Dysphagia refers to pathologies of the esophagus and larynx. With this condition, swallowing liquids and food is difficult or impossible. The causes may include both disturbances in the functioning of various organs and diseases of a neuralgic nature. To make a diagnosis, a thorough examination is necessary, and therapeutic measures are selected individually for each patient.
Pathology cannot be left without attention, since it is impossible to do without the help of doctors. Doctors at the 24-hour Yusupov Hospital specialize in this pathology and successfully cope with dysphagia of any severity.
Physiology of swallowing
Swallowing while eating is carried out by a person reflexively. This means that we do not think or specifically strain any part of the body to ensure the function of passing food from the mouth to the stomach. Although we can force ourselves by a strong-willed decision to swallow, for example, saliva, a bitter medicine.
In the act of swallowing, physiologists distinguish 3 successive phases:
- oral - initial, controlled, initiated by the centers of the brain, activating the swallowing apparatus with their impulses, while the contents of the mouth extend beyond the palatine arches;
- pharyngeal - ensured by involuntary movements, responsible for the entry of the food bolus into the upper part of the esophageal tube and reflex movement downwards;
- esophageal - occurs inside the esophagus due to peristaltic movements of the muscles, guarantees the transport of contents through the cardiac sphincter into the stomach.
The study of changes during swallowing showed that esophageal dysphagia as a pathological condition is a disorder of either a functional or organic nature at any stage of the process. The disease can be treated correctly only by understanding the type of lesion.
Dysphagia: causes
The causes of dysphagia have different origins. These can be both functional malfunctions in the digestive system, pathological processes in the mucous membranes and tissues of the esophagus, and mental disorders of the patient’s personality. Among the many causes of swallowing disorders, the main ones can be identified:
- Inflammatory processes in the mucous membrane of the esophageal tube - esophagitis. This disease is caused by the systematic reflux of stomach acid into the esophagus, which inevitably destroys the mucous membrane, and this, in turn, leads to discomfort and pain during the process of swallowing food.
- Healed ulcer in the esophageal canal. In the area where it is localized, the esophagus narrows, reducing its diameter, which prevents the normal passage of food masses.
- Tumors , benign or oncological in nature. Neoplasms can be localized both in the esophageal tube itself and in neighboring organs. Tumors put pressure on the esophageal walls and make it difficult to swallow food.
- Pathologies caused by impaired muscle tone and motor disorders. The essence of these disorders lies in the inability of the muscles to perform their main task - to move food through the esophagus. These diseases include: stroke, Parkinson's disease, achalasia, polio, multiple sclerosis and others.
- Inflammatory diseases, bacterial and fungal infections, syphilis, tuberculosis, viruses and abscesses.
- Scleroderma is a pathology of connective tissue. Manifested by atrophy of the mucous membrane of the esophageal tube. Genetic and infectious factors play a role in the origin of this disease, and the disease is also provoked by injuries, hypothermia and endocrine changes in the body.
- Esophageal diverticulum is an abnormal protrusion of the wall of the organ, a sac-like formation against the background of weakness of the esophageal wall. Diverticulitis is characterized by a feeling of food being stuck in the mountain, even between meals.
- Age-related aging of the body. With age, muscle tone noticeably decreases, and since the esophagus is a muscular tube, accordingly, dysphagia often develops in older people.
Causes
Temporary (functional) dysphagia causes excessive stimulation of some cortical centers of the brain. False signals contribute to short-term spastic contractions of the circular muscles of the esophagus. The condition is provoked by mental illness, stress, and strong emotions.
In such cases, people say that the symptoms develop “from nervousness.” In this case, there are no mechanical obstacles to the movement of food.
A similar symptom may occur in a child with a reluctance to eat something, fear, or hysterical behavior.
Nervous dysphagia accompanies other manifestations of neurosis: irritability, tearfulness, insomnia. In such cases, treatment by a neuropsychiatrist is indicated. The use of soothing methods helps to avoid swallowing disorders. Organic causes include diseases of the esophagus and stomach, mouth and pharynx, thyroid gland, heart, and brain.
The most significant lesions of the esophagus include:
Pain in the esophagus after eating
- inflammation (esophagitis);
- narrowing due to scars after a burn (alkali or acid), developmental anomalies, cardiospasm, replacement with connective tissue in scleroderma;
- gastroesophageal reflux disease - the acidic contents of the stomach are thrown back into the lower part of the esophagus, causing inflammation and irritation;
- wall diverticula - saccular protrusions due to the weakening of individual sections of the muscular membrane; they can be congenital or formed as a result of prolonged untreated inflammation;
- tumors of the esophagus, stomach, benign and malignant;
- achalasia cardia - damage to the cardiac sphincter, causing a delay in the passage of food from the esophagus to the stomach;
- injury from a swallowed sharp foreign object (fish bone, small toy, button) or injury to the chest.
The esophagus can be compressed from the outside by enlarged neighboring organs: dilated veins with portal hypertension (liver cirrhosis), aortic aneurysm, hypertrophied heart, tumor coming from the mediastinum, growth of the thyroid gland, strangulation of the hernial opening in the diaphragm.
The most common causes of dysphagia among diseases of the oropharynx are:
- severe tonsillitis with significant enlargement of the tonsils;
- tumors;
- stuck foreign bodies;
- severe swelling as a manifestation of an acute allergic reaction;
- incorrect positioning of teeth, ulcerative stomatitis.
