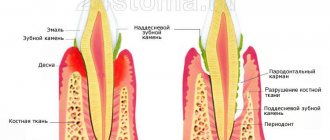
Gingivitis is an inflammatory disease of the gums that occurs due to insufficient oral care. Along the edge of the gums and in hard-to-reach places, plaque, which consists of bacteria, accumulates. After 72 hours, in the absence of proper hygiene, plaque may thicken, which leads to the formation of tartar, which cannot be removed with a regular toothbrush.
During puberty, pregnancy, menstruation and the use of contraceptives, the incidence of the disease increases significantly. Progression of gingivitis without the necessary medical intervention can lead to the development of periodontitis and eventual tooth loss.
Methods for treating gingivitis in adults
Treatment of acute and chronic gingivitis includes 3 components:
- Sanitation of the oral cavity
Removing tartar and bacterial plaque, eliminating carious cavities, removing decayed teeth. This will prevent further spread of the infection.
- Local anti-inflammatory therapy
Antiseptic rinses, applications of anti-inflammatory and wound-healing gels, use of natural toothpastes with herbal ingredients.
- General restorative therapy
Taking vitamin-mineral complexes and immunomodulators. This promotes the regeneration of soft tissues and increases the body's defenses to fight infection.
Diagnosis of gingivitis
Diagnosis of the disease is carried out on the basis of clinical data and additional research methods. Particular attention is paid to the assessment of oral hygiene, which, as a rule, has the greatest violations.
The depth of the gingival sulcus is measured from four surfaces of the tooth using a special graduated probe.
Special methods for studying gingivitis include the Kulazhenko method, the Schiller-Pisarev test, x-ray assessment of the condition of bone tissue, as well as rheoparodontography, the results of which determine the functional state of the blood vessels.
Means for the treatment of catarrhal gingivitis
The catarrhal form of the disease refers to the initial stage of inflammation. It can be easily eliminated with ultrasonic cleaning and drug therapy.
Physiotherapy is also useful, for example, hydromassage of the gums, exposure to short-spectrum UV rays, electrophoresis, etc. These are painless procedures that improve tissue trophism and remove accumulated toxins. The course of treatment includes 5-10 sessions.
Drug treatment
- Rinse with chlorhexidine;
- applying oil solutions with vitamins A and E;
- the use of antimicrobial ointments and sprays - Romazulan, Metrogyl Denta, Cholisal or others.
Chronic inflammation of the gums can develop as a result of dental deformations. In this case, you should definitely see an orthodontist to correct your bite.
Causes and symptoms
Not only internal but also external factors can provoke the development of this disease:
- Congenital or acquired malocclusion.
- Decreased immunity.
- Large accumulation of tartar.
- Poorly performed sanitation of the oral cavity.
- Pregnancy period.
- Injury to soft gum tissue.
- Hormonal disorders.
- Insufficient amount of vitamins in the body.
- Progression of serious pathologies, for example, hepatitis, diabetes, AIDS.
People can suspect the occurrence of a pathological condition based on the characteristic symptoms:
- There is swelling and an increase in gum size.
- Painful sensations occur that have varying degrees of intensity.
- The development of hyperemia is observed.
- The gums began to lose their contour.
- The sensitivity of the mucous membranes has increased, and the threshold of their irritability has decreased.
- There is a foul odor from the oral cavity.
- The mucous membranes begin to bleed.
- There is a deterioration in general health.
- The temperature rises slightly.
- Lymph nodes may become enlarged.
- Over time, due to the reduction in size of the papillae, the interdental space increases.
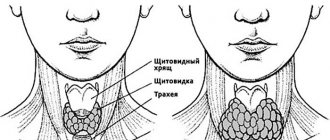
Drugs for the treatment of hypertrophic gingivitis
The cause of the hypertrophic form of inflammation often lies in hormonal imbalances, as well as diseases of the gastrointestinal tract. Therefore, do not be surprised if your dentist refers you to a specialist in the appropriate field - an endocrinologist or gastroenterologist.
And to relieve local symptoms, the following therapy is used:
- applying dressings with antimicrobial ointments;
- taking oral antibiotics - Erythromycin, Amoxicillin, Metronidazole;
- darsonval, electrophoresis and other methods of physiotherapy;
- at an advanced stage - injections of hypertrophic solutions into the gingival papillae - calcium chloride, calcium gluconate, glucose.
In the most severe cases, surgical excision of damaged gum tissue is used.
Diagnostics
To diagnose gingivitis, doctors perform a comprehensive examination.
Basic methods:
- Survey . The patient is asked about the timing of the first unpleasant sensations, their characteristics, what he associates their appearance with, changes in sensations, and whether any gingivitis has been treated. External visual examination: the dentist notes the patient’s behavior, appearance, and palpates the lymph nodes.
- Oral examination . The doctor examines the space between the lips and teeth to assess the bite, the condition of the frenulum of the lips, palate, pharynx, tongue and buccal mucosa. Such an examination suggests the presence of diseases of the internal organs. Next, the doctor examines the patient’s teeth and finds out the presence of caries, pulpitis, microbial plaque and tartar, and pathological pockets inside the gums. Their appearance (color, shape, swelling, bleeding) is also assessed.
