Polyneuropathy is considered multiple damage to peripheral nerves, which is manifested by paralysis, sensory disturbances, trophic and vegetative-vascular disorders. Develops predominantly in the distal extremities. The disease is a common symmetrical pathological process, which is usually localized in the distal muscles and gradually spreads proximally.
Polyneuropathy - what is it?
Polyneuropathy is translated from Greek as “suffering of many nerves.” These nerves can be affected by external factors that affect them for a long time and impair their functioning. Unlike a brain tumor or stroke, which cause a strictly defined set of symptoms depending on the location, polyneuropathy reveals a special clinical picture, which will be discussed below.
First of all, polyneuropathy is caused by diseases in which any substances that have a harmful effect on the nerves accumulate in the body. Such diseases include endocrine pathology and diabetes mellitus.
High levels of glucose in the blood, which last for a long time, contribute to impaired conduction of peripheral nerves. The result is diabetic polyneuropathy. It belongs to the group of dysmetabolic disorders.
If the culprit of the disease is not an ordinary substance (after all, everyone has glucose in their blood, there is simply too much of it in diabetes), but some external toxin, then toxic damage to the peripheral nerves, both sensory and motor, occurs.
This is how toxic damage to peripheral nerves develops, and the most striking example is alcoholic polyneuropathy, which occurs in people who drink heavily and for a long time.
Malignant neoplasms, which poison the entire body with the products of their metabolic activity and decay, can also cause nerve damage. This polyneuropathy is called paraneoplastic, and it is a serious sign of advanced cancer.
Sometimes serious infections cause nerve damage. Such polyneuropathies can be classified as both infectious and toxic - since microorganisms often use strong toxins, for example, diphtheria bacillus.
Finally, autoimmune polyneuropathies may occur, in which the nerves destroy the antibodies of their own body, attacking the nervous tissue “by mistake.” Such diseases include systemic scleroderma and other “major collagenoses”.
Types of polyneuropathy
There are more than 100 types of peripheral neuropathies, and most of them are polyneuropathies. Each type is classified according to the type of nerve damage. For example, diabetic neuropathy occurs in people with diabetes, while idiopathic neuropathy has no known cause.
There are three main types of polyneuropathy:
- Chronic symmetric peripheral neuropathy
- develops over many months. - Multiple mononeuropathy
is damage to several separate nerve areas. - Acute symmetric peripheral neuropathy
is rare. The most common cause is Guillain-Barré syndrome, a condition that can be fatal.
Some types of neuropathy may take years to develop, while others become severe within hours or days.
Symptoms of polyneuropathy - characteristic signs
The disease has an extremely characteristic clinical picture. Before reviewing the symptoms of polyneuropathy, it should be mentioned that this nerve damage can be of the following types:
- Sensitive or sensory form. Mostly sensory disorders occur: paresthesia, numbness, burning, tingling, a feeling of discomfort or “crawling.”
- Motor or motor form. Muscle weakness, muscle wasting and atrophy occurs.
- Most often there is a combined version of them - sensorimotor polyneuropathy, which occurs in most cases, and especially in diabetes and alcoholism.
- Autonomic polyneuropathy. With this course, the autonomic nerves, which “manage” the internal organs, are affected.
- Finally, there is a mixed form that combines all types of disorders.
Polyneuropathy is characterized by damage to small nerves, since their myelin sheath is thinner and it is easier for all harmful substances to reach them. Therefore, most often there is damage to the hands and feet - polyneuropathy of the upper and lower extremities, the symptoms of which, as neurologists say, are of the “socks and gloves” type.
There is even a type of sensitivity disorder called the polyneuritic type. Thus, polyneuropathy of the upper and lower extremities will have the same symptoms.
The next important symptom of polyneuropathy will be the symmetry of the lesion, since the disease-causing substance circulates in the blood.
For example, symptoms of polyneuropathy of the upper extremities may include weakness of the fingers, burning pain, a feeling of chilliness, and marbling of the skin on the back of the hands (autonomic disorders).
The most common signs of nerve damage are as follows:
- Various and very varied pains, including those with a neuropathic, “burning” tinge.
- Attachment of trembling of fingers.
- The appearance of fasciculations (or muscle twitches that are involuntary).
- Impaired sensitivity (not only tactile, which was described above, but also a decrease in temperature and pain sensitivity). That is why, with diabetic neuropathy, patients “badly feel” a pebble in a shoe, a poorly driven shoe stud and other irritants.
- Muscle weakness, inability or significant difficulty in moving with a large amplitude. Weakness is often combined with muscle hypotonia and asthenia of the patient.
A special group consists of autonomic signs of polyneuropathy. These include hot flashes and the appearance of pallor and cold sweat, poor circulation (and poor healing of wounds and all kinds of damage to the skin).
The disease does not always develop over a long period of time and gradually. Thus, polyneuropathy of the lower extremities, the symptoms of which indicate a decrease in sensitivity, extinction of Achilles reflexes, and the presence of trophic disorders, may indicate a long-term process, or may appear in a matter of days and weeks, for example, with a mild degree of radiation sickness or poisoning with lead and its compounds.
Sometimes surprising complaints arise as part of polyneuropathy. Thus, with pernicious anemia, due to a deficiency of cyanocobalamin (vitamin B 12), posterior column ataxia occurs. In this case, it is not the peripheral nerves that are affected, but the spinal cord, more precisely, its posterior cords (columns), in which the conductive bundles of joint-muscular sense, or Gaulle-Burdach bundles, are located.
What happens when they are defeated? Each of us, undoubtedly, with our eyes closed, knows how our arms and legs are positioned, even if we don’t move them. But the patient with this type of ataxia does not know. Therefore, he cannot walk in the dark, because he gets confused and does not know where and how his legs are located. But in the presence of light and visual control, such a person’s gait is normal.
There are special autonomic or autonomic neuropathies that disrupt the heart rhythm and can even lead to sudden death due to ventricular asystole or other fatal arrhythmias. This polyneuropathy is an autonomic motor cardiac form of the disease.
Causes and Effects
The previous classification gives an idea of the causes of polyneuropathy, more precisely about the diseases and conditions under which it develops. In fact, the etiology of most is unknown.
Let's consider several cases, different in their causes:
Heyhen-Barré syndrome
- Autoimmune pathology causes destruction of the myelin sheath of the nerves, leading to flaccid symmetrical paralysis, developing in an ascending manner.
- The disease begins 2 weeks after acute respiratory viral infection with damage to the legs.
- The onset of polyneuropathy is acute: the feet become numb, pain and weakness in the legs appear. Over the next day, symptoms increase - legs, thighs, torso, arms.
- The most dangerous thing is the involvement of the respiratory muscles in the process (Landry's paralysis). This is fraught with death from respiratory arrest.
- The damage spreads to the cranial nerves. The result is complete paralysis, muscles are flabby, tone is reduced. Only the eyes remain alive. The patient looks depressing.
- This condition lasts about one and a half months. The patient is in a hospital, connected to a ventilator, fed through a tube.
- As time passes, the symptoms of polyneuropathy begin to disappear in the reverse order - head, upper limbs, torso, lower limbs.
- After long-term rehabilitation due to muscle atrophy, 80% have a favorable prognosis and complete recovery. 20% have an undulating course with periodic exacerbations.
Alcoholic polyneuropathy
Occurs with the abuse of alcoholic beverages, especially low quality ones.
- Fusel oils damage the liver and cause vitamin B1 deficiency. This is the predominant cause of destruction of the myelin sheath and degeneration of nerves.
- Alcoholic polyneuropathy is promoted by hypothermia, compression of the nerves during sleep in unfavorable conditions and in an awkward position.
- The affected area extends to the upper and lower extremities in a “socks-gloves” type. Constant pain in the limbs, paresthesia reaches paresis, encephalopathy and mental disorders progress in parallel.
Diabetic polyneuropathy
can complicate diabetes at any stage of the disease, but uncorrected sugar levels increase this risk.
- The reason is metabolic disorders and hypoxia of nerve cells.
- An excess of lactic acid occurs, the potassium-sodium pump and vitamin B1 metabolism are disrupted.
- Hypoxia of nerve cells and tissues is explained by microangiopathy, which disrupts their nutrition.
- The order of destruction of nerve fibers has a certain sequence. At the beginning, the vegetative group of fibers is affected, then vegetosensory symptoms are added, and lastly motor disorders. The nerve fiber thickens and degenerates into scars.
- Patients complain of vague pain in the feet, numbness, coldness of the extremities, and decreased pain sensitivity. Vegetative symptoms are described above.
Polyneuropathy due to botulism
occurs due to exposure to the toxin secreted by the botulism bacillus.
- Spastic paralysis of the muscles of the limbs occurs in severe cases.
- The onset of the disease is accompanied by paralysis of the oculomotor and pharyngeal muscles, followed by diarrhea, vomiting, double vision, immobility of the pupils, and blurred vision.
- Difficulty swallowing and speaking.
