644
0
The quadrivalent cervical cancer vaccine can protect against dangerous strains such as 11, 16 and 18, as well as 6, which can cause cancer precursors.
The Dutch analogue “Cervarix” can also help protect against this type of cancer. However, vaccination against this disease will protect against only two strains: 16 and 18.
Their action is somewhat different from each other and there is no possibility of replacement. Cervical cancer vaccinations are given in three doses and there are two vaccination options:
- Ordinary;
- Extra.
Vaccine against cervical cancer and HPV
The Gardasil® vaccine was developed to prevent girls from getting cervical cancer in the future. In 2006, its manufacturer provided 10,000 euros to fund a prize for excellence in the development of vaccination strategies. The prize was received by Professor Dr. med. Heinz-Josef Schmitt, who at that time headed the standing commission on vaccination. This commission makes decisions on the inclusion of vaccines in the list of materials, the costs of which are reimbursed by health insurance organizations.
What is the cervical cancer vaccine?
Leading doctors believe that vaccination is the best way to protect yourself from uterine cancer. A vaccine is a drug that is administered to help the body develop immunity to resist HPV. The vaccine usually does not cause any discomfort during the injection and is painless.
A woman should choose a vaccine independently, but consultation with a gynecologist is required. Additionally, you can consult an immunologist. The drug chosen by the woman should be injected intramuscularly into the deltoid muscle of the shoulder. A slight inflammatory process at the injection site is possible. There is a schedule that provides for three injections at intervals.
Only after vaccination, immunity against the virus will protect a woman for the rest of her life. You should not vaccinate in the buttock, as this may cause complications or ineffectiveness of the vaccine. The most common problem is injury to the sciatic nerve.
Popular Protecting the body from chickenpox by injection vaccination
The vaccination schedule should be drawn up by a doctor:
- the second injection is given exactly one month after the first;
- the third - in six months.
It is important to follow this schedule, this will guarantee that the vaccination will be effective. If there is a need to vaccinate in an accelerated manner, this must be done with the permission of a doctor. The second and third injections are given with a break of one month.
Vaccination should be carried out only after examination by a doctor. If diseases are detected, it is worth treating them and then vaccinating them.
Where to vaccinate?
You should get vaccinated against uterine cancer at a medical center. The vaccine should be administered by an immunologist, gynecologist or oncologist. If a preliminary laboratory study makes sense, it is worth doing. Vaccination can also be carried out in:
- clinics at the place of registration;
- in immunology centers, such as there are in big cities. It is in the immunology center that you can conduct tests and immediately find out the result;
- in a gynecological clinic.
It is recommended to carry out it in special institutions, because this is the only way to be sure that it was done correctly and it will be effective. When buying a vaccine at a pharmacy before vaccination, you should make sure that it has the correct expiration date, the integrity of the packaging, and the quality certificate. After the vaccination has been administered, you should stay in the doctor’s office for a few minutes. This is to avoid shock and to provide medical care.
The HPV vaccine should always have a stamp and hologram on the package. In some countries, vaccination against HPV and in particular against uterine cancer is mandatory in all schools for girls aged 12-14 years. This is important, because the vaccine should be given to girls who have not yet entered into sexual activity and are not infected.
Best age for vaccination
Manufacturers and researchers say that girls under 26 years of age should be vaccinated against cervical cancer. The effectiveness of the vaccine for people over this age has not yet been studied. To build immunity and protect against the virus, you should vaccinate at the recommended time.
Vaccination against uterine cancer involves administration to different age categories (9-14 years and from 18 to 26 inclusive). In Russia, this vaccination is included in the calendar in schools and is given to girls at the age of 12. The health organization recommends vaccinations from 10 to 13 years and from 16 to 23. This is the optimal age for a vaccine against uterine cancer. If a girl who is vaccinated is sexually active, it is worth notifying the doctor and getting tested.
Doctors say that teenage girls who are successfully immunized have more effective protection than those who were vaccinated at an older age.
Contraindications for vaccination
You should not get vaccinated in the following cases:
- Vaccination against cervical cancer should not be given to pregnant women or during lactation. Vaccination against cervical cancer, the consequences during this period can have an impact on the child’s condition. After the end of the lactation period, vaccination can be done after being examined by a doctor; 2. For cervical dysplasia, erosion and other neoplasms of the reproductive system, vaccination is not recommended. This is possible with treatment. It is recommended to wait several months after treatment, carry out repeated tests and only then vaccinate; 3. You cannot vaccinate if you have allergies. Especially if you are allergic to baker's yeast. Since this product is a component of the vaccine; 4. Vaccination is not recommended if, after the first administration of the drug, the patient experienced severe allergies or other complications. This could be an allergic reaction, rash or other complications.
Popular Basic vaccinations for workers in the health book
A woman who has a respiratory illness or fever should reschedule vaccination to another time. Before each vaccination it is worth conducting an examination.