- Index score . The specialist uses special formulas to calculate the level of severity of the disease.
Additional diagnostic methods include:
- Radiography . Makes it possible to differentiate between gingivitis and periodontitis.
- General blood analysis . Allows you to identify blood diseases.
Treatment methods for atrophic and ulcerative gingivitis
Atrophic and ulcerative forms of the disease are accompanied by necrosis (destruction) of the marginal gum. At this stage, it is important to save living periodontal tissue, since atrophied areas can no longer be restored.
As a rule, dentists prescribe:
- local anesthesia with a solution of novocaine or lidocaine;
- systemic antibiotic therapy;
- oral baths with antiseptics (furacilin, miramistin, chlorhexidine).
Dead gum tissue is removed mechanically or treated with Trispin. This is an enzyme that promotes the resorption of necrotic epithelium.
Treatment of gum inflammation during pregnancy
Catarrhal gingivitis in expectant mothers can be treated in the same way as in other patients, with the exception of taking oral medications that are not approved by the gynecologist. If a hypertrophied form occurs, only local symptomatic therapy is performed.
Traditional medicine recommends that pregnant women drink more milk, take rosehip decoction, fruit juices and rinse their mouths with saline solutions. These remedies should help expectant mothers cope with bleeding gums.
Antibiotic therapy
Most often, adult patients with purulent inflammation of the gums, gingivitis, are prescribed metronidazole. It is effective against protozoa and various anaerobic bacteria. It is taken three times a day, the daily dose of the drug is 1500 mg. The course lasts 10 days.
In dental practice, metronidazole is necessarily prescribed in combination with lincosamides. This group of drugs includes lincomycin and clindamycin.
Lincomycin
Fights infections caused by gram-positive cocci and anaerobic bacteria (daily dose – 1500 mg, divided into three doses of two capsules).
Clindamycin
It differs from lincomycin in its effectiveness against protozoa, taken 300 mg three times a day.
Lincomycin in capsules often causes side effects - gastrointestinal disorders, allergic rash. It is better to replace lincomycin capsules with a 30% solution for intramuscular injection (2 ml twice a day) or give preference to clindamycin. The latter, by the way, can also be taken in the form of intramuscular injections - 2 ml (300 mg) twice a day.
For patients with diabetes mellitus and/or resistance to other antibiotics, drugs based on norfloxacin, ciprofloxacin or ofloxacin are prescribed. For example:
- nomitin – 400 mg twice a day;
- tarivid – 500 mg in two doses;
- Siflox – 250 mg twice a day.
Antibiotic therapy is prescribed only by a doctor; it is prohibited to take antimicrobial drugs on your own!
Injecting antibiotics into the gums is an outdated and ineffective method that only further injures the soft tissue. Antimicrobial drugs are prescribed only orally (by mouth) or intramuscularly (injections into the gluteal or deltoid muscles, the front surface of the thigh).
Types of disease
Doctors distinguish the main forms of the disease:
- catarrhal;
- ulcerative-necrotic;
- hypertrophic.
Catarrhal gingivitis
Catarrhal gingivitis
The main cause of this form of gingivitis is insufficient oral hygiene, which causes an accumulation of microbial plaque and tartar to appear on the teeth. Especially a lot of pathological content accumulates in the area of the necks of the teeth, where they interact with the gums, provoking the appearance of signs of inflammation in it. This is the most common form of the disease.
Dentists include vitamin C deficiency, diseases of the blood clotting and hematopoiesis system, and hormonal imbalance as the causes of this form of pathology.
Signs of the disease include:
- swelling of the gum edge and papillae between the teeth;
- hyperemia of the visible periodontal area or its cyanosis;
- bleeding gums when brushing teeth;
- pain during oral hygiene;
- visible accumulations of plaque and tartar on the dentition.
Types of catarrhal gingivitis
Catarrhal gingivitis can conventionally have several types. Doctors distinguish the following types of disease:
- Generalized . The inflammatory process affects a significant surface of the gums on the upper and lower jaws. This form is usually caused by internal health problems.
- Localized . The disease is characterized by the fact that the mucous tissue covering the roots of the teeth becomes inflamed only in the area of several of them, and the causes of the pathological process are local in nature.
The course of catarrhal gingivitis can be acute or chronic. Treatment options may vary. It is imperative to follow the doctor's instructions!
The acute nature of this form of the disease is accompanied by pronounced symptoms, rapidly progressive development, severe bleeding and pain during hygiene procedures in the oral cavity. The gums are usually very hyperemic. Often, patients suffering from acute catarrhal gingivitis generally refuse to brush their teeth twice a day, which only complicates the situation.
Acute catarrhal gingivitis
Acute catarrhal gingivitis usually develops once and does not recur if adequate therapy is carried out on time. It can develop in young children during teething. Gum inflammation often accompanies childhood infectious diseases. Sometimes this form of gingivitis is a harbinger of viral stomatitis or a manifestation of an allergic reaction.
If you do not pay attention to the treatment of acute gingivitis in time, the pathological process can progress to the chronic stage, which is characterized by systematic low-grade inflammation of the gum tissue with periodic exacerbations.
