will be stressful, which may affect the test results.
DETAILS: Blood groups transfusion compatibility table
The cost on average varies from 370 to 600 rubles. In this case, the type of research is taken into account, because the price differs significantly when conducting an analysis for Torch infections, determining Rh antibodies, and identifying individual pathogens.
Detection of Torch infections, which is prescribed during pregnancy planning, will cost 2,500 rubles. For certain specific infections it will cost no more than 600 and no less than 350 rubles. The cost of the blood draw itself is also taken into account, which in clinics varies from 100 to 200 rubles.
You can undergo a study as prescribed by a doctor or at your own request in order to find out the presence of a particular infection. For the results to be reliable, it is important to follow the preparation rules. An important condition will be to inform the doctor about the medications you are taking in the last days before the procedure. You also need to report on your well-being, quality of sleep and nutrition on the eve of the study.
Why is analysis needed, how to decipher
Immunoglobulins (antibodies) are detected to exclude or confirm the presence of the disease. The concentration of protein cells-agents to the desired infection allows you to determine the diagnosis.
Such a study is also carried out after a vaccine or course of treatment. The test shows how the medical procedures you have undergone have affected your immune system. This analysis also determines the success of therapy.
Antibodies come in three types:
- IgG is an immunoglobulin for the destruction of harmful microorganisms. If there are no IgM bodies, the antigen is not active;
- IgM - occur at the first, acute stage of infection. If only these agents are present, the infection is recent;
- IgA - residual after a previous pathology or virus (in the absence of others), is found in the chronic form of the disease. Such immunoglobulins are detected in the first six months in healthy children whose parents have hepatitis virus;
- IgE – antibodies produced during allergies, acute respiratory viral infections, and other colds.
The result of the study, regardless of the substances sought, is always of two types:
- Positive – there are protective agents. The subject is sick or infected (already cured) with an infection or virus.
- Negative – the requested antibodies are not produced, the person is healthy.
If the result is confirmatory, the concentration of immunoglobulins is often indicated. This indicator means the degree of pathology, its severity. The more antibodies, the higher the activity of the antigen. In the laboratory they also look at the predominance of some antibodies over others, their combination or complete absence.
So, if there are IgA and IgM bodies, the disease is aggravated and intensified. Timely medical assistance is required.
A doctor can interpret the study correctly.
All factors on the basis of which the diagnosis is made are taken into account:
- Patient's condition.
- Symptoms or lack thereof.
- Other studies.
If the test shows the same result on the second visit, you need to go to a therapist, infectious disease specialist and other specialized doctors. Only a specialist will prescribe the necessary treatment. You cannot self-medicate.
False positive result
It happens that the test gives an affirmative answer, but the person is not sick. Therefore, you should not panic right away. This phenomenon happens when:
- A woman is carrying a child - changes in hormonal levels cause deviations of some indicators from the norm.
- Critical days - the body experiences stress and heavy blood loss, which is why “protector” cells are often produced.
- A person has an autoimmune disease that is not related to the one being sought - that is, the test looks for some substances, but finds others, which it stops at.
- Presence of oncology, neoplasms.
If the analysis shows antibodies, it is worth double-checking by donating blood again. It is advisable to do this in another place.
The error may have occurred as a result of the laboratory's actions:
- insufficient competence of the researcher;
- improper storage of the blood sample being analyzed;
- accidental substitution of submitted material;
- incorrectly conducted research.
Having seen a positive result on the document provided, there is no need to panic ahead of time. Compare all factors and retake the analysis. This will help verify the accuracy of the previous study or refute its conclusion.
It is possible that you have already had the infection and have developed immunity to it.
In some cases, more comprehensive tests to determine pathology may be necessary.
This usually applies to viral infections such as:
- viral hepatitis;
- human immunodeficiency virus of both stages;
- sexually transmitted infections.
Group antibody analysis
Another important test for pregnant women is blood testing for antibody titers. The risk of developing Rh conflict is present only if the woman has a negative Rh (Rh factor) and the baby is positive. In this case, the likelihood of the absence of Rh conflict is present only during the primary pregnancy, since during the first pregnancy, anti-D bodies are usually produced in insufficient quantities.
During the second and third pregnancies, the risk of developing anti-Rhesus antibodies increases, which increases the likelihood of the baby's death. It is worth considering that a conflict in the AB0 system can develop even during primary pregnancy. But this only happens if fetal blood, incompatible with maternal blood, enters the woman’s bloodstream in large quantities.
This reaction is due to the fact that in this case the production of anti-group antibodies is activated. Most often, this violation does not lead to dangerous consequences and deviations, but in any case, the woman will have to be constantly monitored by a doctor to minimize the likelihood of complications.
The following factors can provoke the occurrence of group antibodies or Rh conflict:
- late termination of pregnancy;
- prematurity;
- transfusion of inappropriate blood into the body;
- previous births accompanied by multiple complications;
- placental abruption;
- ectopic pregnancy (with incompatible Rh in the fetus).
Currently, there are many preventative methods to prevent complications due to Rhesus conflict. If you are regularly examined by a doctor, the risk of complications will be low.
It is recommended to donate blood for antibody titers even before conception. This will allow you to find out in advance whether the Rh factor of the parents is compatible
To whom and why is a test for antibodies to CMV prescribed?
The analysis is indicated for those individuals who are at risk of developing infection:
- pregnant women (mandatory screening);
- premature newborns;
- patients who have received a blood transfusion;
- patients who have been diagnosed with oncology, blood diseases, AIDS, HIV, immunodeficiency states of various nature;
- medical workers.
In healthy people with strong immunity, primary infection is often asymptomatic and without complications. But CMV in active form is dangerous in case of immunodeficiency and pregnancy, as it causes numerous complications. Therefore, doctors recommend undergoing examination before the planned conception of a child.