An interesting fact is that people who drink alcohol consume canned food contaminated with botulism. Alcoholics who wash down such canned food with their “favorite drink” receive a kind of protective code and do not suffer from botulinum polyneuropathy. This form of polyneuropathy is curable, and recovery occurs with treatment.
Diagnosis of polyneuropathy
The diagnosis is made by a neurologist taking into account complaints, anamnesis and the development of the disease. As a rule, with polyneuropathy, making the correct diagnosis does not cause difficulties.
Neither MRI, nor CT, nor ultrasound help here. The most important method is ENMG - electroneuromyography, which allows you to fully identify conduction disturbances along the nerve fiber and determine what is affected - the axial cylinder of the nerve or the myelin “insulating” sheath.
Blood chemistry tests often show certain endocrine disorders (glucose). In extreme cases, polyneuropathy requires a nerve fiber biopsy, which is studied using histochemical and immune methods.
Diagnosis of polyneuropathies
Diagnosis is made based on medical history, clinical examination, and neurological evaluation. The doctor will conduct a detailed review of all symptoms, lifestyle factors, and family history. He will also check the patient's height, weight, pulse, blood pressure and temperature. The heart, lungs, and abdomen may also be tested to rule out alternative physiological causes.
Blood tests may be ordered to look for diabetes, thyroid function, immune function, nutritional deficiencies and other factors that may cause polyneuropathy.
Some simple tests may be done to check reflexes, muscle strength, sensitivity to temperature and other sensations, coordination and posture.
Other methods that can be used to diagnose polyneuropathy:
- MRI or CT scan
—can help detect tumors, herniated discs, or other abnormalities that may affect nerve function. - Electrodiagnostic tests
—measure electrical activity in muscles and nerves to help detect nerve damage. Examples are electromyography and nerve conduction velocity. - Biopsy
- The doctor may remove a small part of the nerve or a sample of skin to check for abnormalities in nerve function or nerve endings.
Symptoms of polyneuropathy
The disease in question, polyneuropathy of the upper and lower extremities, begins with muscle weakness, and first of all, in the distal parts of the legs and arms. This is due to damage to the nerve fibers. With this disease, the distal parts of the limbs are primarily affected due to the lack of sufficient protection of segments of the peripheral system (for example, the blood-brain barrier located in the brain).
Manifestations of the described pathology debut in the foot area and gradually spread up the limb. Depending on the typology of nerve fibers that are subject to destruction to a greater extent, all types of polyneuropathy are conventionally divided into four subgroups.
Due to damage mainly to the afferent long processes of neurons, patients experience positive or negative symptoms. The first is characterized by the absence of function or its decrease; positive symptoms are those manifestations that have not previously been observed.
In the first turn, in patients with the disease in question, various types of paresthesia are manifested, such as burning, tingling, crawling, and numbness.
the clinical picture is complicated by algias of varying intensity, and the susceptibility to painful stimuli increases. As symptoms increase, patients become overly sensitive to simple touches. Later, they experience manifestations of sensitive ataxia, expressed in unsteady gait, especially with closed eyes, and impaired coordination of movement. Negative symptoms of polyneuropathy include decreased sensitivity in areas where nerve fibers are damaged.
When the axons of movement neurons are damaged, polyneuropathy of the upper and lower extremities manifests itself, firstly, as muscle atrophy and is found in weakness of the legs and arms. The described symptoms progress to the occurrence of paralysis and paresis. Less commonly, a condition manifested by unpleasant sensations in the legs, appearing mainly at rest and forcing people to make movements of a relieving nature (restless lower limbs syndrome) can be observed. In addition, fasciculations and convulsions may occur.
Autonomic dysfunctions are divided into trophic disorders and vascular disorders. The first include the appearance of pigmentation and peeling of the skin, the appearance of cracks and ulcers on the extremities. Vascular disorders include a feeling of cold in the damaged segments, dullness of the skin (the so-called “marble pallor”).
Vegetative-trophic symptoms also include changes in the structure of the derivatives of the dermis (hair and nails). Due to the fact that the lower extremities withstand more load, polyneuropathy of the legs is diagnosed much more often than of the arms.
Development mechanism
The development of chronic inflammatory demyelinating polyneuropathy is based on a combination of several factors:
- Difficult situations, injuries, diseases (cancer, diabetes), exhausting a person mentally and emotionally and leading to exhaustion.
- Entry into the body of an infection that contains a protein similar in structure to human proteins.
- Genetic predisposition.
Due to the combined influence of factors, the destruction of nerve processes, their myelin sheath, or disruption of myelin production occurs. Which of these processes is primary in a patient depends on various reasons and is not always obvious. For example, in an alcoholic patient with a deficiency of folic acid and some vitamins, the primary disorder in the production of myelin.
It is believed that under the influence of certain factors, the production of myelin antigens begins. This probably occurs under the influence of an infection with a similar protein entering the body or a certain internal disorder. As a result, the myelin protein begins to be read by the body as pathogenic. In the area of the nerve, Th1 type cells accumulate, penetrating the blood-neurological barrier. Inflammation develops, leading to the destruction of myelin and disruption of its production.
Polyneuropathy of the lower extremities
The disease in question, polyneuropathy of the extremities, is a dystrophic destruction of nerve cells, causing a malfunction in the functioning of the peripheral nervous system. This disease is manifested by a decrease in motor ability, decreased sensitivity, depending on the location of the pathological focus, any part of the limbs, and muscle pain. With the disease in question, the patient’s nerve fibers that supply the feet are damaged. As a result of structural damage to the nerve fibers, the sensitivity of the legs is lost, which affects the individual’s ability to move independently.
Treatment of polyneuropathy of the lower extremities, as a rule, is quite labor-intensive and lengthy, since more often this disease is progressive in nature and develops into a chronic course.
To determine the reasons that provoke the development of the described illness, first of all, it is necessary to understand the structure of the nervous system, in particular its separate area - the peripheral system. It is based on long processes of nerve fibers, the task of which is to transmit signals, which ensures the reproduction of motor and sensory functions. The bodies of these neurons live in the nuclei of the brain and spinal cord, thus forming a close connection. From a practical point of view, the peripheral segment of the nervous system combines the so-called “conductors” that connect nerve centers with receptors and functional organs.
When polyneuropathy occurs, a separate part of the peripheral nerve fibers is affected. Therefore, manifestations of the disease are observed in certain areas. The pathology in question on the limbs manifests itself symmetrically.
It should be noted that the pathology under consideration has several varieties, which are classified depending on the functions of the damaged nerves. For example, if the neurons responsible for movement are damaged, the ability to move may be lost or impaired. This type of polyneuropathy is called motor polyneuropathy.
In the sensory form of the disorder in question, the nerve fibers that cause sensitivity are affected, which suffers greatly when this category of neurons is damaged.
Insufficiency of autonomic regulatory functions occurs when autonomic nerve fibers are damaged (hypothermia, atony).
Thus, the following significant factors that provoke the development of this disease are identified: metabolic (associated with metabolic disorders), autoimmune, hereditary, nutritional (caused by nutritional disorders), toxic and infectious-toxic.
There are two forms of the described pathology depending on the location of the lesion: demyelinating and axonal. In the first, myelin, the substance that forms the sheath of nerves, is affected; in the axonal form, the axial cylinder is damaged.
The axonal form of leg polyneuropathy is observed in all types of the disease. The difference lies in the prevalence of the type of disorder, for example, there may be a disorder of motor function or a decrease in sensitivity. This form appears as a result of serious metabolic disorders, intoxication with various organophosphorus compounds, lead, mercury salts, arsenic, as well as alcoholism.
There are four forms, depending on the tendency of the course: chronic and recurrent form of the course, acute and subacute.
The acute form of axonal polyneuropathy often develops within 2-4 days. More often it is provoked by severe poisoning of a suicidal or criminal nature, general intoxication due to exposure to arsenic, carbon monoxide, lead, mercury salts, and methyl alcohol. The acute form can last more than ten days.
Symptoms of the subacute form of polyneuropathy increase over a couple of weeks. This form often occurs with metabolic disorders or due to toxicosis. Recovery usually occurs slowly and may take many months.
The chronic form often progresses over a long period of time, six months or more. The disease usually appears against the background of alcoholism, diabetes, lymphoma, blood diseases, and deficiency of vitamins thiamine (B1) or cyanocobalamin (B12).
Among axonal polyneuropathies, alcoholic polyneuropathy, caused by prolonged and excessive abuse of alcohol-containing liquids, is most often diagnosed. A significant role for the occurrence of the pathology in question is played not only by the number of “absorbed liters” of alcohol, but also by the quality of the product consumed, since many alcoholic drinks contain many substances toxic to the body.
The main factor provoking alcoholic polyneuropathy is the negative impact of toxins that alcohol is rich in on nerve processes, which leads to metabolic disorders. In most cases, the pathology in question is characterized by a subacute course. Initially, numbness occurs in the distal segments of the lower extremities, and severe pain occurs in the calf muscles. As pressure increases, pain in the muscles increases noticeably.
