Meniere's disease is a non-inflammatory disease that occurs in the inner ear and is accompanied by progressive hearing loss, recurrent attacks of deafness, loss of balance, dizziness and tinnitus.
The manifestations of this disease were first described by the French physician Prosper Meuniere in 1861, which later gave the disease its name. It is classified as a rare disease: between 20 and 200 cases are diagnosed per 100,000 population. Meniere's disease mostly affects residents of large cities aged 20 to 50 years who are engaged in intellectual activities.
How does Meniere's disease occur?
The human ear is formed of three parts - the outer, middle and inner ear. Sound passing through the canal of the outer ear causes the eardrum to vibrate. In the tympanic cavity (middle ear) there are three auditory ossicles - the malleus, incus and stapes, which transmit sound vibrations to the inner ear.
This part of the hearing organ, also called the labyrinth, is located in the temporal bone. It consists of the vestibule, cochlea and semicircular canals. The sound-receiving apparatus and receptors of the vestibular analyzer are located here. The cavities of the inner ear are filled with endolymph, a viscous and liquid medium involved in the conduction of sound.
Meniere's disease affects this area. The mechanism of its occurrence has not been fully elucidated. Many researchers are inclined to believe that this disease is formed due to increased pressure in the inner ear due to the accumulation of excessive amounts of endolymph in it. An excess of this fluid can cause its increased production, disruption of circulation and absorption processes.
to contents ^
What it is?
Meniere's disease is a disorder of the inner ear that causes an increase in the amount of fluid in its cavity, which puts pressure on the cells that control the body's orientation in space and balance.
It was first described by a French doctor in 1861 and bears his name. The disease occurs among people of different ages from 17 to 70 years old; children are practically not susceptible to Meniere's disease. More often people aged 30-50 years suffer. There were no gender differences in the frequency of occurrence.
Usually the disease affects the inner ear on one side, but in 10-15% the process may initially be bilateral. Sometimes, during the long-term existence of the disease in a patient, a unilateral process transforms into a bilateral one.
https://youtu.be/gOCemp3boY8
Causes of Meniere's disease
To date, several theories have been developed to explain the causes of the disease.
- Anatomical theory indicating the pathological structure of the temporal bone of a sick person.
- People susceptible to this pathology are more likely to experience allergic manifestations compared to the general population. This gave rise to the emergence of an allergic version of the occurrence of Meniere's disease.
- A genetic theory supported by diagnosed familial cases of the disease, which indicates autosomal dominant inheritance.
- Proponents of the viral theory note the provoking effect of a viral infection (for example, cytomegalovirus), which triggers an autoimmune mechanism for the development of the disease.
- The vascular version is supported by cases of simultaneous diagnosis of Meniere's disease and migraine.
- According to the metabolic theory, due to potassium retention associated with impaired endolymph circulation, potassium intoxication of cells occurs in the structures of the inner ear. This leads to dizziness and hearing loss.
Many modern researchers are inclined to believe that this pathology has several causes, highlighting the factors that cause the disease and predispose to its development.
to contents ^
Degrees of the disease
There are three degrees of the disease:
| Lightweight | Attacks of vestibular function disorder are rare and last no more than 1-2 hours, most often a few minutes. After which a long period of remission begins, which practically does not affect the person’s ability to work. |
| Average | An increase in the frequency of attacks of dizziness and nausea; after regaining coordination, a rest period of 3-5 days is necessary. |
| Heavy | A person is given disability due to loss of ability to work. The attacks are long-lasting, from 5 hours to several days. Their frequency is on average 1-5 days. At the same time, there is no need to talk about restoration of working capacity. |
Against the background of this classification, reversible and irreversible forms of pathology are distinguished. Reversible is a mild degree, which is characterized by an increase in the duration of periods of remission and restoration of hearing. In the irreversible form, the patient’s condition worsens or does not make positive progress, there is a persistent decrease in hearing, an increase in the number of attacks, and vestibular disorders may be permanent.
How does Meniere's disease manifest?
The disease is characterized by a triad of symptoms, described in detail by Prosper Meniere:
- Attacks of dizziness of a systemic nature. They appear suddenly, without provoking factors, regardless of the time of day and the general condition of the person (he may feel absolutely healthy). The severity of the dizziness is such that the patient is unable to stand or even sit. Sometimes they are preceded by noise and congestion in the ear - this phenomenon is called an aura. Attacks always occur against the background of various vegetative manifestations. The most common of these are nausea and vomiting, which worsen when trying to change body position.
- Noise in the affected ear. In most cases, Meniere's disease affects one ear; only 10-15% of patients are diagnosed with a bilateral disease. Over time, a unilateral pathological process can develop into a bilateral one. Depending on this, the localization of noise in the ear changes. It gets worse before and during an attack of dizziness.
- Hearing loss, steadily progressing and leading to impaired perception of the entire range of sounds. In the absence of therapeutic measures, complete deafness gradually develops.
You may be interested in reading about ear pain, its diagnosis and treatment. Read
During attacks, the patient has a feeling of sinking or rotating his body, or displacement of surrounding objects. Shortness of breath, tachycardia and increased sweating are noted.
Manifestations of Meniere's disease significantly reduce the quality of life and sometimes lead to loss of ability to work.
to contents ^
Let's clarify the difference between the syndrome and Meniere's disease
In modern medicine, a distinction is made between Meniere's disease and Meniere's syndrome. A disease is a self-occurring pathology, and a syndrome is one of the symptoms of a pre-existing disease. This could be, for example, labyrinthitis (inflammation of the labyrinth), arachnoiditis (inflammation of the lining of the brain) or a brain tumor. In the syndrome, pressure in the labyrinth is a secondary phenomenon, and treatment, as a rule, is aimed at correcting the underlying pathology.
According to recent studies, in the modern world manifestations of Meniere's syndrome are becoming more and more common, and the disease is becoming a rare occurrence.
Features of the course of Meniere's disease
In the development of this disease, experts distinguish an exacerbation phase (repeated attacks) and a remission phase - a period when there are no pathological manifestations.
Raynaud's disease: symptoms, causes, which doctor treats
The disease can occur in the following forms:
- The cochlear form is the initial appearance of hearing impairment, and then vestibular.
- The classic version is when auditory and vestibular disturbances make themselves felt simultaneously; the first moment of dizziness is accompanied by noise in the ear and hearing impairment.
- Vestibular form: the period of exacerbation begins with vestibular dizziness, and auditory disorders appear only after some time.
The development of Meniere's disease goes through 3 successive stages.
