Prevention of ICN
If ICI is detected while expecting a child, then when planning your next pregnancy, you must definitely seek advice from a gynecologist. He examines the woman and, based on the results obtained, prescribes the necessary treatment for the patient.
When a woman is diagnosed with ICI, there is no need to be upset, since today such a pathology can be successfully treated. To do this, it is necessary to follow the treatment regimen and maintain a psychological attitude, which will allow you to carry the baby to term and successfully give birth. Caesarean birth is used for certain indications and is considered a rather complex operation. For a quick recovery, you must follow all the doctor’s recommendations and take care of yourself.
Many women claim that they were able to successfully carry their child to term while following all the doctor’s recommendations. Usually, with timely suturing, pregnancy ends successfully, but cases of its termination due to weakness of the uterine pharynx still occur.
Video: Suture after caesarean section
Video: Scar and suture after cesarean section
The cervix performs a very important function during pregnancy. Thanks to it, the fetus is retained. Its closed state throughout the entire pregnancy helps to retain the embryo in the mother’s body, and, in addition, protect it from infections from the outside. Timely opening of the cervical (cervical) canal should occur after 37 weeks. But if this process begins prematurely, doctors recommend an operation such as suturing the cervix.
The reason is factors that contribute to the onset of labor at a time when the fetus is not yet viable outside the womb. This situation occurs when the uterine muscles fail, called isthmic-cervical insufficiency, or ICI for short. The consequence of the disease is the premature birth of a non-viable baby.
https://youtu.be/6XrLItbz4ko
What treatment methods are there for ICI?
Most often, doctors recommend a suturing method performed in a hospital. He has proven himself to be the best. For a week, women are instructed to stay in the hospital under the supervision of a gynecologist, and then they can move on to their normal lifestyle with minor restrictions.
Surgical method of suturing the uterus in a woman
Conservative treatment of uterine incompetence
This method consists of using obstetric unloading pessaries to prevent the threat. They help keep the growing fetus in the womb by reducing the load on the cervix. With their help, the ability to maintain a pregnancy increases significantly.
An obstetric pessary is a specially shaped structure made of plastic or silicone. It is placed in the vagina in the early stages of pregnancy and removed after 37 weeks.
Method of surgical correction
This type of treatment is carried out by placing suture material on the cervix. After it is carried out, the frequency of premature births, which usually occur before the 33rd week of pregnancy, is significantly reduced. The surgical method in the treatment of ICI is considered the most effective. Most often, with such a correction, the following methods of applying suture materials are used: U-shaped, performed according to Lyubimova, and suturing according to McDonald and Shirodkar, which has various modifications.
They give the greatest effect when they prevent gaping of the pharynx. To achieve the best results, the operation is performed no later than 18 weeks of pregnancy. The suture material is removed just before birth, at 37 weeks.
Signs of ICI for which surgery is indicated
A disease such as cervical incompetence, which occurs during gestation, can occur completely without symptoms. However, when its image becomes progressive, the woman exhibits the following symptoms:
- The urge to urinate becomes significantly more frequent, and discomfort and a feeling of unpleasant pressure appear in the lower abdomen;
- A soft foreign body is felt in the vagina;
- Watery discharge begins, which is a harbinger of rupture of the membranes.
A gynecological examination shows that the amniotic sac begins to rupture, the length and consistency of the cervix changes, it smoothes out, and the cervical canal expands. If such signs appear, it is necessary to urgently suturing the uterine cervix. After the operation, the threat to the life of the unborn child completely disappears.
Additional information about such a sign as rupture of membranes can be found by watching this video:
Conditions required for surgical correction of ICI
For patients diagnosed with cervical incompetence, surgical intervention is recommended. To carry it out successfully, several prerequisites are required:
- Good viability of the fetus, absence of any developmental defects;
- The amniotic sac is undamaged;
- Pregnancy period not exceeding 25 weeks;
- The uterus is in normal tone;
- Absence of bloody discharge from the genital tract;
- Absence of vulvovaginitis and any signs of chorioamnionitis.
Before this operation, a microbiological examination of the secretions of the cervical canal of the uterus and vagina must be carried out. In addition, tocolytic therapy is prescribed for certain indications. After surgery, antibiotic therapy is necessary.
Available contraindications and indications for surgery
If during pregnancy, according to ultrasound and visual examination, signs of ICI are detected, correction of the cervix will be prescribed using suture materials. This is a fairly simple operation that does not harm either the mother or the child.
Additional information about ultrasound during pregnancy can be found in this video:
Indications for suturing surgery
- The entire cervical canal has practically opened;
- The external pharynx is shortened, its gaping is noticeable;
- The consistency of the cervix has changed and become softer.
When such symptoms appear, you should not hesitate to agree to surgical intervention, because the life of the unborn baby is in question.