Decoding the results
Each class of immunoglobulins has its own blood levels.
Thus, the normal level of IgA antibodies for children under the age of twelve is: 0.16-2.6 g/l, for adults – 0.35-3.55 g/l.
If the level of these antibodies exceeds normal values, then the doctor may suspect tuberculosis, cystic fibrosis, chronic hepatitis, cirrhosis of the liver, rheumatoid arthritis, chronic purulent infections of the gastrointestinal tract.
A decrease in IgA levels may indicate atopic dermatitis, pernicious anemia, radiation exposure, or result from taking certain medications.
The normal values of IgG antibodies are as follows: for children under 10 years of age - 7.4-13.6 g/l, for adults - 7.8-18.5 g/l.
Elevated levels of these immunoglobulins may indicate systemic lupus erythematosus, tuberculosis, sarcoidosis, rheumatoid arthritis, or the presence of HIV infection. A reduced level of antibodies is observed in allergic reactions, tumors of the lymphatic system, and hereditary muscular dystrophy.
IgM antibody content level: for children under ten years of age - 0.7-1.4 g/l, for women - 0.8-2.9 g/l, for men - 0.5-2.4 g/l l.
An increase in the level of these antibodies occurs in acute and chronic diseases of the respiratory and digestive system, parasitic diseases, lymphoma, gastroenteropathy, burns and intrauterine infections in newborns.
Knowing the norms for the content of certain antibodies in the body, you can independently judge whether the results of a blood test for immunoglobulins raise any concerns or not. But only a specialist should decipher a blood test for antibodies, since only a doctor can give a competent assessment of all additional factors and, based on a comprehensive picture, make the correct diagnosis.
An immunoglobulin blood test is performed to determine the number of globulins IgA, IgG, IgM. The norm will be different for children, women and men.
| IgA (g/l) | IgM (g/l) | IgG (g/l) | |
| Children | 0,15 — 2,5 | 0,8 — 1,6 | 7,2 — 13,4 |
| Women | 0,53 — 3,44 | 0,38 — 1,96 | 5,88 — 16,2 |
| Men | 1,02 — 4,05 | 0,55 — 1,43 | 6,63 — 14,01 |
IgA globulins are found on mucous membranes, in oral fluid, milk of a nursing woman, tears, bronchial secretions, and stomach. Their task will be to neutralize viral agents. Immunoglobulins of this class protect against pathogen entry through the respiratory system, excretory system and digestive tract.
What does the class A indicator indicate:
- Increased blood levels. It is observed in alcoholism, joint diseases, chronic pathologies of the hepatobiliary system, purulent infectious processes. High levels are also recorded in diseases of the gastrointestinal tract.
- A decrease in antibody titer - in case of blood diseases, pernicious anemia, dermatological pathologies, radiation exposure. Low levels are possible with long-term use of immunosuppressants. There is also a decrease in protein during treatment with cytostatics.
Class M globulins are the first to attack pathological microorganisms that enter the body. The IgM content in the blood serum increases at the beginning of the first month of the infectious disease. These globulins are found in plasma and neutralize viral and bacterial agents in the blood.
What does the M class level indicate:
- Increase in blood. A high level is determined in cases of intrauterine infections, parasitic pathologies, diseases of the respiratory system and gastrointestinal tract. An increase indicates a chronic course.
- Decreased blood levels. Indicates gastrointestinal diseases, lymphoma. Low levels are determined for people suffering from burns.
Class G globulins appear in bacterial infections and allergies.
What does the G class indicator indicate:
- Increase in blood. Occurs with systemic lupus erythematosus, tuberculosis, HIV, sarcoidosis, and joint diseases.
- Decreased immune proteins in the blood. It is observed in the case of muscular dystrophy (genetically determined), allergies, lymphadenitis and neoplasms of the lymphatic system.
Immunoglobulins are determined in the patient’s blood in accordance with their characteristics. The interpretation of the results is carried out by a highly qualified specialist, which allows for a correct diagnosis. IgA titers in a child aged 0 to 12 years should range from 0.16 to 2.6 g/l. In adult patients, the norm is from 0.35 to 3.56 g/l. If immunoglobulins are found in excessive quantities, this may indicate the development of:
- rheumatoid arthritis;
- tuberculosis;
- liver cirrhosis;
- cystic fibrosis;
- chronic hepatitis;
- purulent infections in the digestive system;
- respiratory or dermatological diseases.
If specific antibodies decrease significantly in quantity, this may indicate diseases such as pernicious anemia and atopic dermatitis. This condition occurs after exposure to radiation or taking certain medications.
The normal IgG value is from 7.8 to 18.5 in adults, from 7.4 to 13.5 in childhood. If the analysis shows an increase, then the patient is likely to develop tuberculosis, systemic lupus erythematosus, and sarcoidosis. Results may indicate HIV infection or rheumatoid arthritis.
DETAILS: Pressure 40 60
If the patient's age is less than 10 years, then the normal IgM level should be from 0.7 to 1.4 g/l. In adult men, the norm is considered to be from 0.5 to 2.4 g/l, and in women – from 0.8 to 2.9 g/l. If total antibodies increase, this indicates the occurrence of diseases in the digestive system that are chronic or acute in nature.
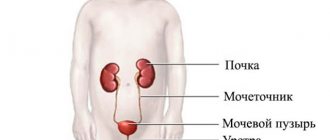
There are Rh antigens on the surface of red blood cells. About 20% of people are carriers of Rh negative antigen. This does not fall into the category of pathological processes. Concerns may arise only when pregnancy occurs in women with Rh-negative blood. This is explained by the fact that after the mother’s antibodies enter the child’s bloodstream, a Rh conflict may occur. It causes the development of diseases of the following organs and systems:
- brain;
- kidneys;
- liver.