- Initial . Systemic dizziness makes itself felt infrequently, 1-2 times a year, sometimes every 2-3 years. They appear at any time of the day, usually lasting from 1 to 3 hours, accompanied by nausea and vomiting. Noise, fullness, or a feeling of fullness in the ear may be bothersome before or during an attack, but are not permanent symptoms. At this point, temporary hearing loss may occur.
- The height of the disease. The nature of the attacks becomes typical of Meniere's disease, with severe systemic dizziness and vivid vegetative manifestations. They bother the patient several times throughout the week or month. The noise and sensation of fullness in the affected ear become constant and intensify during exacerbations. The hearing loss is progressing.
- Decaying stage . Periods of systemic dizziness gradually occur less and less often and may disappear altogether, but the person constantly feels the instability of his own body. His hearing in the affected ear is significantly reduced; at this stage, the second ear is often involved in the pathological process. Some patients develop conditions called Tumarkin crises, which involve sudden falls without loss of consciousness or dizziness.
Taking into account the possibility of maintaining working capacity, the frequency of occurrence and duration of attacks, 3 degrees of severity of Meniere's disease are distinguished.
- A mild degree is characterized by short exacerbations and long periods of remission, sometimes reaching several years.
- In moderate cases, periods of exacerbation occur weekly or monthly and last for several hours. During the attack and immediately after its completion, the ability to work is lost.
- Severe degree is characterized by frequently (daily, weekly) repeated exacerbations lasting several hours with all the manifestations typical of Meniere's disease. The person becomes unable to work.
Hearing impairment in Meniere's disease is steadily progressive. At the beginning of the disease, there is a deterioration in the perception of low-frequency sounds, then the entire sound range. Hearing loss increases with each new exacerbation and gradually turns into complete deafness, with the onset of which the attacks of dizziness usually stop.
At the beginning of the development of mild to moderate Meniere's disease, a combination of periods of remissions and exacerbations is noted. Subsequently, the clinical picture changes: during the period of remission, patients retain general weakness, vestibular disorders and hearing impairment.
The course of this disease is often unpredictable: pathological manifestations can become either more pronounced or gradually disappear. There are situations when Meniere's disease gradually goes away on its own, no longer reminding itself of painful relapses.
to contents ^
Forecasts
The future course and forecasts vary. The disease can be divided into several stages:
- early - oddly enough, the most unpleasant;
- progressive;
- late.
A prognosis of the disease can be made based on the later stages. Prediction is difficult due to the fact that the disease is characterized by periods of exacerbations and remissions.
With early detection of pathology and strict adherence to all doctor’s recommendations and preventive measures, Meniere’s syndrome has a more favorable prognosis.
Over time, the patients' condition tends to spontaneously stabilize. However, many patients experience a decrease in hearing acuity.
How is diagnosis carried out if Meniere's disease is suspected?
There is no universal way to diagnose this disease, since it is characterized by a combination of diverse symptoms. A comprehensive clinical study is required to confirm the diagnosis.
Diagnostic measures for suspected Meniere's disease begin with a study of existing complaints and examination of the patient. To exclude the possibility of inflammatory diseases of the hearing organ, the doctor performs an otoscopy - examining the ear for the presence of pathological changes and studying the condition of the eardrum.
In addition to laboratory blood tests using generally accepted methods, tests for glucose tolerance and thyroid function are recommended.
To assess the state of the patient’s balance system, he is given vestibulometric tests - the study of spontaneous vestibular reactions:
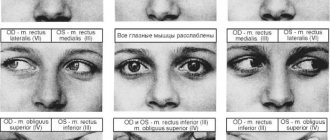
- Spontaneous nystagmus . The patient fixes his gaze on an object located in front of his face at a distance of about 30 cm. The doctor moves the object from one side to the other, up, down and diagonally. The patient tracks the moving object with his gaze, and the doctor notes the position of his eyes.
- Vestibulo-ocular reflex , indicating whether the patient can maintain gaze fixation on an object that moves along with head movements. For example, the doctor may ask the subject to look at the thumbs, brought together and extended forward, and at the same time rotate the torso and head to the sides.
- Function of static balance (Romberg test, in which the patient stands with his feet together and his eyes closed. To complicate the performance, he may be asked to stretch his arms forward or place his feet one after the other).
- Dynamic balance function , carried out to assess the patient’s ability to maintain adequate body position during active movement in space. To do this, the subject is asked to perform various walking options.
Crohn's disease: which doctor to contact, symptoms, treatment
In order to study the state of the patient's vestibular apparatus, rotational tests are used, with the help of which reactions to changes in body position are monitored (rotation in the Barany chair, tests carried out on special computer stands, sinusoidal pendulum test). On the eve of such tests, it is not recommended to consume alcoholic beverages or medications that alter the activity of brain centers. The procedures are carried out on an empty stomach.
To determine the degree of hearing impairment, the following examinations are prescribed:
- Audimetry is the assessment of hearing acuity by monitoring the minimum sound intensity perceived by the patient.
- Studying the state of the auditory analyzer by using different tuning fork tones.
- Otoacoustic emission is the study of the acoustic response of the patient's cochlea to sound.
- Electrocochleography is the study of hearing level using a microelectrode, which, under local anesthesia, is installed on the eardrum or in the area of the external auditory canal.
In order to exclude the possibility of diagnosing an acoustic neuroma, patients with suspected Meniere's disease are prescribed an MRI of the brain.
To diagnose increased endolymphatic pressure, the patient is given a glycerol test. The patient, no less than 12 hours after the last drink of liquid, takes orally a mixture consisting of water or fruit juice and pure medical glycerin at the rate of 1.5 g per 1 kg of body weight. Before this, an audiometric test is done. After 2-3 hours, the necessary examinations are carried out.
to contents ^
Diagnostics
The diagnosis of Meniere's disease is established taking into account specific symptoms and the results of instrumental studies. The American Academy of Otolaryngologists, based on clinical manifestations, distinguishes three degrees of reliability of BM: possible, probable and definite BM. An important diagnostic criterion is the triad of symptoms - dizziness, tinnitus and hearing loss. The diagnosis is confirmed by gradual deterioration of hearing and repeated episodes of vestibular attacks.
Among the instrumental methods for diagnosing Meniere's disease are:
- The main method, according to international diagnostic criteria, is pure tone threshold audiometry. The result of such a study will be an audiogram, which graphically depicts the function of the hearing organ;
- Otoscopy is performed to exclude middle ear pathology;
- Extratympanic electrocochleography evaluates the performance of the auditory nerve;
- A tuning fork test determines the type of hearing loss. In this case, the hearing loss is of the conductive type.
These methods allow you to analyze the degree of hearing impairment. Audiometry is the main criterion when choosing treatment tactics. To detect endolymphatic hydrops, doctors use electrocochleography and a dehydration test.