Contraindications to the procedure
But there are also signs in which the operation is categorically not permitted. These include:
- Somatic diseases, after which it becomes impossible to continue pregnancy. These are infectious processes and various pathologies, both genetic and internal organs;
- Any defects in the development of the fetus;
- Pathogenic microflora present in the cervical canal;
- Increased excitability of the uterus that cannot be removed by medication;
- Complication of pregnancy - bleeding;
- Suspicion of a frozen, undeveloped pregnancy;
- Vaginal flora, having 3–4 degrees of purity.
If the presence of at least one of them is detected, you should consult your doctor about further actions.
Contraindications and possible complications
Before the operation, a woman must undergo a full examination - examination by a gynecologist, microbiological examination of discharge from the vagina and cervical canal, ultrasound of the cervix, general urine test and blood biochemistry. Based on the results obtained, the doctor makes a conclusion about the possibility of suturing.
In what cases is suturing contraindicated:
- infectious pathologies, acute inflammatory processes in the cervical canal, vagina;
- recurrent bleeding;
- serious cardiac, renal, liver pathologies;
- increased uterine tone, which cannot be eliminated with medications;
- pronounced opening of the internal os, into which the amniotic sac prolapses;
- cervical length less than 20 mm;
- developmental anomalies or intrauterine fetal death;
- violation of the integrity of the fetal bladder.
The main complications after suturing are the development of inflammatory processes, increased muscle tone of the uterus, rupture of the walls of the membranes, suture dehiscence, discomfort in the pelvis and lower back.
The most suitable period for fastening the walls of the pharynx is 13–22 weeks; the timing may be slightly shifted, but after 25 weeks it is not advisable to perform surgical intervention.
Surgical intervention, its features
If a woman exhibits symptoms of a threatened miscarriage, she is recommended to undergo a surgical procedure such as suturing the uterine cervix, which is necessary in order to save the child.
Only thanks to her will it be possible to save the fetus. In addition, if you follow all the doctor’s recommendations after it, the last weeks of pregnancy will proceed calmly.
Preparatory activities being carried out
Cervical correction surgery is performed only in a hospital. The first 3 days are allocated for the doctor to carry out preparatory measures before the planned procedure. They consist of sanitizing the vagina with antibacterial drugs, and, in addition, using tocolytic therapy, which effectively relieves uterine tone.
In addition, the woman will need to undergo an ultrasound and undergo laboratory tests. This is a smear that determines the sensitivity of the vaginal flora to antibiotics, a urine test, and a complete blood test. After all their results are obtained, the patient is prescribed a planned correction of the uterine cervix, which makes it possible to avoid spontaneous miscarriage.
How is the operation performed?
To correct the cervix during pregnancy surgically, one of two methods is usually used. The first is the Czendi method, which is most widespread and involves suturing the lips of the cervix. With it, the front and back lips are fastened together using catgut or silk threads.
But this method has a significant disadvantage. It lies in the fact that after such an intervention, the further development of pregnancy may have pathologies. After all, the closed space that is created in the uterus when it is used becomes the cause of exacerbation of any existing hidden infection. Its effectiveness is also quite low when there is erosion on the cervix.
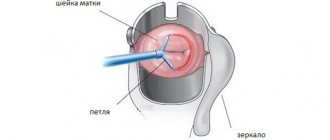
The second, more favorable type of manipulation is to reduce the internal cervical os mechanically. At the same time, the hole necessary for drainage is preserved in the cervical canal. The most widely used methods here are the purse-string circular suture according to MacDonald and the circular suture according to Lyubimova’s method. Also common is the U-shaped one, according to Lyubimova and Mamedalieva.
The operation time does not exceed 15 minutes. It is performed under anesthesia and is completely painless. Normal manifestations that occur after surgery are scanty bleeding and mild nagging pain that quickly passes.
How is the cervix sutured during pregnancy?
The operation of suturing the cervix during gestation at the present stage of development of medicine is carried out in two radically different ways: the external or internal os is sutured.
Stitching the outer edges can harm the general condition and increases the risk of an infectious process. A few days before the operation, the uterine canal and vagina are examined for the presence of harmful bacteria, therapy is carried out to reduce tone, and the vagina is treated with antibacterial agents.
Among all the methods, those that have minimal consequences for the body are distinguished:
- Circular silk sutures on the cervix, applied using the Lyubimova method and secured with wire in polyethylene, are used after the cervix is moved closer to the exit with forceps.
- The Palmer method involves cutting through the vaginal walls to displace the bladder and apply sutures.
- The Lasch method involves an incision from the external os to the isthmus.
- The operation using the Shirocard method is performed using a nylon suture along the external pharynx.
- When using the MacDonald method, excisions are not performed; it is necessary to make numerous punctures at the junction of the vagina and pharynx and fix them using a purse-string suture.
You can see how the cervix is sutured during pregnancy in the video.