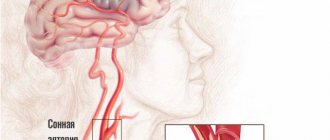
Functional dysphagia must be distinguished from neurogenic dysphagia caused by diseases of the brain (tumors, stroke) and cervical spine. A space-occupying process in brain tissue (including a hematoma) located close to the medulla oblongata, where the swallowing center is located, exerts direct pressure or irritation on neurons and their connections. In addition, impaired blood circulation in certain areas of the brain during an ischemic stroke can lead to paralysis of the pharyngeal muscles.
The nuclei of the medulla oblongata form the respiratory, vasomotor centers, control coughing, vomiting, swallowing and many other body actions
Dysphagia, as a syndrome, is present in patients with Parkinson's disease, multiple sclerosis, cerebral palsy, and myasthenia gravis. Infectious disease doctors observe dysphagia in encephalitis and botulism.
The most common causes of dysphagia and symptoms of difficulty swallowing that accompany these conditions:
1. Neoplasms of the esophagus or tumor formations of adjacent organs , intrathoracic lymph nodes, thyroid gland, which can cause compression of the esophagus. Esophageal cancer is one of the common causes of dysphagia. Dysphagia in tumor oncological diseases is a fairly early symptom, appearing before full-blown systemic manifestations. The symptom of dysphagia in late stages of esophageal cancer is combined with pain during and after eating, loss of appetite, weight loss, and anemia.
Dysphagia in cancer is combined with symptoms of increased salivation, distension in the epigastric zone, painful intractable nausea, repeated retching and self-vomiting. Subsequently, a characteristic symptom is progressive hoarseness and hoarseness of voice, unproductive, ineffective dry cough, difficulty and increased breathing, lymphadenopathy (enlarged lymph nodes), asthenic symptoms.
2. Stenotic transformation of the lumen of the esophagus (narrowing of the esophagus of an organic nature) often leads to symptoms of dysphagia. One of the causes of esophageal stenosis in adults may be post-inflammatory sclerotic changes as a result of scarring of the ulcer. In some cases, narrowing of the esophagus is formed as a consequence of fibrosis during systemic sclerotic processes (systemic sclerosis), in rheumatic diseases, which is manifested by multiple symptoms, including dysphagia.
3. Dysphagia as a consequence of trauma and damage to the esophagus , for example, when injured by a sharp foreign body or bone, is a common symptom. Post-inflammatory or sclerotic changes in the esophagus after chemical (thermal) burns can cause dysphagia and difficulty swallowing. After chemical burns of the esophagus, organic stenoses are common, as a result of which it is possible to consume only liquid food or food products in puree form. Such dysphagia can often be eliminated only by surgery.
4. Cardiac achalasia. Achalasia is a motor-neurogenic disorder of the motor function of smooth muscles of the esophagus. Achalasia cardia is a condition the essence of which is the lack of friendly opening of the esophageal sphincter when food enters the lower part of the esophagus during swallowing, as well as an increase in its tone. As a result, patients feel a feeling of a “lump in the throat”, difficulty swallowing, that is, all manifestations of dysphagia.
Achalasia cardia, the main symptom of which is dysphagia, goes through a number of stages in its development. At the initial stage of the disease, dysphagia and difficulty swallowing are not constant, and expansion of the lumen of the esophageal tube is not yet observed. With progression, the lumen of the esophagus expands, while its distal part remains narrowed. At the last stage, the cardiac part is constantly narrowed due to sclerosis, the overlying parts of the esophageal tube are sharply dilated (widened), and the passage of food through the esophagus is extremely difficult.
Dysphagia and difficulty swallowing are not permanent at first. More often, the symptom of dysphagia appears when eating in a hurry, with insufficient chewing. Dysphagia in this disease may initially manifest itself paradoxically. Solid foods are easy to swallow, while liquids cause dysphagia. Stress and certain types of food, especially those high in fiber, can cause dysphagia.
Dysphagia with achalasia cardia is not the only symptom. Often, discomfort and heaviness behind the sternum, pain localized behind the sternum, and a feeling of fullness in the abdomen (in the epigastric region) are simultaneously observed. In the presence of prolonged stagnation of food in the esophagus, along with dysphagia, its return into the oral cavity (regurgitation) is observed. This can be facilitated by an increase in intra-abdominal pressure, bending forward, or lifting heavy objects. Nocturnal reflux of esophageal contents can result in food entering the respiratory tract (pneumonia, asthma and bronchitis are possible).
Prolonged presence of food in the esophagus leads to its inflammatory transformation, which is manifested by pain, rotten belching, esophageal vomiting, bad breath, weight loss, dysphagia at this stage is constant.
5. Esophagospasm (segmental or total). The cause of the spasm is a violation of the nervous regulation of esophageal myocytes. When there is spasm of the esophagus in a limited area of the organ, the patient is bothered by dysphagia and moderate pain with different localization. Dysphagia and pain do not start and stop abruptly. If the esophagus is spasmed along its entire length, the symptoms of the disease are more vivid, the pain is extremely pronounced, localized behind the sternum, radiating to the epigastrium, reminiscent of the pain of angina pectoris. The difference is the clear connection between symptoms and pain with food intake. An attack of pain and dysphagia can last several hours and decrease with swallowing water and regurgitation. Liquid foods and water are more likely to cause dysphagia (dysphagia paradox). Changing body position and taking antacids can reduce pain and dysphagia.