The chronic nature of this form of the disease is characterized by mild manifestations over a long period of time. Gingivitis in this form has moderate signs of bleeding gums, minor pain when brushing teeth, and the color of the gums is almost unchanged, with the exception of slight cyanosis. When the body's defenses are weakened, the symptoms of the disease worsen. As a rule, this occurs during periods of colds.
Treatment of catarrhal gingivitis
Treatment of the disease should be aimed at eliminating soft microbial plaque and hard tartar. The first one is easily removed during ordinary oral hygiene procedures. Tartar and partially mineralized plaque can only be removed with the help of a dentist.
If the necessary hygienic measures are not taken, microbial plaque is mineralized by calcium and phosphorus salts, which are present in saliva. As a result, the plaque hardens, is tightly attached to the tooth and can no longer be removed with a toothbrush.
How to treat catarrhal gingivitis? After removing plaque, the dentist will prescribe medications for gingivitis, anti-inflammatory rinses, and special gel applications that can be done at home. This anti-inflammatory therapy will need to continue for at least ten days, and then you will need to visit your dentist for a follow-up examination.
Important: remember that it is not enough to simply stop gum inflammation. It will come back very soon if you don't start brushing your teeth properly. To avoid relapses of gingivitis, it is important to sanitize all carious teeth, as they are breeding grounds for infection.
Ulcerative-necrotizing gingivitis
Ulcerative-necrotizing gingivitis
This form of the disease can also be acute or chronic. It develops due to insufficient oral hygiene. The mass of bacterial plaque on the teeth increases greatly, as a result of which the mucous membrane becomes necrotic and ulcerated. Most often, this form of inflammation occurs against the background of a sharp weakening of the body’s defenses or severe chronic diseases.
Signs of ulcerative gingivitis include:
- white or yellow plaque on the gums;
- ulcerated areas of the mucous membrane covering the edges of the jaws;
- papillary necrosis;
- hyperthermia;
- lack of appetite;
- headache;
- unpleasant odor from the mouth;
- bleeding gums and pain in them.
If the disease is chronic, these symptoms of gingivitis are less pronounced.
How to treat necrotizing ulcerative gingivitis
Therapy for this form of gingivitis is carried out urgently in the dentist's office. First of all, the doctor removes necrotic plaque and dental deposits. Then the doctor prescribes a course of antibacterial therapy, rinsing with antiseptics and applications. Treatment should be strictly in accordance with his instructions.
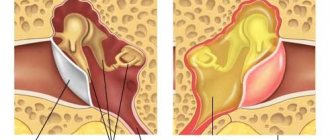
Hypertrophic gingivitis
Hypertrophic gingivitis
This is a chronic form of the inflammatory process in which the gums increase in volume. The cause of this phenomenon can be both its fibrous growth and its swelling. Typically, this type of pathology occurs at the edge of the gum in the area of the outer surface of the upper and lower teeth.
Pathology most often traditionally develops with functional disorders of the endocrine system, hormonal disorders in pregnant women and adolescents, with malocclusion, carelessly placed fillings and crowns. Sometimes gingivitis is a consequence of long-term chronic catarrhal gingivitis.
The symptoms of this inflammatory disease vary depending on its form. Edema hypertrophic gingivitis is manifested by swelling of the gingival papillae. Therefore, they have a loose structure (most often this form of gingivitis develops against the background of hormonal imbalance). At the first stage of treatment, the doctor will remove dental plaque and prescribe treatment with anti-inflammatory drugs. In case of insignificant results, the doctor will use sclerotherapy.
How to treat advanced gingivitis in adults? The fibrous form of this inflammatory process is characterized by a dense structure of the gingival papillae. The doctor will begin treatment of fibrous gingivitis by eliminating traumatic factors and removing soft and hard deposits from the teeth. At the next stage, treatment will include:
- Tissue excision.
- Anti-inflammatory therapy (treatment of gingivitis with bandages with hormonal drugs).
A long-term edematous form of the inflammatory process can become hypertrophic.
Treatment of gingivitis in children
Therapy for children is not very different from treatment for adults, but there are a number of features. The course of events includes:
- Ultrasonic teeth cleaning
The procedure lasts on average 20 minutes and is painless.
- Anti-inflammatory and antibacterial therapy
Applying gels such as Cholisal (for children of any age) and Metrogyl Denta (from 6 years) to the mucous membrane. Mouth rinse with Chlorhexidine or Miramistin.
- Strengthening the immune system
Vitamin therapy will help speed up recovery. Oil solutions with vitamins A and E have a positive effect on the regeneration of gingival tissue.
- Orthodontic treatment
For young patients who have chronic gingivitis due to malocclusion.
Brushing teeth to prevent gingivitis in children
If a child has been diagnosed with necrotizing ulcerative gingivitis, after the first stage of treatment, doctors remove dead soft tissue under local anesthesia and cauterize the gums with an electric current. Before and after the procedure, pain-relieving gels with lidocaine are used - Kalgel, Bobodent, Kamistad.
Of great importance in the treatment of gingivitis is teaching children oral hygiene. After all, without proper dental care, inflammation will appear again.
It is also worth mentioning that children without teeth and infants are treated differently for gum inflammation. It is enough to massage the gums and clean them from germs with a special silicone brush that is placed on your finger.