The entire operating process takes no more than 15-20 minutes. When the question arises about whether it hurts to stitch up, there can be only one answer - no, since all manipulations are carried out under general anesthesia. Minor discomfort, bleeding and pain in the lower abdomen after suturing are considered normal and should subside three days after surgery. After a week, if the patient feels well, the pregnant woman is discharged.
After this type of intervention, the pregnant woman is not allowed to have sexual activity, sit for a long time and must avoid heavy lifting in order to avoid suture dehiscence before the 37th week.
Video of how to sew up the cervix during pregnancy
Pregnancy is an important and responsible period in the life of every woman. Unfortunately, health problems are not uncommon at this time. And in some cases, the doctor recommends a special procedure to the patient, during which a suture is placed. Sutures are needed on the cervix during pregnancy to prevent miscarriage or premature birth.
On the other hand, surgery during pregnancy frightens women. So in what cases is such a procedure prescribed? What risks does it involve? What is the surgical procedure and how is the rehabilitation period? The answers to these questions are of interest to many patients.
Postoperative period, features of its management
This correction operation, prescribed depending on certain medical indicators during pregnancy, is atraumatic and completely safe for the unborn child. There are usually no complications after it. The postoperative period, spent in a hospital, lasts no more than a week. Doctors do not practice mandatory bed rest. You can get up immediately after the correction.
During the entire period of stay in the hospital, antibacterial and hormonal therapy is carried out, and if necessary, if the tone of the uterus is increased, tocolytic therapy is added to them. In addition, antispasmodics are prescribed. Those places where surgery was performed are treated with antibacterial compounds.
The lifestyle recommended for women after surgery and until the time when the stitches are removed should be specific in order to avoid any adverse effects and maintain pregnancy. Any emotional shock should be avoided, physical activity is limited to a minimum.
It is also necessary to observe a gynecologist with strict adherence to all his recommendations. Sexual intercourse should be excluded for the entire period of pregnancy.
During pregnancy, the cervix holds the baby inside the mother's body and begins to gradually open closer to the due date. However, for a number of reasons, this process can begin much earlier - already from 14-15 weeks, when the fetus outside the womb is not yet viable. Incompetence of the uterine muscles is called uterine muscle incompetence (UCI), and this disease is one of the most common causes of spontaneous miscarriages in the 2-3 trimesters of pregnancy and premature birth.
Treatment of ICI during pregnancy
includes a set of measures that minimize the likelihood of reproductive losses. One of the most important methods of therapy is surgical - tightening the cervix with special sutures. This procedure will be discussed in our article.
How is the recovery period going?
To reduce the risk of complications after surgery, a woman should stay in the hospital for 5–7 days, she is prescribed antibiotics, antispasmodics, and the vagina is treated with antiseptic solutions. For several days, a pregnant woman may be bothered by pain in the lower abdomen and the discharge of ichor - such phenomena are not considered pathological and most often go away on their own.
On the first day after surgery, strict bed rest is indicated; in the future, the woman will have to pay increased attention to nutrition and daily routine in order to avoid complications. Stitches removed at 37 weeks
What you can and cannot do after suturing:
- Do not lift heavy objects;
- Doctors recommend abstaining from sexual intercourse until childbirth;
- proper nutrition should be aimed at preventing constipation - the diet should contain more vegetables and fruits, the amount of sweet, fatty foods, and baked goods should be limited;
- Eating dried fruits regularly will help normalize stools and saturate the body with all the necessary microelements.
After surgery, a woman needs to promptly treat all emerging diseases, avoid stress, and follow hygiene rules.
Suturing the uterine cervix is a safe and effective way to preserve pregnancy in case of premature opening of the pharynx. Most women tolerate the operation well, complications rarely occur, you just need to strictly follow all the doctor’s instructions.
Pregnancy and its outcome depend on the condition of the woman’s cervix. After all, it is she who holds the fetus, fencing it off from the world until the time comes to be born. If everything goes well, the cervix gradually dilates before this event. But there are many reasons that cause the natural opening process to begin earlier. Doctors come to the rescue by stitching the neck. This operation is also called cervical cerclage and sometimes allows you to save the life of the unborn baby.
What is cervical suturing surgery?
The operation of suturing the cervix (or cervical cerclage) is a simple manipulation, but it is performed only in specialized hospitals. During the operation, the doctor uses a needle and threads through the vagina to suture the cervix in one of several ways (depending on the indications and size of the pharynx). In exceptional cases, if the transvaginal method of application is impossible or such a suture has already come apart, the sutures for ICI
applied laparoscopically or through an incision in the lower abdomen.
The procedure is carried out individually, the optimal period is 14-20 weeks of pregnancy (most often before 17, but no later than 27), when the fetus is not yet very large, so there is no high risk of developing postoperative complications. As a rule, before surgery in a hospital setting, the uterus and genital tract are prepared for surgery. Sometimes the operation is performed urgently.