To avoid serious complications, a pregnant woman should undergo regular antibody tests. In the first trimester, this procedure is performed once a month. Starting from the second trimester, a woman needs to donate blood once every 2 months. If concerns arise, a woman’s pregnancy should proceed under the supervision of specialists who can prescribe effective treatment.
IgE immunoglobulins give a reaction when infections and parasites enter the body. When their number increases, in most cases syphilis, cytomegalovirus, hepatitis, chlamydia, tetanus, diphtheria, leptospirosis and other infectious processes in the body are determined. Antibodies are special specific proteins that ensure the binding of infectious antigens.
What to do if IgG to CMV is positive?
Antibodies to cytomegalovirus detected in blood and other biological fluids may indicate three possible conditions: primary or re-infection, recovery and carriage of the virus. The test results require a comprehensive assessment.
If IgG is positive, then to determine the acute phase, which is the most dangerous to health, you need to consult an infectious disease doctor and conduct additional ELISA tests for IgM, IgA, avidity or PCR analysis.
If IgG is detected in a child under 1 year of age, it is recommended that the mother also undergo this examination. If approximately the same antibody titers are detected, then it is highly likely that simple transfer of immunoglobulins occurred during pregnancy, and not infection.
It should be taken into account that small amounts of IgM can be detected for 2 or more years. Therefore, their presence in the blood does not always indicate recent infection. In addition, the accuracy of even the best test systems can produce both false positive and false negative results.
Preparing for the study - how it is carried out
In order to determine antibodies in the human body, it is necessary to properly prepare for the analysis. Preparation consists of following a few simple rules:
- Before the examination, a person must follow a diet for several days. It is strictly forbidden to eat fried and fatty foods. A person should also avoid spicy and salty foods. The patient is strictly prohibited from drinking alcoholic, carbonated drinks and strong coffee during this period.
- The day before the examination, the person should avoid strong physical activity. If the patient is undergoing physical therapy, it must be interrupted or wait until the end.
- If the patient has suffered an infectious disease, then it is necessary to withstand a certain time. Its duration is determined by the doctor in accordance with the characteristics of the pathology. It is also recommended to wait a certain time after taking medications.
- Before the examination, emotional overload, nervous strain and stressful situations are strictly prohibited.
- Blood is taken for analysis on an empty stomach.
Preparation for a laboratory blood test for antibodies is as follows:
- Follow a diet for 2-3 days before taking the test. This diet involves eliminating fatty, spicy, salty and fried foods, and avoiding drinking alcohol, carbonated drinks and coffee.
- Maintaining a certain time interval (which is determined by the attending physician) after the incubation period of the disease, as well as after taking a course of medications.
- Avoid physical activity (including physiotherapy) the day before donating blood.
A blood test for antibodies is taken early in the morning on an empty stomach. Blood is drawn from the ulnar vein.
For testing results to be reliable, a woman needs to know how to submit biomaterial for testing. The leading gynecologist should give recommendations for preparation to a pregnant woman. Usually the procedure is carried out at 8 weeks of gestation, and then 2 times in the second trimester.
The only exceptions are those cases when future parents have a conflict of Rh factors. In such a situation, blood is donated for testing every month. You need to prepare for the test 3 days before the blood draw. In this case, you need to adhere to certain recommendations.
Before analysis it is prohibited:
- eat fatty and spicy foods; you also need to refrain from consuming fried foods;
- drink coffee and soda;
- carry out physical procedures.
Only venous blood is suitable for the procedure; biomaterial from a finger is not used. Blood sampling is carried out in the morning on an empty stomach. Decoding the results usually takes no more than 2 days, after which a form with the results is given to the woman.
Rules for taking an immunoglobulin test
The composition of the blood changes depending on factors:
- eating habits;
- smoking or alcohol;
- active or passive lifestyle.
Before donating blood you need:
- For two days before the test, do not eat spicy, smoked, fried or salty foods.
- Do not smoke, avoid strong drinks and juices two days before the test.
Blood is taken from a vein on an empty stomach.
If the test is carried out to detect sexually transmitted diseases or hepatitis, a dairy diet should be followed.
Contraindications to undergoing analysis:
- Emotional shock, states of stress and affect.
- After undergoing FLG, ultrasound, MRI, physiotherapy.
Autoantibodies
Autoantibodies are immune proteins that, unlike other globulins, are aimed at destroying the body’s own tissues. Their formation often occurs spontaneously, and it is impossible to determine the cause. More often they appear after infection.
Their formation occurs in autoimmune diseases - rheumatoid arthritis, sclerosis, systemic lupus erythematosus, infertility. In some cases, the appearance of autoantibodies occurs long before the development of disease symptoms.
How are antibodies formed?
Antibodies are formed after exposure to an antigen, a compound foreign to the body. First, it is absorbed by macrophages, and antigen-presenting molecules appear on their membrane. That is, they show the genetic makeup of the “stranger.” In response to this presentation, cells that produce antibodies - B lymphocytes - react. A specific cell clone begins to multiply, which can produce special immunoglobulins.
Plasmocytes are considered to be the formed elements of blood in which antibodies are synthesized. In the past, they were B lymphocytes, but after contact with the antigen they began to create a population of cells with one task - the formation of protective protein molecules.
Deviations from the norm and possible consequences
The concentration of each type of AT has its own standards:
- IgA content – from 0.35 to 3.55 g/l;
- IgG content – from 7.8 to 18.5 g/l.;
- IgM content – from 0.8 to 2.9 g/l.
How many times can an ultrasound be done throughout pregnancy?