A hasty professor in pursuit of profit
Soon a storm of indignation erupted over Schmitt and the permanent vaccination commission. Harsh criticism, and deeply justified, was heard not only in industry media, such as the organ of the German Medical Association “Deutsches Ärzteblatt”, but also in publications for the general public - “Süddeutsche Zeitung”, “Die Welt”, “Frankfurter Rundschau” and others.
The Gardasil® vaccine trial has become the Professor Schmitt trial. He did not wait for the conclusions, but got a job at the pharmaceutical company Novartis, after the permanent vaccination commission hastened to authorize the use of the Gardasil® vaccine. This happened in March 2007. Experts criticized the company's "apparent haste" in the data it collected.
When the Gardasil® vaccine came to market, two key studies on its effectiveness were still far from complete. Perhaps, as a result of their completion, it would become clear that there are no reasonable grounds for official approval of this drug.
So does the Alliance for Human Rights in Medical Research. Representatives of this American association, which deals with the ethical aspects of medical science, claim that clinical studies have not confirmed either the safety or effectiveness of the vaccine.
Dr. Afanasyev M.S.
“Should girls and young women be vaccinated against cervical cancer?” – I do not have a clear opinion about vaccinating my daughter against HPV infection. At the same time, I am for the state vaccination calendar and for vaccination in general.
The method of vaccination against cervical cancer, or more precisely HPV infection, was invented by the German scientist Harald zur Hauser, for which he was awarded the Nobel Prize in 2008. The very idea and method of combating HPV infection as a cause of cervical cancer, in my opinion, is worthy of high praise. There is one forgotten BUT. The fact that this is a method of prevention, not treatment of cervical cancer. But Elena Malysheva, whom you mentioned in the health program, I know for sure, is committing a crime by promoting vaccination against HPV as a method of treatment.
So, vaccination is a method of prevention and not treatment!
VACCINATION STRICTLY CANNOT BE CARRIED OUT FOR GIRLS, GIRLS AND WOMEN WHO HAVE BEGINNED TO BE SEXUALLY LIFE. THIS WILL CAUSE AN INCREASE IN THE INCIDENCE OF HPV INFECTION AND AS A CONSEQUENCE OF CERVICAL CANCER!
Watch Elena Malysheva’s videos from 2009, where two young girls are sitting, giving the impression of that side of the female gender that has not begun to be sexually active. These programs were a “project” of the Channel One project “The Naked Truth about Cervical Cancer.” It was then, completely justified, that the social problem was made public. And then, in my opinion, everything was correct. The project was completed and the budget for the purchase of vaccines was again allocated 6 years later. And now Lena Malysheva is selling a completely unnecessary, or rather prohibited, vaccine to women who have begun to have sexual activity and even completed their reproductive function.
I cannot consider the opinion of many other doctors and scientists, who are often referred to: Galina Petrovna Chervonskaya, Irina Mikhailovna Sazonova, Galina Borisovna Kirillicheva, etc., who are categorically against vaccination against cervical cancer, to be objective. The respected scientists mentioned above are, in general, categorically against vaccination - ANYONE. The fact that they give examples of complications due to HPV vaccination, there have always been vaccines, the use of which resulted in complications and even deaths, for example, the live polio vaccine.
photodynamic therapy in the treatment of precancer and micro-invasive forms of cervical cancer .
In 95% of my patients, after 1 session of PDT, within six months I get negative results three times for the absence of dysplasia and a negative viral load for HPV infection.
And now I am treating two patients, one of whom had a recurrence of dysplasia after conization of the cervix using the radio wave method and for some reason she was given a three-time vaccine against HPV, the other had a history of two conizations of the cervix and she came to me with a third recurrence of dysplasia . So, the first patient, who after conization underwent three-time vaccination after 1 session of PDT, today received a negative result for dysplasia, but the viral load for HPV of high-risk groups exceeds the norm by more than 20 times.
THEREFORE, DEAR GIRLS AND WOMEN, I CAN SUMMARY AND BARELY ASK YOU NOT TO DO THE HPV VACCINATION AFTER YOUR SEXUAL DEBUT.
BE HEALTHY!
Make an appointment by phone
Consult Dr. Afanasyev by phone..
Ask questions in chat -
A destructive drug as a tool for profit
The Gardasil® vaccine is directed against two specific viruses that cause warts. In total, more than a hundred such viruses are known. They are also called “human papillomaviruses”. An attack of 16 of them can cause cervical cancer. However, Gardasil® only protects against two of these 16 viruses. The vaccine does not help against the remaining 14 out of 16 dangerous viruses.
Since these viruses are sexually transmitted and vaccination only protects against infection, the Permanent Vaccination Commission believes that all girls between the ages of 12 and 17 should be vaccinated. Vaccinating all girls born the same year costs five hundred million euros. This amount represents one percent of all drug costs in Germany.