Return to an active life: how Meniere's disease is treated
Treatment of this disease has two goals: stopping the attack that has occurred and preventing new exacerbations.
All currently known treatment options for Meniere's disease are aimed at alleviating the attack; they cannot influence the sequential development of hearing loss. However, timely therapy prescribed on an individual basis can slow down this pathological process and significantly reduce the frequency and severity of attacks.
To relieve pathological manifestations, sedatives are used, such as diazepam (Relanium), vestibular blockers (Dramine, meclozine). In the acute period, in case of severe vomiting, it is advisable to use drugs in the form of suppositories or administer drugs intramuscularly or intravenously.
Between attacks, complex supportive therapy is carried out using drugs aimed at all components of the pathological process:
- Diuretics (diuretics), prescribed to reduce the accumulation of fluid in the inner ear.
- Drugs that improve cerebral circulation (cinnarizine).
- Histamine-like drug Betahistine dihydrochloride, which reduces the intensity and duration of dizziness, affecting the functioning of the vestibular apparatus.
In the interictal period, people suffering from this disease are recommended reflexology (acupuncture).
Of great importance for patients with Meniere's disease is a diet based on limiting the consumption of salt, liquid, caffeine, and excluding spicy and fatty foods. Drinking alcohol and smoking are contraindicated. In order not to provoke new attacks, it is important to minimize neuropsychic overload associated with stress.
It is not recommended to limit physical activity between attacks. It is advisable to regularly perform exercises aimed at training the vestibular apparatus and coordination of movements.
If conservative therapy does not produce results, the patient is offered surgical treatment.
At the present stage, surgical methods for treating Meniere's disease are used in only 5% of patients.
to contents ^
Definition and forms
Meniere's syndrome is a condition that develops against the background of increased pressure in the endolymphatic system, which predetermines characteristic symptoms and influences the choice of tactics and treatment. It is more often diagnosed in Caucasian patients aged 40-60 years. Mostly, residents of megacities who are engaged in intellectual activities are affected. Meniere's disease is a slowly progressive disease that occurs in the following forms:
- Classic. Manifested by auditory and vestibular disorders.
- Cochlear. Debuts with auditory symptoms followed by the addition of vestibular signs.
- Vestibular. It is characterized by attacks of dizziness, which are subsequently supplemented by hearing disorders.
At the initial stages, the pathology proceeds in paroxysms, periods of exacerbation alternate with periods of remission, when clinical manifestations are completely absent. In the later stages, hearing disorders (hearing loss, imbalance) become permanent.
Pathology of the inner ear caused by endolymphatic hydrops is rarely diagnosed in childhood. Pathology is detected among women more often than among men. The disease occupies 2nd position in the list of causes of dizziness, giving 1st place to benign positional vertigo of the paroxysmal type.
Causes of Mayer-Rokitansky-Küstner syndrome (MRKS)
There is still no definite opinion in medical science about what causes MRKH syndrome. It is believed that the disease occurs during fetal development and is associated with an anomaly of the Müllerian ducts, from which the female genital organs are formed. This occurs in the first trimester of pregnancy (up to 12 weeks). The fallopian tubes form from the upper part of the ducts. The uterus is formed from the middle section, and the upper part of the vagina is formed from the lower. When this order is disrupted, organs are formed incorrectly or their development stops.
Various diseases of a woman during pregnancy can cause significant harm to the unborn child.
Risk factors include diseases of the cardiovascular system, hypertension, and hormonal imbalance. At the stage of organ formation, it is important that the fetus receives a sufficient amount of oxygen. If the metabolic processes between the mother and the unborn baby are disrupted, there is a high probability of developing abnormalities.
Patients with diabetes mellitus during pregnancy should be under close medical supervision and follow his recommendations.
Under the influence of chemicals, as well as some medications, during pregnancy the amount of protein (MIS) in the embryo is significantly reduced, and therefore the pathological process affects the Müllerian ducts.
A genetic predisposition to the disease cannot be ruled out. Cases have been recorded in which the syndrome manifested itself in representatives of the same family.
Diet for Meniere's syndrome
Very often situations arise when excess fluid in the inner ear is combined with high blood pressure and excess fluid in the body as a whole. The manifestation of the disease can be reduced with a special diet. The diet should be formulated in such a way that excess fluid is freely removed from the body and is not retained in it.
It is especially important to follow a diet during an exacerbation. It is based on the following principles: limiting fluid intake to 1.5 liters per day, eliminating strong coffee and tea, avoiding alcoholic beverages, prohibiting fried, salty and spicy foods, and reducing salt intake.
There are no specific products that will help eliminate the disease. The diet should be based on the exclusion of foods that can worsen the patient's condition.
Kinds
There are several types of Meniere's disease, each of which has some characteristics.
Neurological
This type of pathology is characterized by attacks of vestibular disorders and hearing impairment. It is the neurological type of the disease that has the most favorable prognosis.
Neurotic
This type of disorder is characterized by hearing loss in the form of attacks or permanent deafness on a specific side.
Hemorrhagic
With this type of disease, blood cells penetrate into the endolymph. As a result, fluid pressure suddenly increases, leading to complete loss of vestibular function and the ability to hear. Usually the disease is unilateral, but sometimes the pathological process affects both ears.
Bilateral
When this form of Meniere's disease occurs, the abnormal process affects both ears simultaneously.
Drug therapy
It is not possible to completely get rid of this disease. Drug therapy can stop attacks of dizziness and prevent the development of complications in the future. It is also almost impossible to completely restore hearing, but sometimes there are exceptions.
How to treat Meniere's disease? First of all, doctors prescribe diuretics (Furosemide) to eliminate fluid accumulated in the inner ear. They do not contribute to the cessation of the pathological process, but significantly alleviate the patient’s condition. Osmotic diuretics are considered more effective; they are used only during hospitalization and administered intravenously.
In addition to antihistamines (Suprastin, Fenkarol) and diuretics, antipsychotics (Triftazin, Aminazine) and vasodilators (No-spa) are also prescribed.
A balanced diet plays an important role in the treatment of the disease. Patients should choose lean foods, eat more raw vegetables and fruits, as well as greens. Doctors recommend reducing caffeine and salt in your diet for a while. Of course, for the entire duration of therapy it is necessary to abstain from drinking alcoholic beverages, soda, fast food and smoked foods.
To train the vestibular system, you should regularly perform physical therapy exercises. The treatment complex is usually selected individually depending on the patient’s condition. During the period between attacks, physical activity should not be limited.