Before the operation, the expectant mother is usually given an anesthetic drug intravenously (locally or epidurally), which does not harm the health of the fetus, and the woman falls asleep for a short time.
Indications
A suture on the cervix during pregnancy is placed by a surgeon only after a preliminary examination of the expectant mother and the recommendations of a gynecologist. Indications for such a surgical procedure may include:
- Risk of miscarriage or preterm labor due to severe dilatation of the cervix.
- Cases of early pregnancy loss in the past.
- Late miscarriage.
- Shortening and dilation of the cervix before the due date.
- Scarring of the cervix after previous births, caused by severe ruptures.
- Destructive changes due to pathologies of the cervix that appeared during pregnancy.
Source: sheika-matka.ru
The final decision on the need for suturing the cervix during pregnancy is made by the gynecologist after a complete examination of the patient. A simple examination on the chair is not enough for this.
It is important to obtain complete information about the condition of the internal genital organs. To do this, the patient needs to undergo a biometric examination, consisting of colposcopy, ultrasound, and laboratory smear examination. If the risk factors are serious, surgery is prescribed.
Indications and contraindications for the procedure
Surgical treatment of ICI during pregnancy is indicated for:
- progression of the disease according to visual examination and ultrasound examination (change in the consistency of the cervix, its softening, shortening, gaping of the external pharynx, opening of the entire cervical canal or internal pharynx);
- a history of spontaneous miscarriages in the 2-3 trimesters of pregnancy.
Contraindications to cervical cerclage are:
- severe somatic diseases in which further continuation of pregnancy is impossible (pathologies of the cardiovascular system, kidneys, liver, infectious processes, genetic pathologies);
- suspicion of an undeveloped pregnancy;
- pregnancy complicated by bleeding;
- increased excitability of the uterus, which cannot be relieved with medication;
- fetal malformations;
- 3-4 degree of purity of the vaginal flora, the presence of pathogenic microflora in the cervical canal.
How is the operation performed?
- After admission to the hospital for two to three days, the doctor carries out preparatory measures before the operation: for this, tocolytic therapy is used to relieve the tone of the uterus, and the vagina is sanitized with the help of antibacterial drugs.
- In addition, before the operation, you will be asked to undergo general and biochemical blood tests, a general urine test, a smear to determine the sensitivity of microflora to antibiotics, and, if necessary, undergo an ultrasound examination.
- The actual suturing of the cervix
is carried out in one of two ways:
- Suturing the external pharynx.
The most widely used method is the Czendi method, which involves sewing the anterior and posterior lips of the cervix together with silk or kengut threads. However, suturing using this method can become an unfavorable factor for the development of pregnancy: during the operation, a closed space is created in the uterus, which can cause an exacerbation of a latent infection (if any). It is also ineffective when present. - Mechanical narrowing of the internal os of the cervix.
This type of manipulation is more favorable, since such manipulations leave a hole for drainage in the cervical canal. The most common methods of suturing the internal pharynx according to MacDonald (circular purse-string suture), circular suture according to the Lyubimova method, sutures in the shape of the letter P according to the method of Lyubimova and Mamedalieva.
The operation lasts no more than 10-15 minutes, during which the woman is under anesthesia and does not feel pain. After the intervention, it is normal to experience nagging pain and scanty bleeding, which will go away on its own in a few days.
What types are used
If no complications arise, the procedure for suturing the cervix takes approximately 15–20 minutes, the operation is performed under general anesthesia, through the vagina, using high-strength threads made of nylon or lavsan to fasten the pharynx.
Basic techniques:
- method B. Scendi - the external pharynx is completely sutured;
- circular seam;
- Mac Donald method - suturing is carried out on the internal pharynx, which is narrowed. The method of A. I Lyubimova, N. M. Mamedalieva are also types of narrowing of the internal pharynx. During the operation, the internal os is corrected by placing a U-shaped suture on the cervix; this technique is considered the most gentle and effective.
During suturing of the cervix, the pregnant woman does not experience discomfort - epidural or intravenous anesthesia is given before the operation.
Features of the postoperative period
If before the operation there was no prolapse of the amniotic sac into the cervical canal, doctors allow the expectant mother to walk within a few hours. For prevention, injections are prescribed or Magne-B6 is taken; in case of increased excitability of the uterus, drugs are used to reduce tone (ginipral or indomethacin). It is possible to prescribe magnesium electrophoresis and acupuncture.
In addition, in the first few days the cervix and vagina are treated with a solution of furacillin, hydrogen peroxide, and chlorhexidine. In case of extensive erosion and changes in the blood count, antibacterial therapy using approved drugs is indicated.
After 5-7 days, the pregnant woman is discharged from the hospital. Further, the woman is examined at least once every 2 weeks. The stitches are removed at 37 weeks: the process is quick and painless.