Catarrhal gingivitis: symptoms
Among all patients with gingivitis, this form accounts for more than 97% of cases. Those. this is the most common form of this disease. The term “catarrhal” means that the inflammation affects only the mucous membrane of the gums (i.e., it proceeds superficially), without affecting the bone tissue around the teeth and the dentogingival attachment. In Fig. 3-5 you can see exactly what catarrhal gingivitis looks like in the oral cavity.
The cause is exceptionally insufficient oral hygiene, as a result of which soft microbial plaque accumulates in the area of the necks of teeth, and the formation of tartar occurs. Plaque bacteria produce toxins and pathogens, which trigger inflammation in the gum mucosa. At the same time, various chronic diseases or vitamin C deficiency are not the direct causes of the development of gingivitis, but may be a predisposing factor that increases the impact of microbial plaque.
Catarrhal gingivitis: photo
Symptoms –
- swelling of the gingival margin and interdental papillae,
- redness or bluishness of the gums,
- bleeding gums when brushing teeth,
- pain when brushing teeth,
- itching in the gums,
- Usually, accumulations of microbial plaque are visible at the necks of teeth.
The appearance of bleeding is associated with an increase in the permeability of capillary walls, capillary fragility, and a decrease in the thickness of the epithelium of the gum mucosa. All this arises as a consequence of the influence of toxins and microbial plaque pathogens on the gum mucosa. Most often, bleeding occurs when exposed to mechanical factors (injuring weakened gums), for example, when brushing teeth or chewing rough, hard food.
Pain when brushing teeth also occurs due to thinning of the epithelium of the gum mucosa. Thinning of the epithelium against the background of gum inflammation is a natural process, and develops due to an increase in the rate of desquamation of epithelial cells (24stoma.ru).
Forms of catarrhal gingivitis –
There are 2 variants of the course of the catarrhal form of gingivitis. Firstly, there is acute catarrhal gingivitis (Fig. 3-4), which is characterized by bright red gum color, acute development, and sometimes significant bleeding and pain when brushing teeth. With this form of the disease, due to pain when brushing teeth, patients sometimes completely abandon oral hygiene, which leads to an even greater increase in the amount of microbial plaque, and as a result, further aggravates the situation.
Secondly, the chronic form of the disease (Fig. 5-6), which is characterized by sluggish symptoms over a long period of time. In this case, catarrhal gingivitis symptoms of bleeding will be quite minor, and there will be no pain during cleaning. The marginal gum and dentogingival papillae will have a bluish color. However, exacerbation of symptoms may periodically occur, which usually occurs against the background of a decrease in immunity during the period of colds.
Treatment of gingivitis in pregnant women
The so-called “gingivitis of pregnant women” develops against the background of hormonal surges, as well as a deficiency of vitamins and microelements in the body of the expectant mother. Therefore, patients are necessarily prescribed vitamin therapy.
During pregnancy, taking antibiotics is contraindicated, but in any case, the dentist should remove dental plaque and recommend safe antiseptics. Vacuum massage of the gums is also indicated.
You can rinse your mouth with a chamomile decoction at room temperature, this will help relieve bleeding and swelling of the mucous membrane. All oral medications should be used only after consultation with a gynecologist.
To protect your gums from mechanical damage, it is recommended to use toothbrushes with soft bristles, and also avoid eating too hard foods.
Classification of gingivitis
According to the nature of the course, gingivitis is divided into:
- Acute: occurs abruptly and is accompanied by progressive symptoms;
- Chronic: a long process with gradually increasing symptoms;
- Aggravated: increase in chronic symptoms;
- In remission: characterized by complete relief of gingivitis symptoms.
According to the form they are distinguished:
- Catarrhal gingivitis is characterized by unpleasant sensations in the gums, bad breath, impaired taste, and bleeding gums. Pain in catarrhal gingivitis intensifies during meals due to exposure to chemical and mechanical irritants. Periods of exacerbation of the disease are usually accompanied by malaise and low-grade fever. Acute catarrhal gingivitis occurs during the period of teething or changing teeth and is characterized by a sluggish course;
- Hypertrophic gingivitis is a chronic inflammatory process in which the gums grow. Most often, hypertrophic gingivitis is localized on the gingival margin in the area of the front surface of the lower and upper teeth. There are edematous and fibrous forms of hypertrophic gingivitis;
- Ulcerative gingivitis is an inflammation characterized by ulceration and necrosis, which develops with a decrease in the body’s reactivity as a hyperergic reaction (excessive) to the process of tissue sensitization by fusospirillary symbiosis. Ulcerative gingivitis is difficult to tolerate and affects the general condition of the human body. The gums are covered with a gray film, pain occurs when eating, the tongue is thickly coated, the saliva is viscous and thick. Ulcerative gingivitis is often accompanied by fever;
- Ulcerative-necrotizing gingivitis (Vincent), as a rule, occurs with a sharp decrease in immunity or with severe chronic diseases of the body. Ulcerative-necrotic gingivitis is characterized by ulcerations, the presence of areas of necrotic gingival papillae, loss of appetite, bleeding gums, putrid breath, and headaches. In most cases, high body temperature is observed against the background of necrotizing gingivitis.