- the appearance of antibodies to toxoplasmosis. An increased likelihood of infection with toxoplasmosis is present in the initial stages of pregnancy. This pathology can lead to improper development of the liver, spleen and central nervous system. When infected with toxoplasmosis, many doctors recommend abortion;
- presence of antibodies to rubella. Due to the increased likelihood of heart pathologies, damage to eye tissue and nerve fibers, an abortion is also recommended in the first trimester. Rubella infection in the third trimester is usually not accompanied by such dangerous disorders, but can lead to developmental delays;
- cytomegalovirus infection. This pathology is very dangerous because it leads to damage to the baby’s brain and organs. If it is detected, doctors insist on abortion;
- an increase in TPO concentration signals the development of hypothyroidism and can provoke postpartum thyroiditis;
- increase in the concentration of antiphospholipid antibodies. Increases the likelihood of immune aggression. Antiphospholipid syndrome often leads to miscarriage and serious intrauterine pathologies due to problems with blood flow in the placenta.
Rh conflict is no less dangerous for the unborn baby and can cause the development of serious disorders. Most often, it leads to a disruption in blood circulation and insufficient oxygen supply to the fetus. In addition, Rh conflict increases the risk of developing hepatitis, anemia, pathologies of the brain and cardiovascular system.
DETAILS: Norm of CRP in a biochemical blood test
To determine how high the risk is for the fetus, you need to take an AT titer test throughout pregnancy. In this case, doctors will be able to take the necessary measures in a timely manner.
Antibodies are protein cells that are formed by white blood cells and are designed to combat pathogenic conditions in the body. At birth, our body is sterile, but later in life a person encounters various microorganisms and infections. It is antibodies that help the immune system adapt to their effects.
Antibodies include:
- IgM - occurs immediately after infection and forces the body to begin fighting the pathogen. In the first days of infection, its amount increases, and later begins to decrease. Indicators from 0.06 to 2.40 grams per liter are considered normal;
- IgG - creates stable immunity to the pathogen, actively works during vaccination, it takes about four days to begin its production. Their effect lasts up to 25 days. The norms differ only for children under two years of age. After this age, the rate ranges from 5.4 to 18 grams per liter;
- IgA – protects the gastrointestinal tract, urinary system and respiratory tract from pathogens. They block germs and viruses, preventing them from settling on the walls of the mucous membranes. It is constantly present in the blood, and its level depends on the gender and age of the person. May range from 0.01 grams per liter in an infant to 6 grams per liter in an elderly man;
- IgE - designed to protect us from allergens, fungi and various parasites. They are most often formed in the bronchi, intestines and stomach;
- IgD - produced during exacerbations of chronic infections.
Thus, with normal antibody levels, there are no pathogens or chronic diseases in your body.
The doctor must decipher the results of the antibody test and indicate normal values for each item. This is also done for the reason that some laboratories may use different reagents with which tests are carried out. In this case, the doctor will know for sure whether the results obtained are normal.
IgA is located in biological fluids such as:
- mucous membrane;
- urine;
- saliva;
- bile;
- milk;
- saliva;
- gastrointestinal secretion;
- bronchial secretion.
Normal levels of these antibodies in the blood of a healthy adult vary from 0.4 to 3.5 g/l. In children under 12 years of age, the rate is lower and varies from 0.15 to 2.5 g/l.
Expert opinion
Kovaleva Elena Anatolyevna
Doctor-Laboratory Assistant. 14 years of experience in clinical diagnostic services.
If the indicators increase, the doctor can diagnose diseases such as cystic fibrosis, tuberculosis, arthritis, cirrhosis, hepatitis, purulent infections of the digestive system.
When indicators decrease, symptoms of anemia, skin diseases, and radiation exposure appear. Also, indicators may be lowered as a result of long-term use of certain medications.
IgM are antibodies that are harbingers of diseases, since they immediately notice the appearance of pathogens in the blood. Normal values depend on age and gender. Up to 10 years, the concentration of IgM in the blood reaches from 0.8 to 1.5 g/l. In adolescents and men, the concentration of antibodies varies from 0.6 to 2.5 g/l.
In adult women, the rates are higher - from 0.7 to 2.8 g/l. The concentration of immunoglobulins increases in respiratory and digestive disorders. When the concentration of antibodies decreases, we can talk about gastroenteropathies, burns or lymphomas.
The third type, or IgG, refers to specific antibodies produced in the blood during allergies or infections caused by bacteria. Normal levels of these antibodies depend on the person’s age.
In children under 10 years of age, the levels range from 7.3 to 13.5 g/l. In adults, the norm is a concentration of 8 to 18 g/l. An increase in the volume of IgG in the blood is observed in diseases such as sarcoidosis, lupus erythematosus, arthritis, tuberculosis, and HIV.
A decrease in the concentration of IgG in the blood manifests itself in various types of neoplasms that arise in the lymphatic system, muscular dystrophy, and allergies.
Norms for CMV levels in the blood
There is no numerical value for the “normal” level of antibodies in biological fluids.
The concept of counting IgG and other types of immunoglobulins has its own characteristics:
- Antibody concentration is determined by titration. Blood serum is gradually diluted with a special solvent (1:2, 1:6 and other concentrations that are multiples of two). The result is considered positive if the reaction to the presence of the test substance remains during titration. For cytomegalovirus infection, a positive result is detected at a dilution of 1:100 (threshold titer).
- Titers represent an individual reaction of the body, which depends on the general condition, lifestyle, activity of the immune system and metabolic processes, age, and the presence of other pathologies.
- Titers give an idea of the total activity of antibodies of classes A, G, M.
- Each laboratory can use its own test systems to detect antibodies with a certain sensitivity, so they must produce a final interpretation of the results, which indicates reference (borderline) values and units of measurement.
Avidity is assessed as follows (units of measurement – %):
- <30% – low-avidity antibodies, primary infection that occurred about 3 months ago;
- 30-50% – it is not possible to accurately determine the result, the analysis must be repeated after 2 weeks;
- >50% – high-avidity antibodies, infection occurred a long time ago.
In adults
The results for all groups of patients are interpreted in the manner indicated in the table below.