At the next stage of development of the disease, dysfunction of mainly the lower extremities is observed, which is expressed by weakness, often even paralysis. The nerves that cause flexion and extension of the foot are the most damaged. In addition, the sensitivity of the superficial layers of the dermis in the area of the hands, like a “glove,” and the feet, like a “sock,” is disrupted.
In some cases, this disease can have an acute course. This mainly occurs due to excessive hypothermia.
In addition to the above clinical symptoms, other pathological manifestations may also be present, such as a significant change in the color of the skin of the legs and the temperature of the extremities, swelling of the distal parts of the legs (less often the arms), and increased sweating. The disease in question can sometimes affect the cranial nerves, namely the oculomotor and optic nerves.
The described disturbances are usually detected and increase over several weeks/months. This disease can last for several years. When you stop drinking alcohol, the disease can be overcome.
The demyelinating form of polyneuropathy is considered a serious disease, accompanied by inflammation of the nerve roots and gradual damage to their myelin sheath.
This form of the disease is relatively rare. Most often, this disease affects the adult male population, although it can also occur in the weaker half and children. Demyelinating polyneuropathy usually manifests itself as weakness of the muscles of the distal and proximal areas of the extremities, due to damage to the nerve roots.
The mechanism of development and etiological factor of this form of the disease are, unfortunately, not known for certain today, however, numerous studies have shown the autoimmune nature of demyelinating polyneuropathy. For a number of reasons, the immune system begins to consider its own cells as foreign, as a result of which it begins to produce specific antibodies. In this form of pathology, antigens attack the cells of the nerve roots, causing destruction of their membrane (myelin), thereby provoking an inflammatory process. As a result of such attacks, nerve endings lose their fundamental functions, which causes disruption of the innervation of organs and muscles.
Since it is generally accepted that the origin of any autoimmune disease is related to heredity, a genetic factor in the occurrence of demyelinating polyneuropathy cannot be excluded. In addition, there are conditions that can change the functioning of the immune system. Such conditions or factors include metabolic and hormonal disorders, heavy physical activity, infection of the body, emotional stress, vaccination, injury, stress, severe illness and surgery.
Thus, the treatment of polyneuropathy of the lower extremities is represented by a number of features that must be taken into account, because the disorder in question does not arise independently. Therefore, when the first manifestations and signs of the disease are detected, it is necessary to immediately establish the etiological factor, since treatment, for example, of diabetic polyneuropathy differs from the treatment of pathology caused by alcohol abuse.
Treatment
The treatment regimen for lymphadenopathy depends on the disease that caused it. Enlarged lymph nodes in themselves cannot be treated, as they are a symptom of a particular pathology.
Let's look at how diseases accompanied by lymphadenopathy manifest themselves and are treated, and what needs to be done in a particular case.
Tuberculosis of the lymph nodes
The lesion may affect any of the groups of lymph nodes in the neck
It usually develops in children and adolescents (it practically never occurs in adults and older people). Most often the disease affects the cervical and submandibular lymph nodes, less often - the axillary, and very rarely - the elbow and inguinal.
The onset is characterized by a significant increase in body temperature, intoxication, and involvement of the skin and subcutaneous tissue in the pathological process. Lymph nodes increase in size and form large, almost motionless bags.
Lymphadenopathy in tuberculosis quickly turns into lymphadenitis - inflammation of the lymph nodes.
Depending on the nature of the course, tuberculous lymphadenitis is divided into:
- infiltrative, accompanied by an increase in one group of nodes and their compaction;
- caseous, spreading to several groups of lymph nodes and accompanied by cheesy necrosis, suppuration, formation of ulcers and fistulas;
- indurative, characterized by compaction of the lymph nodes with petrification, scarring of the skin at the site of healed fistulas.
Treatment of pathology can be carried out in two ways:
- conservative;
- operational.
The type of medication, as well as its dosage, is selected by the attending physician depending on the nature of the course of the disease.
Surgical treatment is used when conservative treatment is ineffective. In this case, the affected lymph nodes are opened, their contents are removed, the cavity is disinfected and drained.
Occasionally, lymph nodes are excised, but this can lead to relapse of the disease or its spread to other organs and systems of the body.
Infectious mononucleosis
It is a viral disease that develops as a result of infection with the Epstein-Barr virus. The disease is characterized by an acute onset and is accompanied by fever, weakness, headaches, muscle and joint pain, tonsillitis and lymphadenopathy, spreading to the submandibular and posterior cervical lymph nodes (in some cases, the inguinal, axillary and cubital lymph nodes are affected).
Occasionally, acute mesadenitis develops. A quarter of patients develop skin rashes. The liver and spleen usually become enlarged.
Treatment of patients with mild and moderate forms is carried out at home (in this case they are isolated). In more severe cases, they are hospitalized.
In case of liver inflammation, a restorative diet is prescribed - table No. 5.
No specific therapy for the disease has been developed. People suffering from this pathology are given symptomatic, detoxification, desensitizing and restorative treatment.
Antibacterial agents are prescribed only in the presence of bacterial complications. In the presence of hypertoxic lesions and signs of asphyxia, which has developed against the background of enlarged tonsils and swelling of the oropharynx, glucocorticoids are used.
The oropharynx is sanitized with antiseptic solutions.
Prolonged and chronic forms of pathology are treated with the use of immunocorrectors - agents that restore the functioning of the immune system.
Rubella
Take 1 tablet 2-3 times a day
The disease begins with a slight increase in body temperature, a feeling of general malaise, fatigue, drowsiness, and headache. Some patients experience a runny nose, sore throat, dry cough, redness of the throat, and rashes on the soft palate. The posterior cervical and occipital lymph nodes increase moderately in size, and slight pain appears (in some cases, the disease spreads to the parotid, popliteal, anterior cervical and axillary lymph nodes). After a few days, these symptoms are accompanied by a pale pink, small, profuse rash covering the face, chest, limbs and abdomen.
There is no specific treatment for the pathology. Patients are recommended:
- bed rest for three to seven days;
- quality food;
- antiviral agents (Arbidol, Isoprinosine);
- immunomodulators (Anaferon, Cycloferon, Viferon, Interferon, etc.);
- detoxification therapy, including drinking plenty of fluids;
- vitamin therapy – Ascorutin;
- symptomatic therapy - mucolytics, antipyretics, analgesics, antispasmodics and anti-inflammatory drugs.
Hodgkin's lymphoma (lymphogranulomatosis)
It takes development from one lymph node and spreads to others. The affected lymph nodes (usually supraclavicular and mediastinal) increase in size, become densely elastic, and in some cases painful after drinking alcohol (there are no adhesions with the skin).
In addition to lymphadenopathy, patients experience the following symptoms:
- sudden weight loss;
- unexplained rises in body temperature;
- profuse night sweats.
Treatment of pathology is carried out comprehensively and may include:
- radiation therapy;
- chemotherapy;
- bone marrow transplant (in severe cases).
Much attention is paid to preventing relapses of the disease through maintenance therapy.
After recovery and during the remission stage, patients are prohibited from undergoing physiotherapeutic procedures, working in hazardous conditions, or staying in places with high radiation levels.
Non-Hodgkin's lymphomas
They are part of a heterogeneous group of malignant lymphoproliferative neoplasms, differing in biological properties, morphological manifestations, clinical picture, response to treatment, and prognosis.
At the first stage of development, the disease affects one lymph node, then spreads through metastases. The primary tumor focus can be located both in the lymph nodes and in other organs and tissues.
The affected lymph nodes become denser and form conglomerates (adhesion to the skin and underlying tissues, no pain). Enlarged lymph nodes, in turn, compress blood vessels and nearby organs, which is accompanied by the following symptoms:
- superior vena cava syndrome;
- portal hypertension;
- dynamic intestinal obstruction;
- obstructive jaundice.
The main method of treating pathology is chemotherapy using combinations of cytostatic agents. Therapy is carried out in short courses with intervals between them of two to three weeks. If there is no effect, another, high-dose course of chemotherapy is prescribed, followed by hematopoietic stem cell transplantation.
Still's disease
The dosage regimen is individual and depends on the indications, the patient’s condition and his response to therapy.
It is a systemic disease of connective tissue, accompanied by enlarged lymph nodes and spleen, fever, skin rashes, joint pain, and rarely arthritis.
There is no specific treatment for the pathology. Patients are prescribed symptomatic therapy, including:
- non-steroidal anti-inflammatory drugs in the acute period;
- systemic corticosteroids (Prednisolone or Dexamethasone) in the presence of pathological processes in the lungs or the absence of positive dynamics during treatment with non-steroidal anti-inflammatory drugs;
- Cyclophosphamide or Cyclosporin A, which have immunosuppressive, antitumor and cytostatic effects.
Viral hepatitis
In addition to liver symptoms, they are accompanied by lymphadenopathy, fever, lung damage, hemorrhagic vasculitis, Sjögren's syndrome, and polyserositis.
Treatment of viral hepatitis is carried out comprehensively and includes:
- antiviral agents;
- interferons;
- hepatoprotectors;
- antihistamines and hormonal agents;
- antibacterial drugs (rarely, according to indications).