Prices
The cost of dental treatment for gingivitis depends on the methods used and procedures performed. In all cases, therapy includes professional cleaning:
- 200 rubles for mechanical removal of plaque from one tooth;
- from 4,000 rubles for removing tartar using an ultrasonic scaler;
- from 4300 rubles for cleaning using the Air Flow method.
An additional fee will be charged for the treatment of periodontal pockets:
- 100-200 rubles for closed curettage of one pocket;
- from 2,000 rubles for open curettage in the area of one tooth and from 9,000 rubles for a quadrant (around 6-7 teeth).
After removing the stone, many patients experience pathological sensitivity of the teeth, so immediately after cleaning it is recommended to carry out fluoridation - saturation of the enamel with minerals. Coating one crown with fluoride varnish costs an average of 150 rubles.
If for complete rehabilitation it is necessary to cure a carious tooth, 3,500 rubles are added to the total price of therapy - the average price of a filling.
Air Flow device for the prevention of gingivitis
Causes
Dentists say the cause of gingivitis is superficial oral hygiene. The development of the disease is facilitated by pathogenic microorganisms that are present in dental plaque . In combination with accompanying factors, they can cause an inflammatory process of varying shape and severity.
There are people who have no symptoms of gingivitis, while others suffer from the most common symptom of the disease – bleeding gums.
Usually the process begins with the gum papilla becoming inflamed, and then its remaining parts are also involved. The disease quickly becomes chronic, with subsequent periods of exacerbation followed by periods of remission. The pathogenic flora of the oral cavity is very aggressive, so people suffering from gingivitis are twice as likely to suffer from cardiovascular diseases and diabetes.
Associated factors predisposing to plaque accumulation include:
- Physiological . Location and shape of teeth. Crowding, displacement, mobility of teeth, malocclusion. All these anatomical structural features make it difficult to brush your teeth and contribute to the accumulation of plaque. This also includes soft tissue defects - such as a shortened frenulum of the tongue and lips, lateral cords, and a small vestibule of the oral cavity, which facilitates the separation of the mucous membrane from the teeth during eating. The depressions that arise from this help plaque accumulate. Dentists also include oral breathing as a physiological factor, which stimulates the development of the inflammatory process due to the insufficient action of gingival fluid.
- Pathological . The presence of tartar makes it difficult to clean teeth from plaque and is a place where microorganisms accumulate. Trauma to the teeth through aggressive brushing, exposure of tooth enamel to cold and hot foods, and chemical damage also contribute to the development of gingivitis. Open caries is a bacterial reservoir that provokes plaque deposition.
- Wrong medical tactics . Mechanical damage to the oral cavity during careless dental procedures. Incorrectly placed, unground or unpolished filling with an overhanging edge, which helps to fix pathogenic flora. Complications during tooth extraction.
- Installation of prostheses and orthodontic devices . Both of them can damage the gums and make it difficult to brush your teeth.
- System factors . This includes taking medications and diseases of the body that reduce immunity. This group also includes factors such as: age, stress, severe genetic and endocrine dysfunction, blood pathologies, vitamin deficiency, metabolic disorders, severe chronic diseases, intoxication of the body and bad habits.
Causes of disease development in children
The main reason for the development of childhood and adult gingivitis is no different. A pathological process in the oral cavity causes plaque. Children's gum tissue is immature; unlike adults, it continues to grow and develop. Therefore, they are especially vulnerable to harmful factors.
If a child’s defenses are weakened, he suffers from infections or gastrointestinal disorders, is susceptible to allergic reactions, endocrine dysfunction, heart and vascular disease, and does not receive enough vitamins from food, then optimal conditions are created for the development of inflammation.
A key predisposing factor to gingivitis in a child is impaired self-cleaning of teeth, which can lead to:
- early removal of baby teeth;
- treatment by an orthodontist;
- pathological structure and fixation of the frenulum of the lips and tongue;
- viscous composition of saliva;
- poor nutrition;
- the presence of carious teeth and inflamed dental vessels and nerves;
- congenital defects of the salivary glands;
- uneven load on the dentofacial apparatus;
- prolonged teething.
Causes of gingivitis in pregnant women
The main reason for the development of the disease in pregnant women remains the same. The main role in the appearance of the inflammatory process is played by dental plaque . Carrying a child is accompanied by changes in hormonal levels and the functioning of all vital organs and systems of a woman. This almost always causes bleeding gums.
Doctors have proven that under the influence of an increased amount of hormones, the gums become more susceptible to the pathogenic flora of dental plaque. This, in turn, contributes to the occurrence of swelling and inflammation. The composition of dental plaque in expectant mothers is slightly different because some types of microbes begin to use female hormones as nutrients instead.
Prevention of acute gingivitis
Prevention of this disease is quite simple. If you follow all the tips and recommendations written below, the risk of the disease will be reduced to a minimum. To prevent the development of the disease, it is necessary to:
- visit the dentist regularly, at least 2 times a year, even if nothing bothers you;
- maintain simple oral hygiene;
- Have your teeth professionally cleaned every six months at the dental clinic.
Important : in addition to brushing your teeth daily in the morning and evening, you should use pharmaceutical mouth rinses. Dentists also recommend learning how to use dental floss.