Table:
| IgG value | IgM value | Interpretation |
| positive | positive | Secondary reinfection. Treatment is required |
| negative | positive | Primary infection. Treatment required |
| positive | negative | Immunity has been formed. A person is a carrier of the virus. Exacerbation of the disease is possible with decreased immunity |
| negative | negative | There is no immunity. There was no CMV infection. There is a risk of primary infection |
Antibodies to cytomegalovirus can be at low levels for several years, and when reinfected with other strains, the amount of IgG increases rapidly. To obtain an accurate diagnostic picture, the level of IgG and IgM is determined simultaneously, and a repeat analysis is carried out after 2 weeks.
In children
Children during the neonatal period and breastfeeding may have IgG in their blood that they received in utero from their mother. Their level begins to gradually decline after a few months due to the lack of a constant source. IgM antibodies often give false-positive or false-negative results. In this regard, diagnosis at this age causes difficulties.
Taking into account the overall clinical picture, immunological tests are interpreted as follows:
- High level of IgG – exacerbation . In the absence of IgM, the severity of the disease is assessed by the concentration of IgG. In this case, additional testing using the PCR method is recommended, which more accurately determines the presence of the virus. If the DNA of microorganisms is not detected, then the child could receive antibodies from the mother. No true infection occurred. The study also needs to be repeated a year later - if antibodies are found, the result is interpreted as positive.
- Low and medium IgG values – a state of remission . If this is detected in newborns at risk, this indicates a poor state of passive immunity and increases the likelihood of bacterial complications.
Repeated testing allows you to determine the time of infection:
- after birth – increasing titer;
- intrauterine – constant level
During pregnancy
Diagnosis of CMV in pregnant women is carried out according to the same principle. If in the first trimester it is discovered that IgG is positive and IgM is negative, then it is necessary to take a PCR test to confirm the absence of reactivation of the infection. In this case, the fetus will receive maternal antibodies that will protect it from the disease.
The antenatal clinic doctor should issue directions for monitoring the IgG titer also in the second and third trimesters.
If a low avidity index is detected at a period of 12-16 weeks, then infection could have occurred before pregnancy, and the probability of infection of the fetus is almost 100%. At 20-23 weeks this risk decreases to 60%. Determining the time of infection during pregnancy is of great importance, since transmission of the virus to the fetus leads to the development of severe pathologies.
To viruses
Decoding the combinations of antibodies in the blood to viruses:
- Minus IgM, IgG - there is no immunity, the body has not yet encountered the pathogen. This is a reason to get vaccinated and strengthen your defenses. This result indicates a high risk of infection.
- Plus IgM, minus IgG - primary infection has occurred, the viral disease is in the acute stage. In this case, treatment begins, the pathogen is first determined.
- Minus IgM, plus IgG - the disease was previously suffered, and this may also indicate a chronic course of the pathology, which is in remission. The result indicates acquired immunity.
- Plus IgG, IgM - a chronic viral disease in the acute stage. Less often, such a result is obtained during a course of therapy.
Heavy chain classification
There are five classes ( isotypes)
) immunoglobulins, differing:
- amino acid sequence
- molecular weight
- charge
- glycosylation
The IgG class is classified into four subclasses (IgG1, IgG2, IgG3, IgG4), the IgA class into two subclasses (IgA1, IgA2). All classes and subclasses make up nine isotypes that are normally present in all individuals. Each isotype is determined by the amino acid sequence of the heavy chain constant region.
To the Rh factor
Rh antibodies are a protein found on the surface of blood cells such as red blood cells. It may be absent, and then people are called Rh negative.
Absence does not affect health and does not affect the functioning of the immune system. There is a risk when the Rhesus does not match between the pregnant woman and the fetus. The presence of Rh conflict causes pathologies of the kidneys, hepatobiliary system and brain in the newborn.
Tests for Rh and blood group are indicated at the beginning of pregnancy and then every 30 days. If necessary, the woman is prescribed special treatment measures.
Rh conflict causes miscarriage and hemolytic disease. To determine the likelihood of this, a woman should undergo testing while planning a pregnancy and already during pregnancy.
The reasons for conducting a Rh test will be:
- pregnancy planning;
- first trimester;
- complicated pregnancy;
- appointment for blood transfusion;
- hemolytic disease in a newborn.
The result can be negative or positive. In the second case, a separate column will indicate that alloimmune bodies were detected in a certain titer.
Control of proliferation
The most effective control mechanism is that the reaction product simultaneously serves as its inhibitor. This type of negative feedback occurs during the formation of antibodies. The effect of antibodies cannot be explained simply by neutralization of the antigen, because whole IgG molecules suppress antibody synthesis much more effectively than F(ab')2 fragments. It is believed that blockade of the productive phase of the T-dependent B-cell response occurs as a result of the formation of cross-links between the antigen, IgG and Fc receptors on the surface of B-cells. IgM injection enhances the immune response. Since antibodies of this particular isotype appear first after the introduction of an antigen, they are assigned an enhancing role at the early stage of the immune response.
Antibodies in the diagnosis of hepatitis C
Also read: Chlamydia in the blood during pregnancy
Diagnosis of hepatitis C using antibodies is not limited to only the listed types. The hepatitis virus can give false results. Therefore, antibodies to proteins of the NS-3 and NS-4 types are simultaneously detected.
- Detection of the IgG type indicates acute viral hepatitis or transition to a chronic form.
- IgM indicates an active acute process in the liver.
The differences are confirmed using antibodies NS-3 (for the acute phase) and NS-4 (more typical for the chronic course).
Immunoglobulins class A (IgA)
Immunoglobulins A (make up about 15% of all serum Igs) determine the immunological resistance (protection) of all mucous membranes, where they are secreted (produced by the mucous membranes of the gastrointestinal tract, urogenital and respiratory tracts). Antibodies of this type are closest to the external environment, so they are the first to protect the body from the effects of toxins and various pathogenic substances.