6. Esophageal diverticulosis (single or multiple) often leads to dysphagia and other painful symptoms (esophageal pain, heartburn, regurgitation and belching). A diverticulum can be compared to a sac-like formation localized in any area of the esophagus, the wall of which is all layers of the esophageal tube. During meals, food debris, epithelium, and protective mucus are deposited in the diverticulum. When food remains in the saccular formation for a long time, conditions are created for the proliferation of bacteria and subsequent inflammation. Inflammation is aggravated by mechanical compression of the esophagus by the diverticulum itself, which inevitably manifests itself as dysphagia and symptoms of difficulty swallowing.
7. Esophagitis can often lead to dysphagia . Esophagitis can develop as a result of long-term nutritional errors (rough, spicy, hot foods, strong alcohol). The peptic factor in the form of constant irritation of the esophageal mucosa with hydrochloric acid and pepsin is one of the main causative factors of chronic esophagitis. Long-term esophagitis, especially erosive and ulcerative, leads to hypertrophy and dysplasia of the esophageal epithelium, swelling of the mucous and submucosal layer. These pathological changes are reflected in the form of dysphagia. Dysphagia is felt as a “lump in the throat, behind the sternum,” fullness, discomfort along the esophagus. During periods of exacerbation, dysphagia intensifies and is combined with other symptoms (typical pain associated with eating, burning and heartburn).
8. Reflux (reverse reflux) of stomach contents , which are acidic in nature, into the lumen of the esophagus. The epithelium of the esophagus throughout its entire length has reduced resistance to aggressive gastric juice. Prolonged aggression by hydrochloric acid and the substance pepsin of the esophageal epithelium inevitably leads to gastroesophageal disease , which is based on reflux (GERD), which is often manifested by symptoms of dysphagia.
9. Hernia of the opening of the diaphragm, through which the esophagus from the chest cavity enters the abdominal cavity (HH) . Normally, only the esophageal tube passes through this physiological opening, which is small in size. A diaphragmatic hernia is formed if, for one reason or another, the hole in the diaphragm becomes larger and allows part of the stomach (sometimes quite significant) into the chest cavity. A hernia creates significant discomfort, and patients experience symptoms of heaviness in the chest, pain along the esophagus, difficulty swallowing, a feeling of a lump, hiccups, sour taste, difficulty breathing and dysphagia.
Esophageal hernias are formed with prolonged increased pressure in the abdominal cavity (obesity, heavy lifting, prolonged constipation and abdominal wall tension) in combination with weakness of the connective tissue formations of the said area.
10. Difficulty swallowing in childhood (from birth) occurs with congenital defects in the formation of internal organs and the formation of hollow structures (esophagus) . The most common such anomalies include stenosis, narrowing, cysts, congenital esophageal diverticula, and esophageal-tracheal fistulas. Dysphagia in infants manifests itself from birth with uncontrollable vomiting, inability to eat, and weight loss.
11. Hysteria, neuroses and neurotic reactions are often accompanied by subjective sensations of difficulty swallowing in the absence of an organic cause. Dysphagia is most often manifested by the fact that the patient cannot swallow water; eating solid food is not accompanied by dysphagia.
12. A rare cause of dysphagia can be inflammation of the pharynx and larynx of various origins , in which dysphagia may be present along with cough and sore throat. As a rule, dysphagia is reversible after relief of inflammation and swelling in these organs.
13. Dysphagia when a foreign body is in the esophagus is the main symptom of this pathological condition, requiring urgent (urgent) measures.
14. Dysphagia with damage to the muscles and nervous system - conditions not associated with dysfunction of the digestive system. Difficulty swallowing often complicates strokes (cerebrovascular accident), myopathy, and neurodystrophy.
Classification
Depending on the duration of the signs of dysphagia, acute and chronic stages of the disease are distinguished. In addition to functional and organic dysphagia, forms of the disease are distinguished depending on the level of damage to the act of swallowing.
Oropharyngeal or oropharyngeal - the entry of a bolus of food into the upper part of the esophagus is disrupted due to problems in the muscular apparatus of the pharynx, innervation, in neighboring tissues (occurs in 80–85% of patients). In young people, it is more often associated with diseases of an inflammatory nature, the development of connective tissue membranes, and ring-shaped formations. In old age, the cause is cerebrovascular disorders (stroke, parkinsonism, senile dementia).
Esophageal - caused by obstructed passage of food through the esophageal tube, divided into middle and lower. Some authors also identify a pharyngoesophageal form, in which changes concern the involuntary phase of rapid swallowing.
Depending on the course, dysphagia can be:
- constant;
- intermittent (appears from time to time);
- progressive – there is a gradual deterioration in the patient’s condition.
Treatment of dysphagia
Therapy is prescribed after diagnostic measures have been carried out. Depending on the type of pathology, treatment can be medication or surgical interventions.
Medications
- If the cause of the pathology is increased acidity of the gastric juice, medications are prescribed that reduce its levels - Almagel, Phosphalugel, Zantac.
- In case of pathology caused by bacterial infections, antibiotics are prescribed, the group of which is determined by the doctor. This could be Ceftriaxone, Levobax, Levoximed.
In addition, anti-inflammatory drugs and medications that eliminate the present symptoms - antiemetics, painkillers and other pharmacological groups - can be prescribed.