With a prolapsed amniotic sac, bed rest lasts at least 10 days. Additionally, the foot end of the bed is raised to reduce the pressure of the amniotic sac on the lower segment of the uterus. Since when the amniotic sac protrudes into the cervical canal, there is a high risk of infection in its lower area, antibacterial therapy is mandatory. At the same time, drugs are prescribed to prevent viral infection (immunoglobulin, viferon), the vagina is sanitized, and tocolytic therapy is prescribed.
Expectant mothers with this pathology, as a rule, are in the hospital for at least 1 month, depending on the further course of pregnancy. Removing stitches from the cervix
also performed at 37 weeks. After surgery, all women are not recommended to:
- be sexually active;
- lift weights;
- sit for a long time;
- to work a lot.
Possible complications
The most common complications of surgical treatment of ICI are:
- cutting of sutures
(with increased tone of the uterus, incorrect performance of the operation or with severe inflammation of the cervix); - addition of a bacterial infection;
- ruptures and fistulas of the cervix;
- amniotic sac injury (occurs during surgery);
- endotoxic shock;
- sepsis;
- difficulties in childbirth.
However, in most cases, if all the rules of the operation and the postoperative period are followed, pregnancy ends with the birth of a healthy baby at the right time.
But most importantly, remember that if you have received stitches, this does not completely exclude ICI during pregnancy and does not remove the threat of premature birth. Therefore, you need to be extremely attentive to your feelings, and if unusual symptoms appear (pain in the lower abdomen, in the perineum, discharge, fever), you should immediately contact your doctor to exclude the development of complications.
Why do women sometimes have to have their cervix sutured during pregnancy? Pregnancy is a long and not always easy process. At this time, all the mother’s organs work with double force. And the cervix also plays a very important role - it protects the fetus from external influences, infections and other harmful factors, and also prevents the child from being born prematurely. The cervical canal remains closed until the due date of delivery. If the cervix opens earlier, this means that surgical intervention by a doctor is necessary to correct the cervix, otherwise premature birth threatens and the fetus will be dead.
Very often, the opening of the cervical canal occurs due to weakening of the uterine muscles. A pathology such as isthmic-cervical insufficiency (ICI) occurs. It can cause the birth of a baby whose vital organs have not yet formed.
If the opening of the cervix occurs long before the 37th week of pregnancy, treatment should be prescribed immediately. It can be conservative (without surgery) or surgical. It happens when the course of the disease requires combining these two methods for more effective treatment.
If the cervix is slightly opened, a special device (obstetric pessary) can be used. It will help reduce the load on the walls and cervix, thereby increasing the chances of bringing the pregnancy to a timely birth without losing the baby. If the disease progresses, surgery is necessary.
Indications for cervical correction surgery:
The main symptoms of enlargement of the cervical canal:
- An unpleasant feeling appears with signs of pressure. The discomfort is permanent. The urge to urinate increases.
- The presence of discharge of a watery consistency, which indicates a rupture of the membranes around the fetus.
- Sensation of a foreign body inside the vagina, soft to the touch.
With such symptoms, it is necessary to urgently suturing the cervical canal. Otherwise there will be premature birth. Such signs indicate that the cervix has dilated and the waters are ready to break. The fruit begins to move towards the exit. With timely surgical intervention, the threat of miscarriage is completely eliminated.
Interesting video:
Prevention of complications
Any surgical intervention in the body does not exclude the possibility of complications. They appear not only in the absence of adequate therapy, but also due to the individual characteristics of the functioning of the reproductive system, the general condition of the body and other provoking factors.
The most common complications include:
- rupture of the amniotic sac;
- inflammation of the amnion (a temporary organ that provides an aqueous environment for fetal development);
- seam rupture;
- bleeding of varying intensity;
- infectious diseases of the vagina;
- pain in the pelvic and lumbar region.
If any sign of a pathological condition appears, consultation with a gynecologist is required. In most cases, the patient is hospitalized. The length of stay in the hospital department depends on the recovery process.
To prevent the complications listed above, it is necessary to maintain a gentle daily and nutritional regimen.
Prevention measures include the following procedures:
- Limiting physical activity. Prohibition on lifting weights (more than 1 kg).
- Complete sexual rest. Contraindication to vaginal sex due to injury to the cervical canal and provoking uterine tone.
- Regular consultations with a gynecologist. Constant monitoring of the area of manipulation and compliance with the recommendations of the attending physician.
- Treatment of systemic diseases. The treatment regimen is developed by the doctor individually.
- Elimination of stressful situations. Violation of the psycho-emotional state is a trigger for the development of all kinds of complications.
- Balanced diet. The diet must include a large amount of fiber, which promotes the normal functioning of the intestines and prevents the development of constipation.