Additional measures
To treat gingivitis in adults and children, it is necessary to use additional measures in the form of physiotherapeutic treatment and diet correction.
Nutrition
For several weeks after completing the course, you must adhere to some rules to completely cure the pathology.
The main recommendations are as follows:
- food should be warm and pureed;
- it is necessary to increase the amount of cereals, soups, and stewed vegetables in the diet;
- exclude the consumption of alcohol, carbonated and caffeinated drinks;
- You should not eat sour, salty, hot, spicy, smoked foods.
It is strongly recommended to minimize the amount of canned food, marinades, sauces and hard foods that irritate the gums.
Physiotherapy
To speed up recovery, physiotherapy methods are used to help stop the development of the pathological process.
The most common types of treatment will be:
- Irradiation of the affected area with ultraviolet light helps stimulate tissue regeneration, prevents the development of complications, and destroys pathogenic microorganisms. The procedure is performed for adults and children from 3 years of age. It will take up to 10 sessions for complete recovery.
- Electrophoresis with medicinal solutions or ointments helps in the treatment of advanced forms of the disease. During the session, tissue permeability improves, the components of the drug reach the area of inflammation directly. At least 5 procedures are performed to obtain a lasting result.
- Hydrotherapy with special water enriched with carbon dioxide gently cleanses the surface of the teeth, prevents the accumulation of dental plaque, and soothes sore gums. The course consists of 7-10 sessions.
Physiotherapeutic procedures act as an auxiliary element of treatment and help speed up the healing process.
Treatment of ulcerative-necrotizing gingivitis
This form of gingivitis is treated by a dentist. First, fossilized plaque and deposits are removed, as well as necrotic areas of the mucosa. After removing the infected tissue, rinse with an antiseptic solution - peroxide, Chlorhexidine. Hydrogen peroxide eliminates the accumulation of bacteria and stops bleeding.
In case of severe bleeding, instead of peroxide, drugs that break down necrotic tissue are used. For example, Trypsin is prescribed, which resolves dead epithelial cells.
Then a course of antibiotics is prescribed to destroy anaerobic microorganisms, spirochetes and fusobacteria. In addition to manipulations, antiseptic rinses and gel applications are prescribed. After eliminating the aggressive microenvironment, medications are prescribed to restore the mucosal epithelium, for example, Solcoseryl gel.
Possible complications
Ignoring symptoms or self-medication leads to the development of severe complications. The most common will be periodontitis and periodontal disease. They affect tooth enamel, alveolar processes and lead to tooth loss.
When an infection occurs, an abscess may form, requiring surgical intervention. When the disease spreads to the mucous membranes of the oral cavity, the upper respiratory tract is affected, and symptoms of tonsillitis, laryngitis, and sore throat appear.
The tongue often suffers, ulcers appear on the surface, wounds affect healthy areas, preventing normal conversation and eating.
Symptoms of acute gingivitis
Acute gingivitis occurs with symptoms such as:
- swelling of the gums;
- increased temperature in the mouth;
- pain syndrome;
- bleeding gums;
- the appearance of ulcers;
- Tartar deposits.
Bleeding gums.
As a rule, the general condition of patients with acute gingivitis remains the same. But sometimes, additional symptoms of this disease can be: a rise in body temperature to 39 degrees, bad breath, sore gums when eating and drinking cold or hot drinks, general weakness, enlarged lymph nodes.
Important : with acute gingivitis, the gums become bright red. They swell and begin to bleed when touched.
Forms
Acute gingivitis can occur in 3 forms:
- Easy.
- Medium-heavy.
- Heavy.
In mild cases, inflammation develops only in the area of the interdental papillae. In the moderate form, not only the papillae are affected, but also the marginal edge of the gums. The severe form has the most vivid clinical picture. Almost the entire area of the gum is affected by inflammation (papillae, marginal margin and tissue attached to the alveolar bone).
Acute inflammatory process can be local and generalized. With local damage, the inflammatory process covers a small area located in the area of 3–4 teeth. Generalized gingivitis is characterized by damage to the entire gum. In the generalized form, the symptoms of the disease are more pronounced and are often accompanied by general manifestations.
Depending on the nature and etiology, acute gingivitis is classified into the following forms:
- catarrhal;
- ulcerative;
- ulcerative-necrotic;
- hypertrophic.
Disease prevention
To prevent the occurrence of the disease, a number of conditions must be met:
- use a soft brush;
- use toothpaste with ingredients that care for gums and teeth, a special rinse and dental floss to remove food particles between the teeth.
Gingivitis causes tooth loss more often than caries. Although in the first stages it can be treated with the help of a dentist without much discomfort. As long as the periodontal ligaments are not atrophied and the teeth are held in place, the disease can be cured by promptly consulting a dentist.
Rating: (
1 ratings, average: 5.00 out of 5)
Treatment
Therapeutic measures are aimed at eliminating signs of gum inflammation and normalizing the general condition. Treatment for adults and children is somewhat different. During pregnancy, a special approach is required to avoid any negative impact on the baby.
Adults
You can find out how to treat gingivitis in an adult from your dentist. Typically, therapy depends on the clinical manifestations and the degree of neglect of the condition.