Operation
Surgery is used if there is no therapeutic effect from drug therapy. Most often, manipulations are performed for dysphagia caused by cancerous tumors, chemical burns of the esophagus, or severe inflammatory lesions. After surgery, the patient requires bed rest in a hospital setting.
Diet therapy
Diet therapy is also important for dysphagia. It involves eating frequent meals in small portions. During the rehabilitation period it is necessary to exclude:
- Alcohol products;
- Fatty, fried, spicy foods;
- Fast food products;
- Smoked meats, saltiness, spices and herbs.
While eating, food must be chewed thoroughly, avoiding swallowing large pieces.
The disease is quite dangerous and requires a competent approach from a certified specialist. In this case, it is important to choose the right doctor, because the final result and prognosis depend on this. With incorrect manipulations, there is a risk of developing aggravating consequences and the pathology becoming severe.
By turning to the Yusupov Hospital, the patient provides himself with safe and effective treatment without complications, which is guaranteed to lead to quick relief from severe pathology. In addition, in the clinic you can undergo a rehabilitation course under the close supervision of a doctor and prevent the recurrence of dysphagia.
Medicines are taken only in consultation with a doctor. Self-medication in all cases aggravates the situation and leads to dangerous complications.
How it manifests itself
Depending on the cause, impaired swallowing by category can be considered as a separate pathology (primary) or dysphagia syndrome in a specific disease (secondary). Disrupted act of swallowing food causes:
- pain behind the sternum and in the epigastric area;
- belching of food and air;
- heartburn due to regurgitation (return of contents from the stomach), especially when bending forward, at night, if dinner occurs late;
- hoarseness (dysphonia);
- increased salivation;
- feeling of lack of air.
Patients usually complain of difficulty swallowing tough, solid foods, improvement when drinking or switching to liquid meals. Due to disrupted connections and the sequence of physiological processes of swallowing, the contents of the mouth do not enter the esophagus, but into the respiratory tract (nose, larynx, trachea). In response, a spastic contraction, paroxysmal cough, and suffocation develop.
With the oropharyngeal form of the disease, patients always point to the area of the neck and throat that causes difficulty
Symptoms
The swallowing reflex is often impaired after a stroke. Whatever the cause of this phenomenon, a person experiences the following symptoms:
- Unable to swallow solid food. In severe cases - liquid, saliva.
- Reflux occurs and stomach contents flow back into the esophagus and throat.
- There is a feeling of a lump in the throat due to the fact that the sour contents penetrate the throat and burn the mucous membrane.
- When swallowing, there is a feeling of lack of air.
- After eating there is a feeling as if it is stuck in the throat.
- There is a sore throat and shortness of breath.
How is the severity of pathology determined?
The disease is distinguished into certain degrees of dysphagia based on a detailed description of patient complaints:
- I - a person experiences difficulties only when eating dry food or solid foods;
- II - it is impossible to swallow dry and solid food, but semi-liquid and liquid food passes freely;
- III - you can only swallow liquids;
- IV - absolutely impossible to swallow anything.
Depending on the degree, dysphagia treatment tactics are developed.
Treatment and diagnosis of dysphagia
Thus, each type of dysphagia requires an individual approach and treatment depending on the cause that causes it. Difficulty in swallowing, caused by an organic lesion (tumor, stenosis, narrowing, diverticulum), requires surgical (combined) treatment. In case of inflammation or ulcerative lesions , treatment aimed at stopping this process will bring relief to the patient and the disappearance of the painful symptoms of dysphagia. Functional pathologies of the neuromuscular regulation of esophageal tone require complex treatment, including the use of pharmacological and psychotherapeutic methods of treatment.
Diagnostic approaches to clarify the nature of dysphagia are dictated by the patient’s accompanying complaints. X-ray (using barium contrast) and endoscopic (EGD) imaging techniques are used to identify the cause of dysphagia. The diagnosis is clarified using R-graphy of the lungs, ultrasound of adjacent organs, blood vessels, and examination of the composition of peripheral blood.
Important!!! Dysphagia can be a symptom of a serious disease, the effectiveness of treatment of which depends on timely consultation with a doctor.
Why does it occur in children?
A feature of dysphagia in childhood is its connection with a disorder of underdeveloped nervous regulation of swallowing. The disease can be congenital or acquired. Often accompanies cerebral palsy and developmental anomalies.
Constant spitting up should cause concern for parents
Parents can suspect the first signs in infants by slow eating, refusal of nipples with a large hole, choking and coughing when eating quickly, better condition with slow feeding, adjustment of the baby's head before sucking, milk flowing into the nose. Less commonly, the pathology is detected against the background of frequent bronchitis and pneumonia, bronchial asthma.
Prevention of dysphagia
In order to reduce the likelihood of developing pathology, you must follow simple rules and recommendations:
It is important to promptly treat conditions that can lead to swallowing problems.
- Maintaining a healthy lifestyle - giving up alcohol and smoking.
- Maintaining proper nutrition - excluding fried and canned foods, too hot foods and including fruits, herbs and vegetables rich in fiber in the diet.
- Eliminating the risk of foreign objects entering the esophagus.
Diagnostics
Diagnosis of both forms of dysphagia requires a thorough interview of patients in order to clarify symptoms, identify connections and causes, and establish the level of damage to the act of swallowing. General blood, stool, and urine tests help identify the primary disease that contributes to dysphagia. Therefore, they should be carried out for differential diagnosis.