A huge amount of class A antibodies is contained in breast milk, which compensates for the lack of immunoglobulins in the newborn’s body and, thus, protects the baby from many adverse factors. There is a lot of IgA in saliva (to neutralize microbes and viruses that enter the body), in the mucous membrane of the cervix (mucus plug), that is, they are a reliable barrier that prevents pathogenic microorganisms from penetrating our mucous membranes. A deficiency of these antibodies at production sites inevitably leads to a decrease in local immunity and infection. Elevated class A antibodies have diagnostic value in identifying TORCH infections and some STIs:
- When infected with Toxoplasma gondii (toxoplasmosis), as always, the primacy belongs to class M immunoglobulins (Toxo-IgM), they appear approximately a week after infection, and specific IgA begins to be detected 2 weeks after penetration of the pathogen, and after a month their level reaches a maximum. However, Tocho-IgA disappears in most cases (90%) over the next six months. Very rarely, class A antibodies to toxoplasmosis persist for up to a year, so it is hardly advisable to consider them the main criterion for primary infection (like Tocho-IgM), although they suggest that the duration of infection may be limited to 12 months. Meanwhile, taking into account the fact that IgA is not able to overcome the transplacental barrier, Tocho-IgA can become an assistant in the diagnosis of intrauterine infection in congenital toxoplasmosis (the decisive role belongs to clinical data, obstetric history, and determination of toxoplasma DNA by PCR). Class G antibodies have more accurate information regarding the timing of toxoplasmosis infection and the duration of the disease, namely, their avidity index, which indicates the strength of the connection between the antibody and the antigen.
- It is not surprising that once it reaches the mucous membrane of the genital tract and begins its development, chlamydia causes increased production of class A immunoglobulins, which at the first stage try to cope with the invasion of uninvited “guests”. An increased titer of antibodies to chlamydia is detected within 1.5-2 weeks after exposure to the pathogen and continues to increase for several months. If the process is not stopped in a timely manner by active treatment, it will become chronic and subsequently worsen with an increase in IgA levels. It should be noted that the laboratory search for chlamydia is based on polymerase chain reaction (PCR), and antibody testing is only an addition to diagnostic measures.
Technique
The most modern and effective method for detecting antibodies in blood serum is immunofluorescence analysis. With the help of such a laboratory test, it is possible to determine the type and titer (activity) of immunoglobulins, as well as to determine how much the pathology has developed. The research includes the following stages:
- the laboratory assistant takes biological material from the patient;
- a few drops of the resulting blood are dripped onto a special plate with wells containing purified antigens of the suspected pathogen;
- then the laboratory assistant adds a special reagent to the wells;
- Taking into account the staining, the doctor draws conclusions about the result of the analysis.
The study itself can be of 2 types:
- quality. Prescribed to confirm the presence or absence of the desired antigen;
- quantitative. This type of analysis is considered more complex and shows the concentration of antibodies in the serum being studied. It can be used to assess how quickly the infection is developing.
Regardless of the type of analysis, deciphering the results takes from 1 to 3 days.
Types of antibodies
Over different periods of life, the human body “gets acquainted” with various pathogens, chemicals (household chemicals, medications), and products of the breakdown of its own cells (for example, in case of wounds, inflammation, purulent skin lesions). In response to this, it begins to produce its own immunoglobulins or antibodies in the blood - these are special protein compounds formed from lymphocytes and acting as immune stimulants.
In immunological laboratories, five types of antibodies are distinguished, each of which acts strictly on certain antigens:
- IgM is the first immunoglobulin that begins to be produced when an infection enters the body. Its role is to stimulate the immune system to primarily fight the disease.
- IgG - appears 3-5 days after the onset of the disease . It forms stable immunity to infections and is responsible for the effectiveness of vaccination. This class of protein compounds is so small in size that it can penetrate the placental barrier, forming the primary immunity of the fetus.
- IgA - protects the gastrointestinal tract, urinary system and respiratory tract from viruses, bacteria, microbes. They bind foreign objects, preventing them from attaching to the walls of the mucous membranes.
- IgE - activated to protect the body from parasites, fungi and allergens . They are localized mainly in the bronchi, submucosal skin, intestines and stomach. They take part in the formation of secondary immunity. They are practically absent in free form in blood plasma.
- IgD is a fraction that has not been fully studied. It is believed that these agents are responsible for the formation of local immunity and begin to be produced during exacerbation of chronic infections or multiple myeloma. In blood serum they make up less than 1% of the fraction of all immunoglobulins.
About the differences between IgG and IgM immunoglobulins
The enzymatic substances of the two described classes differ in their functional significance.
Immunoglobulins type M (IgM) are responsible for the primary response of the body's defense system. As soon as a viral agent (in particular, CMV) enters the body, the immune system begins to produce so-called rapid substances (antibodies) to fight the pathogenic pathogen. Class M enzymatic components are significant in size, but are only suitable for rapid response and destroy the virus here and now. They do not form cellular memory, therefore such immunity is temporary. The reaction lasts up to 5 months.
G-immunoglobulins (IgG antibodies to cytomegalovirus) are smaller in size. They are produced by the protective structure of the body much later, after several weeks, or even months. Actively produced for life. Anti cmv IgG forms a stable memory, therefore they contain the virus throughout the patient’s life.
Despite this, stable immunity to cytomegalovirus is not observed. It is enough for the immune system to fail, and the symptoms will flare up with renewed vigor and the disease will take on an acute form.
What does human blood consist of?
If you have ever looked at a drop of blood through a child's microscope, then even in this way you may have noticed that it is not uniform.
The composition of blood can be divided into two components :
- Plasma;
- Shaped components.