Diagnosis of the disease
Early diagnosis of Meniere's disease increases the chances of successful treatment. The diagnosis is made based on clinical signs and data:
- audiological examination,
- neurologist consultations,
- otoscopy,
- electrocochleography,
- studies of the functioning of the vestibular apparatus,
- thyroid examinations,
- blood tests for hormones,
- magnetic resonance imaging,
- promontorial test,
- tuning fork examinations,
- bacteriological tests,
- indirect otolitometry,
- stabilography,
- electronystagmography,
- videoculography,
- auditory evoked potential studies.
It is very important in the treatment process to differentiate Meniere's syndrome from pathologies of the hearing organs: otitis media, eustachitis, vestibular neuronitis, tumors, etc.
Traditional medicine
To use traditional medicine methods, first of all, it is necessary to professionally confirm the diagnosis so as not to mistake it for Meniere’s disease, for example, a hypertensive crisis, characterized by similar manifestations. And under no circumstances refuse the help of a doctor who will help you avoid mistakes and tell you how to treat Meniere’s disease.
During the acute phase of the disease, it is necessary to help the patient do the following:
- Take a horizontal position - preferably in a comfortable position, because any movement aggravates the patient's condition.
- Avoid compresses and lotions.
- If the acute phase is over and the patient still feels unwell, you can offer 1-2 slices of lemon with peel in tea before bed. You can also add mint, lemon balm, and linden blossom.
- After the end of the acute phase, the patient may still hear tinnitus for some time. To get rid of noise, the following exercise is suggested: the palm is pressed tightly to the ear and rotated clockwise for 2 minutes, after which the palm must be sharply withdrawn.
- The amount of water and salt that retains it should be limited.
Instead, traditional medicine recommends introducing phosphorus-containing foods into the diet: fish, bran, nuts, yolk. Sea kale is also recommended, which can be eaten fresh or dried, adding a teaspoon to various dishes.
Among the popular infusions and mixtures, the following are described:
- Rose hips, meadowsweet flowers, hawthorn and motherwort herb are mixed in a tablespoonful and poured with a liter of boiling water, hiding the mixture in heat for a day. And then for 3 months, drink one glass three times a day before meals.
- For nausea and vomiting, 20 g of mint is immersed in half a liter of boiling water and left for 20 minutes. For the same amount of water, you can take 12-13 g of dry centaury or caraway seeds. This infusion is drunk in 2 tablespoons: mint - every half hour, centaury and cumin - every hour or two.
- Dried fireweed and red clover in inflorescences (1 tablespoon), taken in equal parts, are boiled for about three minutes, then filtered and taken three times a day before meals, a tablespoon.
- Dry dill (a handful) is poured with boiling water and stored in a thermos for half an hour. Drink half a glass three times a day before meals for 1.5 months. Dill essential oils dilate blood vessels and reduce blood pressure, improve blood flow.
- For dizziness, 250 g of onions are ground in a meat grinder, mixed with a glass of honey and added to the diet for a month - a tablespoon three times a day before meals.
- Clover inflorescences at the rate of 2 g per 300 ml are kept in boiling water for half an hour. After this, the infusion is filtered and taken four times a day before meals, ¼ cup.
- During the initial phase of clover blossoming, clover heads are collected and placed in a jar, but not compacted. The mound is filled with vodka and infused for three weeks. Take a teaspoon three times a day before meals.
237
Features of attacks
Patients can feel the approach of an attack by the following signs:
- lack of coordination, especially with sudden movements,
- a feeling of tide or filling in the ear,
- ringing or noise in the ears.
If an attack occurs without any warning signs, the patient may fall and be injured. Due to vestibular disorders, a person cannot stand up.
At the end of the attack, patients feel:
- weakness, fatigue,
- headaches, heaviness in the head,
- instability, lack of coordination,
- drowsiness,
- hearing loss,
- unsteady gait.
Meniere's disease has an unpredictable course. The periods between attacks, their frequency and strength may increase or decrease. Sometimes the attacks follow each other, and at times the periods between them stretch for several years. Factors that can trigger an attack include:
- stressful situation,
- drinking alcohol,
- lack of sleep,
- increase in body temperature,
- overwork,
- ARI or ARVI,
- change in atmospheric pressure,
- tobacco smoke,
- sudden noise
- taking coffee,
- excess salt in food,
- medical procedures performed on the ear,
- strong nose blowing.
The onset of attacks also depends on the course of the underlying disease, which causes an increase in the production of endolymph.
Patients do not notice any manifestations of the disease between attacks. Sometimes they complain of slight dizziness or slight ringing in the ears, which cannot be treated.
Helping a patient during an attack
The patient should be placed on his back with his head turned to the side. Dim or turn off the lights and ensure silence.
Taking antiallergic medications reduces dizziness, and antiemetics are taken to relieve nausea and prevent vomiting.
Treatment methods
Treatment of Meniere's disease should be aimed at stopping its progression. The main goal of therapy is to establish control of symptoms. Medicine is unable to completely get rid of the disease . To control attacks in the treatment of Meniere's disease, the following are used:
- Anti-nausea remedies.
- Antihistamines.
- Vasodilators. Such drugs can reduce headache attacks. But such drugs are not prescribed to all patients.
- Neuroleptics.
- Preparations for dilating the blood vessels of the inner ear.
You can most often stop an attack at home, without hospitalizing the patient. But, if the patient experiences repeated bouts of vomiting, he needs to have IVs installed to administer antiemetic drugs.
In order to reduce the volume of fluid in the body, it is necessary to take diuretics. This allows you to normalize pressure, including in the inner ear. Diuretics are prescribed for a long period of time, so patients are advised to simultaneously take vitamins and minerals. Drugs in this group wash away beneficial substances from the body.
Treatment of Meniere's disease must be carried out using drugs that improve cerebral circulation. Such drugs normalize metabolism in brain tissue and tone blood vessels. Meniere's syndrome is treated by giving an injection directly into the middle ear. This procedure has an effect similar to surgery.
The following agents are introduced into the ear:
- Antibiotics – Gentamicin, it relieves the intensity of attacks. But this type of treatment carries a high risk of complete hearing loss.
- Hormonal drugs - Dexamethasone, Prednisolone. They reduce the risk of hearing loss and also help establish control over the condition and progression of the disease.
Surgical treatment of Meniere's disease is prescribed if conservative methods do not lead to any result.
Diagnosis of the disease
ENT doctors and neurologists are involved in the diagnosis and treatment of pathology. If the patient has dizziness, tinnitus and hearing loss, the diagnosis is made without much difficulty. To confirm it, additional diagnostic studies are carried out.