Sarcoidosis
It is a granulomatous inflammation, accompanied by inflammation of the bronchopulmonary (less commonly peripheral) lymph nodes, damage to the lungs and other organs, and suppression of cellular immunity.
Treatment for sarcoidosis is symptomatic and includes:
- hormonal drugs;
- antiviral agents;
- vitamin and mineral complexes.
Tularemia
Tularemia can only be treated in a hospital setting
It is characterized by an acute onset - a significant increase in body temperature, headaches and muscle pain, weakness, lack of appetite, vomiting, regional lymphadenitis. In addition, you may experience:
- delirium, agitation, lethargy (rarely);
- pain in the eye, in the throat when swallowing, behind the sternum, in the abdomen (in the area of the developing bubo).
By the end of the first week of the disease, the liver and spleen enlarge.
Treatment of tularemia is carried out in a hospital setting. Patients are prescribed:
- antibacterial drugs;
- detoxification agents;
- anti-inflammatory and antipyretic drugs;
- antihistamines;
- cardiovascular medications (if necessary).
The ulcerations are covered with sterile bandages, the festering buboes are opened and drained.
Cat scratch disease (benign lymphoreticulosis)
It is an infectious disease that develops after being bitten, scratched or salivated by infected cats. Accompanied by regional lymphadenopathy, quickly turning into lymphadenitis, fever, enlarged liver and spleen.
The disease begins with the appearance of an ulcer or pustule at the site of penetration of the pathogen. 15-30 days after infection, the axillary, cervical or elbow lymph nodes enlarge. They reach three to five centimeters in diameter, become painful, and suppurate (there are no adhesions with surrounding tissues). At the same time, the following appear:
- signs of general intoxication;
- fever;
- enlarged liver and spleen.
Lymphadenitis can persist for several months.
Treatment of pathology is carried out comprehensively and includes:
- antibacterial drugs;
- non-steroidal anti-inflammatory drugs;
- painkillers.
When the lymph nodes suppurate, their contents are sucked out and the cavity is washed with an antiseptic solution.
HIV infection
It develops against the background of infection with the human immunodeficiency virus (HIV), is characterized by a slow course and is accompanied by damage to the nervous and immune systems, the addition of opportunistic infections, the appearance of tumors, and persistent generalized lymphadenopathy (PGL). When progressing to the AIDS stage, it most often ends in death.
The only treatment for HIV is the use of highly active antiretroviral therapy (HAART), which slows the progression of the disease and stops its transition to the AIDS stage.
Polyneuropathy of the upper extremities
This disorder occurs due to damage to the nervous system and leads to paralysis of the upper limbs. With this disease, there is usually symmetrical damage to the nerve fibers of the distal areas of the extremities.
Signs of hand polyneuropathy are almost always the same. Patients experience increased sweating, impaired pain sensitivity, thermoregulation, skin nutrition, changes in tactile sensitivity, and paresthesia in the form of “goosebumps” appears. This pathology is characterized by three types of course, namely chronic, acute and subacute.
Polyneuropathy of the upper extremities is manifested, first of all, by weakness of the arms, various algias, which in their content are burning or bursting, swelling, and occasionally tingling may be felt. With this pathology, vibration sensitivity is impaired, as a result of which patients often experience difficulties in performing basic manipulations. Sometimes people suffering from polyneuropathy experience decreased sensitivity in their hands.
Hand polyneuropathy is most often caused by various intoxications, for example, due to the consumption of alcohol, chemicals, and spoiled foods. Also, the occurrence of the disease in question can be provoked by: vitamin deficiency, infectious processes (viral or bacterial etiology), collagenosis, liver and kidney dysfunction, tumor or autoimmune processes, pathologies of the pancreas and endocrine gland. Often this disease appears as a consequence of diabetes.
The described disease can occur differently in each patient.
According to pathogenesis, polyneuropathy of the upper extremities can be divided into axonal and demyelinating, and according to clinical manifestations into: vegetative, sensory and motor. It is quite difficult to encounter the listed varieties of this disease in their pure form; more often the disease combines the symptoms of several variations.
Types and classification
Neuropathy is classified according to several criteria: the cause of its occurrence, the nature of its course, and the type of damage to the nerve fibers. It can develop against the background of allergies, trauma, inflammation or poisoning.
Acute inflammatory demyelinating polyneuropathy (AIDP) is characterized by rapid progression of symptoms - up to a month after the manifestation of the first signs.
The subacute form of the disease also occurs quite quickly, but less violently: an increase in symptoms is observed over several months. The duration of the disease varies from one month to six months.
The chronic form is understood as a long-term course of polyneuropathy, which slowly progresses over two months or more.
Based on the type of lesion, a distinction is made between demyelinating polyneuropathy itself and axonal demyelinating polyneuropathy, accompanied by the destruction of axons - the long processes of nerve cells. It is the axons that transmit nerve impulses from the cell body (soma) to other nerve cells and innervated organs and structures.
There are 4 atypical forms of chronic neuropathy: distal, focal, isolated sensory and motor. Distal neuropathy affects only the distal parts of the lower and upper extremities; with focal – one or more nerves of the lumbosacral or brachial plexus.
The isolated sensitive form is characterized by damage exclusively to sensory fibers; isolated motor – motor areas.
Treatment of polyneuropathy
Today, treatment methods for the disease in question are quite scarce. Therefore, to this day, the treatment of polyneuropathies of various forms remains a serious problem. The level of knowledge of modern physicians in the field of the pathogenetic aspect and etiological factor of this category of diseases has determined the advisability of identifying two areas of therapeutic intervention, namely undifferentiated methods and differentiated ones.
Differentiated methods of therapeutic correction involve treatment of the underlying ailment (for example, nephropathy, diabetes) for endogenous intoxications; for pathologies of the digestive system caused by malabsorption, they require the administration of large dosages of vitamins B1 (thiamine) and B12 (cyanocobalamin).
For example, diabetic polyneuropathy is treated with drugs and their choice is determined by maintaining a certain glycemic level. Therapy for polyneuropathy due to diabetes should be gradual. At the first stage, you should adjust your body weight and diet, develop a set of special physical exercises, and monitor your blood pressure levels to normal. Pathogenetic methods of therapy involve the use of neurotropic vitamins and the injection of alpha-lipoic acid in large dosages.
Undifferentiated methods of therapeutic intervention are represented by glucocorticoids, immunosuppressive drugs and plasmapheresis.
Polyneuropathy treatment drugs should be prescribed in combination. The specificity of the choice of therapeutic measures for the pathology in question always depends on the etiological factor that provoked the disease and determined its course. For example, the symptoms of polyneuropathy caused by excess levels of pyridoxine (vitamin B6) disappear without a trace after its level is normalized.
Polyneuropathy caused by a cancerous process is treated by surgery - removal of the tumor that was putting pressure on the nerve endings. If the disease occurs against the background of hypothyroidism, then hormonal therapy is used.
Treatment of toxic polyneuropathy, first of all, involves detoxification measures, after which medications are prescribed to correct the disease itself.
If it is impossible to identify or eliminate the cause that provoked the development of the described disease, the main goal of treatment involves relieving pain and eliminating muscle weakness.
In these cases, standard physiotherapeutic methods and the prescription of a number of medications are used to relieve or relieve pain caused by damage to nerve fibers. In addition, physiotherapy methods are actively used at all stages of rehabilitation treatment.
It is quite difficult to overcome algia with the help of analgesic drugs or non-steroidal anti-inflammatory drugs. Therefore, it is more common to prescribe local anesthetics, anticonvulsants and antidepressants to relieve attacks of pain.
The effectiveness of antidepressants lies in their ability to activate the noradrenergic system. The choice of drugs in this group is determined individually, since antidepressants often cause mental dependence.
The use of anticonvulsants is justified by their ability to inhibit nerve impulses emanating from the affected nerves.
Diagnostics
Diagnostic methods depend on the location of the pathology. To prescribe the correct course of treatment, it is necessary not only to make an accurate diagnosis, but also to identify the cause of the progression of the pathological process.
The standard procedure includes:
- UAC and OAM;
- tumor markers;
- Ultrasound of the abdominal organs;
- radiography.
Since PAP is a kind of marker of another disease, the cause of the development of the disease should first be diagnosed.
What is polyneuropathy?
The online magazine psytheater.com calls polyneuropathy a disease of the peripheral nervous system, which is accompanied by two main symptoms: muscle weakness and pain in the affected area. Polyneuropathy is characterized by trophic disorders, vegetative-vascular disorders, flaccid paralysis, and sensitivity disorders. All this is observed in the limbs. If left untreated, the disease will progress, causing an increase in the affected area.
How the disease will proceed depends on the type and its form. Most often, a person experiences severe pain. Treatment is often protracted because there is no quick cure. The disease itself can develop slowly or lightning fast, which is purely individual.
The classification of polyneuropathy is as follows:
- According to the nature of the flow:
- Acute - develops in a couple of days, and treatment lasts several weeks.
- Subacute - development occurs within a few weeks, and therapy lasts for months.