- Complete hygiene of the genital organs. Keeping the vagina clean prevents the possibility of infection by pathogenic microorganisms.
Surgical plastic surgery of the cervix makes it possible to prevent possible complications caused by incompetence of the muscles of this organ due to polyhydramnios, large fetuses, and multiple pregnancies. Regular consultations with your doctor and strict adherence to his recommendations will allow you to go through this period as comfortably as possible.
6905 0
1. Place the woman on the gynecological chair.
2. Do a bimanual examination.
3. Treat the external genitalia and vagina with an antiseptic solution.
4. Pain relief is individual, depending on the psycho-emotional state of the woman.
5. Expose the cervix in the speculum.
6. Fix each lip with bullet forceps and pull it anteriorly and downward (do not remove the mirror and lift!).
7. At the border of the transition of the mucous membrane of the anterior fornix of the vagina and the cervix, 0.5 cm from the midline to the right, the cervix is pierced with a needle with a Mylar thread through the entire thickness with a puncture in the posterior fornix, then the end of the thread is transferred to the lateral fornix on the left, pierced with a needle mucous membrane and part of the thickness of the cervix with a puncture in the anterior fornix on the left at the level of the first puncture (do not cross the cervical canal!). The ends of the thread are held on a clamp.
8. The second lavsan thread is also passed through the entire thickness of the cervix, departing 0.5 cm from the midline to the left and 0.5 cm above the previous injection, the end of the second lavsan thread is transferred to the lateral fornix on the right, the mucous membrane and part of the thickness of the cervix are pierced with a puncture in the anterior arch.
9. The ends of the threads are tightened and tied with three knots in the anterior arch.
10. Insert a dry tampon into the vagina for 4-6 hours.
11. Remove tools.
12. Transport to a bed in a supine position.
The process of suturing the cervix and the conditions for its success
In most cases, with early opening of the external and internal pharynx, surgery is recommended. In this case, the incompetence of the cervical canal is very dangerous for the child’s life and must be immediately eliminated by suturing.
At this time, the timing of pregnancy is important. This operation can be performed no later than 21 weeks of pregnancy. It is also recommended from the 15th week of gestation if there is a high risk of premature birth. This is explained by the fact that at such early stages, the cervix is still not open enough and the muscles are not very stretched. In this case, the operation will take place quickly and without difficulty. In the later weeks of pregnancy, cervical correction becomes much more difficult, since the uterus is very weakened and the canal is quite open.
Important! The operation takes little time (15 minutes) and is performed under general anesthesia, which is selected in accordance with the timing and characteristics of the pregnancy.
Suturing can be either external or internal pharynx. This depends on their condition and level of premature opening, as well as whether there are any new growths on them. For example, the external os cannot be sutured if there is erosion on it. In other cases, it is sutured by connecting the anterior and posterior edges of the cervical canal with a thread. Of course, there is a risk of developing infectious diseases, since after the operation a closed space is formed in the cervix. In this case, the doctor monitors the patient more carefully and, if inflammation occurs, prescribes timely treatment.
Note! Correction of the internal os is more acceptable, as it has the advantage that a small hole remains in the canal for drainage. This method of surgery reduces the risk of developing various types of infections in the cervical canal.
There are many factors that are the key to a good outcome of the correction operation and further safe gestation of the fetus:
- the gestational age should not be more than 25 weeks;
- absence of any defects and pathologies in the development of the child;
- there should be no discharge with blood from the vagina;
- absence of inflammatory processes of the vaginal lining and other infections;
- the tone of the uterus should be in normal condition without any deviations;
- absence of even minor damage to the amniotic sac.
Before the operation, analyzes of vaginal discharge are carried out, and the microflora of the endometrium and cervical canal is examined. After correction of the cervix using surgery with suturing, the doctor prescribes a comprehensive treatment, which includes therapy based on antibacterial agents.
It is important to note that there are contraindications for uterine canal suturing surgery during pregnancy. This method of surgical intervention is impossible for the following abnormalities in a woman’s body:
- Constantly increased tone of the uterus, which does not return to normal, even after drug treatment.
- Bleeding from the vagina during pregnancy.
- Risk of miscarriage or missed pregnancy.
- Pathologies in child development, defects of varying complexity.
- The presence of diseases of the genitourinary system or other organs of the woman’s body (heart, liver, kidneys), which are an obstacle to maintaining pregnancy.
- Disturbance in the development of the cervical canal.
For any deviations that may negatively affect the consequences of the operation, correction by suturing is not recommended and may be prohibited. In this case, the doctor is looking for other treatment options.
When is a suture placed on the cervix and why?
During pregnancy, the cervix serves as a “gate” that holds the unborn baby inside the mother’s body. In some situations, there is a risk that it will open ahead of time. To prevent this from happening, doctors perform a simple operation on the woman - they tighten the cervix with special sutures.