The examination of patients traditionally begins with otoscopy, which is an examination of the surface of the eardrum and ear canal using a special device - an otoscope. Then they move on to additional instrumental techniques: audiometry, tympanometry, reflexometry, tuning fork examination, impedance measurement, electrocochleography, otolitometry, stabilography, videooculography and electronystagmography.
To carry out differential diagnosis and exclude other pathologies that can provoke paroxysmal dizziness, nuclear magnetic resonance, rheovasography, and doppleroscopy of cerebral vessels are used.
A CT scan of the brain is performed to exclude other damage to the structures of the inner ear. Vestibulometry reveals hyporeflexia of the vestibular analyzer, which is replaced by hyperreflexia during an attack. All patients are required to be examined by a neurologist, establish their neurological status, and undergo an examination, including electroencephalography, echoencephalography, rheoencephalography, and duplex ultrasound scanning.
Treatment with traditional methods
Traditional methods can be used to treat Meniere's syndrome:
- 2 tablespoons of hawthorn fruits must be washed, dried and finely chopped. Pour 300 ml of boiling water over the berries, brew in a thermos and drink throughout the day.
- You can prepare a remedy from elecampane root . One teaspoon of root is poured into 200 ml of warm water, then leave for 10 minutes. Strain the resulting product and drink 50 ml throughout the day.
- Calendula – this plant helps remove excess fluid from the body. 10 grams of dried flowers are brewed in 200 ml of water. You need to take one tablespoon three times a day.
- The seaweed is dried and crushed into powder. You should eat one teaspoon before lunch.
- You can make a vodka tincture from clover inflorescences . 2 tablespoons of clover should be poured over half a liter of vodka, the tincture is prepared in a dark place for 10 days in a glass container. Drink one teaspoon of tincture before meals. The course of treatment is long, at least three months.
It is important to understand that traditional medicine cannot replace drug treatment. But together they relieve symptoms well.
Symptoms of the disease
Symptoms of Meniere's disease are characterized by the fact that an exacerbation can be replaced by a complete remission, during which hearing is restored. As the disease progresses, even during remission, hearing is not restored. A person’s performance decreases and vestibular disorders appear.
The manifestation of the disease occurs in attacks, during which a person feels a ringing in the ears, which a person hears regardless of whether there is a source of noise nearby or not. Patients often compare this sound to a bell. It can intensify at the beginning of the attack and change throughout it.
Hearing loss or decrease. A person stops completely hearing low-frequency sounds. This is a sign that allows you to diagnose Meniere's syndrome. Particular sensitivity occurs to high-pitched sounds, and increased noise may cause ear pain .
The patient is worried about dizziness, which is accompanied by a feeling of nausea and vomiting that occurs repeatedly. The head can become so dizzy that a person loses balance, and it seems to him that all objects are spinning around him. The patient may feel a feeling of the body sinking. The attack can be felt from several minutes to several hours. The patient's condition worsens when trying to turn his head.
There is a feeling of pressure and congestion in the ear cavity. This feeling intensifies before an attack. During an attack, the patient may experience rapid oscillatory movements of the eyeball. They intensify when the patient lies on the inflamed ear. A person is worried about shortness of breath, increased sweating, and pale skin.
The patient's coordination is impaired, which can lead to a sudden fall. The person begins to sway from side to side. The seriousness arises from the fact that there are no harbingers of the coming fall. The man falls sharply. This could result in serious injury. After the attack passes, the person may be left with a feeling of heaviness in the head and tinnitus. The patient feels weak. As the disease progresses, symptoms intensify.
After a long course of the disease, hearing impairment begins to progress. At the very beginning of Meniere's disease, a person cannot distinguish only low-frequency sounds, but later he ceases to distinguish the entire auditory range. Hearing loss gradually turns into complete deafness. As soon as a person becomes deaf, dizziness stops bothering him.
Many patients can anticipate the onset of an attack. They first begin to hear a slight ringing in their ears. Sometimes the harbinger of an attack is a temporary improvement in hearing.
Prevention
Since the exact causes of Meniere's disease have not been established to date, preventive recommendations are of a very general nature:
- Strengthening the immune system: giving up bad habits, a balanced diet (fewer preservatives and additives), if possible, eliminating stressful situations from life;
- Avoiding skull injuries, especially when doing extreme sports, when riding a motorcycle or bicycle;
- Reducing the manifestation of provoking factors by treating the underlying disease (allergies, viral infections, vascular lesions, endocrine pathologies).
The same measures should be used by patients with Meniere's disease; they will help reduce the frequency of attacks and reduce their effectiveness.
Everything you wanted to know about acute tracheitis: what are the first symptoms, why does it appear and how to treat
This article will tell you how to treat tonsillitis during pregnancy //drlor.online/zabolevaniya/gortani-glotki-bronxov/angina/osobennosti-lecheniya-tonzillita-pri-beremennosti.html
Treatment of tracheitis in children //drlor.online/zabolevaniya/gortani-glotki-bronxov/traxeit/simptomy-i-ego-lechenie-u-detej.html
Treatment
Treatment of Meniere's disease is empirical (experimental, observational). Taking into account the nature and severity of the symptoms, and excluding other diseases affecting the inner ear, the doctor prescribes treatment. Therapy is aimed at eliminating symptoms and reducing the manifestations of the disease, which worsen the patient’s quality of life. During an attack, the effect of dizziness is relieved.
In the period between attacks, Meniere's syndrome is treated as a chronic, progressive pathology, influencing the mechanisms of the pathological process. After a course of therapy, patients tolerate attacks of dizziness more easily. However, existing treatment methods cannot prevent the progression of sensorineural hearing loss or significantly affect the pathological process. Main therapeutic methods:
- Drug therapy. The drugs Betahistine dihydrochloride, diuretics (diuretic effect), glucocorticosteroids (anti-inflammatory, immunostimulating effect) are prescribed.
- Surgical intervention (dissection of the endolymphatic canal) in the area of the endolymphatic system.
- Destruction of the labyrinth (chemical, ultrasound).
- Vestibular neurectomy (destruction of the vestibulocochlear nerve), laser destruction of the ampulla of the semicircular canal are operations that are performed to treat dizziness in the later stages of the disease.
Additional treatment methods include psychotherapy, lifestyle changes (diet low in salt, caffeine, alcohol, exclusion of trigger factors that provoke dizziness - stress, physical fatigue). During an attack, the patient is placed in a horizontal position.
The patient should avoid sharp turns of the head, and should not close the eyes (the gaze is fixed on a stationary target). Drug therapy during an attack includes vestibular suppressants (antihistamines, anticholinergics) and antiemetics (medicines against nausea and vomiting).