- Chronic – progresses over several months (six months or more), after which the duration of treatment is purely individual.
- By the nature of the lesion:
- Axonal - inflammation is observed in the axial cylinder of the nerve fiber. The axon is the core of the central nerve, which is responsible for its nutrition. For this type of disease, treatment is lengthy, and the prognosis is not always favorable.
- Demyelinating - inflammation affects the myelin sheath of the fiber. Myelin is a special protein that envelops nerve fibers and is responsible for the conduction of signals. During illness, it disintegrates. If this type of disease is treated, then the prognosis is favorable.
- Neuropathic – damage to nerve cell bodies.
- According to the functionality of the affected nerves:
- Sensory – symptoms include numbness, loss of sensitivity, pain and burning.
- Sensorimotor – symptoms manifest themselves in loss of sensitivity and impaired motor functions.
- Motor – the predominant symptoms are loss of motor function: weakness, muscle thinning.
- Vegetative - the disease affects the nerve fibers that are responsible for regulating the functioning of internal organs or for performing certain functions of the body, for example, sweating, dry skin, constipation, rapid heartbeat.
- Mixed - symptoms of damage to all nerves appear.
- For the reasons for the development of polyneuropathy:
- Dysmetabolic – metabolic disorder.
- Inflammatory – inflammatory processes are observed in nerve fibers.
- Allergic – the disease is the result of a malfunction in the immune system.
- Traumatic – resulted from traumatic incidents.
- Toxic – is a consequence of damage to the body by various toxins, for example, lead.
- Idiopathic - the causes are not known to doctors, but it is assumed that the immune system played an important role here.
- Post-infectious – is a consequence of some infectious disease, for example, HIV, diphtheria, etc.
- Hereditary - develops as a tendency of the body to the appearance of the disease in question, since it was also observed in one of the parents.
- Paraneoplastic - the disease develops together with cancer.
- Due to systemic diseases - when polyneuropathy is a consequence of transformation of connective tissue.
Accordingly, what causes provoke polyneuropathy?
- A disorder of the immune system that attacks the body's own cells, producing special cells and antibodies.
- Infections that first develop other diseases and then lead to polyneuropathy. For example, with diphtheria, the nervous system is affected and a film forms in the larynx.
- Heredity - when a person from birth has special disorders that can lead to the development of polyneuropathy.
- Oncological diseases.
- Disturbed metabolism, for example, diabetes mellitus, which is characterized by a constant or periodic increase in blood glucose levels, which has a toxic effect on the condition of tissues.
- Poisoning from organic solvents, heavy metals, drugs or alcohol.
- Systemic diseases that affect the condition of connective tissue.
The most common form is diabetic polyneuropathy. The nerves of the lower extremities are more often affected due to their remoteness, which is why they lack protective barriers and it is quite easy for infectious agents to penetrate through the blood to them.
Any type of disease requires urgent treatment. If there is no therapy, then the disease will begin to progress. This will lead to ulcers or muscle atrophy. The most dangerous consequences of polyneuropathy are paralysis of the legs and arms, then the respiratory muscles.
go to top
Causes of polyneuropathy
The disease can occur due to various factors. In most cases, the cause of the disease is diabetes mellitus type I or II, since the pathology affects the functioning of the vessels that feed the nerves and causes disruption of metabolic processes in the myelin sheath of nerve fibers, which leads to their damage. In diabetes mellitus, the lower extremities are primarily affected.
In rarer situations, the causes are considered to be:
- elderly age;
- AIDS virus;
- AIDS;
- negative environmental conditions or prolonged exposure to toxins on the body;
- alcoholism;
- smoking;
- drug use;
- hereditary and genetic predisposition.
The level of B vitamins is no less important. Long-term deficiency can lead to the development of polyneuropathy. Since vitamins are vital for the proper functioning of the nervous system.
There can be several causes of damage to the nerves themselves:
- poor blood supply to the nerves;
- abnormal deformations of nerve processes.
Symptoms of polyneuropathy
First, the nerve fibers are irritated by pathological agents, and then their functionality is impaired. This is why symptoms are divided into two stages of disease development:
- The period of irritation is characterized by the following symptoms:
- Trembling of limbs.
- Cardiopalmus.
- Painful muscle cramps.
- Feeling of goosebumps crawling on the skin.
- Involuntary contraction of individual muscles, which is visible to the naked eye.
- Increased blood pressure.
- Pain in the skin and muscles.
- The period of loss is characterized by the following symptoms:
- Muscle weakness that begins in nerves distant from the head. So, it may be painful for a person to walk on his heels at first, and then on his toes. Toxic poisoning affects the extensor muscles of the fingers.
- Amyotrophy.
- Unsteadiness of gait with eyes closed, since the supply of information to the brain about the spatial position of the limbs is disrupted.
- Loss of muscle tone.
- Lightheadedness, dizziness and the appearance of spots before the eyes when changing position from horizontal to vertical.
- Decreased sensitivity in the skin, most often localized in the feet and hands.
- Constant pulse rhythm due to loss of nerve regulation of heart functions.
- Dry skin due to loss of sweating functions by the skin.
- Constipation due to loss of functionality of the gastrointestinal tract nerves.
go to top
Types of treatment
Successful treatment of neuropathy is possible only with an integrated approach. The goal of therapy is to restore nerve fibers and conduction of impulses along nerve pathways. To do this, it is necessary to improve tissue nutrition, restore blood circulation and metabolic processes. Improvements can be achieved by combining different types of therapy. It is also necessary to treat the underlying disease.
Drug therapy
The patient is given a course of treatment with the following medications:
- vasoactive drugs to improve tissue nutrition (Trental, Emoxipin, Nicotinic acid and others);
- antioxidants (vitamin E, Actovegin, Mexidol, etc.);
- B vitamins to improve conductivity and restore nerve sheaths;
- anticholyesterase drugs that improve the conduction of nerve impulses (Amiridine, Epidacrine);
- Muscle relaxants are used with some caution to restore muscles (Mydocalm, Baclofen), but it should be remembered that they are not suitable for all patients (they can increase muscle weakness);
- non-steroidal anti-inflammatory drugs (Nimesulide, Ketoprofen, Meloxicam), as well as ointments and patches containing them (Lidocaine ointment, Voltaren patch and others) are used for pain relief;
- antidepressants (Duloxetine, Sertraline, Ketadolon);
- anticonvulsants (Pregabalin, Neurontin);
- in severe cases, narcotic painkillers (Tramadol, etc.) are prescribed to relieve pain.
In addition to the listed medications, the patient is prescribed drugs and procedures to combat the underlying disease. In the case of diabetes, these will be drugs that correct blood sugar levels. For toxic neuropathy, measures are taken to cleanse the body of toxins. For pathologies of the thyroid gland, autoimmune diseases, hormonal therapy is possible, and so on.
Physiotherapy
Physiotherapeutic procedures are designed to “develop” the leg, returning lost functions to its muscles, ligaments, and nerves. For this purpose the following may be prescribed:
- massage,
- acupuncture;
- physiotherapy;
- mud therapy;
- electrophoresis;
- magnetotherapy.
For treatment of neuropathy to be successful, the patient needs persistence, patience and a great desire to be healthy. A prerequisite is to get rid of alcohol consumption and other bad habits, adherence to a daily routine, and a healthy diet. For some diseases that cause leg neuropathy, a strict diet is indicated (diabetes, kidney disease, etc.).
Polyneuropathy of the upper extremities
The upper extremities can also become an affected area. Symptoms of polyneuropathy are manifested in impaired pain sensitivity, increased sweating, skin nutrition, thermoregulation, changes in tactile sensitivity, and paresthesia in the form of “goosebumps.”
A person feels weakness in his arms. Burning, bursting, and swollen algias occur. Tingling of hands appears. The person also loses the ability to perform basic manipulations.
Each patient's symptoms proceed according to their own scenario. It is difficult to identify clear forms of the disease, since they are often mixed.
go to top
Prevention
To reduce the risk of developing demyelinating polyneuropathy, the following measures are taken:
- for work involving toxic substances, use protective clothing;
- do not drink alcohol;
- take medications only as prescribed by a doctor;
- lead an active lifestyle;
- the menu includes vegetables and fruits;
- prevent acute diseases from becoming chronic;
- monitor health status.
Polyneuropathy of the lower extremities
The lower extremities are most often affected due to their distance from the brain. Polyneuropathy manifests itself in muscle pain, weakening and loss of movement functions, as well as nerve sensitivity. The nerves supplying the feet are predominantly affected. This leads to the fact that over time a person not only loses sensitivity, but also loses the ability to move independently.
Treatment of lower extremities with polyneuropathy becomes lengthy and almost never gives complete recovery. The disease is progressive and therefore always develops a chronic form.
Self-medication in this case will be ineffective. When the first symptoms of the disease appear, you should consult a doctor to identify the causes of its development and ways to eliminate it.
go to top
Prognosis of polyneuropathy
The disease is very dangerous for human health. Since it never goes away on its own and requires long-term treatment and rehabilitation. If the disease is allowed to develop, the consequences will be quite severe.