The results of liver tests and ECG must be studied. To identify the oropharyngeal form, the main criteria are obtained using:
- Screening test - the patient is given to drink 150 ml of water as quickly as possible, at which time the doctor counts the number of sips and time. The data obtained allows us to calculate the rate of swallowing and the volume of the sip (average). Diagnostic accuracy, with a decrease in both indicators, ensures correct diagnosis in 95% of cases.
- Fluoroscopy studies of the upper esophageal sphincter during barium swallow.
- Laryngoscopy is a technique for examining the posterior wall of the larynx.
Esophageal dysphagia is particularly difficult to identify due to the need to exclude many diseases that contribute to the formation of a mechanical obstruction. First of all, the doctor must make sure that there is no malignant process.
The tumor is favored by the duration of dysphagia for more than four months, the progressive course, severe symptoms when eating solid food rather than liquid, and the patient’s weight loss. X-ray examination with contrast reveals disrupted contours of the esophagus, signs of an ulcer or neoplasm, diverticulum, achalasia and other organic pathology.
Endoscopic detection of tumors and disruption of the internal structure of the esophagus
Esophagogastroduodenoscopy - allows you to visually examine the inner surface of the esophagus, stomach and duodenum, and take questionable tissue for examination for biopsy. The motor function of the esophagus is checked with a four- or eight-channel device (water-perfusion catheter), which, like a manometer, measures the tone of the upper and lower esophageal sphincters and the thoracic region.
The technique used in specialized centers is considered more accurate. These are high resolution manometry and 3D volumetric manometry. It is possible to obtain not only indicators, but also a color image of peristalsis waves. The method of radionuclide scintigraphy of the esophagus is based on measurements of radioactivity after the patient swallows water mixed with Technetium 99.
If contractility is impaired, the release of the radioactive substance into the stomach slows down.
To conduct a differential diagnosis, you may need an ultrasound examination of the abdominal organs; magnetic resonance imaging of brain structures, electroencephalography of the brain, consultations with a gastroenterologist, neurologist, or otolaryngologist.
Surgical treatment
If medications are not effective, surgical treatment is used. Plastic fundoplication is performed to eliminate acid reflux. Tumors, cysts, and polyps that interfere with the passage of food are removed. The expansion of the lumen of the esophagus with air balloons and the bougienage method is used.
Myotomy of the esophagus is performed through punctures of the abdominal wall - laparoscopy or by penetration into the chest - topacotomy. The surgeon excises the sclerotic area, eliminates adhesions or adhesions, lengthens and widens the lumen of the esophageal tube.
In difficult cases, a gastrostomy tube is installed. A thin tube is inserted through the anterior abdominal wall. There is a cap at the tip of the tube, which is opened to introduce food with a special probe. Often, gastrostomy is the only method of salvation from starvation.
Treatment
In the treatment of oropharyngeal dysphagia with neurological and neuromuscular disorders, there is positive experience with the use of drugs only for myasthenia gravis and Parkinson's disease. In other cases, all therapy is aimed at preventing food from entering the respiratory tract and further complications.
For this, patients are recommended:
- switch to liquid and soft foods;
- adapt to nutrition by choosing a posture.
Swallowing reflexes are activated by adding citric acid to food. Exercises are prescribed to retrain the swallowing act. To suppress the cough reflex, drugs from the group of angiotensin-converting factor inhibitors are recommended. If there is a high risk of aspiration or the impossibility of feeding through the mouth, food is administered by tube.
Stroke patients with oropharyngeal dysphagia have to have a gastrostomy tube (an artificial opening for infusing liquid food directly into the stomach) removed. With the help of surgery, spastic contraction of the laryngeal muscles is eliminated.
Treatment of esophageal dysphagia requires a gentle diet (switching to frequent intake of warm liquid food, in small sips, avoidance of alcohol, fried foods, spices, hot seasonings), prevention of gastroesophageal reflux with the help of drugs that reduce acidity, and anti-inflammatory measures. In case of cicatricial and adhesive processes, the esophagus is bougienage with rubber tubes.
Mechanical obstacles can only be removed surgically. The scope of intervention is determined individually in a particular case.
What other diseases can cause dysphagia?
- Benign tumor or cancer of the pharynx. In this case, in addition to problems with swallowing, there will be discomfort in the throat, a sensation of a “lump”, swallowing will be painful, and such pain will radiate to the ear.
- The pharyngeal “pocket” is a pathology most often of a congenital nature, when the mucous membrane protrudes, forming a pocket. In this case, there will be dysphagia and bad breath, and a protruding pouch will be visible on the neck.
- Stroke. In this case, other symptoms also occur: paralysis of the limbs, facial asymmetry, impaired understanding or reproduction of speech, confusion.
- Encephalitis. Dysphagia occurs against the background of usually impaired consciousness (inadequacy and agitation or stupor), elevated body temperature, and other symptoms of brain damage: breathing problems, decreased blood pressure.
- Botulism. In addition to difficulty swallowing, there is double vision, the inability to read text, and wide pupils that do not respond to light. Usually, with the onset of dysphagia, breathing problems also appear. Blood pressure and temperature do not change during botulism.
- Myasthenia gravis will also manifest itself as weakness of the facial muscles, difficulty chewing, and weakness of the muscles of the limbs.