Possible complications
Since a complete cure for Meniere's disease is impossible, but comes down to reducing symptoms, in particular, the severity of attacks of dizziness, the main complication of the disease is the psychological aspect and a violation of social status. The patient experiences fear of attacks that occur suddenly, and is no longer able to cope with all matters, both personal and social.
The second serious consequence of the developing disease is progressive hearing loss, which without proper treatment can develop into complete deafness. This also contributes to the loss of the individual from society - without normal hearing, the patient cannot communicate, work and relax. In combination with attacks of dizziness, this can have a very strong negative effect on the nervous system, and even cause severe nervous pathologies.
With timely and correct treatment, Meniere's disease is curable in most cases.
Modern possibilities for diagnosing and treating Meniere's disease
For the first time, a symptom complex characterized by hearing loss, tinnitus and periodic dizziness was described by P. Meniere in 1861. At the same time, P. Meniere suggested that this condition is associated with pathology of the inner ear [1]. Later (in 1938), Hallpike and Cairns proved that the basis of Meniere's disease is endolymphatic hydrops [2]. Despite the constant long-term interest in this problem, the etiology of the disease remains unclear. There are various theories about the development of Meniere's disease. According to the anatomical theory, Meniere's disease may be associated with pathology of the structure of the temporal bone, in particular, reduced pneumatization of mastoid cells and hypoplasia of the vestibular canal, while the small endolymphatic sac is incorrectly located behind the labyrinth. Genetic: hereditary transmission of Meniere's disease was identified more than half a century ago, and the results of recent studies indicate an autosomal dominant type of inheritance of this pathology. It is believed that the DFNA9 region of the COCH gene plays a special role. The immunological theory is supported by the detection of immune complexes in the endolymphatic sac in patients with Meniere's disease. The vascular theory is supported by the frequent combination of Meniere's disease with migraine, which was noticed by P. Meniere himself. Allergic reaction. The incidence of allergic reactions in patients with Meniere's disease is higher than in the general population. Thus, of 734 patients with Meniere's disease examined by MJ Derebery (USA), 59% said that they suffered from known or suspected allergies to airborne agents, and 40% from known or suspected allergies to food products. By comparison, the incidence of allergic reactions in the US population is approximately 20%. According to the metabolic theory, with Meniere's disease, potassium retention occurs in the endolymphatic space. This causes potassium intoxication of hair cells and vestibular neuroepithelium, resulting in hearing loss and dizziness. Many authors are inclined to the polyetiology of this disease and identify “causing factors” and “predisposing factors” [3]. Prevalence Meniere's disease affects predominantly Caucasians, regardless of gender. The average age of patients ranges from 20 to 50 years, but the disease can also occur in children. The disease is somewhat more common in people with intellectual work and in residents of large cities. Clinical picture In the vast majority of cases (80–90%), Meniere's disease is characterized by unilateral lesions with possible “involvement in the pathological process” to varying degrees of the second labyrinth. In this case, we should talk about “bilateral disease” [4,5]. Meniere's disease can debut with both vestibular and auditory (hearing loss, ear congestion, tinnitus) disorders. Hearing loss can be gradually increasing or fluctuating (transient) - at the same time, at the beginning of the disease (in the first 2-3 years), almost complete restoration of hearing is observed in the interictal period. Over the years, hearing decreases, up to complete deafness. The most painful symptom of Meniere's disease is dizziness: systemic, accompanied by spontaneous nystagmus, ataxia, coordination disorders, pronounced autonomic manifestations (hypersalivation, hyperhidrosis, blood pressure fluctuations, dyspeptic disorders). The duration of the attack varies from several minutes to days (status meniericus). The severity of dizziness can also vary: from mild “precursors” to a violent reaction, during which patients take a forced position on their side, corresponding to the sore ear (or the direction of the fast component of spontaneous nystagmus). Ataxia and coordination disorders persist for several days after the end of the attack. Vestibular manifestations of Meniere's disease are characterized by periods of remission and obvious manifestations of vestibular dysfunction. In the first years of the disease (up to 3 years), during periods of remission, even when conducting experimental vestibular tests, vestibular dysfunction is not always detected. Later, in the interictal period, vestibular hyporeflexia is recorded on the affected and then on the opposite side. Typically, after 10 years or more, the severity of vestibular manifestations decreases. The American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS) (1995) defines “obvious” Meniere's disease as follows: • two or more spontaneous attacks of dizziness lasting 20 minutes. and more; • hearing loss confirmed by audiological studies in at least one case; • tinnitus or a feeling of fullness in the causative ear; • other reasons are excluded. In the classic course of Meniere's disease, three stages of the disease are distinguished: I – the predominant symptom is dizziness, often accompanied by nausea and vomiting. Paleness and sweating may occur. Typically, an attack of dizziness is preceded by a feeling of pressure in the ear or the corresponding half of the head, lasting from 20 minutes. up to several hours. Between attacks, hearing is normal. II – sensorineural hearing loss develops with a predominant decrease in sound perception at low frequencies. Attacks of dizziness reach maximum severity with a subsequent tendency to reduce the severity of manifestations. III – there is a progressive decrease in hearing with the development of bilateral deafness. Episodes of dizziness decrease and then disappear completely; however, ataxia may persist, especially in the dark. Differential diagnosis and additional studies Diagnosis of the classic form of Meniere's disease is based on characteristic clinical manifestations and audiometric data. Difficulties in making a diagnosis may be due to the fact that many patients whose disease begins with attacks of dizziness cannot clearly describe their complaints. In addition, there are a number of diseases and conditions accompanied by vestibular disorders (6): • benign paroxysmal positional vertigo; • vertebrobasilar insufficiency; • vestibular neuronitis; • traumatic brain injury; • fistula of the labyrinth; • infectious labyrinthitis; • consequences of otosurgical interventions; • otosclerosis; • cerebellopontine tumors; • multiple sclerosis; • side effects of medications; • acute purulent otitis media; • hyperventilation. The final diagnosis of Meniere's disease is made based on the results of dehydration tests (in response to drug dehydration, sound perception thresholds at low frequencies are lowered and auditory perception of speech is improved), transtympanic electrocochleography (a curve characteristic of endolymphatic hydrops) [7]. The summation potential (SP) and action