“It sounds like cervical cancer is a national epidemic,” in an article entitled “Premature Prevention,” published October 22, 2010.
In fact, seven out of ten women will become infected with the viruses that cause warts during their lifetime. However, this infection does not cause any symptoms and clears up on its own in 90 percent of women. Only in exceptional situations is it possible to develop a chronic disease. Then cancer may occur.
However, in the vast majority of cases, this danger is detected in a timely manner using a cytological smear at an appointment with a gynecologist. At an early stage, the chances of cure are very high. The fact that 1,700 women die from cervical cancer every year in Germany is explained by the fact that only every second woman undergoes preventive examinations. Vaccination does not replace early diagnosis. And if the diagnosis is carried out, there is no need for vaccination.
Pointless vaccination is fraught with other dangers. Young women may believe that they are already sufficiently protected, and therefore will use condoms less often and will not undergo preventive diagnostics. In addition, vaccination can contribute to the colonization of the body with other dangerous viruses. The fact is that due to the destruction of two types of viruses, a niche is formed that other viruses are happy to occupy. Large-scale studies already indicate this.
Consequences of vaccination
It has not been medically confirmed that the cervical cancer vaccine causes infertility; it is only known that after vaccination the ovaries may not function well for a short time. In some cases, disturbances in the course of menstruation are possible.
The vaccine can have consequences, and this is why it is used after the age of 15. Before vaccination, you should familiarize yourself with the possible consequences and risks. Canada has banned the use of this vaccine in its country.
Possible consequences of vaccination:
- Temporary feeling of a cold;
- Slight fever;
- A slight increase in body temperature in a woman;
- Severe headaches, malaise;
- Some girls showed slight swelling of the body.
To prevent uterine cancer, it is important to get vaccinated in a timely manner and carry out the following preventive measures:
- Visit a gynecologist at least once a year;
- Take cytological tests recommended by your doctor;
- If erosion is detected, it is worth conducting additional tests. Now erosion is not considered a serious disease, but it is necessary to treat it, especially for those who want to carry out further vaccination.
Cervical cancer is considered a dangerous disease that is best detected in the early stages. Cancer can form over many years and be asymptomatic. The vaccine can prevent the development of such a disease. It is worth warning your doctor about the consequences after vaccination.
A visit to the gynecologist and timely vaccination will help avoid complex diseases like cervical cancer. Vaccination should be carried out after a full examination and consultation. It is possible to prevent cancer; this requires regular screening. Uterine cancer develops due to a chronic infectious process that causes HPV. Vaccination helps produce antibodies and protect a woman’s body. Doctors recommend vaccination as early as possible, thereby preventing the disease from manifesting itself.
https://youtu.be/Zp4SuMo4VnY
HPV does not cause cervical cancer
As early as 1992, doubts arose about the validity of the generally accepted and deeply rooted theory that HPV causes cervical cancer. This view was criticized by two molecular biologists from the University of California at Berkeley, Peter Duesberg and Jody Schwartz. They expressed concern that there is no convincing evidence for the presence of HPV genes specifically in HPV-positive malignant tumors.
Scientists have hypothesized that the cancer is caused by rare, spontaneous or chemical-induced chromosomal abnormalities—such abnormalities have been consistently found in both HPV DNA-positive and HPV-DNA-negative cases of cervical cancer.
Thus, the possibility was identified that the main cause of pathological cell development is carcinogens, and not HPV. The main argument is that because actively proliferating cells (i.e., growing cancer cells) are much more susceptible to infection than normal cells, viruses are only an indicator of unhealthy growth, not the cause.
Experts from the American National Cancer Institute have so far also not found evidence that HPV is a direct cause of the development of cervical cancer.
Vaccines and rules for their use
Two vaccines are used worldwide to prevent cervical cancer:
- Quadrivalent Gardasil, which was registered in the USA in 2006 and is aimed at preventing infection with HPV types 6, 11, 16 and 18. Its effectiveness has been proven in the prevention of cancer and dysplastic changes of the cervix, vaginal and vulvar cancer, as well as anogenital genital warts and dysplastic lesions of the anal area.
- The divalent Cervarix, registered in the same year in England and directed against HPV strains 16 and 18, is effective in preventing dysplastic changes in the cervix and its damage by malignant neoplasms.
Both drugs are approved for use in Russia. They are a suspension containing virus-like purified L1 protein particles. The latter are obtained using a recombinant technological process and are fixed on the AS04 adjuvant system or on amorphous aluminum hydroxysulfate as an adjuvant. Vaccines do not contain viral DNA, so infection is not possible.
Where do you get the cervical cancer vaccine?