The standard regimen involves the use of the following groups of drugs:
- Antibacterial medications are indicated in case of infection or inflammation spreading to large areas. The most commonly prescribed broad-spectrum tablet medications are: Erythromycin, Ciprofloxacin, Sumamed. The duration of treatment ranges from 7-10 days.
- Local anesthetics are used to relieve severe pain. A spray containing lidocaine is suitable; they are used 2 to 4 times per knock until acute clinical manifestations disappear.
- Non-steroidal anti-inflammatory drugs are indicated for severe conditions. They relieve pain and lower body temperature. Ibuprofen or any drug containing Nimesulide, for example Nimesil, will do. You are allowed to take medications for no longer than 4 days in a row without consulting a specialist.
- Antiallergic drugs are usually prescribed to patients with a tendency to such manifestations in combination with other medications. Tavegil, Claritin, Zodak are considered effective.
- Ointments with regenerating properties help speed up healing and have antimicrobial and anti-inflammatory effects. An effective medicine would be Solcoseryl, Traumeel S. The drugs must be used for at least 5 days in a row.
- Antiseptics for local use. Tantum Verde solution is ideal. Has an antiseptic, anti-inflammatory effect, prevents the spread of bacteria in the oral cavity. Used for rinsing 1 to 3 times a day for 10 days.
- Vitamin complexes to strengthen the immune system will speed up recovery. It is allowed to take any multivitamin complex: Alphabet, Supradin, Complivit, Vitrum. The minimum course is 30 days.
A disease not complicated by infection can be treated without the use of antibiotics. The decision is made by a specialist, who also determines the dosage and duration of the course.
Children
The treatment regimen for children is almost no different from that for adults. For children, smaller dosages of similar antibacterial agents are used; the course is determined by the pediatric dentist during the initial examination.
Among antihistamines, preference should be given to Claritin in the form of syrup. Anesthetics in the form of a spray are used less frequently, but Kalgel gel is prescribed, which contains lidocaine, approved for infants.
Among non-steroidal anti-inflammatory drugs, medications containing ibuprofen are chosen to alleviate the child’s condition and improve sleep. Ointments are rarely prescribed to children. Usually a numbing gel is sufficient. Vitamin complexes are required. The manufacturer of Alphabet offers a wide selection of vitamins for children of different ages.
It is not recommended to treat yourself: there may be a risk of developing severe complications.
Pregnant and nursing
During pregnancy and breastfeeding, most medications should not be taken. Dentists recommend that all women monitor their oral health and prevent the formation of dental plaque through good hygiene.
If symptoms of gingivitis appear, you should consult a specialist. Doctors usually allow the use of Kalgel, which has minimal side effects. Absorption into the blood occurs in small quantities. The drug has no effect on the baby’s body and does not pass into breast milk.
In the absence of allergies, you can additionally use herbal decoctions of chamomile, sage, and calendula. To prepare, you need to boil a tablespoon of raw material in 500 ml of water, cool and filter. Rinse your mouth up to 3 times a day for a week.
In the absence of a therapeutic effect, only a specialist determines the further sequence of actions.
How is gingivitis different from other gum diseases?
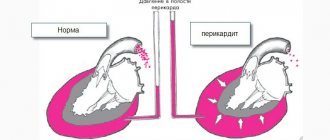
Gingivitis, periodontitis and periodontal disease are gum diseases that have similar symptoms, but differ in severity and consequences.
Gingivitis is the initial stage of the inflammatory process that does not affect the ligaments of bone tissue and periodontal tissue. When diagnosed with gingivitis, treatment in adults with drugs
in combination with professional cleaning of tooth enamel shows excellent results.
If the patient ignores the problem, gingivitis progresses and becomes a complicated form, which is already diagnosed as periodontitis. With this disease, the inflammatory process spreads to the tooth tissue and provokes the formation of periodontal “pockets” in which purulent masses accumulate. All this leads to tooth mobility and subsequent loss.
Periodontal disease can occur as a result of untreated gingivitis and periodontitis, as well as independently under the influence of certain provocateurs. These may be disrupted metabolic processes, which result in mucosal atrophy (decrease in volume), which leads to exposure of tooth roots. As a rule, this disease is more common among older people, and this is due to natural age-related changes in the body.
Main distinctive features:
1. With gingivitis, the inflammatory process affects only the gums; with periodontitis, pathological changes are observed in all periodontal tissues. With periodontal disease, inflammation may be completely absent.
2. Periodontal “pockets” are formed only during periodontitis.
3. With gingivitis and periodontal disease, tooth mobility is not observed. This symptom is also more characteristic of periodontitis.
4. Gingivitis does not have serious consequences and is easily eliminated with therapeutic treatment. With periodontal disease and periodontitis there are risks of serious complications, and surgical methods may be chosen to treat the disease.
Folk remedies
In the initial stages, gingivitis can be treated with folk remedies. Basic recipes for treating gingivitis at home:
- cut an aloe leaf, knead it slightly and apply to the sore areas of the gums;
- pour boiling water over a collection of yarrow, calendula, chamomile (take herbs in equal proportions) and leave for an hour in a thermos. Use for rinsing;
- make a decoction of sage and use it for medicinal rinses up to 5-6 times a day;
- Mix oak bark and celandine in equal proportions, pour boiling water over it, let it brew and rinse your mouth with the infusion.