Prolonged muscle weakness quickly leads to a decrease in muscle tone, and then to complete muscle atrophy. In turn, this is dangerous with the risk of ulcers.
If the disease is ignored for a long time, polyneuropathy can result in complete paralysis of the limbs or respiratory system. A progressive disease causes a lot of inconvenience to the victim, forcing him to change his usual lifestyle, as people lose the ability to move independently and take care of themselves in everyday life. This can lead to problems with nerves, increased anxiety and depression. Therefore, it is important for the patient to receive timely help from a specialist - a psychologist.
How to treat polyneuropathy?
A doctor should treat polyneuropathy. First, he will diagnose the disease in order to find out the possible causes of its occurrence, as well as determine the form of its course. Diagnostics include:
- Collection of complaints and medical history: how long ago the symptoms appeared, whether the person drinks alcohol, whether there was polyneuropathy in relatives, whether the patient has diabetes, the connection of the profession with toxins.
- External examination of the functionality of the affected limbs. Sensitivity and motor activity are revealed.
- Blood test for levels of toxins, glucose, antibodies, etc.
- Electroneuromyography.
- Nerve biopsy.
Treatment is aimed primarily at eliminating the causes of polyneuropathy:
- Replacement therapy for kidney problems.
- Reducing glucose levels in diabetes mellitus.
- Refusal of alcohol.
- Limit contact with toxins.
- Elimination of infectious diseases.
- Removal of tumors by surgery.
Additional treatment methods are:
- Improving the nutrition of nerve fibers by taking B vitamins and metabolites.
- Taking medications to lower blood pressure, painkillers to relieve pain, wearing special orthoses for muscle weakness.
Drug treatment can be supplemented with instrumental treatment:
- Physiotherapy.
- Reflexology.
- Magnetotherapy.
- Treatment massage.
- Stimulation of nerve fibers.
Knowing the causes of polyneuropathy, you can prevent its development using preventive measures, which include:
- Refusal of alcohol.
- Monitoring blood glucose levels.
- Taking medications to eliminate toxins.
- Take medications only as prescribed.
However, prevention will not always help in preventing the development of polyneuropathy if, for example, a person has a genetic predisposition.
go to top
Prevention of polyneuropathy
To prevent polyneuropathy of the upper extremities, you should categorically avoid drinking alcoholic beverages, smoking, and drugs, and regularly monitor glucose levels, even in the absence of diabetes. When working with potentially hazardous and toxic substances, you should use personal protective equipment to protect the body from the harmful effects of toxins.
It is recommended to lead a calm and relaxed rhythm of life, avoid stressful situations and emotional overloads that can directly affect the nervous system, adhere to proper nutrition and lifestyle, and constantly listen to the state of the body and personal feelings in order to prevent a relapse.
For the purpose of prevention after recovery and relief of symptoms of the disease, it is recommended:
- wear loose shoes that do not pinch your feet and do not interfere with proper blood flow;
- do not walk long distances;
- do not stand in one place for a long time without changing position;
- wash feet and hands in cool water to promote greater blood flow to distal areas.
Do not ignore physical therapy, which is necessary to ensure that the muscles of the body are always in good shape. Regular exercise will help prevent muscle atrophy and strengthen the body, restoring strength and flexibility.
It is worth remembering that it is impossible to prevent the development of polyneuropathy. You can minimize the risk of occurrence by using simple precautions. That is, when working with toxic substances, use appropriate protection to prevent damage, take medications only after a doctor’s prescription and do not self-medicate, and treat any infectious diseases in a timely manner and keep them under control, not letting them take their course. Thanks to a balanced diet rich in vitamins, regular physical activity and complete abstinence from alcohol, you can significantly reduce the risk of the disease and extend your life.
Author
Svetlana Vladimirovna Shcherbakova
Anesthesiologist-resuscitator, cardiologist
Treatment of idiopathic facial neuropathy
Treatment is prescribed only after confirmation of the diagnosis by a medical specialist. Hormones, diuretics, antispasmodics, vasodilators, analgesics are indicated. From 5-7 days - physical therapy, B vitamins, anticholinesterase drugs. In the subacute period - therapeutic exercises and facial muscle massage.
Essential drugs
There are contraindications. Specialist consultation is required.
- Metipred (systemic GCS). Dosage regimen: in the first hours and days of the disease, pulse therapy is used in a dose of 1.0 g intravenously, in the morning for 3 days daily. Next, the patient takes Metypred orally at a dose of 1 mg/kg body weight for 5 days, after which the dose is gradually reduced by 5 mg every day.
- Diacarb (a diuretic from the group of carbonic anhydrase inhibitors). Dosage regimen: adults are prescribed 250-500 mg once in the morning for 3 days, on the 4th day - a break.
- Xeomin (muscle relaxant). Dosage regimen: injection of small doses of the drug into areas of synkinesis and contractures. A 2-3-stage administration is used with an interval of 10-12 days. The total therapeutic dose is 1/3-1/2 of the dose contained in 1 bottle of the drug. The duration of the therapeutic effect is 3-4 months.
- Milgamma (B complex of vitamins). Dosage regimen: therapy begins with 2 ml intramuscularly 1 time per day for 5-10 days. Maintenance therapy - 2 ml IM two or three times a week.
Classification
Nerve fibers consist of myelin sheaths, and inside are axons. This variety is divided into 2 subcategories:
- When the membranes are deformed, symptoms develop more rapidly. More damage occurs in sensory and motor nerve tissues. The transformation in the vegetative sections does not appear very clearly. Deformation is observed in the proximal and distal processes.
- Axonal ones are destroyed slowly. Damage to autonomic nerve fibers is observed. Muscle tissue atrophies faster. First, the disease spreads to the distal parts.
Based on location they are distinguished:
- Distal. In such a situation, your legs may be damaged.
- Proximal - lesions are observed in parts of the legs located higher.
Classification by reason of occurrence:
- Dysmetabolic. It appears as a result of disorders in the course of processes in nerve tissues, provoked by substances produced in the body as a result of the development of certain diseases. When pathologies spread in the body, substances spread simultaneously with the blood.
- Toxic polyneuropathy of the arms and legs occurs when using toxic drugs such as mercury, lead, and arsenic. Often used when using antibiotics.
- The most common type of polyneuropathy is considered to be the alcoholic form . It is characterized by increased pain, insufficient ability to move on the legs, and poor sensitivity. The muscles begin to noticeably atrophy.
- Diabetic polyneuropathy of the arms and legs appears in patients with diabetes and develops over a long period of time, about 5-10 years. Spots appear on the skin, a burning sensation on the feet.
Stages of development:
- Primary – hereditary predisposition and idiopathic variety like Geyhan-Barré syndrome.
- Secondary polyneuropathy appears after poisoning of the body, with metabolic pathologies, infections.
Clinical picture
Autonomic neuropathy occurs differently in each patient. Some patients do not suspect for a long time that their autonomic system is not functioning properly, and the symptoms that arise are perceived as a minor malfunction in the body.
For others, autonomic disorder becomes a real torment, as the symptoms become pronounced and prevent them from leading a full life.
There are two forms of the disorder:
- Acute – characteristic of poisoning, acute porphyria, botulism, autoimmune lesions. With the acute development of the disease, symptoms appear suddenly and rapidly increase.
- Chronic - its development is said to occur in hereditary disorders, diabetes mellitus, amyloidosis, and infections. In this case, symptoms appear gradually over several months.
Experts also distinguish two types of neuropathy based on the number of affected fibers:
- Mononeuropathy - damage is localized to only one nerve.
- Polyneuropathy – multiple lesions of nerve fibers are observed.
Symptoms of autonomic neuropathy appear in the form of disorders of the vascular digestive, urinary and reproductive systems. Other autonomic disorders may also be observed.
What symptoms are characteristic of autonomic neuropathy:
- From the digestive system: vomiting, nausea, bloating, increased gas formation, heartburn, diarrhea.
- From the urinary side: urinary incontinence, frequent and false urge to urinate.
- Vascular disorders: arrhythmia, orthostatic hypotension, dizziness.
- From the genital area: decreased libido, in women – absence of orgasms and low vaginal secretion, in men – erectile dysfunction and ejaculation.
These symptoms may be accompanied by:
- the appearance of spots before the eyes when standing up suddenly;
- fainting;
- increased sweating;
- heat intolerance;
- disturbances in visual functions.
The most serious complications:
- Parkinson's syndrome;
- amyotrophy;
- convulsive syndrome;
- gastric paresis;
- death.
httpv://www.youtube.com/watch?v=embed/5x456hMTJ_s
Symptoms
Symptoms of polyneuropathy may include:
- Gradual onset of numbness and tingling in the legs or arms that may spread up the arms and legs
- Sharp stabbing or burning pain
- Increased sensitivity to touch
- Lack of coordination and falling
- Muscle weakness or paralysis if motor nerves are damaged
If autonomic nerves are involved, symptoms may include:
- Heat intolerance, as well as changes in sweating
- Digestive, bladder, or bowel problems
- Changes in blood pressure, which may cause dizziness
Polyneuropathy symptoms, diagnosis and treatment principles
This concept means a severe neurological disorder characterized by damage to peripheral nerves. Pathology is found in people of different ages, but few know how to deal with it.