potential (AP) are recorded. Violation of the ratio of SP/AP amplitude values (p>0.3) is a characteristic sign of hydrops of the labyrinth, recording of vestibular evoked myogenic potentials (characteristic is the absence of peaks P13, N23 - a graph in the form of a straight line). Examination of patients with Meniere's disease should include a number of mandatory tests. Traditional equilibrium tests that are diagnostically quite reliable include the Romberg test, the Unterberger test, the Babinski-Weil test, and the Barany index test. The listed studies have somewhat lost their significance in recent years, since specialized clinics use special equipment for vestibulometry and complicated tests. Caloric tests (heat and cold) are carried out by irrigating the external auditory canal along its posterior-superior wall with water (with air - in the presence of perforation of the eardrum). The water (air) temperature should be at least 7°C higher or lower than the patient’s blood temperature. The subject is in a supine position so that his head is at an angle of 30° to the horizontal axis. According to the theory of R. Barany, under the influence of cooling or heating of individual sections of the semicircular canals, the endolymph changes its density, and therefore the cooled endolymph particles sink down, and the warm ones rise up. The movement of endolymph causes irritation of the vestibular apparatus. The cause of caloric nystagmus is the convection currents of the endolymph resulting from changes in its density during heating and cooling. The direction, duration and amplitude of nystagmus are assessed. Barany rotation test - the patient is in a Barany chair with the head lowered forward 30° (horizontal channels in the plane of rotation). Using a special handle, the researcher makes 10 full rotations of the chair in 20 seconds. in both directions with an interval of 5 minutes. After the chair stops, the subject raises his head and fixes his gaze on an object located 60–70 cm from the face and shifted from the midline in the direction opposite to the rotation by 45°. Normally, the nystagmus is small-scale, degree I, lasting 20–30 s. During rotation, the labyrinths located in the plane of rotation are irritated, and to a greater extent the one in which, after stopping, the endolymph flow is directed to the ampulla. Conducting a smooth pursuit test is necessary, since most vestibulometric tests are based on assessing eye movements; it is important to assess the state of the actual oculomotor function of a particular subject. This test makes it possible to identify asymmetric movements, “catch-up” (corrective) saccades, indicating pathological changes in the central nervous system (impaired oculomotor function, damage to areas of the cerebral cortex in the occipital and/or parietal lobes, in the pons or cerebellum). The subject follows with his gaze (the head is motionless) the tip of a pencil moving in a horizontal plane (right-left) at a distance of approximately 60 cm from his face. The doctor observes the patient's eye movements, assessing their smoothness and familiarity. Saccade test - two objects (for example, pencil tips) are placed at a distance of 50–60 cm from the patient’s face, forming an angle of 30–40°. The patient is asked to move his gaze from one tip of the pencil to the other. The accuracy of the study increases when tracking moving stimuli (for example, pencils) moving in a random manner (randomized saccades). Saccades are rapid conjugal deviations of the eyes (lasting from 10 ms to 80 ms) during the fast phase of vestibular and optomotor nystagmus, the initial phase of the tracking reaction, when the eye jump “captures” a moving visual target during visual inspection of the external world. Deviation of the results from the accepted norm may indicate the presence of retrolabyrinthine disorders. Optokinetic nystagmus is examined using a rotating drum with black and white stripes applied to it. The drum is rotated by the researcher's hand or driven by a motor at a certain speed. The patient is located at a distance of 1 meter from the cylinder. The frequency of optokinetic nystagmus increases as the cylinder rotation speed increases from 1 to 6 rpm. Retrolabyrinthine disorders are characterized by dysrhythmia, complete loss of reactions or changes in the shape of nystagmus cycles. In our clinic, patients undergo a comprehensive audiological (including transtympanic electrocochleography) and vestibulometric study, including the study of spontaneous otoneurological symptoms, optokinetic nystagmus, tests of smooth visual pursuit, visual saccades, Dix/Hallpike positional test, bittermal (+30° and +44° ) binaural caloric test, rotation test with recording on VNG Stad Alone Unit VO 25 (Heinemann Medizintechnik GmbH), study of statics, coordination and gait on the posturographic complex Smart EquiTest Balans Master (NeuroCom), recording of vestibular evoked myogenic potentials on the electromyographic complex Nicolet Viking Select . Electrocochleography with a transtympanic method of installing an electrode on the promontorial wall is performed using a Nicolet Viking Quest unit. Treatment Since there is no consensus on the etiopathogenesis of Meniere's disease, treatment of this disease is empirical. All currently existing methods and methods of treatment are aimed at making patients more tolerant of attacks of dizziness, but do not significantly change the course of the process and do not prevent the development of hearing loss [6]. However, individual therapy, selected taking into account concomitant diseases, can slow down the development of hearing loss, reduce the severity of tinnitus, and reduce the frequency and severity of dizziness [5]. Conservative measures When treating an acute attack of Meniere's disease, mainly medication and, if conditions exist, carbogen or oxygen therapy are used. They use sedatives and drugs that improve cerebral circulation (prochlorperazine, promethazine, cinnarizine, diazepam) [6], and dehydration agents. In the acute period, it is advisable to administer drugs parenterally or in suppositories. It is advisable to carry out behind-the-ear novocaine blockades [4]. One of the most well-known schemes for relieving an acute attack of Meniere’s disease is the scheme developed by I.B. Soldatov and N.S. Khrappo (1977): glucose 40%–20.0 i/v, pipolfen 2.5%–2.0 i/m (or aminazine 2.5%–1.0 i/m), atropine sulfate 0.1% –1.0 s.c. (or platiphylline hydrotartrate 0.2%–2.0 s.c.), caffeine–sodium benzonate 10%–1.0 s.c.; mustard plasters on the cervical-occipital region, a heating pad on the legs [8]. Sometimes xanthinol nicotinate 15%–2.0 IM or cinnarizine or vinpocetine is added to the indicated regimen [4]. Treatment in the interictal period (maintenance therapy) should be comprehensive and quite active. Drugs that prevent the development or reduce endolymphatic hydrops are indicated: diuretics (furosemide, amiloride, hydrochlorothiazide), vasodilators (histamine analogue - betahistine dihydrochloride), drugs that improve cerebral circulation (cinnarizine, propranolol), corticosteroids, as well as non-drug treatment - vestibular rehabilitation, acupuncture . One of the medications that effectively eliminates dizziness and reduces subjective ear noise is betahistine dihydrochloride (Vestibo), a synthetic analogue of histamine. Betahistine dihydrochloride was first synthesized in 1941 by Walter et al., and in 1970 it was registered as a drug for the treatment of Meniere's disease. Betahistine dihydrochloride does not have such histamine side effects as severe headache, facial flushing, diplopia and vomiting, and it is taken orally. According to modern