- massage with rosehip and sea buckthorn oils;
- rinsing with propolis tincture - 10 drops of alcohol infusion per glass of water.
Types and classification
Modern medicine knows the following types of gingivitis:
- Atrophic. Against the background of pathological processes, soft tissue atrophy occurs, resulting in recessions.
- Catarrhal. The simplest and most quickly treatable form. With its development, inflammation of the gums and papillae occurs, relief is lost, and bleeding occurs.
- Hypertrophic. Soft tissues begin to grow, dental crowns are completely or partially covered by gums. Painful sensations arise, severe itching appears, and the mucous membranes begin to bleed.
- Ulcerative-necrotic. In parallel with the standard symptoms, the following signs appear: ulcerative lesions appear, hyperemia is observed, and general health deteriorates.
Symptoms of atrophic gingivitis
The classification of gingivitis distinguishes the atrophic type of the disease.
It occurs with significant degradation of the affected gum tissue, as a result of which the tooth root is exposed.
The main reasons for the progression of the disease are improper orthodontic treatment and impaired gum growth.
Symptoms of atrophic gingivitis:
- severe pain and itching in the gum area upon contact with hot, cold or sour foods;
- the formation of ulcers and wounds that do not heal for a long time and in some cases begin to fester;
- swelling with a large number of microtraumas of the gum surface.
Treatment during pregnancy
During pregnancy, hormonal levels change, which affects the condition of the gums. The disease is noted by the vast majority of expectant mothers, but in each patient it manifests itself differently. Some people experience bleeding gums when brushing their teeth, while others experience severe pain in the mouth and overgrowth of certain areas of soft tissue.
If gingivitis is mild, then in addition to careful oral care, pregnant women are prescribed:
- Miramistin for treating gums or Tantum-Verde;
- treatment of mouth with Chlorhexidine solution;
- resorption of Lizobact tablets;
- treatment of damaged areas with sea buckthorn or rose hip oil;
- applying Levomekol ointment to ulcers and purulent papules.
Gingivitis is a common disease that affects adults and young children equally often. Typically, each form of the disease begins with signs of catarrhal gingivitis: redness and bleeding of the gums and their pain when brushing. These signs should not be ignored, since early treatment will prevent the development of pathology and its consequences.
Prevention and hygiene rules
To avoid developing gingivitis, maintain good personal hygiene. Replace the medium-hard brush with a soft or silicone one - such products do not injure the gums. Choose the right paste for gingivitis, do not forget to floss.
Brushes need to be changed regularly - at least once a quarter. Also
Regular rinsing is a good way to soothe your gums - at least twice a day, ideally after each meal. You can rinse your mouth with plain water, special products, or herbal decoctions. Carefully remove dental plaque - the main reason for the active proliferation of bacteria and, accordingly, the development of gingivitis.
Regular use of gum protection pastes will prevent many problems. They can be alternated with any others.
How to treat gingivitis
If gingivitis occurs, treatment includes several stages and is carried out by a dentist. To cure gingivitis, you need to remember three main rules for its treatment:
- A complex approach . When treating any form of the disease, it is necessary to use both local and general therapy. It is necessary to treat not only the symptoms, but also to eliminate the causes of the disease.
- Individual approach. Correctly chosen treatment must take into account all the associated factors of the disease, the state of health and the patient’s immune system.
- Systematicity. If the disease has become chronic, then systematization of treatment is necessary to bring it into stable remission.
Therapy differs somewhat depending on the form of the disease, but treatment of any gingivitis must begin with eliminating foci of infection in the oral cavity (treatment of caries) and removing hard dental deposits. These procedures can only be performed by a dentist; you should not try to remove tartar at home using any traditional methods. This can only injure inflamed gums and aggravate the pathological process.
Often, gingivitis indicates a decrease in the body's defenses. Therefore, in addition to eliminating the inflammatory process, treatment should also be aimed at increasing the overall protective functions of the body. In this case, the appointment of immunocorrectors is quite justified. Drugs in this group activate the protective forces of the oral mucosa.
The prognosis for gingivitis is favorable, but if left untreated, the process can develop into a deep form - periodontal disease can develop, which can lead to tooth loss.
Causes of gingivitis
The causes of the disease are divided into external and internal. External ones include:
- smoking;
- injury to the gums with a hard toothbrush;
- burns;
- radiation exposure;
- penetration of infection;
- mouth breathing;
- women's use of oral contraceptives;
- poor-quality prosthetics and fillings.
- improper oral care;
- tartar, caries;
- malocclusion;
- vitamin deficiency and lack of minerals;
- weak immunity;
- allergic reactions;
- diseases of the endocrine system;
- ARVI;
- tuberculosis;
- AIDS;
- diabetes;
- pregnancy;
- disorders of the gastrointestinal tract.
Read also: Relieve gum inflammation
In babies, gingivitis occurs during teething. The main reason is the habit of children to put foreign objects in their mouths, which damage the gums and cause infection. The use of orthopedic structures leads to the proliferation of microbes that can cause disease. In adolescents, gingivitis occurs due to hormonal imbalance during puberty.