Symptoms of the disease
The disease affects most of the peripheral nerves of the human body. Polyneuropathy is characterized by the following symptoms:
- decreased sensitivity;
- lack of reflexes;
- limbs become very weak;
- severe pain throughout the body;
- periodically goosebumps and burning sensations appear;
- muscles twitch involuntarily;
- swelling of the hands and feet;
- dyspnea;
- dizziness;
- lack of coordination;
- wounds heal very slowly.
Symptoms can be either strong or mild. Sometimes the disease develops over years, while in others polyneuropathy progresses rapidly. According to statistics, the disease is diagnosed in 2.5% of people. However, among the elderly population this figure is much higher and equals 8%. This may be due to age-related changes in the human body.
Why does polyneuropathy occur?
A number of factors and other diseases provoke the occurrence of polyneuropathy:
- toxins;
- previous infection;
- diabetes;
- deficiency of B vitamins;
- Guillain-Barre syndrome;
- injuries;
- osteochondrosis;
- genetic predisposition.
Sometimes the disease can begin during pregnancy. Doctors explain this by saying that an inadequate reaction of the body to the fetus can lead to a malfunction of the immune system, toxicosis and deficiency of B vitamins. All these disorders during pregnancy can trigger the occurrence of polyneuropathy.
Types of disease
Doctors distinguish several types of this disease, each of which has certain characteristics:
- motor polyneuropathy begins with muscle weakness and leads to muscle atrophy;
- sensory polyneuropathy manifests itself in the form of tingling, goosebumps, burning;
- autonomic polyneuropathy is characterized by increased pallor of the skin, a person suffers from rapid heartbeat and digestive disorders;
- sensorimotor polyneuropathy combines muscle weakness and tingling;
- mixed polyneuropathy is distinguished by the fact that the patient has all the symptoms of the types described above, and is the most severe form of the disease.
Different types of polyneuropathy have their own methods of combating the disease. The sooner the patient begins treatment, the faster he will recover. Otherwise, the consequences can be quite serious. With the progression of polyneuropathy:
- muscle atrophy occurs;
- ulcers appear;
- paralysis of the limbs and respiratory organs is diagnosed;
- the patient loses the ability to walk, the person cannot move independently;
- Anxiety and depression appear, which can lead to mental disorders. The patient becomes withdrawn and closes himself off from the outside world. Due to polyneuropathy, a person may stop communicating with friends and become lonely.
Diagnostics
Diagnosing pathology is quite difficult. This is due to the fact that the symptoms of this disease are similar to other ailments.
httpv://www.youtube.com/watch?v=embed/gsaMYF7gT6Q
It is impossible to determine polyneuropathy only on the basis of patient complaints. It is necessary to apply laboratory and instrumental studies.
Diagnosis begins with the doctor examining the patient's limbs and checking reflexes. Then, various studies are prescribed:
- general blood analysis;
- electroneuromyography;
- nerve biopsy.
This is the only way to accurately determine the presence of the disease.
NEUROPATHY in neurology
NEUROPATHY in neurology
(
neuropathy
; Greek, neuron nerve + pathos suffering; synonym:
polyneuropathy, neuropathy
) - a condition based on damage to the peripheral nerves of a primary degenerative nature, caused by various reasons - intoxication (including alcohol), vitamin deficiency ( B1, B12, pantothenic acid), vascular, autoimmune, neoplastic processes, with certain hereditary diseases. Most often N. occurs in diabetes mellitus, periarteritis nodosa, hron, alcohol intoxication. Compression of nerve trunks and the vessels feeding them in narrow canals (ligamentous, bone) leads to compression-ischemic neuropathies of various localizations - the so-called. tunnel syndromes (see).
Polyradiculoneuropathy (damage to the nerve roots and nerves) with achylia was described by P. M. Sarajishvili in 1946 (see Neuroahile syndrome).
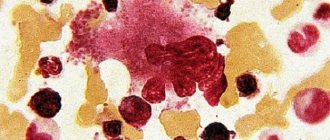
Morphological picture
depends on the type of fibers affected. The pulp fibers undergo axonal degeneration and segmental demyelination. They exhibit hyperplasia of lemmocytes (Schwann cells), the appearance of formations in the form of processes and bulbs. Electron microscopic examination reveals the accumulation of neurofilaments, an increase in the number of mitochondria and dense bodies in the affected and thickened axons. When the soft nerves are damaged, a decrease in the density and diameter of nerve fibers and denervation atrophy in the muscles are possible.
Clinical picture
polymorphic. Motor disorders are manifested by weakness in the arms and legs, mainly in the distal parts, and muscle hypotonia. Sensory disorders are characterized by paresthesia, hypoesthesia, anesthesia or hyperesthesia, pain in the muscles and along the nerve trunks. Dry skin or hyperhidrosis, trophic ulcers, and muscle hypotension are noted. Tendon (usually Achilles) and periosteal reflexes are usually reduced. Characteristic are quantitative and qualitative changes in the electrical excitability of nerves and muscles. Electrical excitability changes little during axonal degeneration caused by exogenous causes. The conduction speed sharply decreases during segmental demyelination, which occurs in certain diseases, in particular hereditary ones - Charcot-Marie-Tooth amyotrophy (see Amyotrophy), Dejerine-Sotta hypertrophic polyneuropathy (see Dejerine-Sotta hypertrophic neuritis), Refsum's disease (see Refsum syndrome), etc.
Diabetic neuropathies have been well studied, which are divided into vegetative and somatic. Vegetative N. occurs in elderly patients with benign diabetes. Their main symptom is pain in the legs, often at night, sometimes in the form of causalgia; Vibration sensitivity is impaired on the legs and less so on the arms, trophic changes in the skin are possible, Achilles and sometimes knee reflexes are reduced. Somatic N. occurs in young people with severe diabetes; they are characterized by sharp pain along the affected nerve, sensitivity disorders of the mononeuritic type and often symptoms of tension in the nerve trunks, for example, ankylosing spondylitis's symptom (see Bekhterev's reflexes, symptoms), Lasegue's symptom and Neri's symptom (see Radiculitis).
N.'s course is usually chronic, but can also be acute.
Diagnosis
established on the basis of anamnesis, a characteristic wedge, pictures, studies of electrical excitability and biopsy (muscles, nerves).
Treatment
. The underlying disease is being treated. In cases of unknown etiology, it is advisable to use vitamins and physiotherapeutic procedures. If conservative treatment of compression N. is ineffective, surgical intervention is indicated.
Bibliography:
Panchenko D.I. Diseases of the nerve trunks, Kyiv, 1966; Sarajishvili P. M. About the so-called neuro-Achilles syndrome (polyradiculoneuritis), Neuropath, and psychiat., vol. 51, century. 5, p. 79, 1951; X o Dosovskaya S.V. On the issue of hereditary polyneuropathies, in the book: Peripheral nervous system, ed. I. P. Antonova, V. 1, p. 126, Minsk, 1978; S 1 uga E. Polyneuropathien, Typen und Differenzierung, B. - NY, 1974.
Diagnosis and treatment
Diagnosis of the disease is based on identifying autonomic disorders and the causes that led to the development of this condition. First of all, the doctor collects anamnesis: the presence of symptoms, what diseases have been suffered, hereditary predisposition.
To identify the cause, it is necessary to take a general blood test and definitely a sugar level test, and consult with various specialists to rule out the presence of concomitant diseases.
The main instrumental diagnostic methods include:
- Orthostatic test.
- Valsalva test.
- Heart rate measurement.
- ECG.
- Nerve conduction study.
- Electromyography.
- Nerve and skin biopsy.
- CT scan.
- MRI.
Additional laboratory tests may be needed for diagnosis:
- cerebrospinal fluid puncture;
- immunogram;
- PCR for infections, antibodies to lupus and other diseases.
If the cause of the disorder is known, then the primary disease is treated first, in particular:
- If you have digestive problems, you should consult a gastroenterologist for nutritional recommendations. To treat autonomic neuropathy, various drugs are used depending on the symptoms that have developed:
- For urinary incontinence, hormones with an antidiuretic effect (Vasopressin) and myotropic antispasmodics (No-shpa) are indicated, and muscle relaxants (Mydocalm) and alpha-1-blockers (Tamsulosin) are needed to relax the sphincter.
- Men with impaired potency need to consult a specialist. In some cases, a vacuum device and stimulant drugs may be required. Women can benefit from special lubricants and ointments containing estrogen.
- For orthostatic hypotension, strong tea and coffee, split meals, increased salt intake and exercise can help. But if these methods are ineffective, drugs that normalize blood pressure (Gutron) are used.
Patients with autonomic neuropathy, regardless of the cause, need to take sedatives and antidepressants (Deprim, Sedafiton), vitamins and mineral complexes.