concepts, betahistine dihydrochloride has three levels of action: • On the cochlear bloodstream • On the central vestibular apparatus • On the peripheral vestibular apparatus. Being a weak H1 receptor agonist and an active H3 receptor blocker, this drug stimulates postsynaptic histamine receptors. It is the H3 antagonistic effect of betahistine dihydrochloride that explains the effect of normalizing the excitation of the vestibular nuclei in the subcortical structures of the central nervous system and the vasoactive component of the action of this drug [9,10]. It should be emphasized the selectivity of the vasoactive effect of betahistine dihydrochloride [9], which improves microcirculation of the inner ear and capillary permeability, and also normalizes endolymph pressure in the labyrinth, without leading to a pronounced decrease in blood pressure. The drug also has a positive effect on the transmission of nerve impulses in the medial and lateral vestibular nuclei and peripheral vestibular receptor formations [11]. The experience of many clinicians indicates that betahistine dihydrochloride reduces the intensity of dizziness, shortens the duration of dizziness episodes, and makes them more rare. The drug is effective both for relieving attacks of dizziness and preventing their relapses, and for reducing subjective ear noise. In the period from October 2006 to September 2007, we observed 18 patients with Meniere's disease (interictal period) aged from 34 to 52 years (13 women and 5 men), the duration of the disease ranged from a year to 15 years. During an audiological examination, unilateral impairment of sound perception was registered in 11 patients, bilateral – in 7. The diagnosis of Meniere's disease in all patients was established based on the results of a dehydration test (with xylitol), electrocochleography and the results of registration of vestibular evoked myogenic potentials. All patients had static ataxia, mainly due to the vestibular component (during digital posturography) and experimental vestibular (peripheral) hyporeflexia (in 13 patients - bilateral). For 2 months, all patients received betahistine dihydrochloride (48 mg/day). As a result of the treatment, all patients, during the control posturography, recorded a decrease in static ataxia, and 12 of them - the results of a re -study of the equilibrium function were within the accepted age norm (Fig. 1). All patients have a positive dynamics of re -vestibulometry indicators. None of the patient was recorded in the side effects, the treatment was suffered well. It is advisable to use betagistine dihydrochloride in the postoperative period (in particular after the lasergutition of the labyrinth) - dizziness, as a rule, disappears on the 3-4th day after surgery [5]. The use of aminoglycosides that have a toxic effect in relation to neuroepithelium of the inner ear is apart. The method can be used in the later stages of BM for bilateral lesion and is used in persons who are contraindicated in surgical treatment. Intra -Panelal administration of aminoglycosides is quite effective and possibly with one -sided lesion [12]. Surgical treatment with obvious inefficiency of conservative treatment is advisable for various surgical interventions, both sparing (auditory -preserving) and destructive. Destructive methods are indicated in severe disabled forms of Meniere's disease. 5 groups are distinguished: 1 - interventions on the autonomous nervous system (chord - and chordplexusectomy); 2 - interruption of tendons of the muscles of the drum cavity; 3 - decompressive operations on the inner ear; 4 - destructive operations on the maze; 5 - destructive operations on the prejudice - upper nerve [5]. The auditory -preserving operations include: • Shunting of an endolymphatic bag - the most common surgical intervention at BM; • Sacculotomy - a decompressive operation on a spherical bag; • The intersection of the vestibular nerve in order to stop the afferent impulse, which contributes to the disappearance of vestibular disorders. With unsuccessful sparing types of surgical interventions, such destructive operations as: • Labyrintectomy; • Kochleosakkulotomy; • Vestibular neurectomy. It should be noted that operations on the autonomous nervous system and interruption of tendons of the muscles of the drum cavity are ineffective, and decompressive and destructive surgical interventions, as a rule, lead to deafness to the operated ear and renew the seizures of dizziness in a long period due to fibrous infection of the created susters; Destructive operations on the pre -war -upper nerve are performed in neurosurgery departments. Currently, two more operations are distinguished: cochlear implantation and lasergustration of the ampoule of the horizontal semicircular canal, which allows you to get rid of dizziness in the next and remote dates, maintain hearing and delay the development of the hydropical process in another ear during a one -way process. However, despite the abundance of scientific papers on Meniere's disease, many means and methods used in its treatment, the problem, in essence, remains unresolved, since so far there is no unified medical tactics recognized by all leading specialists.
References 1. Menie?re MP Pathologie auriculare. Maladies de l'orielle interne offrant les symptoms de la congestion cerebrale apoplectiforme//Gaz. Med. de Paris. – 1861. – t. 16. – P. 88–89. 2. Hallpike CS, Cairns H. Observation on the pathology of Meniere's syndrome// J. Laryngol. Otol. – 1938. – Vol. 53. – P. 625–655. 3. Sagalovich B. M., Palchun V. T. Meniere’s disease. – M.: Medical Information Agency LLC, 1999. – 525 p. 4. Babiyak V.I., Lantsov A.A., Bazarov V.G. Clinical vestibulology. – St. Petersburg: “Hippocrates”, 1996. – 336 p. 5. Patyakina O.K. Therapeutic tactics for vestibulogenic dizziness // Consilium medicum. Application. – 2001. – p. 9–12. 6. Nurmukhametova E. Diagnosis and treatment of Meniere’s disease // Russian Medical Journal. – 1998. – No. 20. - With. 1346–1347. 7. Gibson WP R, Prasher DK, Kilkenny GPG Diagnostic significance of transtympanic electrocochleography in Meniere's diseas // Ann. Otol. Rhinol. Laryngol. – 1983. – Vol. 92. – P. 155–159. 8. Soldatov I. B., Khrappo N. S. Methods of treating Meniere’s disease // Journal. ear, nose and throat bol. – 1977. – No. 6. p. 8–14. 9. Timmerman H. Pharmacotherapy of vertigo: any news to be expected? Acta Otolaryngol.(Stockh)1994,Suppl 513,28–32. 10. Van Cauwenberge PB, De Moor SEG Physiopathology of H 3-receptors and pharmacology of betahistine // Acta Otolaryngol. (Stokh). – 1997. – Suppl. 526. – P.43–46. 11. Arrang JM, Garbarg M, Quach TT, Toung MDT, Yeramian E, Schwarts JC Actions of betahistine at histamine receptors in the brain. Eur Pharmacol. – 1985. – Vol. 11. – P. 73–84. 12. Pfleiderer AG The current role of local intratympanic Gentamicin therapy in the management of unilateral Meniere's disease. Clin Otolaryngol. – 1998. – Vol.23 (1). – P. 34–41.
Meniere's disease code according to ICD-10
ICD-10 is an international classification of diseases, that is, it is a kind of rubricator of diseases and pathologies. Every diagnosis or condition known in the world is assigned a specific code. Each code has an alphanumeric designation. In this encrypted form, it is much easier to store and analyze data on morbidity and mortality obtained from different parts of the world.
Once every decade, this classification is revised under the guidance of the World Health Organization (WHO). The number 10 in the abbreviation ICD-10 indicates that the current classification has already been revised ten times.
According to this classification, Meniere's disease is coded H81.0.