- Parkinson's disease. In this case, movement disorders, tremors, and mental disorders come to the fore.
- In addition to dysphagia, multiple sclerosis can manifest itself with various symptoms: paresthesia, blurred vision, speech impairment, limb weakness, and cognitive impairment.
- Guillain-Barré syndrome usually begins with a fever, then pain in the extremities. Then the range of movements in the limbs decreases up to paralysis; such paralysis rises from the legs upward - to the muscles of the abdomen and chest.
Features in children
The main causes of dysphagia in children occur with diseases of the nervous system, for example, with cerebral palsy (the risk of developing this symptom is especially increased in a child with paralysis of all four limbs).
The risk is also high in children suffering from athetosis (constant involuntary movements), which is often congenital. Dysphagia also develops with muscle diseases, spina bifida, and Arnold-Chiari malformation. The symptom can also develop with congenital malformations of the pharynx and esophagus, Rossolimo-Bekhterev syndrome.
You should suspect a problem in a child with the following symptoms:
- small amount of food eaten by the baby;
- prolonged sucking of formula or breast;
- cough or facial flushing after eating/drinking;
- placing the head and neck in an unusual position when feeding;
- cough and shortness of breath will not always be pronounced if a small volume enters the trachea during feeding;
- milk or formula appears in the nose.
If a child often suffers from pneumonia or bronchitis, his face is red after eating, or he has developed asthma (but his relatives do not suffer from this disease) - this may also be a sign of problems with the innervation of the esophagus.
A lump in the throat can be caused by cervical osteochondrosis.
Find out all the details about this disease. Read about vegetative-vascular dystonia here.
Nervous dysphagia
It is also called functional. It is caused by various kinds of neuroses - inorganic diseases of the nervous system. The pathology develops in children, adolescents, and adults of both sexes up to 40 years of age; after this age, the disease is practically not registered in men.
In children, neurosis can “linger” from an early age. Initially, it manifests itself in the fact that the child has a decreased appetite, regurgitation, vomiting, and poor sleep.
At school age, such children are characterized by increased pain, thinness, intolerance to transport, and poor appetite. In adults, such dysphagia develops for the first time against the background of a traumatic situation and is characterized by choking followed by difficulty in breathing, which is accompanied by a panic attack.
Diagnostics
Diagnosis can be made by swallowing liquids or solids. Next, based on research, the problem that led to the development of dysphagia is diagnosed:
- X-ray of the esophagus with contrast (barium);
- Ultrasound of the thyroid gland;
- FGDS;
- examination by an ENT doctor;
- MRI of the brain.
Diagnosis of the disease
When making a diagnosis, it is necessary to consult several doctors at once - a neurologist, therapist, surgeon, psychiatrist, otolaryngologist. Dysphagia of the esophagus or larynx is determined by the following methods:
- Laryngoscopy;
- Esophagoscopy;
- Ultrasound;
- Esophagomanometry;
- Contrast X-ray examination.
In severe cases, the doctor uses computed tomography.
Diet
Treatment of dysphagia is complex, therefore, to alleviate the physical condition, it is necessary to follow certain nutritional rules.
- Fractional consumption of food in small portions.
- Thoroughly grinding or chewing food.
- Increasing the volume of fluid consumed.
- Refusal of foods that irritate the esophageal mucosa (hot, salty, spicy, too cold or hot), dry food, strong coffee and tea, fizzy drinks and alcohol.
It may be necessary to carry out bougienage - multiple expansion of the lumen of the esophagus with a bougie, a special dilator. This is what treating dysphagia is all about.
Most often, there is no need to adhere to a special diet, except in exceptional cases. You need to eat right, in small portions. The food needs to be chewed well so that a piece does not get stuck. You need to separate the bones from the fish. You can’t eat dry or on the go. After eating, it is better not to bend over again. It is important to forget about eating before bed.
Harmful foods and solid foods should be postponed until complete recovery. The same should be done with tea, coffee and soda.
Home therapy
It should only be carried out under the supervision of a doctor. The action of the medications is aimed at eliminating inflammation, muscle spasms, and calming the nervous system:
- "Atropine" - helps relax the muscles of the esophagus, eliminates spasm and pain.
- Buscopan is a rectal suppository used to relieve spasms of smooth muscles and reduce the secretion of digestive enzymes.
- "Gastrocepin". The drug temporarily blocks the vagus nerve and eliminates excess secretion of hydrochloric acid.
- "Motilium". The drug stimulates gastric motility, which accelerates the passage of food through the gastrointestinal tract.
- "Platifillin." It calms the nervous system and eliminates vascular hypertonicity.
- "Nikoshpan." Has a relaxing effect on cerebral vessels, improves blood circulation in the brain.
The drugs have contraindications and side effects. Therefore, they should be treated only after consultation with a doctor.
Venereal diseases
Painful sensations when swallowing, soreness and inflammation of the mucous membranes of the ENT organs can be a symptom of the development of a sexually transmitted infection. Hoarseness of voice, swelling of the throat and enlargement of regional lymph nodes may be associated with the development of pathologies such as:
- syphilis is a sexually transmitted bacterial disease caused by treponema; the introduction of pathogens into the ciliated epithelium leads to tissue compaction and chancre formation; as a result of a decrease in local immunity, microbial flora penetrates into the affected area, which causes purulent processes;
- gonorrhea is a sexually transmitted pathology that occurs as a result of damage to the genital organs by gram-negative diplococcus; untimely treatment of the disease leads to damage to the mucous membranes of the oropharynx, conjunctiva and intestines.