Plasma is a liquid that flows out when a small scratch occurs. It has no color, but is extremely important for our body. It contains and delivers to all cells of our body:
- Protein;
- Carbon dioxide;
- Oxygen;
- Useful microelements;
- Glucose and other vitamins necessary for the quality functioning of organs and systems.
Shaped components include:
- Red blood cells are the same molecules that color the blood. Their main task is to transport carbon dioxide and oxygen. These cells look like bulging discs. Their lifespan is 4 months, after which they are destroyed;
- Platelets are cells designed to fight vascular damage. They instantly react to injury to the vessel wall and, sticking to each other, clog the site of the lesion;
- Leukocytes are particles involved in the formation of immunity and capable of penetrating into tissues from the blood channel. When an infection arises in your body, they strive to destroy it, for which they produce antibodies and various cells that can absorb pathogenic formations.
Initially, blood is a sterile substance, but it is susceptible to viruses no less than other organs of our body.
Methods for producing monoclonal antibodies
Obtaining monoclonal antibodies is a complex multi-step process that goes through the following stages:
- Animal immunization. Typically mice or rats are used. This is necessary in order to increase the number of lymphoblasts - cells that produce the necessary antibodies and transfer these cells to an active state. Once isolated from the body, these cells cannot exist for long in laboratory conditions; they will die even on nutrient media containing growth factors. To prevent this, they are crossed with malignant myeloma cells.
- Preparation of myeloma cells. In parallel with immunization of animals, tumor myeloma cells are prepared. They, firstly, have the ability to synthesize monoclonal antibodies, and secondly, they have unlimited life potential (they are immortal and capable of endless reproduction). To prevent myeloma cells from dying outside the body, they are cultured in special media using growth factors.
- Hybridization (fusion) of lymphoblasts and myeloma cells to form a hybridoma. To do this, cells are treated with various antibodies to change the structure of their membranes and provoke the formation of cytoplasmic contacts. In this case, different types of cells are formed that have a double set of chromosomes (dicaryons). These can be dikaryons formed only by lymphocytes, or only by myeloma cells. But for the production of monoclonal antibodies, it is dikaryons formed by a lymphocyte and a myeloma cell—hybrid cells—that are needed.
- Selection of hybrid cells. For this purpose, special solutions are used that allow only lymphoblastic and hybridoma dikaryons to survive. The former soon die, because they do not have the ability to divide without limits, but hybridoma cells remain viable.
- Recloning of hybridoma clones.
- Identification and selection of hybridomas producing monoclonal antibodies. Typically, an enzyme immunoassay is used for this.
- Massive build-up of antibodies.
- Purification of the resulting antibodies. The degree of purification will be determined by the area of application of the drug. If this is diagnostic, 70-95% purity is sufficient. If the drug is to be used for immunotherapy, a higher degree of purity is required. Affinity and ion exchange chromatography are used for purification.
- Removing remaining impurities and disinfecting the resulting drug from viruses and bacteria.
Currently, there is a trend towards refusing to use animal antibodies for therapeutic purposes. Firstly, they are foreign agents to the body and can provoke allergic reactions, including anaphylaxis, which directly threatens the lives of patients. Secondly, the human immune system, recognizing such antibodies as foreign, will try to inactivate them, which will reduce the effectiveness of antitumor treatment. It is not possible to obtain human monoclonal antibodies using the method described above due to the following problems:
- Immunizing humans with various antigens is unethical.
- Even if you obtain immunized human lymphocytes, there will be problems at the stage of their fusion with mouse myeloma cells—the resulting hybridomas will be unstable.
- Human myeloma cell lines that could be effectively used within biotechnologies to produce antibodies have not yet been obtained.
In this regard, it was necessary to look for new technologies for producing antibodies. The solution to the problem was hybrid, humanized and single-chain antibodies, the production of which involved the use of hybridoma technology, briefly described above, and recombinant DNA technology.
- A hybrid or chimeric antibody is an antibody in which its constant domain is replaced with human immunoglobulin. They are obtained using recombinant DNA technology, when the fragment of mouse DNA responsible for the synthesis of the constant domain is removed and replaced with a fragment of human DNA. Thus, the antibody will have a human protein as a constant domain, which has immunogenic and effector properties, which will allow the body to perceive it as “one of its own,” and the variable domain, which specifically interacts with the antigen, will remain mouse. All together, this will preserve the specificity and reduce the allergenicity and immunogenicity of the drug used.
- The humanized antibody contains even less mouse protein due to only the antigen-binding hypervariable regions of the variable domain. This further reduces the likelihood of complications from the immune system.
- A single-chain antibody is the smallest fragment of an antibody that is still able to bind well to the antigen and exert its effect. It does not contain a constant domain at all.
Antisperm antibodies in men
Immunoglobulin proteins are most often concentrated in the male body. There are several types of antibodies. The most dangerous cells are those of the IgM class. They have a depressing effect on the structure of sperm, thereby provoking the development of asthenozoospermia.
IgG antibodies - Description
IgG class antibodies disrupt the rate of dilution of seminal fluid, change the pH of the sexual environment and increase the number of leukocytes. In addition, both types of antisperm antibodies can reduce the volume of ejaculate, thereby reducing the chances of conception. In some cases, they block sperm receptors responsible for binding to the egg. The reasons for the increase in antisperm antibodies in a man’s body include the following:
- Chronic prostatitis;
- Venereal diseases;
- Malignant formations;
- Injury to the scrotum;
- Consequences of surgery;
- Clogging of the vas deferens;
- Varicose veins of the testicle;
- Inflammatory processes of the reproductive system.
Prostatitis - Description
If a study determining antibodies in sperm showed 4 units, this is normal. The situation requires the attention of specialists if the figure in the analysis results exceeds 60 U/ml.
Conception in the presence of ASAT in men or women is carried out by intrauterine insemination. But before this, the couple is prescribed drug therapy aimed at the cause of the disease. During this period, it is necessary to use barrier contraception. In some cases, doctors resort to in vitro fertilization.