The drugs are available in bottles or disposable syringes of 0.5 milliliters (1 dose) and are administered only intramuscularly into the outer upper third of the shoulder (deltoid muscle) or into the area of the outer upper sections of the middle 1/3 of the thigh. Full vaccination, regardless of age, includes:
- First introduction.
- After 2 months.
- Six months after the first administration.
Immunization is also allowed 1 and 3 months (respectively) after the first administration. The vaccines are approved for use in girls and women from 9 to 45 years of age.
Until what age is vaccination against cervical cancer given?
The maximum effect of immunization can be achieved before the body potentially encounters the virus. Vaccination against HPV after infection, naturally, cannot have any preventive effect. Considering that infection occurs through sexual contact, it is absolutely clear that it is most advisable to vaccinate before sexual activity begins, that is, for children 12 to 14 years of age. This is in accordance with WHO recommendations.
At the same time, vaccination against HPV in the presence of the virus identified as a result of the examination is also possible for women under 26 years of age. This is due to the fact that the drugs are almost 47% capable of causing cross-immune protection against other oncogenic viruses and dysplastic lesions of the cervix, regardless of the strain of the papilloma virus.
Vaccination for women after 30 years of age sometimes makes sense for the same reasons, but it is more appropriate in cases where there has been no prior sexual intercourse. Although some clinicians note a milder course of cervical lesions and a higher degree of effectiveness of specific therapy for an existing disease after vaccination, these data are still isolated and require further research.
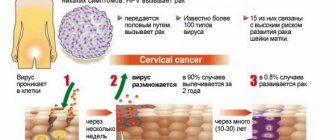
Effect of the vaccine
The cervical cancer vaccine affects the body in the same way as all other vaccine options. It allows you to develop immunity and prevent infection of the female body with the human papillomavirus. Currently, more than 100 types of HPV are known, which lead to the development of various pathologies. Of these, 15 types provoke the growth of cancer cells, and types 16 and 18 pose the greatest danger. These pathogens are easily spread through unprotected sexual intercourse. That is, patients who do not use condoms during sex are at risk.
The vaccine contains a virus shell devoid of a genome. It helps develop the body’s immune response to all types of HPV, but does not lead to illness or exacerbation of existing pathologies. Patients are often afraid to get vaccinated, but it is worth understanding that it is easier to prevent a disease than to try to cure it later. It is not always possible to cure cervical cancer and save women’s lives. Among the possible consequences of HPV infection may be infertility, which is also very sad.
Vaccination against cervical cancer in the Russian Federation is allowed from 12 years of age. This requires three injections. Exactly 2 months should pass between the first and second, and the last vaccination is given six months after the initial administration of the vaccine. The vaccine is active against viruses of types 6, 11, 16 and 18, that is, the most dangerous. It is given to girls aged 9-26 years.
It is best to inject into muscle tissue. The serum contains aluminum hydroxide, which enhances the body's immune response to the active substances from the vaccine entering the bloodstream. At the same time, protein genes are better absorbed into the blood, and inflammation occurs at the injection site, that is, the immune system is activated.
Types of drugs against cervical cancer registered and used in Russia
The disease in question is caused by the human papillomavirus (HPV). Human papillomaviruses are transmitted sexually. According to the latest data, almost all people living in the world are carriers of this virus. They don't get sick because not all strains are considered pathogenic, but only some. Usually these microorganisms are neutralized by the immune system.
Certain types of viruses can trigger the development of precancerous diseases. These are the so-called high-risk papillomaviruses - HPV-HR. They stimulate the development of abnormal cells in the surface layer of the cervix. If the number of such cells exceeds two-thirds of the total, this condition in gynecology is usually called precancerous, or precancerous. If nothing is done, there is a high probability that the changed cells will transform into malignant ones, thereby causing cervical cancer. It does not develop in all patients with precancer, but it is not easy to predict who will experience it and who will die using the capabilities of modern medicine.
Precancerous conditions and cervical cancer are provoked by high-risk papillomaviruses. The most dangerous HPV-HRs are 16 and 18. They are responsible for 70% of cases of malignancy of pathological formations in the organs of the female reproductive system. This is evidenced by studies conducted by the World Health Organization and the scientific Internet platform Cochrane.
The drugs that will be considered do not have antigens against all strains, but only against HR HPV - those that ultimately lead to death.
Only two drugs are registered and used in our country:
- Cervarix;
- Gardasil.
Both vaccines are produced by foreign companies. Gardasil is produced in Holland and is able to fight against 4 types of the virus, while the Belgian Cervarix is only able to fight against 2 strains.
The formulas of Gadrasil and Cervarix include only the protein shells of HPV. Due to this, it is impossible to contract an infection, since there is no genetic information in the drugs, and as a result, the virus is not able to multiply in the human body. In addition, the composition includes:
- yeast proteins;
- Al(OH)3;
- antibacterial component;
- preservative
The drugs considered can prevent the development of the disease and some precancerous conditions.