Extragenital chancre on the mucous membranes of the throat can provoke the development of meningoneuritis, which is fraught with atrophy of the optic and auditory nerves.
Some clinical manifestations of sexually transmitted diseases are difficult to distinguish from the symptoms of tonsillitis. Syphilitic inflammation of the oropharynx is fraught with the development of severe systemic and local complications. For this reason, if purulent plaque is detected on the tonsils and oropharyngeal mucosa, it is not advisable to postpone a visit to a specialist for a long time.
Features of the course of functional dysphagia
Functional dysphagia of the esophagus occurs due to various neuroses. This form of pathology can be detected in people of any gender before reaching 40 years of age, and in men after this age limit it almost never occurs.
In childhood, functional dysphagia may be present from an early age. In such cases it manifests itself:
- loss of appetite;
- frequent regurgitation or vomiting;
- deterioration in sleep quality.
Starting from the age of 7, children are diagnosed with dystrophy, poor appetite and intolerance to traveling in vehicles.
In adults, this form of dysphagia most often develops after a traumatic situation. They may develop panic attacks and experience difficulty breathing.
Forms of the disease
There are 2 main groups into which diseases are divided that can provoke dysphagia.
Depending on the location of the process, the following forms of dysphagia are distinguished:
- oropharyngeal (the passage of food into the esophagus is difficult, the voluntary phase of swallowing is impaired);
- pharyngoesophageal (the entry of food into the esophagus is complicated, the fast involuntary phase of swallowing is disrupted);
- esophageal (the passage of food through the esophagus is complicated, the slow involuntary phase of swallowing is disrupted).
Prevention
To reduce the risk of dysphagia, you must follow simple recommendations:
- You should stop smoking.
- A balanced diet is required, and if possible, rough foods should be avoided.
- It is necessary to promptly treat ailments of the esophagus, throat, and ENT organs.
- It is important to have regular check-ups with your doctors.
To prevent problems in your child, it is important to monitor what toys he plays with. They should not contain small parts that could be easily swallowed.
Therefore, dysphagia must be treated promptly. Only effective therapy will relieve unpleasant symptoms. And preventive measures will prevent this pathology.
Vegetative-vascular dystonia
Vegetative-vascular dystonia is pathological changes in the autonomic nervous system, characterized by a decrease in the elasticity of blood vessels in internal organs and systems. It is often complicated by hyperventilation syndrome – disturbances in the respiratory regulation system.
Intensification of breathing leads to drying out of the oropharyngeal mucosa, resulting in discomfort.
Vegetative-vascular dystonia can be complicated by coronary heart disease, bronchial asthma and hypertension.
Pathological changes in blood vessels prevent normal gas exchange in tissues, as a result of which their nutrition deteriorates and reactivity decreases.
Due to a decrease in general and local immunity, the risk of developing infectious pathologies increases. Septic inflammation of the airways inevitably leads to painful sensations when swallowing saliva.
Types of dysphagia
Dysphagia can have different stages, depending on the location of the problem. Varieties identified:
- Oropharyngeal (oropharyngeal) - difficulty passing food and liquid into the esophagus. Caused by a disorder of the muscles of the pharynx.
- Pharyngeal-esophageal - a violation of the rapid entry of food into the esophagus.
- Dysphagia of the esophagus (esophageal) - develops with difficulties in slow swallowing, making it difficult to pass food.
A person has difficulty swallowing.
4 stages of swallowing disorders have been identified, when:
- Obstructions in swallowing are present only when eating certain hard foods.
- Without obstacles, only a watery or puree-like consistency passes into the esophagus; it is impossible to swallow a solid lump.
- Sometimes paradoxical dysphagia occurs. Its paradox is that solid food passes better than liquid food (another name for Lichtenstern's symptom). Only liquid is inaccessible for swallowing.
- A person cannot swallow in principle.
About consequences and prevention
In emergency cases, emergency medical care is required, or emergency hospitalization of the patient is carried out. Medical care comes down to measures to clear the airways from food that has entered them and restore the patency of the esophagus if a food coma gets stuck in it,
If you ignore the causes leading to dysphagia in everyday life, the consequences can be the most tragic: perforation of a diverticulum leading to mediastinitis, rupture of an aortic aneurysm that can cause death within minutes, slow decline from esophageal cancer.
This implies the need to prevent the pathology leading to the described condition. It is carried out through clinical observation by doctors: pediatrician, oncologist, ENT doctor, neurologist and other specialists.
Equally important is the fulfillment by parents of young patients and adult patients of doctors’ instructions regarding diet, regimen, and adherence to the rules for taking prescribed medications.
Physiology of pain
Why does it hurt to swallow? Pain is an unpleasant sensory experience that results from tissue damage. The mucous membrane of the ENT organs contains many nociceptors, which, when excited, cause discomfort. Specific receptors can be excited by mechanical, chemical and thermal stimuli.
Activation of pain receptors in the peripheral nervous system signals the body about the presence of harmful processes in tissues. Septic inflammation, burns and proliferation of ciliated epithelial tissue excite nociceptors, which through nerve cells transmit impulses to the corresponding parts of the brain. Painful sensations signal the danger of disease and tissue damage by pathogens or cancer cells.
Dysphagia - what is it?