Most likely you will be interested!
- Fluid in the retrouterine space (Douglas space): Causes, treatment, consequences
- What is fertility in a woman? Fertility in women in simple words.
- Implantation bleeding on what day after conception?
- Menstrual cup: How to use? How to insert?
- Is it possible to get pregnant while breastfeeding?
- Delay of menstruation
Immunoglobulins classes D and E
Immunoglobulin D (IgD) is synthesized in the embryonic period in the fetus, and in an adult it is found only in trace amounts (and even then not always). These antibodies have no clinical significance, causing only highly specific interest among doctors of a certain profile. Little is known about them: they are present on the membrane of B cells and, together with IgM, can participate in antigen binding.
Immunoglobulins E (IgE) are present in blood plasma in negligible concentrations and act as reagins. Having a high degree of affinity for the surface membranes of mast cells and basophils, antibodies of this class perform an important function in triggering allergic reactions: the antigen binds 2 nearby IgE molecules that are located on the surface of the mast cell, which serves as a signal for the release of histamine and the triggering of an immediate reaction. By the way, sera for determining class E immunoglobulins are very expensive, so the price of tests for antibodies, indicating allergization of the body, is, as they say, “biting.”
What can you tell from antibodies?
The development of immunology has shown that antibodies can be distinguished not only by the degree of accumulation, but also by type. Five main varieties have been identified that react to certain microorganisms and foreign substances and their breakdown products. Therefore, a blood test for antibodies can help answer the questions:
- whether there are specific bacteria or viruses in the body;
- if any, then in what quantity (whether a person is considered infected or is it just protection);
- How fully does one’s own immunity respond to infection? Are additional medications needed?
- during an infectious disease, it is possible to determine the stage of the disease and predict the outcome;
- whether a person has antibodies in his blood that are markers for malignant cells if he is suspected of having cancer;
- how the mother’s body reacts to the fetus;
- how rapidly the process of engraftment of the transplanted organ or tissue proceeds after transplantation;
- what antigen causes the allergy?
The possibilities for using antibody detection in diagnostics continue to be studied. It is still not clear why, under the same conditions, one person suffers an acute illness, while another copes independently without any symptoms.
Reasons for testing
Antibody tests are carried out to determine and track the dynamics of the development of the following pathologies:
- Antibodies to thyroid peroxidase (TPO) - analysis is carried out to determine pathologies of the thyroid gland, including those of an autoimmune nature,
- Hepatitis C, B, D, A, E,
- HIV – carried out up to 3 times, diagnosis is made after 3 positive tests,
- Leptospirosis,
- Diphtheria,
- Rubella,
- Chlamydia,
- Herpes,
- Syphilis,
- Tetanus,
- Cytomegalovirus,
- Ureaplasmosis.
When conducting an antibody test, not only the type of agent matters, but also the time of the study. If no immunoglobulins are detected in the first 5 days of the disease, this does not indicate the absence of infection.
The primary immune response takes longer to form than the secondary one. During primary infection, the presence of class M antibodies is characteristic, while G-globulins appear later.
What might be the results of the analysis?
Reference values:
- No response (negative) – <0.8 S/CO (signal/cutoff).
- Doubtful (intermediate) – 0.8 < 1.0 S/CO (signal/cutoff).
- Reaction is present (positive) – 1.0 S/CO (signal/cutoff).
Various biological fluids are used as material for analysis:
- deoxygenated blood;
- urine; If Klebsiella is found in the urine, its meaning can be found here.
- saliva;
- sweat.
Treatment
When antisperm bodies are detected, treatment is prescribed, the main goal of which is to reduce them for pregnancy. For this, the following types of treatment are used:
- Plasmapheresis is the removal of plasma from a certain volume of the patient’s blood in which toxic components are found.
- Artificial insemination with husband's sperm, treated for the presence of antisperm antibodies.
- The contraceptive method is the use of a condom for a period of 3–6 months, which prevents the entry of sperm into the woman’s body.
- Therapy that reduces the viscosity of cervical mucus.
- Vegetative resonance testing.
Plasmapheresis can be used to solve other problems:
Please note that infertility is a serious disease that requires more thorough examination, since the immune factor is one of the causes. It is imperative that both spouses undergo examination to determine inflammatory infections of the genitourinary system. They may be the main source of antisperm antibodies.
It should be noted that the detection of these antibodies in one or both spouses does not exclude the possibility of becoming pregnant, since they reduce the likelihood of conception and do not completely prevent it.
- Author: Boris
How did I become a doctor? Quite a difficult question... If you think about it, there was no choice. I was born into the family of a resuscitation doctor, and every day at dinner I heard my father’s story about how his day went. As a child, this all seemed fantastic, beyond reality. Rate this article:
- 5
- 4
- 3
- 2
- 1
(0 votes, average: 0 out of 5)
Share with your friends!
Analysis for immunoglobulins M and G
Tests for immunoglobulins M and G can accurately indicate the presence of an infectious or bacterial infection. The following clinical studies are being conducted:
- radioimmunoassay;
- linked immunosorbent assay;
- RPHA – indirect hemagglutination reaction;
- RMP – microprecipitation reaction;
- RIF – immunofluorescence reaction.
All studies serve for the comprehensive detection of antibodies and antigens that cause the growth of immunoglobulins. There are other methods for diagnosing diseases using immunoglobulins. Humoral immunity is a very complex process that requires extensive knowledge in immunology and other areas of medicine. When you visit a doctor, you can consult an experienced specialist, undergo a full examination and receive effective treatment. You can make an appointment with a doctor by calling the Yusupov Hospital.
Author
Dmitry Nikolaevich Staroverov
Head of the department of anesthesiology and resuscitation with intensive care and intensive care wards - anesthesiologist-resuscitator