The cervix can open prematurely for several reasons. Some women (fortunately not many) have cervical tissue that is too weak from birth. As the future baby grows, the load on the tissues increases, and one day they may not be able to cope with it. The cervix may dilate prematurely in women with an irregularly shaped uterus; if the uterus is damaged; and also with certain hormonal disorders (for example, with increased levels of male hormones). Expectant mothers who have already had difficulties during a previous pregnancy, such as premature birth, should be especially careful. An examination by an obstetrician-gynecologist and an ultrasound will help a woman identify the problem in advance, make an accurate diagnosis and provide timely treatment. Sometimes this requires several examinations; they are carried out from the 12th to the 25th week of pregnancy.
What happens when the cervix opens before its due date? In this case, the membranes in which the baby is located will descend along its canal into the vagina and rupture. If the period is still short (up to 22 weeks), the pregnancy will be terminated after that. If the cervix opens “without asking” by the time the baby is old enough (after 28 weeks), the baby will be born ahead of time.
To prevent this problem, doctors “sew up” the cervix with special sutures - a “ring”. And there is another way out - the expectant mother is prescribed bed rest until the end of pregnancy. True, this method can only help if it is too late to apply a suture (after 25 weeks of pregnancy) or if the operation is not worth doing for some reason.
Stitching the cervix is a simple operation, but it is only done in a hospital. This method was invented 50 years ago by the Indian doctor Shirodkar. The surgeon sutures the cervix with non-absorbable nylon or mylar thread and then secures the thread with a knot.
Most often, this procedure is performed at 13-20 weeks of pregnancy. Before the operation begins, the woman is given a painkiller that is safe for the baby, and she falls asleep for a short time.
After the stitch is applied, the expectant mother usually remains in the hospital for several days. During this time, doctors give her a short course of treatment with antibiotics and drugs that relax the uterus. Immediately after surgery, many women feel a slight nagging pain; bloody discharge appears. These symptoms are completely normal and usually go away on their own within a few days.
Sutures from the cervix are removed at 37 weeks of pregnancy. This operation is painless; it is carried out in a antenatal clinic or in a maternity hospital without pain relief. Even if the baby decides to be born immediately after this, it’s okay. But more often than not, the expectant mother goes home and gives birth, as expected, in about half a month.
As a rule, cervical surgery does not greatly affect the lifestyle of the expectant mother; You need to take special care of yourself only in the first week after the procedure
But, like all pregnant women, the expectant mother should not work hard, drive for a long time and - what is especially important - under no circumstances should she lift heavy objects. In addition, she needs to be examined by a doctor every 2-3 weeks.
After suturing the cervix, doctors often advise women to refrain from having sex, because uterine contractions during intimacy can cause premature contractions. But even if the doctor finds that there are no obstacles to love, it is worth remembering: despite the suture, in the second trimester of pregnancy the cervix remains open and becomes more vulnerable to microbes. So the expectant mother should ask her partner to get tested for sexually transmitted infections or use a condom.
The period after the cervical correction procedure
Discharge occurs 3–5 days after surgery. There are no significant restrictions in a woman’s life. The only thing you need to do is to be extremely attentive to any changes in the body. It is necessary to adhere to the correct sleep schedule, not to overexert yourself with physical activity, rest more and abstain from intimate relationships. All these methods will help reduce the risk or even eliminate increased uterine tone, which can cause miscarriage. Also, visits to the doctor will now be much more frequent than during a normal pregnancy. This is explained by the need for constant monitoring of the condition of the cervix, and the general development of pregnancy, in order to preserve the fetus. The examination is carried out through the vagina very carefully so as not to injure the canal.
During pregnancy after cervical correction surgery, you should carefully monitor your diet. Pushing is prohibited, which means constipation is undesirable. This is why proper diet is so important. It is necessary to eat dried fruits, they have a good effect on a woman’s stool and fill the body with essential elements, vitamins and minerals.
Towards the end of pregnancy, at a gestation period of 35 to 37 weeks, the expectant mother is assigned to a hospital for further observation. Using an ultrasound, the child’s readiness for childbirth is determined and the necessary procedure is selected (natural birth or surgery by cesarean section). When the pregnancy reaches 37 weeks, the woman's preparation begins. At this time, the sutures are removed from the cervix before childbirth. After this, the child can be born at any time.
Recovery
After surgery, the expectant mother remains in the hospital for several days. Doctors are closely monitoring the patient’s condition at this time. If the tone of the uterus is increased, antispasmodics and bed rest are prescribed. The doctor sanitizes the vagina every day to destroy any harmful microorganisms in the genitals. If everything went well, the woman is discharged 4-5 days after the operation.
During the recovery period and up to childbirth, the following are prohibited:
- Any physical activity;
- Long walking, running and even standing in an upright position;
- Lifting weights;
- Active intimate life.