Physiotherapy and therapeutic exercises can be added to treatment - they have a positive effect not only on the nervous system, but also on the entire body as a whole.
httpv://www.youtube.com/watch?v=embed/9GkAql5HB14
Obvious and hidden dangers of the disease
The consequences will depend on what caused the polyneuropathy. With timely treatment, the prognosis for patients is generally favorable. Complete recovery is almost impossible, however, mortality from polyneuropathy is relatively low. The patient needs constant monitoring by the attending physician.
With a hereditary form of the disease, it is very difficult to improve the patient’s health. The disease progresses slowly, and all the doctor can do is ease its course. Patients are able to quickly adapt to their new condition. Even at later stages they remain capable and continue to care for themselves.
The severe consequences of various types of polyneuropathy include impaired motor activity caused by muscle weakness. In some types of the disease, respiratory problems occur.
Due to dysfunction of the nerves that provide movement of the respiratory muscles, a person practically loses the ability to supply himself with oxygen independently. If the function of the nerves that support cardiac activity is impaired, the patient runs the risk of dying from sudden cardiac arrest. However, such consequences occur infrequently.
Features of therapy
Therapy for polyneuropathy of the lower extremities has its own characteristics; for example, the diabetic form cannot be eliminated by giving up alcohol. Such pathologies do not develop on their own. At the first appearance of symptoms, it is necessary to determine the cause of the disorder.
After this, it will be possible to determine the provoking factors. Therapy for polyneuropathy should be comprehensive and aimed at eliminating the root of this pathology. Therefore, other options will not have the desired effect.
Before therapy, a diagnostic procedure is carried out in which pathology is identified and its cause is determined in order to exclude the possible development of diseases manifested by similar symptoms.
Let's list the drugs:
- Methylprednisolone is used for complex development of pathology.
- Tramadol is used for unbearable pain.
- Vasonite stimulates blood supply to the damaged area.
- Vitamin B.
- Medicines that help saturate cells with micronutrients.
Physiotherapeutic procedures:
- Massage.
- Exposure to magnetic fields.
- Processing the nervous system.
- Indirect treatment of internal organs.
When toxins are detected in the body, you need to cleanse the blood. Doctors often prescribe several physical therapy exercises.
What is peripheral neuropathy?
Peripheral neuropathy is a painful condition that results from damage and dysfunction of the nerves in the peripheral nervous system (PNS).
Peripheral nervous system
In addition, the peripheral nervous system can effectively help the central nervous system work, as it has an extensive nervous network.
Nerves are a set of axons, that is, long cylindrical processes of neurons that propagate a nerve signal.
Through its nerves, the PNS communicates with the arms, hands, feet, legs, internal organs, mouth and face. Cranial nerves and spinal nerves are part of the PNS and extend from the brain and spinal cord .
Mainly:
- Sensory nerves are the nerve that carries sensory information captured from the periphery. Pain, tactile perception, and proprioceptive sensitivity are just some examples of sensory information.
- Motor nerves are the nerves that control skeletal muscles. They are activated by signals emanating from the central nervous system.
- Autonomic nerves are nerves that regulate automatic body functions such as blood pressure, digestion, or bladder filling/emptying.
Treatment options and prognosis
The main component of the treatment of the disease is the restoration of damaged nerve fibers. Treatment of pathology is aimed at providing the nerve with the necessary amount of blood and beneficial microelements, as well as eliminating destructive factors.
First of all, with this disease, it is necessary to identify the cause that provoked its occurrence, and only then move on to eliminating the disease itself.
httpv://www.youtube.com/watch?v=embed/BPGg8RW2izw
Treatment regimen
Peripheral neuropathy of the upper and lower extremities is treated comprehensively. For this purpose, the following methods are used:
- drug treatment;
- physiotherapeutic procedures;
- physiotherapy.
The basis of drug therapy is taking medications such as:
- Neuromidin and Prozerin, which help restore sensitivity to the affected area or limb.
- Meloxicam and Diclofenac, which help cope with pain.
- Pentoxifylline and Instenon, which improve blood circulation.
- Alpha Tocopherol to eliminate vitamin deficiency.
- Carbamazepine, which has the property of relieving muscle cramps.
In addition to these medications, peripheral neuropathy is treated with:
- antidepressants (Deprim);
- decongestants (Furosemide);
- antioxidant drugs (Mexidol).
Additional methods include procedures such as:
- massage;
- electrical stimulation;
- acupuncture;
- mud baths;
- magnetic therapy;
- medicinal applications;
- Darsonvalization.
httpv://www.youtube.com/watch?v=embed/gzoeqM2S1Ew
Therapeutic gymnastics consists of a set of special physical exercises aimed at eliminating the symptoms of the disease and restoring the functionality of the affected area of the face or limb.
Possible consequences
If peripheral neuritis is detected in time and proper treatment is started, the prognosis will be favorable. Recovery largely depends on the patient himself, that is, on his actions aimed at combating pathology.
As a rule, peripheral nerves have the ability to recover on their own, but if the cause that caused the development of the disease is not eliminated, the disease can return again, even after quality treatment.
In cases where the disease is genetic in nature, therapy rarely leads to a complete cure. Even with complex treatment, it is most often possible to only temporarily eliminate the symptoms of the disease, but most often it is not possible to completely restore the affected nerve.
The most dangerous can be considered the diabetic form of pathology, which can affect most parts of the body, causing serious complications.
Diabetic neuropathy
For example, when a nerve related to the digestive system is damaged, the functions of the stomach are disrupted, causing bloating, diarrhea, vomiting and nausea. When the lower extremities are affected, the disease contributes to deterioration of blood flow, the appearance of ulcers and even gangrene. In the latter case, the limb is amputated.
Peripheral neuropathy is a serious disease that brings extremely negative consequences to the patient. However, it is worth remembering that in most cases it is curable. To achieve positive treatment results, you must seek help from a doctor in time and carefully follow all his recommendations.
httpv://www.youtube.com/watch?v=embed/fFQWq98KXCY
How is any type of neuropathy diagnosed?
The procedure for diagnosing neuropathy:
- Collection of clinical history, analysis of complaints.
- Examination of the legs, assessment of their condition.
- Assessing established symptoms.
- Application of electrophysiological examination methods.
- Other diagnostic techniques: nerve biopsy, skin punch biopsy, non-invasive techniques.
First, the doctor must interview the patient about the main complaints, ask him leading questions, and ask him about the sensations caused by the progressive pathology.
Typical symptoms of neuropathy: paresthesia, tingling, burning sensation, lumbago at rest, severe pain even in the absence of an irritant. It is necessary to find out when the symptoms appeared, what they are associated with, and whether they intensify at night or in the evening.
Examination of the feet and other parts of the extremities is mandatory; it will show the presence of keratosis (calluses) in areas with excess pressure, pay attention to increased dryness of the skin, the presence of ulcerations, and obvious deformities of the feet.
To analyze subjective and objective symptoms, appropriate scales and questionnaires are used. Regardless of the scale used, a visual analysis of the condition of the limbs is carried out. To determine tactile sensitivity, it is convenient to use a monofilament device.
https://feedmed.ru/bolezni/nervnoj-sistemy/perifericheskaya-neyropatiya.html
Pain syndrome is tested by pricking the dorsum of the feet, the area of the terminal phalanx of the finger. To test temperature sensitivity, use a tip-therma type instrument. Tendon reflexes are examined using the classical scheme - first the Achilles, then the knee.
Electrophysiological methods (for example, stimulation electroneuromyography) complement the results of general clinical diagnostics.
They are:
- Non-invasive - objective and reliable;
- Assessing the severity, dynamics, and nature of progression of the pathology;
- Carrying information about the function of nerve fibers, their structural features;
- Carrying out differential diagnosis of neuropathies.
The disadvantage of electrophysiological diagnostics is that it is quite painful.
Causes of the disease
This disease can occur for a number of reasons, but it is not always possible to accurately determine them. Polyneuropathy of the lower extremities has the following main causes:
- inherited causes;
- problems with the immune system that appear as a result of disorders of the body;
- various types of tumors;
- lack of vitamins in the body;
- taking medications unnecessarily or not according to instructions;
- disruption of the endocrine glands;
- kidney and liver problems;
- infections that cause processes that cause inflammation in peripheral nerves;
- poisoning of the body with all sorts of substances.
Prognosis and treatment results
Timely and adequate treatment of CIDP allows for complete or significant regression of the disease in almost 90% of cases. Symptoms persist or worsen in only 10% of patients. The most important prognostic criterion is the duration of the primary increase in clinical signs. If it is more than three months, then health is restored after 12 months. However, very often patients experience a return of symptoms and require long-term maintenance treatment.
Most patients diagnosed with Guyon-Barré syndrome recover within six months to a year. Residual symptoms may be observed in 10-12% of cases. AIDP recurs relatively infrequently, in 4% of cases, death is recorded in 5 patients out of 100. The cause of death can be respiratory failure, infection and pulmonary embolism. The likelihood of death is much higher in people over 65 years of age.