Dysphagia (Greek dys - denial, phagein - is) is the general name for a swallowing disorder.
Dysphagia is a syndrome (complex of symptoms) manifested by a violation of the act of swallowing.
Oropharyngeal dysphagia
Oropharyngeal dysphagia is also called “upper”; with this form of dysfunction, the oral and oropharyngeal phases of swallowing are disrupted.
Oropharyngeal dysphagia syndrome includes the following symptoms:
- difficulty at the very beginning of swallowing;
- return of food through the nasal passages;
- cough;
- attack of suffocation;
- neurological diseases leading to oropharyngeal dysphagia often occur with dysarthria (impaired articulation and pronunciation) and diplopia (impaired function of the visual muscles);
Causes of oropharyngeal dysphagia:
- Obstruction of the esophageal tract.
- various infectious processes (sore throats, pharyngitis, abscesses);
- enlargement of the thyroid gland (thyromegaly);
- various lymphadenitis;
- Zenker's diverticulum;
- various types of myositis and fibrosis;
- cervical osteochondrosis;
- oropharyngeal malignancy;
- Disturbance in the conduction of nerve impulses to muscle fibers:
- diseases of the central nervous system (brain tumors, stroke, Parkinson's disease);
- disorder of nerve impulse transmission to smooth muscles (ACD dysfunction).
- Psychosomatic disorders (neuroses, various functional disorders).
Treatment of oropharyngeal dysphagia depends on the etiology of the disease.
Dysphagia in stroke
Swallowing is a complex reflex reaction.
Peripheral innervation of the muscles involved in the act of swallowing is carried out by pairs of cranial nerves, their afferent and efferent fibers (trigeminal nerve, facial nerve, glossopharyngeal nerve, recurrent, hypoglossal nerve).
The central nuclei of regulation of the act of swallowing are located in the reticular formation of the brain stem. The cortical swallowing centers are located in the posterior parts of the frontal lobes.
Esophageal dysphagia: symptoms
Esophageal dysphagia is most often caused by esophageal diseases, diseases of the gastrointestinal tract, and pathology of the mediastinal organs.
Acute esophageal dysphagia occurs as a result of:
- allergic edema (Quincke's edema);
- obstruction by a foreign body.
Causes of esophageal dysphagia:
- Narrowing of the lumen of the esophagus causes esophageal cancer (stomach cancer localized in the cardia) and GERD also occur. Cicatricial narrowings occur after chemical burns and radiation therapy for thoracic oncology.
- When the esophagus is compressed by tumors of the chest organs (lung cancer, bronchi), enlarged lymph nodes of the mediastinum, paraesophageal hiatal hernia, cardiac pathology with severe myocardial hypertrophy.
- Violation of coordinated contraction of the esophageal muscles can be a sign of achalasia, total spasm of the esophagus, diabetes mellitus, and scleroderma.
- Infectious diseases (tuberculosis) and uncontrolled use of certain drugs (calcium antagonists, nitrates) can lead to disruption of esophageal peristalsis.
Symptoms of esophageal dysphagia:
- in the initial stage of the disease, patients complain of difficulty swallowing dry, solid food;
- retrosternal pain, drooling, often heartburn, dry cough, hoarseness appear;
- As the symptoms progress, the symptoms increase, and difficulties appear when swallowing soft foods and then liquids.
Surgery
It is necessary to remove surgically the consequences of burns of the esophagus that caused its narrowing, inflammation, and tumors. There are no other ways to eliminate these obstacles that disrupt the swallowing process.
If the patient’s condition during the recovery period after a stroke does not allow surgical treatment to eliminate the cause of dysphagia (for example, with a tumor of the esophagus), then temporary measures are taken to make the patient feel better.
Is it possible to treat dysphagia with folk remedies? More on this later.
Causes
Esophageal dysphagia can be of several types, with various predisposing and directly causing disease factors:
- True, associated with disruption of the nerve elements that control the swallowing process.
- Functional, manifested when the central nervous system is damaged. This also includes pseudodysphagia, a condition associated with impaired swallowing, but of hysterical origin.
- Anatomical - associated with an anatomical obstacle to the passage of a bolus of food through an organ.
Diseases of the esophagus most often cause dysphagia, creating an obstacle to the passage of solid or semi-liquid food. Peptic ulcer of the esophagus, reflux esophagitis, strictures in the lumen of the organ, benign and malignant neoplasms and a number of other diseases are associated with this condition.
In addition, diseases of nearby organs can play a certain role, causing compression of the esophagus and a decrease in its lumen. Such diseases include: hiatal hernia, various forms of goiter, in particular nodular goiter, thoracic aortic aneurysm, tumors in the mediastinum.
Gastroesophageal reflux
Gastroesophageal reflux disorder can cause stomach acid to leak into the upper respiratory tract. A decrease in the tone of the muscles responsible for the functioning of the lower esophageal sphincter often causes aspiration of gastric masses. Caustic juices irritate the mucous membrane of the pharynx and provoke the appearance of microcracks and even burns.
The gradual desiccation of the ciliated epithelium is accompanied by tissue degeneration and the formation of ulcers on the inner surface of the airways. The problem is further complicated by the fact that aspiration of gastric juice occurs several times a day, which is one of the causes of chronic inflammation of the throat. A decrease in local immunity creates conditions for the development of opportunistic organisms that cause septic inflammation and the formation of abscesses in the ciliated epithelium.