- Push when constipated.
Doctors recommend paying special attention to your diet. Include more fresh fruits, vegetables, and natural juices in your daily menu. Avoid large amounts of protein, salt, flour and sweets.
A gynecologist should monitor the condition of the sutures on the cervix, so be prepared to visit him often. Sutures are removed at 36-37 weeks. During this period, the pregnant woman should already be in the hospital and prepare for childbirth.
Complications after suturing the cervix
Any surgical intervention, even the most minor one, and using the safest method, can lead to some deviations. When suturing the cervical canal, there is a risk of inflammation and a significant increase in the tone of the uterus. The development of infections can be a response to foreign bodies (threads in sutures), hence the inflammation. Also, after such a procedure, minor discharge of varying consistency is observed, including the bloody type. To keep everything under control and avoid unnecessary problems, you need to regularly visit your doctor and take all tests on time. You should also pay special attention to personal hygiene and avoid physical activity in any way. During this period they are extremely undesirable.
Increased uterine tone may also be a reaction to external stimuli and mechanical intervention. In this case, special treatment is prescribed and, as a rule, the uterus returns to normal in a short time. You should also avoid any stress and shock, to which the uterus now reacts very painfully. A woman needs only positive emotions and a healthy diet, no heavy lifting and a complete exclusion of intimate life until childbirth. All this has a beneficial effect on the further course of pregnancy and is one of the ways to preserve it.
Nowadays, numerous pathologies of the cervix have become the cause of many terminated pregnancies or premature births. Basically, the most dangerous period occurs in the second trimester. At this time, the fetus cannot yet live outside the mother, since its vital organs are very poorly formed, and some are not even there yet. Therefore, premature birth is a threat of losing a child. That is why doctors strongly recommend contacting a gynecologist at the first manifestations of an unwanted disease. Identified pathology in the early stages allows the problem to be eliminated without harm to the mother and the unborn baby. And paying attention to yourself and your body is the key to a healthy future for you and your baby. There is not a single way to lose to save the pregnancy.
Suturing the cervix during pregnancy
For a variety of reasons, many women are unable to carry their pregnancy to term. Therefore, bed rest and suturing of the cervix during pregnancy can help her.
Isthmic - cervical insufficiency
Isthmic-cervical insufficiency is the main reason for suturing the cervix during pregnancy, in which the so-called locking function is disrupted.
Ideally, the cervix should be closed until birth. This protects the baby from infections and amniotic fluid from premature release. However, in the presence of the above pathology, the cervix begins to open in the early stages and requires surgical intervention. In this case, suturing of the cervix is more common during multiple pregnancies.
Causes of cervical insufficiency
Among the causes of isthmic-cervical insufficiency can be identified hyperandrogenism or an excess of male hormones in the body of the expectant mother; numerous abortions preceding pregnancy; changes in the cervix that occurred during previous births; as well as underdevelopment of the cervix.
Why is the cervix sutured during pregnancy? So that a woman can carry the fetus to term and prevent infection from getting to it.
How to sew up the cervix during pregnancy
In order to carry out an operation to suture the cervix during pregnancy, it is necessary to make a correct diagnosis. This can be done based on a vaginal examination and ultrasound data. If the diagnosis of isthmic-cervical insufficiency is confirmed, then surgical procedures are performed. Their meaning is simple: sutures are placed on the cervix, which perform a locking function.
The operation to suture the cervix during pregnancy is carried out in a hospital setting, where the woman undergoes all the necessary tests and undergoes control studies. An important study is to check the vagina for the presence of inflammation and infections, if detected, treatment is prescribed first and only then surgical intervention.
Is it painful to have the cervix sutured during pregnancy?
All surgical procedures are performed under internal (local) anesthesia, so the woman does not feel anything during suturing. After performing surgical procedures, the pregnant woman spends some time in the hospital under the supervision of the attending physician. During the rehabilitation period, it is necessary to take special medications that have a positive effect on the tone of the uterus and ensure the normal course of pregnancy.
When suturing the cervix, the sutures are removed after 37 weeks of pregnancy. This is also done in a hospital setting, where the woman undergoes tests, undergoes research, and, in principle, can remain until childbirth, if there are prerequisites for the onset of labor.
How to prevent cervical suturing during pregnancy?
In order to prevent cervical divergence prematurely, a pregnant woman should take care of herself, regularly visit her local gynecologist and undergo all tests.
In addition, in order to prevent isthmic-cervical insufficiency, it is necessary to exclude all possible causes of its occurrence, namely:
recover completely after previous pregnancies or abortions: restore hormonal levels; cure all inflammatory diseases and prevent chronic diseases, and also be observed by a local gynecologist.
The navel came out during pregnancy Pregnancy not only changes the female body from the inside, but also affects the appearance of the expectant mother. And such changes are not always desirable and beautiful.